Abstract
Mild traumatic brain injuries (mTBIs) are often associated with posttraumatic stress disorder (PTSD). In cases of chronic mTBI, accurate diagnosis can be challenging due to the overlapping symptoms this condition shares with PTSD. Furthermore, mTBIs are heterogeneous and not easily observed using conventional neuroimaging tools, despite the fact that diffuse axonal injuries are the most common injury. Diffusion tensor imaging (DTI) is sensitive to diffuse axonal injuries and is thus more likely to detect mTBIs, especially when analyses account for the inter-individual variability of these injuries. Using a subject-specific approach, we compared fractional anisotropy (FA) abnormalities between groups with a history of mTBI (n = 35), comorbid mTBI and PTSD (mTBI + PTSD; n = 22), and healthy controls (n = 37). We compared all three groups on the number of abnormal FA clusters derived from subject-specific injury profiles (i.e., individual z-score maps) along a common white matter skeleton. The mTBI + PTSD group evinced a greater number of abnormally low FA clusters relative to both the healthy controls and the mTBI group without PTSD (p < .05). Across the groups with a history of mTBI, increased numbers of abnormally low FA clusters were significantly associated with PTSD symptom severity, depression, post-concussion symptoms, and reduced information processing speed (p < .05). These findings highlight the utility of subject-specific microstructural analyses when searching for mTBI-related brain abnormalities, particularly in patients with PTSD. This study also suggests that patients with a history of mTBI and comorbid PTSD, relative to those without PTSD, are at increased risk of FA abnormalities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The global incidence of mild traumatic brain injury (mTBI) is estimated at 600 per 100,000 people (Cassidy et al., 2004; Faul et al., 2010). Despite the frequency of these injuries, difficulties in diagnosis persist, as no objective measures of mTBI currently exist. This becomes understandable, given that mTBIs vary in their mechanism of injury, course of pathophysiology, and clinical sequelae – all of which can interact, making this condition highly heterogeneous (Bigler and Maxwell, 2012; Cassidy et al. 2014; McMahon et al. 2014). Diagnosis is further complicated by common comorbidities with symptoms that overlap mTBI-related sequelae. More specifically, a significant proportion of chronic post-concussive sequelae are shared with posttraumatic stress disorder (PTSD), including depression, anxiety, insomnia, irritability, and fatigue (see Stein and McAllister, (2009) for a review). Additionally, PTSD often occurs concomitantly with mTBIs, especially in combat veterans (Carlson et al., 2011). Thus, the concurrent diagnosis of mTBI and PTSD presents an important and unique diagnostic challenge.
Diffuse axonal injury is increasingly recognized as a consequence of traumatic brain injury along the entire spectrum of severity, including mild cases (for a review, see (Johnson et al., 2013)). Human and animal histological studies both show that brain white matter is vulnerable to alteration following mTBI (Blumbergs et al., 1994; Browne et al., 2011). Unfortunately, evidence of mTBI-related diffuse axonal injuries has not been supported using conventional neuroimaging tools, such as computerized tomography (i.e., CT scans) or structural magnetic resonance imaging, both of which are used in clinical settings (for detailed review of this issue see Shenton et al., 2012). A lack of positive neuroimaging findings also has important implications for the minority (between 15 and 30%) of mTBI patients who have chronic symptoms (i.e., persistent post-concussion syndrome; see review in Shenton et al., 2012). Without radiological evidence of injury using conventional imaging, some of these cases have their post-concussive symptoms attributed to behavioral etiologies (Mounce et al., 2013) or often co-occurring disorders such as PTSD (Hoge et al., 2008). Thus, there is a crucial need to develop tools to explore whether mTBI induced brain alterations can be characterized in vivo.
Diffusion tensor magnetic resonance imaging (DTI) - with its ability to quantify the diffusivity of water molecules along axons (Basser, 1995; Pierpaoli and Basser, 1996) - has provided an important approach in the search for brain biomarkers of mTBI axonal injury. Of the commonly studied DTI metrics, fractional anisotropy (FA) is the most popular DTI metric to measure whole-brain and region-of-interest white matter architecture in mTBI (Aoki et al., 2012). Although reduced FA has, in some studies, been associated with mTBI (Aoki and Inokuchi, 2016), this is not always the finding (e.g., Ilvesmäki et al., 2014). The heterogeneity of these injuries - which occur at a microstructural level – thus presents a unique challenge. Traditional, group-based analyses of DTI may, in fact, overlook individual profiles of injury, which are inherently more subtle and heterogeneous across individuals. Recently, subject-specific approaches have emerged to meet this challenge.
Subject-specific analyses standardize patients’ FA profiles to those of healthy controls, at the individual level, before groups are compared (Bouix et al., 2013; Davenport et al., 2012; Lipton et al., 2012; Taber et al., 2015). In this way, subject-specific analyses of DTI metrics overcome the measurement limitations imposed by the spatially expansive and individually variable white matter injuries associated with mTBI. An extension of the subject-specific approach is the cluster-based (or “pothole”) analysis. This approach was first advanced by White et al., (2009) in a DTI study of schizophrenia. To summarize: clusters of voxels with abnormal values (e.g., z-scores beyond a given threshold) are calculated at the subject-specific analysis level before they are compared between groups. Although this approach has shown promise in adult and pediatric DTI studies of mTBI (Jorge et al., 2012; Ling et al., 2012; Mayer et al., 2012; Miller et al., 2016), the absence of cross-validation methods (e.g., leave-one-out; see Methods) in those studies raises the risk of bias (Mayer et al., 2014; Watts et al., 2014).
