Abstract
Premenstrual syndrome (PMS) is a menstrual cycle-related disorder. Although the precise pathophysiology is not fully understood, it is increasingly believed that the central nervous system plays a vital role in the development of PMS. The aim of this study is to elucidate specific functional connectivity between the thalamus and cerebral cortex. Resting-state functional magnetic resonance imaging (fMRI) data were obtained from 20 PMS patients and 21 healthy controls (HCs). Seed-based functional connectivity between the thalamus and six cortical regions of interest, including the prefrontal cortex (PFC), posterior parietal cortex, somatosensory cortex, motor cortex/supplementary motor area, temporal and occipital lobe, was adopted to identify specific thalamocortical connectivity in the two groups. Correlation analysis was then used to examine relationships between the neuroimaging findings and clinical symptoms. Activity in distinct cortical regions correlated with specific sub-regions of the thalamus in the two groups. Comparison between groups exhibited decreased prefrontal-thalamic connectivity and increased posterior parietal–thalamic connectivity in the PMS patients. Within the PMS group, the daily record of severity of problems (DRSP) score negatively correlated with the prefrontal-thalamic connectivity. Our findings may provide preliminary evidence for abnormal thalamocortical connectivity in PMS patients and may contribute to a better understanding of the pathophysiology of PMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thalamus is a critical subcortical structure that plays a pivotal role in information transmission and processing in human brain, which is generally believed to act as a ‘relay station’ or ‘gateway’ that connects with distinct zones of the cerebral cortex (Saalmann 2014; Sherman 2001). Patients with local thalamus lesions could have abnormalities of emotion processing, multimodal cognition, perception and motivation, such as schizophrenia, Alzheimer’s disease, autism spectrum disorder and major depression (Byne et al. 2002; Skåtun et al. 2017; Zarei et al. 2010; Nair et al. 2013; Tadayonnejad et al. 2016; Greicius et al. 2007). The functional organization of thalamus comprises multiple parallel loops with dense reciprocal connections to nearly all regions of the cerebral cortex. In other words, the thalamocortical networks are topographically organized into multiple parallel loops linking distinct zones of cerebral cortex to specific thalamus nuclei (Haber 2003), which is considered to underlie basic alertness, sensory, motor information processing, and attention processes. Considerable evidence has also demonstrated the close relationship between neuropsychiatric disorders and aberrant thalamocortical connectivity (Woodward et al. 2012; Zhang et al. 2008, 2010).
Premenstrual syndrome (PMS) is defined as moderate-to-severe emotional, cognitive, physical and behavioral symptoms that cyclically occur during the luteal phase and resolve shortly after the onset of menstruation (Halbreich et al. 2007). It is estimated that 30–40% of reproductive women suffer from PMS (Ryu and Kim 2015). And women with PMS have higher rate of medical expenses, higher work absence and lower occupational productivity, which significantly disturb the quality life of a subset of women (Jr 2005). However, the pathophysiology of PMS is not fully understood. To date, the abnormal central nervous system (CNS) processing may be involved in PMS. Accumulating functional magnetic resonance imaging (fMRI) studies have revealed that PMS patients have dysfunctions of several brain regions, mainly including the frontal cortex, precentral gyrus, anterior cingulated cortex, temporal cortex and precuneus (Liao et al. 2017a, b; Liu et al. 2015; Duan et al. 2018; Bondt et al. 2015). For instance, Liu and his colleagues found that PMS patients had decreased functional connectivity in the middle frontal cortex and parahippocampus, as well as increased connectivity in the temporal cortex and precentral gyrus (Liu et al. 2015). Our team also found that PMS patients had abnormal regional homogeneity (ReHo) and fractional amplitude of low-frequency fluctuation (fALFF) in the prefrontal cortex (PFC) and temporal cortex at the late luteal phase (Liao et al. 2017a, b; Duan et al. 2018). Pathogenetic theories posit that a disorder of neurosteroid metabolism or action results in a luteal phase deficit in γ-aminobutyric acid (GABA)-mediated inhibition in PMS (Smith et al. 2003). The inhibitory GABA neurons of thalamus are associated with the generation of normal and abnormal synchronized activity in the thalamocortical networks (Kim et al. 1997). Recently, our voxel-based morphometry (VBM) study reported that PMS patients had morphological change of thalamus and abnormal thalamic-prefrontal structural covariance pattern by structural MRI (Liu et al. 2018). In view of these existent findings and the fundamental importance of thalamocortical networks, it raises an interesting question: whether there exists abnormal functional connectivity between different cortical areas and specific thalamic nuclei in PMS patients, which may account for the clinical symptoms of PMS. Determining the specificity of thalamocortical networks abnormalities could be valuable for our understanding of PMS. However, to our best knowledge, few studies have explored thalamocortical dysconnectivity in PMS patients.
