Abstract
Neuroimaging studies have shown that chronic pain is maladaptive and influences brain function and behavior by altering the flexible cerebral information flow. We utilized power spectral analysis to investigate the impact of classic trigeminal neuralgia (TN) on the oscillation dynamics of intrinsic brain activity in humans. The amplitude of low-frequency fluctuations (ALFF) and fractional ALFF (fALFF) were measured in 29 TN patients and 34 age- and sex-matched healthy controls (HCs) via resting-state functional MRI (R-fMRI). Two different frequency bands (slow-5: 0.01–0.027 Hz; slow-4: 0.027–0.073 Hz) were analyzed. Differences in blood oxygen level-dependent (BOLD) signal fluctuations and related resting-state functional connectivity (rsFC) between the TN patients and HCs were identified. The TN patients had reduced ALFF/fALFF in the posterior cingulate cortex (PCC), left insula, left dorsolateral prefrontal cortex (DLPFC), left putamen and bilateral temporal lobe, exclusively in the frequency of the slow-5 band. Whole brain rsFC analyses with these six different regions as seeds revealed two weaker circuits including the PCC-medial prefrontal cortex (mPFC) and DLPFC-hippocampus circuits, indicating abnormal interactions with the default mode network (DMN) in TN patients. The functional connectivity between the default-mode regions (mPFC and PCC) in the slow-5 band tracked pain intensity. Together, our results provide novel insights into how TN disturbs the cortical rhythms and functional interactions of the brain. These insights may have implications for the understanding and treatment of brain dysfunction in chronic pain patients, including TN patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Classical trigeminal neuralgia (TN), one of the most painful diseases in humans, is characterized by paroxysmal attacks of intense, sharp or lancinating pain lasting from a split second up to 2 min and is located in the distribution of the trigeminal nerve (Maarbjerg et al. 2015). The pain may occur spontaneously or be provoked by trigger factors (Maarbjerg et al. 2015). As the disorder progresses, pain may become frequent and sustained, thereby increasing the risk of anxiety and depression and substantially diminishing the quality of life (Meskal et al. 2014; Wu et al. 2015).
Chronic pain, including TN, is maladaptive for the brain (Baliki et al. 2011a). The brain of a TN patient must process both the normal resting activity and the intermittent painful input, which disturbs the flow and integration of information across brain regions. By exploring the relationship between TN and gray matter morphology, several structural imaging studies have shown that TN patients display gray matter volume reductions in various brain regions, including the cingulate cortex, insula, limbic, subcortical, and temporal regions (Desouza et al. 2013; Gustin et al. 2011; Li et al. 2017; Obermann et al. 2013; Wang et al. 2017). More recently, observations of abnormal microstructure within various white-matter tracts have been reported in TN (DeSouza et al. 2014; Wang et al. 2017). These results indicate that TN is associated with structural alterations in distributed brain regions.
However, these findings have ignored that the experience of pain in the brain is not static and is highly flexible (Rogachov et al. 2016). This flexibility requires dynamic changes in neuronal integration that are not provided by structural changes; rather, they involve dynamic changes in brain oscillations and functional connections (Ploner et al. 2017). Consistently, the recent concept of the dynamic pain connectome emphasizes that the dynamics of flexible brain oscillations and functional connections in the default mode network (DMN), salience network (SN), and nociceptive system are responsible for pain processing (Cheng et al. 2017; Kucyi and Davis 2015, 2016). Specifically, abnormal brain rhythms at different frequencies have been identified for various chronic pain conditions in previous functional imaging studies (0.01–0.25 Hz) and EEG/MEG studies (range from theta-delta to gamma oscillations) (Baliki et al. 2011a; Malinen et al. 2010; Sarnthein et al. 2006; Stern et al. 2006). Thus, as a specific condition of chronic pain, TN may also be associated with specific brain alterations with complex temporal-spectral patterns of dynamic neuronal activity in spatially extended networks.
Resting-state functional MRI (R-fMRI) is a promising imaging technique that enables researchers to investigate brain properties as a function of different frequencies of blood oxygen level-dependent (BOLD) signal oscillations (Baliki et al. 2011a; Baria et al. 2011). This approach, as opposed to correlation-based analyses, may identify the oscillatory dynamics of the BOLD signal along a wide range of frequencies, thus providing novel insights regarding abnormalities in spontaneous brain activity underlying chronic pain (Baliki et al. 2011a). For example, chronic back pain patients show increased high-frequency (0.12–0.20 Hz) BOLD signal oscillations circumscribed mainly to regions in the DMN (Baliki et al. 2011a) and SN (Malinen et al. 2010). Chronic neuropathic pain exhibits altered low-frequency (0.03–0.06 Hz) BOLD signal oscillations within the ascending pain pathway (Alshelh et al. 2016). Interstitial cystitis/painful bladder syndrome is associated with altered slow-5 band (0.01–0.027 Hz) BOLD signal oscillations in the sensorimotor network (Kilpatrick et al. 2014). Thus, these studies have further demonstrated that chronic pain is associated with frequency-dependent alterations in BOLD signal oscillations, and these changes are dependent on pain conditions. However, in contrast to many other neuropathic pain patients, TN patients typically do not exhibit major sensory loss and are pain-free between pain attacks (DeSouza et al. 2014; Nurmikko and Eldridge 2001). Furthermore, different types of pain may affect different areas of the brain (Gustin et al. 2011). The extent to which these changes in brain oscillations are involved in TN patients and whether they are frequency dependent remain to be determined.