As reviewed by Stein & McAllister, (2009), several neuroimaging modalities have started to elucidate brain regions that appear, both commonly and differentially, associated with PTSD and mTBI. Those authors point out that the dorsolateral prefrontal cortex, orbitofrontal cortex, and hippocampus have been implicated in structural and functional neuroimaging studies of both conditions. Despite these commonalities, there appears to be greater divergence between these conditions, in general. mTBI is typically associated with expansive disruption of anterior and ventral areas of the temporal and prefrontal cortices (Bigler & Maxwell, 2012). On the other hand, PTSD is predominately linked to the amygdala, anterior cingulate gyrus, medial retrosplenial cortex, and precuneus, each of which has been associated to the clinical features of PTSD (Sartory et al., 2013). Moreover, recent evidence suggests that PTSD affects DTI measures differently than mTBI, with both evincing different abnormal signatures (Bazarian et al., 2013; Davenport et al., 2015). Taken together, the evidence suggests that comorbid mTBI and PTSD would demonstrate greater cerebral disruption than either condition alone.
The aim of this study was to compare the profile of FA between groups with a history of mTBI, comorbid mTBI and PTSD (mTBI + PTSD), and no prior brain injury (i.e., healthy controls). We studied these three groups using conventional approaches to DTI analyses (i.e., tract-based spatial statistics), as well as cluster-based analyses using a leave-one-out approach. We hypothesized that the greatest number of abnormal clusters would be present in those with mTBI + PTSD, followed by the mTBI-only group. Furthermore, we explored associations between abnormal clusters and various mTBI-relevant neuropsychiatric and neuropsychological measures.
Methods
Recruitment
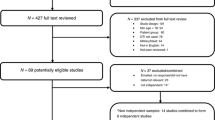
We recruited participants via a 10-site PTSD/TBI clinical consortium funded by the Department of Defense: Injury and Traumatic Stress (INTRuST; intrust.sdsc.edu) Consortium. The INTRuST Consortium comprises 10 academic and medical sites collaborating to improve the care and understanding of PTSD and traumatic brain injuries. Six of these sites acquired neuroimaging data on three-Tesla (3 T) scanners (two per manufacturer: Siemens, General Electric, and Philips).
Inter-site imaging variability
Inter-site acquisition of imaging data may contribute to variability in diffusion imaging metrics, despite similar acquisition parameters across scanners (Helmer et al., 2016). As a preliminary step, we investigated the variability of FA in healthy controls (n = 112) across the six INTRuST sites where imaging data were acquired. We used traditional analyses of DTI, as described below, but without adjusting for years of education. Across sites, FA varied widely (p < .05). However, there were no significant within-manufacturer differences for the Philips and Siemens scanners (see Fig. 1). The data acquired from the Philips scanners were the least variable and were drawn from the largest subset of participants. Thus, the current study only includes data obtained from the sites that used Philips scanners, and it represents an interim analysis of the entire dataset from the INTRuST Consortium. Our group recently reported a method to harmonize multi-site MRI data (Mirzaalian et al., 2016), and efforts are underway to analyze the neuroimaging data across all six INTRuST imaging sites using the newly developed harmonization algorithm (see above).
Participants
We obtained data from three groups of participants for this study: mTBI (n = 35), mTBI and PTSD (mTBI + PTSD; n = 22), and healthy controls (HCs; n = 37). The groups’ demographic data are presented in Table 1. To be included in the study, participants were English speaking males or females, 18 to 65 years of age, and capable of providing informed consent. Inclusion criteria specific to the mTBI and mTBI + PTSD groups were: history of mTBI, PTSD (mTBI + PTSD group only). Psychoactive medications were permitted, as well as a history of alcohol or substance dependence, if in remission for 30 days preceding data collection.
Exclusion criteria for the mTBI and mTBI + PTSD groups were: bipolar I, psychotic, delirium, or dementing disorders, uncontrolled chronic disease, any other CNS disease or event affecting the brain, and oral or intramuscular steroid use in the last 4 months. The following exclusionary criteria were applied to HCs: any brain-impacting medical condition or medication, uncontrolled hypertension, Axis I psychiatric diagnosis, English acquisition after 5 years of age, history of learning disability, and history of brain injury accompanied by a hospital stay or abnormal imaging findings. We excluded potential participants from all groups on the basis of MRI contraindications.
Screening and diagnostic instruments
As part of the INTRuST protocol, participants completed a series of measures spanning cognitive, psychosocial, and behavioral domains (see supplementary material). For the present study, we selected a relevant subset of all available INTRuST measures. To assess participants’ study eligibility, we used the Mini International Neuropsychiatric Instrument (MINI; Sheehan et al., 1998) in concert with a 20-min screening interview. Similarly, we used the MINI to determine PTSD diagnosis in all but five participants. For those participants, PTSD diagnosis was determined with the PTSD Checklist - Civilian Version (PCL-C; Blanchard et al., 1996), which is a 17-item, self-report measure of PTSD symptoms occurring over the previous month. All participants completed the PCL-C, from which a symptom severity score was derived. We established participants’ history of mTBI with the INTRuST TBI Screening Instrument, which is a three item, self-report questionnaire on history of mTBI, based on the diagnostic criteria advanced by the American Congress of Rehabilitative Medicine (Mild Traumatic Brain Injury Committee of the Head Injury Interdisciplinary Special Interest Group of the American Congress of Rehabilitation Medicine, 1993). This instrument establishes mTBI on the basis of past head or brain injury with either: 1) immediate loss of consciousness or alteration of consciousness or unawareness of the event or 2) amnesia before or after the event(s).
Clinical and behavioral measures
With the Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001), we measured participants’ depression symptoms. The PHQ-9 is a nine-item, self-report measure with strong sensitivity and specificity in TBI populations (Fann et al., 2005). We measured post-concussive symptoms with the Rivermead Post Concussive Symptoms Questionnaire (RPQ; King et al., 1995). We used the Eyres et al., (2005) scoring scheme, where the first three items (RPQ-3) reflect current headaches, dizziness and nausea, and the subsequent items (RPQ-13) capture other lifestyle-interfering symptoms that tend to manifest in the post-acute phase of injury. We did not measure post-concussive symptoms in HCs using the RPQ. We assessed information processing speed with the following measures: coding and symbol search subtests from the Wechsler Adult Intelligence Scale III (WAIS; Wechsler, 1997) and the Trail Making Test (Trails A, Trails B; US Army, 1944).