The focus of this study was to map intrinsic connectivity between the specific thalamus and distinct zones of cerebral cortex, and to explore potential relationships between the neuroimaging findings and clinical characteristics of PMS. Functional connectivity method based on resting-state fMRI is considered to be an ideal method for examining the integrity of thalamocortical connectivity (Zhang et al. 2008). Thus, we used this method to elucidate PMS-related alterations of thalamocortical connectivity in this study. Here, we hypothesized that 1) patients and healthy control (HC) group would exhibit specific thalamocortical functional connectivity, respectively; 2) PMS patients may have thalamocortical dysconnectivity, particularly implicated in emotion, cognition or attention processing; and 3) the neuroimaging findings would be associated with several clinical characteristics.
Methods
Experimental paradigm
To exclude organic diseases and verify menstrual cycle stage, gynecological examination and B-ultrasonic wave were adopted for each participant before the study. Based on the participants' physical characteristics and hormone level, all the participants were arranged to undergo MRI scanning in the late-luteal phase, ranging from 1 to 5 days before menstruation. To obtain a low level and relatively stable of endogenous estradiol and cortisol (Bao et al. 2004), all MRI scanning were carried out between 8:00 p.m. and 10:00 p.m.
Participants
Twenty-three PMS patients and twenty-two HCs were recruited through advertisement in the Guangxi University of Chinese Medicine. Each participant was individually diagnosed by a gynecologist with 10 years of experience. The recruitment criteria and evaluation of PMS patients were based on the recommendations and guidelines described by Halbreich et al. (2007). The inclusion criteria for recruitment of patients were as follows: 1) aging from 18 to 45 years old; 2) being right-handed; 3) having regular menstrual cycles ranging from 24 to 35 days; 4) the premenstrual symptoms occurred up to 2 weeks before menses in most menstrual cycles; 5) the symptoms alleviated shortly following menses and were absent during most of the mid-follicular phase of the menstrual cycle; 6) the menstrual-associated periodicity, occurrence during the late luteal phase of cycle (days −5 to −1) and absence during the mid-follicular phase (days +6 to +10) were documented by repeated observations by the PMS patients basing on daily record of severity of problems (DRSP) criterion, and the mean score in the luteal phase was at least 30% greater than the follicular phase; 7) the symptoms were not just a worsening of another physical chronic or mental disorders; and 8) the symptoms were related to impairment in daily functioning and/or relationships and/or caused suffering, behavioral, physical and emotional distress. The inclusion criteria for HCs were similar to those for PMS patients except the premenstrual symptoms. The exclusion criteria for all participants were: 1) being currently pregnant or lactating; 2) having a history of dysmenorrhea, gynecological inflammation, menopausal syndrome, thyroid disease, bilateral oophorectomy or hysterectomy, mastopathy or cancer, or any other structural diseases; 3) having obviously psychiatric disorders diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) (American Psychiatric Association 2013), such as delusional mental disorder, schizophrenia, schizoaffective disorder, organic mental disorder, psychotic features coordinated or uncoordinated with mood or bipolar disorder; 4) treating with any benzodiazepines, steroid compound (e.g., hormonal intrauterine devices and oral contraceptives) or other psychoactive drugs that affecting PMS; 5) having any contraindication of MRI scanning; and 6) being alcohol abuse or smoker.