Thus, we initially calculated the amplitude of low-frequency fluctuations (ALFF) and fractional ALFF (fALFF) (Zang et al. 2007; Zou et al. 2008) at different frequency bands to investigate frequency-specific alterations in intrinsic brain oscillations in TN patients. The frequency spectrum of BOLD signal oscillations could be decomposed into distinct frequency bands to better reflect the neural origin of the sources (Zuo et al. 2010). More importantly, Zuo et al. (2010) showed that the ALFF of gray matter was the greatest at the slow-4 (0.027–0.073 Hz) and slow-5 (0.01–0.027 Hz) frequency bands. Furthermore, by investigating the ALFF/fALFF at the slow-4 and slow-5 bands, an expanding body of studies has identified frequency-dependent changes in brain oscillations in various neuropsychiatric conditions (Kilpatrick et al. 2014; Zhang et al. 2015; Zhou et al. 2017). Motivated by the previously developed framework, we also selected the slow-4 and slow-5 bands to address how amplitudes of fluctuations change specifically in TN patients. Moreover, the ALFF is thought to reflect the local or regional brain activity (Zuo et al. 2010), whereas resting-state functional connectivity (rsFC) is thought to characterize the brain at a functional circuit or network level. As rsFC is defined as the inter-regional BOLD signal correlations, it is theorized that the shift in the ALFF/fALFF is coupled with changes in rsFC (Baliki et al. 2011a). Furthermore, rsFC studies using regional alterations in ALFF as seeds, which would take advantage of the cross-information from both regional and inter-regional features, have provided nuanced insights into the neural underpinnings of various chronic pain conditions, although not in TN (Baliki et al. 2011a; Kilpatrick et al. 2014). A recent study has demonstrated that slow-5 dynamic rsFC reflects the capacity to sustain cognitive performance during pain (Cheng et al. 2017). Thus, we further used the regions showing altered ALFF as seeds in subsequent rsFC analyses to identify specific circuits related to these BOLD oscillations that differ between TN patients and HCs.
Based on previous reports of other chronic pain conditions (Alshelh et al. 2016; Baliki et al. 2011a; Kilpatrick et al. 2014), we hypothesized that (1) altered ALFF/fALFF in TN patients may depend on the specific frequency bands, particularly the slow-4 and slow-5 bands that were primarily associated with neuronal oscillations, and (2) these changes in oscillatory dynamics would be related to functional connectivity alterations within resting-state networks.
Materials and methods
Subjects
This study included 63 subjects: 29 consecutive patients with classical TN (19 women and 10 men; mean age ± SD: 48.1 ± 11.9 years) and 34 healthy controls (HCs) with similar distributions of age, gender and years of formal education (21 women and 13 men; mean age ± SD: 43.3 ± 10.1 years). All patients had right-sided pain and met the criteria of the International Headache Society for TN. All patients had painful attacks of active TN at the time of study inclusion. No patients had undergone prior micro-vascular decompression (MVD) surgery or other treatments (i.e., gamma knife radiosurgery) for TN or received tricyclic antidepressants, opioids, or serotonin/norepinephrine reuptake inhibitors. Individuals were excluded if they had a history of other chronic pain conditions, psychiatric disorders, stroke/cerebrovascular ischemia, other neurological or sensory deficits or TN attributed to other disorders. According to the Edinburgh Handedness Inventory, 28 TN patients and all recruited HCs were right-handed. Written informed consent was obtained from each participant prior to study inclusion, and the study was approved by the local ethics committee of the Chinese People’s Liberation Army (PLA) General Hospital.
All subjects were asked to rate the extent of their neuralgia within 1 week on a visual analogue scale (VAS, 0–10, where 0 = no pain and 10 = maximum imaginable pain). The 17-item Hamilton Depression Rating Scale (HAMD) and the 14-item Hamilton Anxiety Rating Scale (HAMA) were used to quantify the depression- and anxiety-related symptoms of the subjects, respectively. The HAMD was administered to each participant by a psychiatrist using the Structured Interview Guide for Hamilton-Depression interview format (Williams 1988). The HAMA was administered by the same psychiatrist immediately after the HAMD interview. The TN medication statuses were also recorded for each patient.
Image acquisition
The TN patients stopped their pain medication for at least 24 h prior to the MRI scan. MRI data acquisition was performed on a GE750 3.0 T scanner with an eight-channel phase array head coil. High-resolution structural images were collected using a sagittal Fast Spoiled Gradient-Echo (FSPGR) sequence with the following parameters: repetition time (TR), 6.7 ms; echo time (TE), 2.9 ms; flip angle, 7°; slice thickness, 1 mm; no gap; 192 sagittal slices; field of view (FOV), 256 × 256 mm2 and voxel size = 1 × 1 × 1 mm3. The functional images were obtained using an echo-planar imaging (EPI) sequence with the following parameters: repetition time = 2000 ms, echo time = 30 ms, flip angle = 90°, thickness/gap = 3.5 mm/0.5 mm, slices = 36, field of view = 224 × 224 mm2 and voxel size = 3.5 × 3.5 × 3.5 mm3. During the scan, the participants were fitted with soft earplugs and instructed to keep their eyes closed, remain motionless, and not think of anything in particular. After the scanning, a simple questionnaire indicated that no participants had fallen asleep.
Data preprocessing
Image preprocessing was performed using Statistical Parametric Mapping (SPM12, http://www.fil.ion.ucl.ac.uk/spm) and Data Processing & Analysis for (Resting-State) Brain Imaging (DPABI) (Yan et al. 2016). The first ten images were discarded to ensure steady-state longitudinal magnetization, and the remaining 230 images were subsequently corrected for temporal differences and head motion. After subject selection, the translation and rotation parameters in any given data did not exceed ±1.5 mm or ± 1.5°. The mean frame-wise displacement (FD) was calculated to further determine the comparability of the head movement across the groups. T1-weighted images were co-registered to the resulting functional image using a linear transformation and were segmented into gray matter, white matter, and cerebrospinal fluid using a unified segmentation algorithm (Yan et al. 2016). The co-registered functional images were spatially normalized to the Montreal Neurological Institute (MNI) space and resampled to 3-mm cubic voxels. The global signal, the white matter signal, the cerebrospinal fluid signal and 24 head motion parameters (6 motion parameters for the current volume, 6 motion parameters for the previous volume and 12 corresponding squared items) were subsequently regressed out from the data. Finally, linear trend removal was performed to reduce the effect of low-frequency drifts.