Image acquisition and preprocessing
As part of the INTRuST neuroimaging protocol, each participant completed MRI scanning sessions comprising the following imaging modalities: T1 weighted, T2 weighted, susceptibility weighted, proton density, functional, and diffusion weighted. For the present study, only the diffusion weighted imaging data were analyzed; their acquisition parameters are listed in Table 2.
We first conducted a quality verification of our data. Our pipeline comprised visual and semi-automated quality checks of the data, including the detection of signal dropout or venetian blind artifacts, as well as head motion, ghosting, inter-slice and intra-slice intensity artifact, and checkerboard artifact. Further, we applied head motion and eddy current correction scripts. No datasets were excluded due to the presence of excessively poor quality, which we defined as at least five instances of the above-noted compromises of quality per individual volume. We used 3D Slicer version 4.5 (Surgical Planning Laboratory, Brigham and Women’s Hospital, Boston, USA) for visual inspections, while our in-house scripts were written for and run with Matlab R2012b 64-bit (MathWorks, Inc., Natick, MA, USA). Moreover, we used in-house scripts to generate tensor masks, which we manually corrected in 3D Slicer, when needed. At the voxel level, we estimated eigenvalues and eigenvectors using a multivariate linear fitting algorithm on the diffusion tensor. From the tensor data, we calculated an image of FA for each participant. All measures were completed blind to group membership.
Next, we conducted tract-based spatial statistics (TBSS; Smith et al., 2006), preprocessing the FA images using FSL version 5.0 (FMRIB Software Library, Oxford, UK). We non-linearly registered each FA image into a 1x1x1mm standard space using the FMRIB_58 template via the tbss_2_reg script. We then applied the tbss_3_postreg script to affine-align the warped images into MNI152 (Montreal Neurological Institute) space. Using tbss_4_prestats, we generated a mean FA image thresholded at 0.2, a binarized FA mask image, and a 4-D image of each participant’s mean FA values along the FA skeleton. These measures were also completed blind to group membership.
Statistical analyses
Clinical and behavioral characteristics analysis
We used SPSS version 22 (IBM Corp., New York, USA) for non-TBSS analyses, which comprised one-way analyses of variance (ANOVA), Tukey’s HSD Tests, Kruskal-Wallis H Tests, Mann-Whitney U Tests, and Pearson correlations between FA clusters and participant characteristics. We compared the three groups with respect to clinical and behavioral characteristics. However, we examined correlations only for the mTBI and mTBI + PTSD groups, as scores on these measures were, as would be expected, uniformly low and have little variance HCs.
Traditional FA analysis
We used a one-way ANOVA general linear model for between-group comparisons of the FA images. We entered years of education as a covariate, since the groups differed significantly with respect to this variable (p < .05). We conducted TBSS using the voxel-wise approach implemented in FSL. We did these analyses using FSL’s randomise feature set to 5000 permutations and using threshold-free cluster enhancement (Smith and Nichols, 2008). We considered results significant at p < .05, after Bonferroni correction for multiple comparisons.
Variance of FA analysis
Given the heterogeneous pathology of mTBI, measures of whole-brain FA variability at the subject-level are a promising approach to increasing sensitivity (Delic et al., 2016) - particularly when traditional, voxel-wise FA analyses can be equivocal (Ilvesmäki et al., 2014). To explore this concept further, we calculated the variance and mean of FA over the entire TBSS skeleton. Using in-house Matlab scripts, we adjusted FA values at the voxel-level using a fitted general linear model when the model, including the effect of education, was significant. We compared the variance and mean FA values separately between groups.
Subject-specific FA analysis
Next, for each participant, we created an individual profile of injury by computing a voxel-wise z-score map over the TBSS FA skeleton (adjusted for years of education, as above). For controls, we calculated z-scores using a leave-one-out approach to account for potential bias. Although this method has been absent from recent cluster-based studies of diffusion metrics in mTBI, it can reduce the risk of false positives introduced by reference groups with nonindependence (Bouix et al., 2013; Mayer et al., 2014; Watts et al., 2014). For all groups (i.e., mTBI + PTSD, mTBI, HCs), we computed voxel-wise z-scores based on the mean and standard deviation of the healthy control group.
Using FSL’s cluster and fslmaths programs, we calculated the number of clusters with a minimum of five voxels with z-scores of three or greater, thresholds previously shown to be sensitive to mTBI by Miller et al., (2016). We generated subject-specific FA z-score images of positive, absolute, and negative values. We created images of positive and negative z-scores to measure FA-related abnormal increases and decreases, respectively. We generated images of absolute z-scores to measure overall FA abnormalities. When conducting group-based statistics, we square-root transformed each group’s total number of clusters to remove the observed positive skew of the original distribution, as done by Miller et al., (2016).
Exploratory analysis of age-effect
To explore whether there was an association between age and the number of abnormal FA clusters, we conducted Pearson correlations across each of the groups. We then conducted exploratory analyses (i.e., ANCOVA) covaried with age to determine if this variable impacted our findings across the groups.
Exploratory analysis of depression
In line with the literature demonstrating high comorbidity between depression and PTSD (Ginzburg et al., 2010; Rytwinksi et al., 2013), our results revealed that depression had a similar pattern to PTSD across our groups (see Table 1). Specifically, the MTBI + PTSD group evinced greater PTSD and depression than either the mTBI group and healthy controls. In turn, the mTBI group demonstrated increased PTSD and depression, relative to healthy controls. Thus, we explored whether depression and PTSD were sufficiently independent to examine their unique contributions to the between-group differences of abnormal FA clusters. Accordingly, we conducted a Pearson correlation between depression (i.e., PHQ-9 scores) and PTSD symptom severity, prior to further exploration.