Questionnaires
To quantify the premenstrual symptoms, eligible participants were asked to document their daily symptoms for 2 months using the DRSP questionnaire (Endicott et al. 2006), and required to finish an assessment of body mass index (BMI), menophania (years), length of menstrual cycle (days) and menstruation (days). And Hamilton anxiety scale (HAMA) and Hamilton depression scale (HAMD) were also used to quantify each participant’s anxiety and depression level before MRI scanning.
Imaging data acquisition
Imaging data were acquired on a 3.0 T Siemens Magnetom Verio MRI System (Siemens Medical, Erlangen, Germany), using an 8-channel head coil. Head movement was minimized with foam pillows around participants’ head. Resting-state fMRI data were obtained with a single-shot gradient-recalled echo planar imaging (EPI) sequence using the following settings: repetition time (TR) = 2000 ms; echo time (TE) = 30 ms; flip angle = 90°; field of view (FOV) = 240 mm; The slice thickness was 5 mm (no-gap) with a matrix size of 64 × 64. Each resting-state fMRI brain volume comprised 31 slices, and each functional run contained 180 image volumes. The total scanning time approximately 6 min. High-resolution T1-weighted anatomical images were then obtained using a three-dimensional fast spoiled gradient recall sequence with the parameters as following: TR = 1900 ms; TE = 2.22 ms; flip angle = 9°; FOV = 250 mm; 250 × 250 matrix; slice thickness = 1 mm and slices = 176. During the scanning, each participant was required to keep eyes closed, to stay awake and think of nothing systematically. After scanning, each participant was asked whether she was awaking.
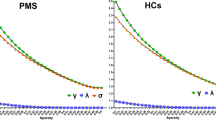
Imaging data preprocessing
The fMRI data were preprocessed and analyzed in DPABI toolbox (V2.3, http://rfmri.org/dpabi), based on Statistical Parametric Mapping 12 (SPM12, http://www.fil.ion.ucl.ac.uk/spm/software/spm12/) on MATLAB platform. The details of processing methods have been described in prior publications (Yan et al. 2016; Chao-Gan and Yu-Feng 2010). Briefly, after converting DICOM files to NIFTI images, the first five time points were discarded from each run to remove effects of signal instability, and slice-time correction was employed to correct for acquisition delays within functional volumes. Next, realignment through rigid body transformation to correct for head motion. Functional MRI data with maximum displacement in any cardinal direction >2 mm or head rotation >2o were discarded from further analysis. The corrected images were then spatially normalized to the Montreal Neurological Institute (MNI) space by using EPI template (Calhoun et al. 2017), resampled to isotropic 3 mm3 voxel size, and spatially smoothed to a Gaussian kernel of full-width at half maximum of 4 mm. 24 head motion parameters (6 head motion parameters, 6 head motion parameters first derivatives, and their corresponding squared items), cerebral spinal fluid signal (CSF), and white matter (WM) signal were modelled as nuisance variables and removed with regression. After the linear trend of time courses removal, band-pass filter (0.01 < f < 0.1 Hz) was applied to remove the influences of low-frequency drift and physiological high-frequency noise.
Functional connectivity analysis
Largely consistent with the approach carried by Woodward et al. (2012), the cerebral cortex was partitioned into six disjoint regions of interest (ROIs). These cortical ROIs were defined as 1) the prefrontal cortex consisting of the superior, middle, and inferior frontal gyri, middle and lateral orbitofrontal gyri, anterior cingulate gyrus and gyrus rectus; 2) the posterior parietal cortex (PPC) encompassing the superior parietal, supramarginal gyrus, angular gyrus, precuneus and posterior cingulate; 3) the somatosensory cortex involving the postcentral gyrus; 4) the temporal lobe including the superior, middle, and inferior temporal gyri, the fusiform gyrus and parahippocampal gyrus; 5) the motor cortex/supplementary motor area containing the precentral gyrus and the supplementary motor area; and 6) the occipital lobe embracing the superior, middle, and inferior occipital gyri, cuneus and lingual gyrus. The cortical ROIs were masked using the Laboratory of Neuroimaging (LONI) probabilistic atlas gray matter tissue map, excluding voxels below a threshold of 0.15 (Failla et al. 2017; Woodward et al. 2012).