ALFF/fALFF analysis
The ALFF/fALFF was calculated using the DPABI toolbox. Briefly, the time series data were converted to the frequency domain using a fast Fourier transform, and the power spectrum was obtained. The square root of the power spectrum was calculated and subsequently averaged across a predefined frequency interval. This averaged square root was termed the ALFF at the given voxel (Zang et al. 2007). The fALFF is the fraction of the ALFF in a given frequency band relative to the ALFF over the entire frequency range detectable in the given signal (Zou et al. 2008). Using a previously developed framework, the full frequency range (0–0.25 Hz) was divided into five different bands: [slow-6 (0–0.01 Hz), slow-5 (0.01–0.027 Hz), slow-4 (0.027–0.073 Hz), slow-3 (0.073–0.198 Hz) and slow-2 (0.198–0.25 Hz)] (Buzsáki and Draguhn 2004; Zuo et al. 2010). The signals of slow-6, slow-3 and slow-2 were discarded because they mainly reflect very low frequency drift, white matter signals, and high-frequency physiological noises, respectively (Biswal et al. 1995; Zuo et al. 2010). We computed the ALFF/fALFF at the slow-5 and slow-4 bands. Of note, the computation was constrained within a grey matter mask (Nvoxels = 45,381), which was generated by thresholding (a threshold of 0.2) on the mean GM probability map of all subjects.
To examine the effects of group, frequency band, and their interactions in ALFF/fALFF, two-way repeated-measures analysis of variance (ANOVA) was used. Group (TN patients vs. HCs) served as a between-subject factor; frequency band (slow-5 vs. slow-4) served as a repeated-measures factor; and age, gender and education level served as covariates. All statistical maps were corrected for multiple comparisons to a significant level of the cluster-forming threshold to 0.01 with a familywise error rate (FWE) corrected cluster of P < 0.05. Post hoc t-tests were performed (P < 0.05, FDR corrected) for regions that exhibited a significant interaction between groups and frequency bands.
Functional connectivity analysis
Functional connectivity analysis was performed using the seed-based approach. Regions that exhibited significant ALFF/fALFF differences between the TN patients and HCs (refer to results) were used as seeds in the subsequent rsFC analysis. Preprocessed functional data were bandpass filtered using slow-5 and slow-4 bands, and band-specific Fisher-z transformed maps of the correlation between seed time courses and all other voxels were created using DPABI. Group-level, band-specific rsFC maps were obtained by performing one-sample t-tests on spatially smoothed z maps (FWHW = 6 mm) for each individual seed. Using the nonparametric method in SPM12, the significance level was determined by the cluster-forming threshold of Pvoxel < 0.001 with a FWE corrected cluster of P < 0.05. Differences in the band-specific rsFC maps between the TN patients and HCs for each seed were separately examined using a general linear model with age, gender and education level as nuisance factors (P < 0.05, FWE corrected).
Brain-behavior relationships
To explore relationships between altered brain imaging indices (ALFF/fALFF and rsFC) and behavioral measures (pain intensity, pain duration, HAMA and HAMD scores), correlation analyses were performed using the mean ALFF/fALFF or rsFC strength within regions that exhibited significant group differences against behavioral measures, controlling for age, gender and education level.
Additional analyses for each factor involving frequency and group
To evaluate the robustness of our results, we performed additional analyses involving examining the differences of ALFF/fALFF between slow-4 and slow-5 bands in each group separately. Furthermore, we compared the ALFF/fALFF of TN patients with HCs in slow-4 and slow-5 bands, separately.
Results
Subject demographics
Table 1 summarizes the clinical and demographic characteristics of the study participants. No significant differences were found in age, gender, years of education or head movement between the TN patients and HCs. However, the TN patients showed significantly elevated HAMA and HAMD scores.
ALFF results
Main effect of the frequency band factor: The main effect of the frequency band from two-way repeated-measures ANOVA is shown in Fig. 1. Compared with the slow-5 band, the slow-4 band exhibited significantly higher ALFF in the midbrain, striatum, thalamus, hippocampus, and cerebellum and significantly lower ALFF in the medial prefrontal cortex (mPFC), temporal lobe and parietal lobe. These findings were consistent with previous studies (Zhang et al. 2015; Zuo et al. 2010, 2017).
Main effect of the frequency band factor on ALFF. Red color represents the significantly greater ALFF and blue color represents the significantly lower ALFF in the slow-4 band than in the slow-5 band. The results were obtained by a two-way repeated-measure ANOVA. FWE corrected P < 0.05. Abbreviations: ALFF, amplitude of low-frequency fluctuation; ANOVA, analysis of variance
Main effect for group factor: Specific brain regions exhibited significant main effects for group; the TN patients had lower ALFF than the HCs for the left middle/superior temporal gyrus (MTG/STG), bilateral mPFC/anterior cingulate cortex (ACC), bilateral postcentral gyrus (PoCG), and right middle frontal gyrus (MFG) (Fig. 2 and Table 2).
Main effect of the group factor on ALFF. Red color represents the higher ALFF and blue color represents the lower ALFF in the TN group than the HC group. The results were obtained by a two-way repeated-measure ANOVA. FWE corrected P < 0.05. Abbreviations: ALFF, amplitude of low-frequency fluctuation; ANOVA, analysis of variance
Interaction effects between the group and frequency band: A significant interaction was identified between the group and frequency band (Supplementary Material and Fig. S1). Furthermore, a post hoc t test revealed that ALFF exclusively decreased in the slow-5 band (0.01 to 0.027 Hz). The TN patients exhibited significantly lower ALFF in the slow-5 band in the posterior cingulate cortex (PCC), left insula, left dorsolateral prefrontal cortex (DLPFC), left temporal lobe and left putamen (P < 0.05, FDR corrected) (Fig. 3 and Table 3). Notably, the insula and DLPFC regions receive nociceptive input from the periphery and play crucial roles in pain perception and modulation (Apkarian et al. 2005; Hemington et al. 2016). The PCC and left temporal lobe are the regions of DMN.