Results
Clinical characteristics analyses
Table 1 contains summary statistics and analysis results for data pertaining to our study sample’s clinical characteristics. The groups did not differ in age or sex distribution (p > .05). However, participants with mTBI and PTSD (i.e., the mTBI + PTSD group) had fewer years of education than the mTBI and HC groups (ANOVA, p < .001). Not surprisingly, we found a main effect of group for PTSD symptom severity (ANOVA, p < .001). Our post hoc analysis revealed the greatest mean PTSD symptom severity was in the mTBI + PTSD group, followed by those with mTBI only (p < .05). We observed the same pattern with respect to depression symptoms (ANOVA, p = < .001). Mann-Whitney U tests revealed, relative to participants with mTBI, that those with mTBI + PTSD reported greater post-concussive symptoms (RPQ-3, p = .001; RPQ-13, p = < .001). Across each neuropsychological measure of information processing speed, the mTBI + PTSD group performed more poorly than at least one comparison group (see Table 1 for post hoc comparisons; all p < .05).
Analyses of education-adjusted FA
We conducted all FA analyses using years of education-adjusted values. We first analyzed FA using a traditional TBSS approach. Across the three groups, the omnibus test of FA was non-significant (p > .05). Similarly, the groups did not differ in terms of the mean or variance of FA (both p > .05).
Next, using omnibus tests, we compared the groups with respect to the number of abnormal FA clusters of at least five voxels, each of which had a z-score of three or more. Table 3 displays the group-wise mean number of abnormal clusters, which were square-root transformed to remove the positive skew of the original distributions. For the analyses of positive and absolute z-score clusters, the groups were equivocal (p > .05). When visually inspecting the distribution of clusters of negative z-scores, we observed one outlier in the mTBI and HC groups. We confirmed the outliers had a standardized score greater than four and omitted them from analysis. The omnibus test for the negative z-score cluster analysis was statistically significant (F(2, 91) = 4.409, p = .015). Our post hoc Tukey test showed the mTBI + PTSD group had significantly more clusters of negative FA compared to both the mTBI group and HCs (p < .05; see Fig. 2). To illustrate the heterogeneity of mTBI pathology, Fig. 3 contains axial slices from eight members of the mTBI + PTSD group along with clusters of abnormally low FA. The mTBI group did not differ from the mTBI + PTSD group or the HCs with respect to clusters or abnormally low FA (p > .05).
Group-wise mean number of clusters of five or more voxels with z-scores of 3 and more (or −3 and less in the case of clusters of low FA). We applied a square-root transformation to the means to remove positive skew of original distributions. Error bars represent the standard error of the mean. a The groups did not differ with respect to overall FA abnormalities (i.e., absolute FA; p < .05), b The groups did not differ in terms of mean number of clusters with abnormally high FA, c The MTBI + PTSD group had a significantly greater number of clusters of abnormally low FA compared to mTBI and HCs (p < .05)
Age-effect analysis
Age was not significantly associated with the number of clusters with abnormally positive, negative, or absolute FA (all p > .05). When we compared the groups with respect to the number of clusters of abnormal FA, covaried with age, our principal findings remained unchanged. Specifically, the groups did not differ in terms of the number of abnormal absolute or positive FA clusters (both p > .05). As was the case when we did not control for age, there was a significant difference in the number of clusters of abnormally negative FA (F(2,91) = 4.175, p = .019), with the mTBI + PTSD group evincing a greater number of such clusters, relative to the mTBI group and the HCs (p < .05). Thus, age did not impact our findings.
FA and symptom measures
Across the mTBI and mTBI + PTSD groups, we conducted exploratory analyses of associations between the number of abnormally negative clusters and our symptom severity measures (see Fig. 4). We found significant positive associations between the number of negative clusters and the following: PTSD symptom severity (r(53) = .37, p = .006), RPQ-13 post-concussive symptoms (r(54) = .35, p = .011), depression (r(56) .37, p = .005), and Trails B (r(54) = .32, p = .019). We found a significant negative association between the number of abnormally negative clusters and WAIS coding (r(39) = −.30, p = .034). We conducted these analyses on an exploratory basis, and the p-values we report were not adjusted for multiple comparisons. When we applied a Holm-Bonferroni correction (Holm, 1979), significant relationships (for the number of abnormally negative clusters) remained with PTSD symptom severity and depression, although those with postconcussive symptoms, Trails B, and WAIS coding were lost.
Relationships between clusters of abnormally low fractional anisotropy (FA) and clinical measures in the mTBI and mTBI + PTSD participants. The number of clusters was square-root transformed to account for positive skew of the original distribution. We conducted these analyses on an exploratory basis, and the p-values we report were not adjusted for multiple comparisons. When we applied a Holm-Bonferroni correction (Holm, 1979), significant relationships (for the number of abnormally negative clusters) remained with PTSD symptom severity and depression, although those with postconcussive symptoms, Trails B, and WAIS coding were lost
Exploratory analysis of depression
We found a strong positive association between depression and PTSD, r(91) = .86, p = .000). As PTSD and depression were insufficiently independent, we did not conduct further analyses to explore their relative contributions to the between-group differences of abnormal FA clusters.
Discussion
In contrast to more conventional, voxel-based analyses of fractional anisotropy (FA), this study demonstrates subject-specific characterizations of FA that can distinguish mTBI in the context of PTSD, relative to mTBI alone and the absence of either (i.e., healthy controls HCs)). In addition to increased white matter abnormalities, patients with both mTBI and PTSD (i.e., the mTBI + PTSD group) reported greater post-concussive symptoms, depression, and evinced slower speed of information processing, relative to the other two groups: mTBI only and HCs.