To investigate the specific functional connectivity between the cortex and thalamus, the six ROIs defined above were used as seed-to-voxel functional connectivity analysis. Briefly, the mean time series from each seed (ROI) was extracted separately as a reference time course, and voxel-based general linear modeling (GLM) was then employed to quantify the relationship between the seed and the thalamus. Subsequently, Fisher’s r-to-z transformation was performed to normalize the resulting r values into z values.
Statistical analysis
The demographic and clinical characteristics of the PMS patients and HCs were examined by SPSS 22.0 (IBM, Armonk, New York). The two-sample t-test was adopted for variables and the threshold was set at a significance level of p < 0.05.
To delineate the statistical parametric maps between the thalamus and cortical ROIs, one-sample and two-sample t-test were adopted to examine only positive functional connectivity maps (Woodward et al. 2012; Nair et al. 2013) in the PMS patients and HCs at a threshold of p < 0.05 (family-wise error (FWE) corrected) within the template of the Oxford Thalamic Connectivity Probability Atlas.
Within the PMS group, we performed a Pearson’s correlation to examine the potential relationship between the clinical symptoms (e.g., HAMA, HAMD and DRSP) and thalamocortical connectivity showing group differences. The significant level was set at p < 0.05 with the Bonferroni correction.
Results
Demographic characteristics
For significant head movement, three PMS patients and one HC were excluded. Finally, 20 PMS patients and 21 HCs were included in this study. Demographic characteristics of PMS patients and HCs are summarized in Table 1. The HAMD score of PMS group was higher than that of healthy group (PMS: mean = 13.10, standard deviation (SD) = 6.54; healthy control: mean = 8.29, SD = 3.95; p < 0.05). And the DRSP score in the late luteal phase from PMS patients was significantly higher than that from HCs (PMS: mean = 73.47, SD = 7.84; healthy control: mean = 35.17, SD = 7.90; p < 0.001). No significant difference in terms of other demographic and clinical analyses was found (p > 0.05). Besides, during the late luteal phase, the mean DRSP score of all PMS patients exceeded 50. And PMS group averaged 46.24% (SD = 7.06%) increase in the symptom severity during the late luteal phase of their cycles compared with the mid-follicular phase (Table 2).
Thalamocortical connectivity
Correlation maps between the cortical ROIs and thalamus for healthy controls were largely consistent with previous studies (Woodward et al. 2012; Zhang et al. 2010). Figure 1a exhibits that each cortical region was correlated with distinct, spatially restricted regions within the thalamus. Specifically, the PFC was correlated strongly with the anterior and dorsomedial regions of the thalamus; The PPC was functionally connected to lateral posterior portions and pulvinar; The somatosensory cortex correlated with the ventral posterior-lateral nucleus of the thalamus; The temporal and occipital lobe were functionally connected to the posterior medial and lateral regions of the thalamus, respectively; The motor cortex/supplementary motor area correlated with the ventral lateral portions of thalamus. PMS patients also exhibited a high degree of segregation in the thalamus. The functional connectivity maps of PMS patients were similar to the ones of HCs.
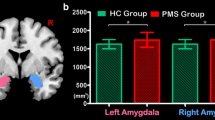
Functional connectivity between the cerebral cortex and thalamus. a Each cortical region was specifically correlated with distinct regions of the thalamus in both PMS patients and HCs. b Comparison between groups demonstrated decreased prefrontal connectivity with the thalamus and increased connectivity between the posterior parietal cortex and thalamus in PMS patients
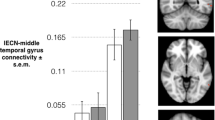
The results of group differences in thalamocortical connectivity are shown in Fig. 1b. Compared to HCs, the PMS patients had significantly decreased connectivity between the PFC and right dorsomedial thalamus, and increased connectivity between the PPC and the lateral posterior nucleus. Furthermore, we detected that the connectivity of prefrontal-thalamus negatively correlated with DRSP score (r = −0.59, p = 0.006) in the PMS patients. No other correlation between the connectivity changes and clinical symptoms, including HAMA and HAMD, were found in PMS patients (p > 0.05) (Fig. 2).