Interaction between the frequency band and group on ALFF. A two-way repeated-measure ANOVA and a post-hoc test indicated a significantly lower ALFF in TN patients in the slow-5 band (blue color). No significant between-group differences were found in the slow-4 band. FDR corrected P < 0.05. Abbreviations: ALFF, amplitude of low-frequency fluctuation; ANOVA, analysis of variance
fALFF results
The pattern of the main effect of frequency band was very similar to that in ALFF (Fig. S2). Brain regions with a main effect of group included the left insula, mPFC/ACC, right superior frontal gyrus and left inferior frontal gyrus (Fig. S3). We also observed significant interaction between frequency band and group in the bilateral lateral temporal lobe, left insula and left putamen. Further post-hoc t test reveals that the group differences in fALFF exhibited in the slow-5 band specifically (Fig. 4 and Table 4).
Interaction between the frequency band and group on fALFF. A two-way repeated-measure ANOVA and a post-hoc test indicated a significantly lower fALFF in TN patients in the slow-5 band (blue color). No significant between-group differences were found in the slow-4 band. FDR corrected P < 0.05. Abbreviations: fALFF, fractional amplitude of low-frequency fluctuation; ANOVA, analysis of variance
Resting-state functional connectivity between TN patients and HCs
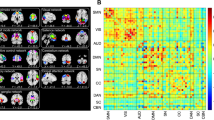
The rsFC in the slow-5 band of the brain regions that exhibited altered ALFF/fALFF was examined in the TN patients and HCs. As the left insula, putamen and left lateral temporal regions showed equal alterations in both ALFF and fALFF, we used the ALFF-altered regions as the representative seeds in the subsequent rsFC analysis. Further, we also used the PCC, left DLPFC (showing altered ALFF) and the right lateral temporal region (showing altered fALFF) as the seeds for rsFC analysis, respectively. The seed-based rsFC maps of each group are presented in Figs. 5 and 6. Visual examination indicated that both the TN patients and HCs exhibited remarkably similar rsFC patterns despite some differences in strength. Further between-group comparisons revealed weaker connectivity between the PCC and mPFC (a DMN region) in the TN patients than in the HCs. Weaker connectivity was also identified between the left DLPFC and right hippocampus (a DMN region) (Fig. 5 and Table 5). However, no significant rsFC differences were identified between the TN patients and HCs for the left insula, bilateral temporal lobe or left putamen seeds (Fig. 6). Furthermore, rsFC between the seed and each cluster was considered as individual circuits, and TN was mainly associated with abnormalities in circuits related to functional connectivity between the pain-related regions and DMN, and within DMN.
ALFF/fALFF and related rsFC differences between TN patients and healthy controls. Between-group differences in rsFC analyses were only found related to the seed of PCC and left DLPFC. (A) Seed regions for rsFC analyses. (B) Functional connectivity patterns in TN patients and healthy control subjects. Green: healthy controls; red: TN patients; yellow: overlaps. (C) Functional connectivity differences between the two groups (P < 0.05, corrected). The color bar displays t-values. Abbreviations: ALFF, amplitude of low-frequency fluctuation; DLPFC, dorsolateral prefrontal cortex; fALFF, fractional amplitude of low-frequency fluctuation; Hippo, hippocampus; mPFC, medial prefrontal cortex; PCC, posterior cingulate cortex; rsFC, resting-state functional connectivity
Related rsFC of the regions that exhibited significantly altered ALFF/fALFF. a Seed regions for rsFC analyses. b Functional connectivity patterns in TN patients and healthy control subjects (P < 0.05, corrected). Green: healthy controls; red: TN patients; yellow: overlaps. To note, no between-group differences in rsFC analyses were found related to the seed of bilateral lateral temporal regions, left insula and left pallidum. Abbreviations: ALFF, amplitude of low-frequency fluctuation; fALFF, fractional amplitude of low-frequency fluctuation; rsFC, resting-state functional connectivity
Brain-behavior relationships
Two circuits that exhibited altered slow-5 band rsFC strengths were identified from the 6 seeds of the ALFF/fALFF differences between the TN patients and HCs. The rsFC strengths of the PCC-mPFC circuit were strongly negatively correlated with pain intensity (Fig. 7). However, the pain duration and mood ratings (HAMD and HAMA scores) did not exhibit significant correlations with the rsFC strength of abnormal brain circuits. In addition, no relationship was identified between the behavioral measures and ALFF in regions that exhibited between-group differences.
Brain-Behavior Relationships. The rsFC strength of the PCC to the mPFC was negatively correlated with the pain intensity in TN patients. Arrow illustrates the rsFC between the seed and the target region but is not meant to suggest directionality. Abbreviations: FCS, functional connectivity strength; mPFC, medial prefrontal cortex; PCC, posterior cingulate cortex; VAS, visual analogue scale
Additional analyses for each factor involving frequency and group
Our main results were reproducible when we examined each factor including frequency and group. In the group of TN patients, we found that the differences of ALFF/fALFF between slow-4 and slow-5 bands (Fig.S4 and Fig.S5) were remarkably similar to that in the above-mentioned mixed effect analysis for frequency. Similar results were found in the group of HCs (Fig.S6 and Fig.S7). Furthermore, we compared the ALFF/fALFF of TN patients with HCs in slow-4 and slow-5 bands, separately. To note, we identified that the ALFF/fALFF exclusively decreased in the slow-5 band in multiple brain regions including the PCC, insula, DLPFC and lateral temporal regions (Fig.S8 and Fig.S9).
Discussion
To our knowledge, this study is the first report of frequency-dependent abnormalities in the intrinsic oscillation of the resting brain in TN patients. TN patients showed decreased ALFF/fALFF in the PCC, insula, DLPFC and lateral temporal regions, exclusively in the slow-5 frequency band (0.01–0.027 Hz). In addition, two clusters that exhibited altered ALFF/fALFF demonstrated frequency-specific alterations in rsFC. Consequently, 2 rsFC circuits, including the PCC-mPFC and DLPFC-hippocampus circuits, differed between the groups, indicating abnormal interactions within the DMN in TN patients. Strikingly, aberrations in within-network functional connectivity between PCC and mPFC in the slow-5 band tracked pain intensity. Together, our results provided empirical evidence that TN is associated with brain dysfunction with frequency-dependent functional abnormalities in neural oscillations and reorganized connectivity between the pain-related network and DMN.