Our study adds to a growing literature that suggests that subject-specific approaches may improve the detection of white matter abnormalities in mTBI (Bouix et al., 2013; Davenport et al., 2012; Jorge et al., 2012; Lipton et al., 2012; Mayer et al., 2012; Miller et al., 2016; Taber et al., 2015). This is an important area of research, since this injury is challenging to detect by visual inspection using conventional neuroimaging (i.e., magnetic resonance imaging, computed tomography (CT)), and traditional, voxel-wise analyses of DTI data result in inconsistent findings (e.g., Aoki et al., 2012). Accordingly, we were unable to find voxel-level group differences in FA with tract-based spatial statistics (TBSS), even when examining the spatial extent of FA irregularities (i.e., variance of FA). We first measured the variability of FA to capture the subtle and expansive nature of mTBI, but this approach led to negative findings. We then used an approach we thought more sensitive, where we computed individualized maps of FA to capture the heterogeneity of mTBI. This latter step was crucial to discovering between-group differences in FA. Thus, by building subject-specific profiles of injury, we were able to demonstrate how voxel-based techniques are able to detect mTBI-related white matter irregularities at a group level of analyses.
We found that participants with mTBI who had no history of PTSD (i.e., the mTBI group) did not have a significantly different number of abnormally low FA clusters in white matter, relative to HCs. This finding is in contrast to other subject-specific studies of mTBI (Lipton et al., 2012; Mayer et al., 2012). However, it is noteworthy that the aforementioned studies explored whole-brain FA, whereas we concentrated on the skeleton of the principal white matter (which includes a limited number of proximal voxels). Relatedly, we have previously shown abnormal FA in gray matter regions in an independent sample with persistent post-concussive symptoms (Bouix et al., 2013). Thus, for the present study, it may be that, by excluding areas outside the principal white matter tracts (i.e., gray matter), our attempts were too circumscribed to detect FA abnormalities in patients with mTBI and no comorbidities. On the other hand, our present findings are in line with Ling et al., (2012), who conducted a subject-specific mTBI study that failed to find a significant presence of abnormally low FA clusters in a whole-brain analysis. Future work is needed to clarify these disparate findings.
Aside from inter-study methodological differences, one reason for the inconsistent findings is likely the stage of the head injury, relative to the measurement period. For example, Lipton et al., (2012) found clusters of abnormally high FA 2 weeks post-mTBI, but on 3- and 6-month follow-up of the same sample, clusters of both low and high FA were noted. Further, and as pre-viously noted, in mTBI patients with chronic (9.5 to 138 months post-injury) symptoms, Bouix et al., (2013) found distributed clusters of increased FA within gray matter, but few clusters of abnormal values in white matter regions. Thus, when it comes to measuring clus-ters of abnormal FA, timing is important. The present study examined self-reported chronic mTBI, and data were not available to explore time-since-injury (although it should be noted that most subjects had been injured years previously). As mTBI studies that account for in-dividual profiles of injury have only recently emerged, future work should elucidate the time course of injuries along with FA abnormalities, which may change as patients recover or experience chronic symptoms.
In addition to a significant number of FA “potholes” (White et al., 2009), the mTBI + PTSD group evinced more psychological dysfunction, relative to the two other groups. More specifically, the mTBI + PTSD group showed increased depression, chronic post-concussive symptoms, and PTSD symptom severity. From a cognitive function perspective, the mTBI + PTSD group displayed decreased speed of information processing. Furthermore, psychological and cognitive functioning shared expected associations with the number of clusters of abnormally low FA. Increases in psychological dysfunction were significantly positively correlated with the number of FA potholes. Moreover, increases in the number of FA potholes were significantly negatively associated with decreased cognitive efficiency.
Our finding of greater depression in the mTBI + PTSD group is consonant with the well-established co-occurrence of depression with PTSD (Rytwinski et al., 2013). Although we recruited our mTBI + PTSD group from a predominantly civilian population, studies of veteran samples show strong associations between post-traumatic stress, depression, and post-concussive symptoms (Hoge et al., 2008; Lange et al., 2014). Additionally, information processing speed can be negatively influenced by depression, PTSD, mTBI, and abnormal FA (Bernstein, 2002; Kennedy and Raz, 2009; Tsourtos et al., 2002; Wrocklage et al., 2016). The presence of these factors and their associations in this study highlight further the challenges faced by patients with mTBI and PTSD. Furthermore, across the mTBI and mTBI + PTSD groups, we found participants with more white matter potholes were psychologically less well, overall. This suggests that the greater the extent of brain injury (i.e., white matter FA potholes), the greater the severity of a broad range of mental health and neurocognitive symptoms. This calls for a much wider examination of the white matter pothole analysis across a range of neuropsychiatric disorders.
The intersection of depression, PTSD, and mTBI is an important area of research, particularly in light of the overlap in symptomatology across these three often-comorbid conditions. With this overlap, it remains a scientific and clinical challenge to measure and disentangle the relative contributions of each condition. Accordingly, in our sample, we found a strong association between PTSD and depression.
Self-report measures of PTSD, and especially depression, often assess sequelae that represent shared facets. For example, although the PHQ-9 is predominately a depression measure, three of its nine items assess domains that are often adversely impacted, at least acutely, in mTBI (i.e., energy, concentration, slowed cognitive efficiency). Moreover, symptoms of PTSD are also captured by the PHQ-9, including fatigue, hyperarousal, and, as already mentioned, concentration. Nevertheless, as with most (if not all) self-report measures of depression, some items of the PHQ-9 also reflect domains generally unique to the construct of depression: loss of interest, low mood, changes in appetite, shame, self-harm, and suicidal ideation. Thus, regardless of the absence of a “pure” measure of depression, given the often co-occurrence of depression and mTBI, it remains important to measure depression (with current tools, despite their limitations) in studies of mTBI. However, future work should be directed towards developing improved tools to differentiate PTSD and depression.