Discussion
In the current study, the resting-state fMRI was used to identify the specific of thalamocortical network dysconnectivity in PMS patients. We found that 1) compared to HCs, PMS patients had decreased functional connectivity between the PFC and dorsomedial thalamus as well as increased functional connectivity between the PPC and lateral posterior thalamus; and 2) the connectivity of prefrontal-thalamus negatively correlated with DRSP score in PMS patients.
One of compelling findings of this study was that the thalamic functional connectivity with the PFC was decreased in PMS patients. The PFC is a collection of interconnected neocortical regions that has access to diverse information about both the external state of the world and the internal state of the system of cognitive control (Ridderinkhof et al. 2004). Among the emotion-related brain systems, PFC has widely been considered to be primarily implicated in elaborating upon and regulating the more basic emotional processes occurring in subcortical regions (Dixon et al. 2017). Nearly most of studies of affective disorders are associated with prefrontal dysfunction, including bipolar disorder, depression and anxiety (Frye et al. 2007; Goldin et al. 2009; Bishop et al. 2004; Davidson 2002). And altered functional connectivity between the PFC and dorsomedial regions of thalamus have been reported in schizophrenia (Woodward et al. 2012). Thereby, our finding may suggest that the aberrant circuit involving the PFC and thalamus may contribute to the functional neuroanatomy of PMS. In addition, the DRSP score was used to estimate the severity levels of PMS. The DRSP is recognized as an easily accessible, well-validated prospective rating scale that can be used for prospective assessment of symptoms and impairment at various phases of menstrual cycle, and it has been used to aid in the diagnosis and evaluation of PMS in clinical (Ryu and Kim 2015; Endicott et al. 2006; Nevatte et al. 2013). In the present study, the DRSP score of PMS patients was significantly higher than that of HCs, suggesting that PMS patients have higher level of severity symptoms or experience behavioral and functional impairment. Moreover, the DRSP score significantly negatively correlated with prefrontal-thalamus connectivity in PMS group. Hence, we infer that the more decreased thalamic functional connectivity with the PFC follows the worse severity of PMS, which would be one of the crucial underpinnings of PMS.
In the current study, PMS patients also exhibited significantly increased functional connectivity between the PPC and thalamus. The PPC serves as an interface between sensory and motor cortices and plays a pivotal role in sensorimotor transformations, perceptual attention and episodic memory retrieval (Sestieri et al. 2010, 2017). And the PPC is enrolled in orienting attention to important information in the environment on the basis of internal goals and the sensory distinctiveness and adaptive value of stimuli (Corbetta and Shulman 2002). For example, the functional/structural changes of PPC and thalamus suggested abnormal attention and emotion modulation arising from the viscera in irritable bowel syndrome patients (Seminowicz et al. 2010; Fadgyasstanculete et al. 2014; Wang et al. 2017). Greene et al. (2014) found that the distinct sites of PPC were functionally connected with mood, arousal and the interaction during recognition memory. Hence, it is plausible to speculate that, with increased thalamic connectivity with PPC, PMS patients may be more sensitive to emotional arousal and perception of visceral sensations, which could induce memory consolidation for unpleasant condition. Further studies on this issue could be needed in future.
Limitations
There are several limitations of our investigation that merit consideration. Firstly, our present study was limited by the relatively small sample size, which could affect the statistical power and results. Future studies should be reassessed based on a larger clinical and imaging dataset. Secondly, only young PMS patients were enrolled in this study, which may limit the generalizability of the findings. Therefore, future study should recruit a greater age range of participants. Finally, although we employed a well-established method to investigate thalamocortical functional connectivity, there are nonetheless limitations of the large cortical seeds. Future study with smaller functional regions will be used to explore the specificity of connections between more narrowly specialized regions (e.g. middle orbitofrontal cortex or angular gyrus) and thalamus.