Frequency-specific alterations in cortical rhythms in TN
In this study, the ALFF in TN patients decreased in distributed brain regions in the slow-5 band; however, it did not significantly change in the slow-4 band. This result reflected the existence of a selective sensitivity of specific frequency bands in detecting abnormalities in spontaneous brain activity in TN patients. Notably, abnormal BOLD signal fluctuations occur at different frequency bands that range from 0.1 Hz to 0.25 Hz for different chronic pain conditions (Alshelh et al. 2016; Baliki et al. 2011a; Malinen et al. 2010). Although the neurophysiological mechanisms that underlie the different frequency bands remain largely unclear, they may result from different neuronal origins, cytoarchitecture, or links to specific behavioral states, such as sleep, cognition, and activation (Buzsáki and Draguhn 2004; He et al. 2010). Therefore, the frequency-specific changes in BOLD signal oscillation in the TN patients may reflect changes in neural activity and may be related to distinct TN-related symptoms.
Importantly, we showed that TN patients are associated with abnormalities in spontaneous brain activity in the insula, DLPFC, lateral temporal cortex, putamen and PCC. Notably, the insula and DLPFC regions receive nociceptive input from the periphery and play seminal roles in pain processing (Apkarian et al. 2005). For example, the insula is implicated in salience, as well as pain intensity, anticipation and negative emotions, such as anxiety (Desouza et al. 2013). The DLPFC may play a central role in the experience, localization, and modulation of pain (Coghill et al. 1999; Lorenz et al. 2003); it may also modulate pain perception through a “top-down” mechanism via cortical-subcortical pathways (Lorenz et al. 2003). Although the role of the temporal cortex in pain processing is undetermined, gray matter decreases in this region are frequently identified in different pain conditions, including chronic back pain (Baliki et al. 2011b), fibromyalgia (Schmidt-Wilcke et al. 2007), migraine (Absinta et al. 2012), and TN (Li et al. 2017), which suggests the involvement of the temporal cortex in the maintenance of chronic pain. The putamen, a major site of cortical and subcortical inputs into the basal ganglia, is frequently activated during pain and is associated with pain-related motor response processing (Coghill et al. 1994; Starr et al. 2011). Given that TN patients often restrict facial movements, such as chewing, to avoid pain attack triggers (Bennetto et al. 2007), the reduced ALFF/fALFF in the putamen may partially reflect abnormal motor behaviors in TN. Consistently, several structural imaging studies have demonstrated anatomic changes in the putamen in TN patients (Desouza et al. 2013; Gustin et al. 2011). Additionally, as the PCC has been described as functional “hubs” or core regions of the DMN (Fransson and Marrelec 2008), our findings may suggest some general DMN dysfunction in TN patients. Moreover, recent studies have demonstrated that the activity of PCC is linked more to disgusting than painful aspects of stimuli (Benuzzi et al. 2008). Following this notion, our primary observation of abnormal intrinsic activity in PCC may underlie the negative emotional valence in TN patients.
Taken together, brain changes in infra-slow cortical rhythms in TN patients encompass a wide range of insular, prefrontal and subcortical regions, which are involved not only in the perception and modulation of pain but also its affective and cognitive aspects. Mechanistically, two physiological aspects are proposed to underpin the changes in infra-slow BOLD signal fluctuations in chronic pain including TN (Ploner et al. 2017). First, changes in infra-slow BOLD signal fluctuations in chronic pain may implicate a disturbance of slowly propagating waves of spontaneous neuronal activity across large-scale cortical networks (Buzsáki and Draguhn 2004; Ploner et al. 2017). As slowly propagating waves are intimately linked to slow waves during sleep and memory consolidation (Mitra et al. 2015), this disturbance of cortical rhythms may relate to abnormal learning and memory consolidation processes in chronic pain (Ploner et al. 2017). Second, infra-slow fluctuations interplay with substantially faster oscillations at alpha and gamma frequencies (Brookes et al. 2011; Mantini et al. 2007). Thus, the abnormal infra-slow fluctuations in TN patients may interfere with oscillations at higher frequencies and the flexible information flow across the brain (Ploner et al. 2017).
Abnormal functional connectivity in TN
The shift in oscillations is associated with reorganized connectivity within the resting-state networks in chronic pain. Malinen et al. (2010) identified increased spectral power at 0.12 to 0.25 Hz in the insula and ACC. Using seed-based rsFC analysis, they showed altered spatial connectivity between these two regions. Similarly, Baliki et al. (2011a) showed altered BOLD signal oscillations in the mPFC (a DMN region) in chronic back pain patients, and further correlation analysis related mPFC aberrant BOLD signal dynamics to altered rsFC in pain signaling/modulating brain regions. Both studies suggested that the changes in BOLD signal fluctuations were linked to changes in functional connectivity. Consistently, we determined that the regions (PCC and DLPFC) with abnormal BOLD signal oscillations were also associated with disrupted functional connectivity of selective regions (mPFC and hippocampus) in the DMN. These results could be attributed to the repetitive barrage of salient and pain input via peripheral nociceptive pathways that permeates the brain and consequently disturbs interactions within and between several key large-scale brain networks including the DMN.
The DMN is normally active at rest and suppressed during task or stimulus exposure, including exposure to acute pain (Fox and Raichle 2007; Seminowicz and Davis 2007). However, patients with chronic pain fail to show typical task- or pain-related DMN deactivation and exhibit disrupted DMN functional connectivity, which is related to pain intensity and rumination (Baliki et al. 2008; Kucyi et al. 2014). Moreover, abnormal within-network functional connectivity in the DMN occurs in chronic pain and tracks pain and disease-related symptoms. In the present study, we identified reorganized between- (DLPFC-hippocampus) and within-network (PCC-mPFC) functional connectivity with the DMN. Chronic pain patients often exhibit cognitive deficits with a high risk of mental disorders; thus the observed breakdown in cross-network connectivity with the DMN may be related to disrupted cognitive functions. Nevertheless, no relationship was observed between behavioral measures and the rsFC of abnormal brain circuits within the DMN. Future studies are warranted to determine the interaction between pain-related and cognition-related brain abnormalities and their relationship with behavioral deficits.