Our findings also suggest that diffuse axonal injury may play an aggravating role in chronic mTBI-related dysfunction in persons with PTSD. MTBI + PTSD participants - at the exclusion of those with mTBI only (and, of course, HCs) - had a greater presence of FA potholes and were more symptomatic. This is in contrast to Miller et al., (2016), who reported that white matter irregularities mediate the association between blast-related mTBI (with loss of consciousness) and physical post-concussive symptoms - after controlling for post-traumatic stress symptoms. Relevant distinctions between our studies are worth noting. First, where we used a leave-one-out approach to minimize the risk of bias, Miller et al., (2016) did not include such a cross-validation technique, the absence of which can increase false positives (Mayer et al., 2014; Watts et al., 2014). Next, where we included an mTBI group with PTSD, Miller et al., (2016) did not include such a group in their veteran samples. Nonetheless, they measured PTSD symptom severity, which did not differ between their groups. Additionally, PTSD symptom severity had no effect on clusters with reduced FA. In contrast, we found FA potholes were related to increased dysfunction, including PTSD symptom severity. Thus, by including a group with mTBI and PTSD (i.e., the mTBI + PTSD group), our findings suggest that white matter potholes play an important role in the burden of co-occurring mTBI and PTSD. Furthermore, our study highlights the importance of the pothole analysis within the mTBI + PTSD population, particularly when other voxel-wise approaches may fail to find an association between white matter abnormalities and PTSD in the context of mTBI (Morey et al. 2013).
There are, nonetheless, limitations in this study that warrant consideration when interpreting results. For example, we did not include a PTSD-only group. Compared to HCs and those with mTBI only, participants with PTSD and mTBI had a greater number of negative FA clusters. However, we cannot rule out the possibility that PTSD alone accounted for our findings. Additionally, we captured history of mTBI via participant self-report, which may have been inaccurate and contributed to our null findings of negative FA clusters in the mTBI only group. Along those lines, we did not capture data regarding the frequency of mTBI exposure, which could have moderated the relationships between mTBI and FA potholes. Our search for FA abnormalities was restricted to only the TBSS white matter skeleton, which comprises the principal white matter tracts and their nearby surrounding voxels. Relatedly, and as noted previously, there is increasing evidence of diffusion changes in gray matter, particularly in more chronic cases of mTBI (Bouix et al., 2013). Thus, as previously mentioned, the scope of our search for abnormal FA clusters may have been too limited to detect differences between mTBI and HCs. Another limitation to this study is the absence of injury location data, which raises the possibility that the unique profiles of abnormal FA in our sample reflected a diversity of mTBI impact and/or rotational mechanisms. In future analyses, and having recently developed techniques to harmonize neuroimaging data acquired from different scanners (Mirzaalian et al., 2016), we will work on full-brain diffusion analyses of combined data from the INTRuST sites. It is our hope that by increasing our statistical power we will be able to discriminate FA profiles of mTBI alone from those of HCs. Nonetheless, and despite the aforementioned limitations, the present study makes a novel contribution to the mTBI and PTSD literature: cross-validated, subject-specific, voxel-wise analysis of FA is a sensitive measure of mTBI for those who are also diagnosed with PTSD. Additionally, we have shown associations between white matter potholes and dysfunction across a number of domains commonly impacted by PTSD and chronic mTBI.
Summary
By using a subject-specific approach, this study demonstrated that conventional, voxel-based analyses of DTI data might be improved upon to detect DTI evidence of mTBI in patients with PTSD. Furthermore, participants with a history of mTBI and PTSD showed increased FA potholes and were more symptomatic with respect to depression, post-concussive symptoms, and information processing speed. Additionally, there was a positive association between these domains and the number of clusters of abnormally low FA. In summary, equivocal neuroimaging findings – which may occur when only conventional imaging, such as MRI and CT are used – can promote nonbiologic, behavioral explanations of chronic post-mTBI PTSD symptoms. In contrast, we have shown radiological evidence that brain abnormalities in this population can be detected using more advanced imaging techniques such as DTI. Uncovering a biological correlate of comorbid mTBI and PTSD dysfunction is an important first step towards improving early detection and treatment of these frequently co-occurring conditions.
References
Aoki, Y., & Inokuchi, R. (2016). A voxel-based meta-analysis of diffusion tensor imaging in mild traumatic brain injury. Neuroscience and Biobehavioral Reviews, 66, 119–126. doi:10.1016/j.neubiorev.2016.04.021.
Aoki, Y., Inokuchi, R., Gunshin, M., Yahagi, N., & Suwa, H. (2012). Diffusion tensor imaging studies of mild traumatic brain injury: a meta-analysis. Journal of Neurology, Neurosurgery, and Psychiatry, 83(9), 870–876. doi:10.1136/jnnp-2012-302742.
Army, U. S. (1944). Army individual test battery: manual for directions and scoring. Washington: War Department, Adjutant General’s Office.
Basser, P. J. (1995). Inferring microstructural features and the physiological state of tissues from diffusion-weighted images. NMR in Biomedicine, 8(7-8), 333–344 http://www.ncbi.nlm.nih.gov/pubmed/8739270.
Bazarian, J. J., Donnelly, K., Peterson, D. R., Warner, G. C., Zhu, T., & Zhong, J. (2013). The relation between posttraumatic stress disorder and mild traumatic brain injury acquired during operations enduring freedom and Iraqi freedom. The Journal of Head Trauma Rehabilitation, 28(1), 1–12. doi:10.1097/HTR.0b013e318256d3d3.
Bernstein, D. M. (2002). Information processing difficulty long after self-reported concussion. Journal of the International Neuropsychological Society, 8(5), 673–682 http://www.ncbi.nlm.nih.gov/pubmed/12164676.
Bigler, E. D., & Maxwell, W. L. (2012). Neuropathology of mild traumatic brain injury: relationship to neuroimaging findings. Brain Imaging and Behavior, 6(2), 108–136. doi:10.1007/s11682-011-9145-0.
Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., & Forneris, C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. doi:10.1016/0005-7967(96)00033-2.
Blumbergs, P. C., Scott, G., Manavis, J., Wainwright, H., Simpson, D. A., & McLean, A. J. (1994). Staining of amyloid precursor protein to study axonal damage in mild head injury. The Lancet, 344(8929), 1055–1056 http://www.ncbi.nlm.nih.gov/pubmed/7523810.
Bouix, S., Pasternak, O., Rathi, Y., Pelavin, P. E., Zafonte, R., & Shenton, M. E. (2013). Increased gray matter diffusion anisotropy in patients with persistent post-concussive symptoms following mild traumatic brain injury. PloS One, 8(6), e66205. doi:10.1371/journal.pone.0066205.
Browne, K. D., Chen, X.-H., Meaney, D. F., & Smith, D. H. (2011). Mild traumatic brain injury and diffuse axonal injury in swine. Journal of Neurotrauma, 28(9), 1747–1755. doi:10.1089/neu.2011.1913.
Carlson, K. F., Kehle, S. M., Meis, L. A., Greer, N., Macdonald, R., Rutks, I., et al. (2011). Prevalence, assessment, and treatment of mild traumatic brain injury and posttraumatic stress disorder: a systematic review of the evidence. The Journal of Head Trauma Rehabilitation, 26(2), 103–115. doi:10.1097/HTR.0b013e3181e50ef1.
Cassidy, J. D., Carroll, L. J., Peloso, P. M., Borg, J., von Holst, H., Holm, L., et al. (2004). Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine, (43 Suppl), 28–60. doi: 10.1016/j.apmr.2013.08.299.
Cassidy, J. D., Cancelliere, C., Carroll, L. J., Côté, P., Hincapié, C. A., Holm, L. W., et al. (2014). Systematic Review of Self-Reported Prognosis in Adults After Mild Traumatic Brain Injury: Results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Archives of physical medicine and rehabilitation, 95(3), S132–S151. doi:10.1016/j.apmr.2013.08.299
Davenport, N. D., Lim, K. O., Armstrong, M. T., & Sponheim, S. R. (2012). Diffuse and spatially variable white matter disruptions are associated with blast-related mild traumatic brain injury. NeuroImage, 59(3), 2017–2024. doi:10.1016/j.neuroimage.2011.10.050.
Davenport, N. D., Lim, K. O., & Sponheim, S. R. (2015). White matter abnormalities associated with military PTSD in the context of blast TBI. Human Brain Mapping, 36(3), 1053–1064. doi:10.1002/hbm.22685.
Delic, J., Alhilali, L. M., Hughes, M. A., Gumus, S., & Fakhran, S. (2016). White matter injuries in mild traumatic brain injury and posttraumatic migraines: diffusion entropy analysis. Radiology, 279(3), 859–866. doi:10.1148/radiol.2015151388.
Eyres, S., Carey, A., Gilworth, G., Neumann, V., & Tennant, A. (2005). Construct validity and reliability of the rivermead post-concussion symptoms questionnaire. Clinical Rehabilitation, 19(8), 878–887 http://www.ncbi.nlm.nih.gov/pubmed/16323387.
Fann, J. R., Bombardier, C. H., Dikmen, S., Esselman, P., Warms, C. A., Pelzer, E., et al. (2005). Validity of the patient health questionnaire-9 in assessing depression following traumatic brain injury. The Journal of Head Trauma Rehabilitation, 20(6), 501–511 http://www.ncbi.nlm.nih.gov/pubmed/16304487.
Faul, M., Xu, L., Wald, M. M., & Coronado, V. G. (2010). Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. http://www.cdc.gov/traumaticbraininjury/tbi_ed.html.
Ginzburg, K., Ein-Dor, T., & Solomon, Z. (2010). Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. Journal of Affective Disorders, 123, 249–257. doi:10.1016/j.jad.2009.08.006.
Helmer, K. G., Chou, M.-C., Preciado, R. I., Gimi, B., Rollins, N. K., Song, A., et al. (2016). Multi-site study of diffusion metric variability: effects of site, vendor, field strength, and echo time on regions-of-interest and histogram-bin analyses. In SPIE Medical Imaging (p. 97882U–97882U–10). Presented at the Medical Imaging 2016: Biomedical Applications in Molecular, Structural, and Functional Imaging, International Society for Optics and Photonics. Accessed 9 June 2016. http://proceedings.spiedigitallibrary.org/proceeding.aspx?articleid=2511179.
Hoge, C. W., McGurk, D., Thomas, J. L., Cox, A. L., Engel, C. C., & Castro, C. A. (2008). Mild traumatic brain injury in U.S. Soldiers returning from Iraq. The New England Journal of Medicine, 358(5), 453–463. doi:10.1056/NEJMoa072972.
Holm, S. (1979). A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics, 65-70.
Ilvesmäki, T., Luoto, T. M., Hakulinen, U., Brander, A., Ryymin, P., Eskola, H., et al. (2014). Acute mild traumatic brain injury is not associated with white matter change on diffusion tensor imaging. Brain, 137(Pt 7), 1876–1882. doi:10.1093/brain/awu095.
Johnson, V. E., Stewart, W., & Smith, D. H. (2013). Axonal pathology in traumatic brain injury. Experimental Neurology, 246, 35–43. doi:10.1016/j.expneurol.2012.01.013.
Jorge, R. E., Acion, L., White, T., Tordesillas-Gutierrez, D., Pierson, R., Crespo-Facorro, B., & Magnotta, V. A. (2012). White matter abnormalities in veterans with mild traumatic brain injury. The American Journal of Psychiatry, 169(12), 1284–1291. doi:10.1176/appi.ajp.2012.12050600.