Conclusions
To summarize, we observed altered functional connectivity between the thalamus and cerebral cortex in PMS. The alterations are characterized by decreased thalamic connectivity with PFC, and increased thalamic connectivity with PPC. The altered functional connectivity may partially disturb processing of emotion and/or attention, and may enhance unpleasant perception of visceral sensations in PMS patients. Furthermore, the prefrontal-thalamic connectivity might be a pivotal circuit to the underpinning of PMS because of the significant correlation between this imaging finding and DRSP score. We hope that the current preliminary evidence for abnormal thalamocortical connectivity may contribute to improving our understanding of the pathophysiology of PMS.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Washington, DC: American Psychiatric Press.
Bao, A. M., Ji, Y. F., Van Someren, E. J., Hofman, M. A., Liu, R. Y., & Zhou, J. N. (2004). Diurnal rhythms of free estradiol and cortisol during the normal menstrual cycle in women with major depression. Hormones and Behavior, 45(2), 93–102.
Bishop, S., Duncan, J., Brett, M., & Lawrence, A. D. (2004). Prefrontal cortical function and anxiety: controlling attention to threat-related stimuli. Nature Neuroscience, 7(2), 184–188.
Bondt, T. D., Smeets, D., Pullens, P., Hecke, W. V., Jacquemyn, Y., & Parizel, P. M. (2015). Stability of resting state networks in the female brain during hormonal changes and their relation to premenstrual symptoms. Brain Research, 1624, 275–285.
Byne, W., Buchsbaum, M. S., Mattiace, L. A., Hazlett, E. A., Kemether, E., Elhakem, S. L., Purohit, D. P., Haroutunian, V., & Jones, L. (2002). Postmortem assessment of thalamic nuclear volumes in subjects with schizophrenia. American Journal of Psychiatry, 159(1), 59–65.
Calhoun, V. D., Wager, T. D., Krishnan, A., Rosch, K. S., Seymour, K. E., Nebel, M. B., Mostofsky, S. H., Nyalakanai, P., & Kiehl, K. (2017). The impact of T1 versus EPI spatial normalization templates for fMRI data analyses. Human Brain Mapping, 38(11), 5331–5342.
Chao-Gan, Y., & Yu-Feng, Z. (2010). DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Frontiers in Systems Neuroscience, 4, 13. https://doi.org/10.3389/fnsys.2010.00013.
Corbetta, M., & Shulman, G. L. (2002). Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews Neuroscience, 3(3), 201–215.
Davidson, R. J. (2002). Anxiety and affective style: role of prefrontal cortex and amygdala. Biological Psychiatry, 51(1), 68–80.
Dixon, M. L., Thiruchselvam, R., Todd, R., & Christoff, K. (2017). Emotion and the prefrontal cortex: an integrative review. Psychological Bulletin, 143(10), 1033–1081.
Duan, G., Liu, H., Pang, Y., Liu, P., Liu, Y., Wang, G., Liao, H., Tang, L., Chen, W., Mo, X., Wen, D., Lin, H., & Deng, D. (2018). Hippocampal fractional amplitude of low-frequency fluctuation and functional connectivity changes in premenstrual syndrome. Journal of Magnetic Resonance Imaging, 47(2), 545–553.
Endicott, J., Nee, J., & Harrison, W. (2006). Daily record of severity of problems (DRSP): reliability and validity. Archives of Women’s Mental Health, 9(1), 41–49.
Fadgyasstanculete, M., Buga, A. M., Popawagner, A., & Dumitrascu, D. L. (2014). The relationship between irritable bowel syndrome and psychiatric disorders: from molecular changes to clinical manifestations. Journal of Molecular Psychiatry, 2(1), 4.
Failla, M. D., Peters, B. R., Karbasforoushan, H., Foss-Feig, J. H., Schauder, K. B., Heflin, B. H., & Cascio, C. J. (2017). Intrainsular connectivity and somatosensory responsiveness in young children with ASD. Molecular Autism, 8(1), 25.
Frye, M. A., Watzl, J., Banakar, S., O'Neill, J., Mintz, J., Davanzo, P., Fischer, J., Chirichigno, J. W., Ventura, J., Elman, S., Tsuang, J., Walot, I., & Thomas, M. A. (2007). Increased anterior cingulate/medial prefrontal cortical glutamate and creatine in bipolar depression. Neuropsychopharmacology, 32(12), 2490–2499.