Notably, as key DMN components, both the mPFC and hippocampus exhibit lower connectivity strength with the regions with changed BOLD signal oscillations. The mPFC functionally and anatomically mediates DMN interactions with the pain modulatory system (Kucyi et al. 2014). Chronic pain patients exhibit abnormal rsFC of the mPFC that mirrors their individual degree of pain rumination (Kucyi et al. 2014). Furthermore, longitudinal studies have revealed that rsFC of the mPFC with limbic regions prospectively predicts chronification of pain (Baliki et al. 2012). Interestingly, the rsFC of the PCC-mPFC was correlated with pain intensity. In line with our results, the rsFC related to DMN tracks clinical pain intensity (Napadow et al. 2010). Our study was consistent with this convergent literature regarding mPFC/DMN abnormalities in chronic pain by demonstrating for the first time aberrant rsFC of the mPFC in TN patients and an association with pain intensity.
In addition to abnormalities in rsFC of the PCC-mPFC, we found reduced rsFC of the DLPFC with the hippocampus in TN patients compared with HCs. Chronic pain may be related to continual emotional learning coupled with an inability to extinguish aversive emotional associations (Apkarian 2008). Given the crucial role of the hippocampus in learning and memory (Barkus et al. 2010), increasing animal and human studies have conducted comprehensive examinations of hippocampal contributions to chronic pain. Rodent models of neuropathic pain exhibit robust behavioral, molecular, and synaptic deficits in the hippocampus (Mutso et al. 2012). Consistently, the hippocampal volume is reduced in humans with chronic pain (Mutso et al. 2012), and pain chronification shows changes in functional connectivity within the hippocampus as well as between the hippocampus and prefrontal cortex (Mutso et al. 2014). Thus, we assumed that the observed reorganization of the DLPFC-hippocampus appeared to underlie learning and emotional abnormalities associated with TN patients.
Limitations and future directions
Several limitations in our study are worth noting. First, the nature of these distributed frequencies of brain oscillations remains unclear. Future studies are necessary to investigate the biological and functional relevance of BOLD signal fluctuations. Moreover, we merely investigated between-group ALFF changes in the slow-4 and slow-5 infra-slow frequency bands. Further investigations exploring ALFF changes in all frequency sub-bands and their relationships with TN characteristics may provide additional insights into the neural abnormalities associated with TN patients. Second, although TN patients stopped their pain medication for at least 24 h prior to MRI scanning, the influence of pain medication on cortical rhythms cannot be completely ruled out. Moreover, without monitoring the blood concentration of drugs, we cannot rule out the possibility that some participants may fail to comply with this instruction. Future studies may take the medication condition into account and investigate whether and how it influences cortical rhythms at specific frequency bands. Third, because our main aim is to examine the oscillatory dynamics of BOLD signals and associated functional connectivity patterns in TN patients, we demonstrated the abnormal rsFC related to only the brain regions that exhibited altered ALFF/fALFF in this study. Analysis approaches that take into account all areas of the brain or all networks may also help elucidate the brain changes underlying TN. Finally, as the sample size of this study was relatively small, our analysis may have missed slight differences. Thus, the findings in the present study should be replicated in a large clinical sample in the future.
Conclusion
In summary, classic TN is accompanied by unique frequency-specific alterations in intrinsic brain oscillations involving pain-related and default-mode regions, including the insula, DLPFC, PCC and lateral temporal regions. In turn, the change in the oscillatory properties is coupled with altered functional circuits with nodes including key components of the DMN. Taken together, these results provide insights into how classic TN disrupts the cortical rhythms and cross-network interactions of the brain. Abnormalities in infra-slow fluctuations and their connectivity mirror abnormal slow wave propagation of neuronal activity and related learning processes that contribute to abnormal routing of cerebral information flow in chronic pain. These insights may have implications for the understanding and treatment of brain dysfunction in chronic pain patients, including TN patients.
References
Absinta, M., Rocca, M. A., Colombo, B., Falini, A., Comi, G., & Filippi, M. (2012). Selective decreased grey matter volume of the pain-matrix network in cluster headache. Cephalalgia : an International Journal of Headache, 32(2), 109–115.
Alshelh, Z., Di, P. F., Youssef, A. M., Reeves, J. M., Macey, P. M., Vickers, E. R., et al. (2016). Chronic neuropathic pain: It's about the rhythm. The Journal of neuroscience : the official journal of the Society for Neuroscience, 36(3), 1008–1018.
Apkarian, A. V. (2008). Pain perception in relation to emotional learning. Current Opinion in Neurobiology, 18(4), 464–468.
Apkarian, A. V., Bushnell, M. C., Treede, R. D., & Zubieta, J. K. (2005). Human brain mechanisms of pain perception and regulation in health and disease. European Journal of Pain : EJP, 9(4), 463–484.
Baliki, M. N., Geha, P. Y., Apkarian, A. V., & Chialvo, D. R. (2008). Beyond feeling: Chronic pain hurts the brain, disrupting the default-mode network dynamics. The Journal of neuroscience : the official journal of the Society for Neuroscience, 28(6), 1398–1403.
Baliki, M. N., Baria, A. T., & Apkarian, A. V. (2011a). The cortical rhythms of chronic back pain. The Journal of neuroscience : the official journal of the Society for Neuroscience, 31(39), 13981–13990.
Baliki, M. N., Schnitzer, T. J., Bauer, W. R., & Apkarian, A. V. (2011b). Brain morphological signatures for chronic pain. PLoS One, 6(10), e26010.
Baliki, M. N., Petre, B., Torbey, S., Herrmann, K. M., Huang, L., Schnitzer, T. J., et al. (2012). Corticostriatal functional connectivity predicts transition to chronic back pain. Nature Neuroscience, 15(8), 1117–1119.