Goldin, P. R., Manber, T., Hakimi, S., Canli, T., & Gross, J. J. (2009). Neural bases of social anxiety disorder: emotional reactivity and cognitive regulation during social and physical threat. Archives of General Psychiatry, 66(2), 170–180. https://doi.org/10.1001/archgenpsychiatry.2008.525.
Greene, C. M., Flannery, O., & Soto, D. (2014). Distinct parietal sites mediate the influences of mood, arousal, and their interaction on human recognition memory. Cognitive, Affective, & Behavioral Neuroscience, 14(4), 1327–1339.
Greicius, M. D., Flores, B. H., Menon, V., Glover, G. H., Solvason, H. B., Kenna, H., Reiss, A. L., & Schatzberg, A. F. (2007). Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biological Psychiatry, 62(5), 429–437.
Haber, S. N. (2003). The primate basal ganglia: parallel and integrative networks. Journal of Chemical Neuroanatomy, 26(4), 317–330.
Halbreich, U., Backstrom, T., Eriksson, E., O’Brien, S., Calil, H., Ceskova, E., et al. (2007). Clinical diagnostic criteria for premenstrual syndrome and guidelines for their quantification for research studies. Gynecological Endocrinology, 23(3), 123–130.
Jr, M. D. (2005). Premenstrual disorders: epidemiology and disease burden. The American Journal of Managed Care, 11(16 Suppl), 473–479.
Kim, U., Sanchez-Vives, M. V., & Mccormick, D. A. (1997). Functional dynamics of GABAergic inhibition in the thalamus. Science, 278(5335), 130–134.
Liao, H., Duan, G., Liu, P., Liu, Y., Pang, Y., Liu, H., Tang, L., Tao, J., Wen, D., Li, S., Liang, L., & Deng, D. (2017a). Altered fractional amplitude of low frequency fluctuation in premenstrual syndrome: a resting state fMRI study. Journal of Affective Disorders, 218, 41–48.
Liao, H., Pang, Y., Liu, P., Liu, H., Duan, G., Liu, Y., et al. (2017b). Abnormal spontaneous brain activity in women with premenstrual syndrome revealed by regional homogeneity. Frontiers in Human Neuroscience, 11, 62.
Liu, Q., Li, R., Zhou, R., Li, J., & Gu, Q. (2015). Abnormal resting-state connectivity at functional MRI in women with premenstrual syndrome. PLoS One, 10(9), e0136029.
Liu, P., Wei, Y., Fan, Y., Li, R., Liu, Y., Wang, G., Wei, Y., Pang, Y., Deng, D., & Qin, W. (2018). Altered brain structure in women with premenstrual syndrome. Journal of Affective Disorders, 229, 239–246. https://doi.org/10.1016/j.jad.2017.12.075.
Nair, A., Treiber, J. M., Shukla, D. K., Shih, P., & Müller, R. A. (2013). Impaired thalamocortical connectivity in autism spectrum disorder: a study of functional and anatomical connectivity. Brain, 136(6), 1942–1955.
Nevatte, T., O’Brien, P. M. S., Bäckström, T., Brown, C., Dennerstein, L., Endicott, J., et al. (2013). ISPMD consensus on the management of premenstrual disorders. Archives of Women’s Mental Health, 16(4), 279–291.
Ridderinkhof, K. R., Ullsperger, M., Crone, E. A., & Nieuwenhuis, S. (2004). The role of the medial frontal cortex in cognitive control. Science, 306(5695), 443–447.
Ryu, A., & Kim, T. H. (2015). Premenstrual syndrome: a mini review. Maturitas, 82(4), 436–440. https://doi.org/10.1016/j.maturitas.2015.08.010.
Saalmann, Y. B. (2014). Intralaminar and medial thalamic influence on cortical synchrony, information transmission and cognition. Frontiers in Systems Neuroscience, 8(83), 83.
Seminowicz, D. A., Labus, J. S., Bueller, J. A., Tillisch, K., Naliboff, B. D., Bushnell, M. C., et al. (2010). Regional gray matter density changes in brains of patients with irritable bowel syndrome. Gastroenterology, 139(1), 48–57 e42. https://doi.org/10.1053/j.gastro.2010.03.049.