Baria, A. T., Baliki, M. N., Parrish, T., & Apkarian, A. V. (2011). Anatomical and functional assemblies of brain BOLD oscillations. The Journal of neuroscience : the official journal of the Society for Neuroscience, 31(21), 7910–7919.
Barkus, C., McHugh, S. B., Sprengel, R., Seeburg, P. H., Rawlins, J. N., & Bannerman, D. M. (2010). Hippocampal NMDA receptors and anxiety: At the interface between cognition and emotion. European Journal of Pharmacology, 626(1), 49–56.
Bennetto, L., Patel, N. K., & Fuller, G. (2007). Trigeminal neuralgia and its management. BMJ : British Medical Journal, 334(7586), 201–205.
Benuzzi, F., Lui, F., Duzzi, D., Nichelli, P. F., & Porro, C. A. (2008). Does it look painful or disgusting? Ask your parietal and cingulate cortex. The Journal of neuroscience : the official journal of the Society for Neuroscience, 28(4), 923–931.
Biswal, B., Yetkin, F. Z., Haughton, V. M., & Hyde, J. S. (1995). Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magnetic Resonance in Medicine, 34(4), 537–541.
Brookes, M. J., Woolrich, M., Luckhoo, H., Price, D., Hale, J. R., Stephenson, M. C., et al. (2011). Investigating the electrophysiological basis of resting state networks using magnetoencephalography. Proceedings of the National Academy of Sciences of the United States of America, 108(40), 16783–16788.
Buzsáki, G., & Draguhn, A. (2004). Neuronal oscillations in cortical networks. Science, 304(5679), 1926–1929.
Cheng, J. C., Bosma, R. L., Hemington, K. S., Kucyi, A., Lindquist, M. A., & Davis, K. D. (2017). Slow-5 dynamic functional connectivity reflects the capacity to sustain cognitive performance during pain. NeuroImage, 15761–15768.
Coghill, R. C., Talbot, J. D., Evans, A. C., Meyer, E., Gjedde, A., Bushnell, M. C., et al. (1994). Distributed processing of pain and vibration by the human brain. The Journal of neuroscience : the official journal of the Society for Neuroscience, 14(7), 4095–4108.
Coghill, R. C., Sang, C. N., Maisog, J. M., & Iadarola, M. J. (1999). Pain intensity processing within the human brain: A bilateral, distributed mechanism. Journal of Neurophysiology, 82(4), 1934–1943.
Desouza, D. D., Moayedi, M., Chen, D. Q., Davis, K. D., & Hodaie, M. (2013). Sensorimotor and pain modulation brain abnormalities in trigeminal neuralgia: A paroxysmal, sensory-triggered neuropathic pain. PLoS One, 8(6), e66340.
DeSouza, D. D., Hodaie, M., & Davis, K. D. (2014). Abnormal trigeminal nerve microstructure and brain white matter in idiopathic trigeminal neuralgia. Pain, 155(1), 37–44.
Fox, M. D., & Raichle, M. E. (2007). Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nature reviews. Neuroscience, 8(9), 700–711.
Fransson, P., & Marrelec, G. (2008). The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: Evidence from a partial correlation network analysis. NeuroImage, 42(3), 1178–1184.
Gustin, S. M., Peck, C. C., Wilcox, S. L., Nash, P. G., Murray, G. M., & Henderson, L. A. (2011). Different pain, different brain: Thalamic anatomy in neuropathic and non-neuropathic chronic pain syndromes. The Journal of neuroscience : the official journal of the Society for Neuroscience, 31(16), 5956–5964.
He, B. J., Zempel, J. M., Snyder, A. Z., & Raichle, M. E. (2010). The temporal structures and functional significance of scale-free brain activity. Neuron, 66(3), 353–369.
Hemington, K. S., Wu, Q., Kucyi, A., Inman, R. D., & Davis, K. D. (2016). Abnormal cross-network functional connectivity in chronic pain and its association with clinical symptoms. Brain Structure & Function, 221(8), 4203–4219.
Kilpatrick, L. A., Kutch, J. J., Tillisch, K., Naliboff, B. D., Labus, J. S., Jiang, Z., et al. (2014). Alterations in resting state oscillations and connectivity in sensory and motor networks in women with interstitial cystitis/painful bladder syndrome. The Journal of Urology, 192(3), 947–955.
Kucyi, A., & Davis, K. D. (2015). The dynamic pain connectome. Trends in Neurosciences, 38(2), 86–95.
Kucyi, A., & Davis, K. D. (2016). The neural code for pain: From single-cell electrophysiology to the dynamic pain connectome. The Neuroscientist : a review journal bringing neurobiology, neurology and psychiatry, .
Kucyi, A., Moayedi, M., Weissman-Fogel, I., Goldberg, M. B., Freeman, B. V., Tenenbaum, H. C., et al. (2014). Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. The Journal of neuroscience : the official journal of the Society for Neuroscience, 34(11), 3969–3975.
Li, M., Yan, J., Li, S., Wang, T., Zhan, W., Wen, H., et al. (2017). Reduced volume of gray matter in patients with trigeminal neuralgia. Brain Imaging and Behavior, 11(2), 486–492.
Lorenz, J., Minoshima, S., & Casey, K. L. (2003). Keeping pain out of mind: The role of the dorsolateral prefrontal cortex in pain modulation. Brain: A Journal of Neurology, 126(Pt 5), 1079–1091.
Maarbjerg, S., Wolfram, F., Gozalov, A., Olesen, J., & Bendtsen, L. (2015). Significance of neurovascular contact in classical trigeminal neuralgia. Brain: A Journal of Neurology, 138(Pt 2), 311–319.
Malinen, S., Vartiainen, N., Hlushchuk, Y., Koskinen, M., Ramkumar, P., Forss, N., et al. (2010). Aberrant temporal and spatial brain activity during rest in patients with chronic pain. Proceedings of the National Academy of Sciences of the United States of America, 107(14), 6493–6497.