Sestieri, C., Shulman, G. L., & Corbetta, M. (2010). Attention to memory and the environment: functional specialization and dynamic competition in human posterior parietal cortex. Journal of Neuroscience, 30(25), 8445–8456.
Sestieri, C., Shulman, G. L., & Corbetta, M. (2017). The contribution of the human posterior parietal cortex to episodic memory. Nature Reviews. Neuroscience, 18(3), 183–192. https://doi.org/10.1038/nrn.2017.6.
Sherman, S. M. (2001). Exploring the thalamus. Elsevier.
Skåtun, K. C., Kaufmann, T., Brandt, C. L., Doan, N. T., Alnæs, D., Tønnesen, S., et al. (2017). Thalamo-cortical functional connectivity in schizophrenia and bipolar disorder. Brain Imaging and Behavior, 1–13.
Smith, M. J., Adams, L. F., Schmidt, P. J., Rubinow, D. R., & Wassermann, E. M. (2003). Abnormal luteal phase excitability of the motor cortex in women with premenstrual syndrome. Biological Psychiatry, 54(7), 757–762.
Tadayonnejad, R., Ajilore, O., Mickey, B. J., Crane, N. A., Hsu, D. T., Kumar, A., Zubieta, J. K., & Langenecker, S. A. (2016). Pharmacological modulation of pulvinar resting-state regional oscillations and network dynamics in major depression. Psychiatry Research, 252, 10–18.
Wang, D., Zhang, X., Zhang, X., Huang, Z., & Song, Y. (2017). Magnetic resonance imaging analysis of brain function in patients with irritable bowel syndrome. BMC Gastroenterology, 17(1), 148. https://doi.org/10.1186/s12876-017-0673-y.
Woodward, N. D., Karbasforoushan, H., & Heckers, S. (2012). Thalamocortical dysconnectivity in schizophrenia. American Journal of Psychiatry, 169(10), 1092–1099.
Yan, C. G., Wang, X. D., Zuo, X. N., & Zang, Y. F. (2016). DPABI: data processing & analysis for (resting-state) brain imaging. Neuroinformatics, 14(3), 339–351. https://doi.org/10.1007/s12021-016-9299-4.
Zarei, M., Patenaude, B., Damoiseaux, J., Morgese, C., Smith, S., Matthews, P. M., Barkhof, F., Rombouts, S., Sanz-Arigita, E., & Jenkinson, M. (2010). Combining shape and connectivity analysis: an MRI study of thalamic degeneration in Alzheimer's disease. NeuroImage, 49(1), 1–8.
Zhang, D., Snyder, A. Z., Fox, M. D., Sansbury, M. W., Shimony, J. S., & Raichle, M. E. (2008). Intrinsic functional relations between human cerebral cortex and thalamus. Journal of Neurophysiology, 100(4), 1740–1748.
Zhang, D., Snyder, A. Z., Shimony, J. S., Fox, M. D., & Raichle, M. E. (2010). Noninvasive functional and structural connectivity mapping of the human thalamocortical system. Cerebral Cortex, 20(5), 1187–1194.
Funding
This work was supported by the National Natural Science Foundation of China under Grant Nos. 81771918, 81471738, 81471811 and 81760886; National Basic Research Program of China under Grant Nos. 2014CB543203 and 2015CB856403; Guangxi Natural Science Foundation under Grant Nos. 2016GXNSFAA380006 and 2017GXNSFBA198095; Natural Science Basic Research Plan in Shaanxi Province of China under Grant No. 2017JM6051; and the Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Ethical approval
The experiment procedures were approved by the Medicine Ethics Committee of First Affiliated Hospital, Guangxi University of Chinese Medicine, Guangxi, China. Each research procedure of this study was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent after receiving an explanation of the whole study.
Rights and permissions
About this article
Cite this article
Liu, P., Wei, Y., Liao, H. et al. Thalamocortical dysconnectivity in premenstrual syndrome. Brain Imaging and Behavior 13, 717–724 (2019). https://doi.org/10.1007/s11682-018-9894-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-018-9894-0