Mantini, D., Perrucci, M. G., Del, G. C., Romani, G. L., & Corbetta, M. (2007). Electrophysiological signatures of resting state networks in the human brain. Proceedings of the National Academy of Sciences of the United States of America, 104(32), 13170–13175.
Meskal, I., Rutten, G. J., Beute, G. N., Salden, M. E., & Sitskoorn, M. M. (2014). Cognitive deficits in patients with trigeminal neuralgia: Opportunities to improve care and quality of life. Acta Neurochirurgica, 156(8), 1565–1566.
Mitra, A., Snyder, A. Z., Tagliazucchi, E., Laufs, H., & Raichle, M. E. (2015). Propagated infra-slow intrinsic brain activity reorganizes across wake and slow wave sleep. eLife, 4.
Mutso, A. A., Radzicki, D., Baliki, M. N., Huang, L., Banisadr, G., Centeno, M. V., et al. (2012). Abnormalities in hippocampal functioning with persistent pain. The Journal of neuroscience : the official journal of the Society for Neuroscience, 32(17), 5747–5756.
Mutso, A. A., Petre, B., Huang, L., Baliki, M. N., Torbey, S., Herrmann, K. M., et al. (2014). Reorganization of hippocampal functional connectivity with transition to chronic back pain. Journal of Neurophysiology, 111(5), 1065–1076.
Napadow, V., LaCount, L., Park, K., As-Sanie, S., Clauw, D. J., & Harris, R. E. (2010). Intrinsic brain connectivity in fibromyalgia is associated with chronic pain intensity. Arthritis and Rheumatism, 62(8), 2545–2555.
Nurmikko, T. J., & Eldridge, P. R. (2001). Trigeminal neuralgia--pathophysiology, diagnosis and current treatment. British Journal of Anaesthesia, 87(1), 117–132.
Obermann, M., Rodriguez-Raecke, R., Naegel, S., Holle, D., Mueller, D., Yoon, M. S., et al. (2013). Gray matter volume reduction reflects chronic pain in trigeminal neuralgia. NeuroImage, 74352–74358.
Ploner, M., Sorg, C., & Gross, J. (2017). Brain rhythms of pain. Trends in Cognitive Sciences, 21(2), 100–110.
Rogachov, A., Cheng, J. C., Erpelding, N., Hemington, K. S., Crawley, A. P., & Davis, K. D. (2016). Regional brain signal variability: A novel indicator of pain sensitivity and coping. Pain, 157(11), 2483–2492.
Sarnthein, J., Stern, J., Aufenberg, C., Rousson, V., & Jeanmonod, D. (2006). Increased EEG power and slowed dominant frequency in patients with neurogenic pain. Brain: A Journal of Neurology, 129(Pt 1), 55–64.
Schmidt-Wilcke, T., Luerding, R., Weigand, T., Jürgens, T., Schuierer, G., Leinisch, E., et al. (2007). Striatal grey matter increase in patients suffering from fibromyalgia--a voxel-based morphometry study. Pain, 132(Suppl 1), S109–S116.
Seminowicz, D. A., & Davis, K. D. (2007). Pain enhances functional connectivity of a brain network evoked by performance of a cognitive task. Journal of Neurophysiology, 97(5), 3651–3659.
Starr, C. J., Sawaki, L., Wittenberg, G. F., Burdette, J. H., Oshiro, Y., Quevedo, A. S., et al. (2011). The contribution of the putamen to sensory aspects of pain: Insights from structural connectivity and brain lesions. Brain: A Journal of Neurology, 134(Pt 7), 1987–2004.
Stern, J., Jeanmonod, D., & Sarnthein, J. (2006). Persistent EEG overactivation in the cortical pain matrix of neurogenic pain patients. NeuroImage, 31(2), 721–731.
Wang, Y., Cao, D. Y., Remeniuk, B., Krimmel, S., Seminowicz, D. A., & Zhang, M. (2017). Altered brain structure and function associated with sensory and affective components of classic trigeminal neuralgia. Pain, 158(8), 1561–1570.
Williams, J. B. (1988). A structured interview guide for the Hamilton depression rating scale. Archives of General Psychiatry, 45(8), 742–747.
Wu, T. H., Hu, L. Y., Lu, T., Chen, P. M., Chen, H. J., Shen, C. C., et al. (2015). Risk of psychiatric disorders following trigeminal neuralgia: a nationwide population-based retrospective cohort study. The journal of headache and pain, 1664.
Yan, C. G., Wang, X. D., Zuo, X. N., & Zang, Y. F. (2016). DPABI: Data Processing & Analysis for (resting-state) brain imaging. Neuroinformatics, 14(3), 339–351.
Zang, Y. F., He, Y., Zhu, C. Z., Cao, Q. J., Sui, M. Q., Liang, M., et al. (2007). Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain & Development, 29(2), 83–91.
Zhang, Y., Zhu, C., Chen, H., Duan, X., Lu, F., Li, M., et al. (2015). Frequency-dependent alterations in the amplitude of low-frequency fluctuations in social anxiety disorder. Journal of Affective Disorders, 174329–174335.
Zhou, F., Huang, S., Zhuang, Y., Gao, L., & Gong, H. (2017). Frequency-dependent changes in local intrinsic oscillations in chronic primary insomnia: A study of the amplitude of low-frequency fluctuations in the resting state. NeuroImage. Clinical, 15458–15465.
Zou, Q. H., Zhu, C. Z., Yang, Y., Zuo, X. N., Long, X. Y., Cao, Q. J., et al. (2008). An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: Fractional ALFF. Journal of Neuroscience Methods, 172(1), 137–141.
Zuo, X. N., Di, M. A., Kelly, C., Shehzad, Z. E., Gee, D. G., Klein, D. F., et al. (2010). The oscillating brain: Complex and reliable. NeuroImage, 49(2), 1432–1445.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, Y., Mao, Z., Pan, L. et al. Frequency-specific alterations in cortical rhythms and functional connectivity in trigeminal neuralgia. Brain Imaging and Behavior 13, 1497–1509 (2019). https://doi.org/10.1007/s11682-019-00105-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-019-00105-8