Kennedy, K. M., & Raz, N. (2009). Aging white matter and cognition: differential effects of regional variations in diffusion properties on memory, executive functions, and speed. Neuropsychologia, 47(3), 916–927. doi:10.1016/j.neuropsychologia.2009.01.001.
King, N. S., Crawford, S., Wenden, F. J., Moss, N. E., & Wade, D. T. (1995). The rivermead post concussion symptoms questionnaire: a measure of symptoms commonly experienced after head injury and its reliability. Journal of Neurology, 242(9), 587–592. doi:10.1007/BF00868811.
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi:10.1046/j.1525-1497.2001.016009606.x.
Lange, R. T., Brickell, T. A., Kennedy, J. E., Bailie, J. M., Sills, C., Asmussen, S., et al. (2014). Factors influencing postconcussion and posttraumatic stress symptom reporting following military-related concurrent polytrauma and traumatic brain injury. Archives of Clinical Neuropsychology, 29(4), 329–347. doi:10.1093/arclin/acu013.
Ling, J. M., Peña, A., Yeo, R. A., Merideth, F. L., Klimaj, S., Gasparovic, C., & Mayer, A. R. (2012). Biomarkers of increased diffusion anisotropy in semi-acute mild traumatic brain injury: a longitudinal perspective. Brain, 135(4), 1281–1292. doi:10.1093/brain/aws073.
Lipton, M. L., Kim, N., Park, Y. K., Hulkower, M. B., Gardin, T. M., Shifteh, K., et al. (2012). Robust detection of traumatic axonal injury in individual mild traumatic brain injury patients: intersubject variation, change over time and bidirectional changes in anisotropy. Brain Imaging and Behavior, 6(2), 329–342. doi:10.1007/s11682-012-9175-2.
Mayer, A. R., Ling, J. M., Yang, Z., Pena, A., Yeo, R. A., & Klimaj, S. (2012). Diffusion abnormalities in pediatric mild traumatic brain injury. The Journal of Neuroscience, 32(50), 17961–17969. doi:10.1523/JNEUROSCI.3379-12.2012.
Mayer, A. R., Bedrick, E. J., Ling, J. M., Toulouse, T., & Dodd, A. (2014). Methods for identifying subject-specific abnormalities in neuroimaging data. Human Brain Mapping, 35(11), 5457–5470. doi:10.1002/hbm.22563.
McMahon, P., Hricik, A., Yue, J. K., Puccio, A. M., Inoue, T., Lingsma, H. F., et al. (2014). Symptomatology and functional outcome in mild traumatic brain injury: results from the prospective TRACK-TBI study. Journal of Neurotrauma, 31(1), 26–33. doi:10.1089/neu.2013.2984
Mild Traumatic Brain Injury Committee of the Head Injury Interdisciplinary Special Interest Group of the American Congress of Rehabilitation Medicine. (1993). Definition of mild traumatic brain injury. The Journal of Head Trauma Rehabilitation, 8(3), 86–87 https://www.acrm.org/wp-content/uploads/pdf/TBIDef_English_10-10.pdf.
Miller, D. R., Hayes, J. P., Lafleche, G., Salat, D. H., & Verfaellie, M. (2016). White matter abnormalities are associated with chronic postconcussion symptoms in blast-related mild traumatic brain injury. Human Brain Mapping, 37(1), 220–229. doi:10.1002/hbm.23022.
Mirzaalian, H., Ning, L., Savadjiev, P., Pasternak, O., Bouix, S., Michailovich, O., et al. (2016). Inter-site and inter-scanner diffusion MRI data harmonization. NeuroImage, 135, 311–323. doi:10.1016/j.neuroimage.2016.04.041.
Morey, R. A., Haswell, C. C., Selgrade, E. S., Massoglia, D., Liu, C., Weiner, J., et al. (2013). Effects of chronic mild traumatic brain injury on white matter integrity in Iraq and Afghanistan war veterans. Human Brain Mapping, 34(11), 2986–2999. doi:10.1002/hbm.22117
Mounce, L. T. A., Williams, W. H., Jones, J. M., Harris, A., Haslam, S. A., & Jetten, J. (2013). Neurogenic and psychogenic acute postconcussion symptoms can be identified after mild traumatic brain injury. The Journal of Head Trauma Rehabilitation, 28(5), 397–405. doi:10.1097/HTR.0b013e318252dd75.
Pierpaoli, C., & Basser, P. J. (1996). Toward a quantitative assessment of diffusion anisotropy. Magnetic Resonance in Medicine, 36(6), 893–906 http://www.ncbi.nlm.nih.gov/pubmed/8946355.
Rytwinski, N. K., Scur, M. D., Feeny, N. C., & Youngstrom, E. A. (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. Journal of Traumatic Stress, 26(3), 299–309. doi:10.1002/jts.21814.
Sartory, G., Cwik, J., Knuppertz, H., Schürholt, B., Lebens, M., Seitz, R. J., & Schulze, R. (2013). In search of the trauma memory: a meta-analysis of functional neuroimaging studies of symptom provocation in posttraumatic stress disorder (PTSD). PloS One, 8(3), e58150. doi:10.1371/journal.pone.0058150.
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., et al. (1998). The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(suppl 20), 1–478 http://www.ncbi.nlm.nih.gov/pubmed/9881538.
Shenton, M. E., Hamoda, H. M., Schneiderman, J. S., Bouix, S., Pasternak, O., Rathi, Y., et al. (2012). A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury. Brain Imaging and Behavior, 6(2), 137–192. doi:10.1007/s11682-012-9156-5.
Smith, S. M., & Nichols, T. E. (2008). Threshold-free cluster enhancement: addressing problems of smoothing, threshold dependence and localisation in cluster inference. NeuroImage, 44(1), 83–98. doi:10.1016/j.neuroimage.2008.03.061.
Smith, S. M., Jenkinson, M., Johansen-Berg, H., Rueckert, D., Nichols, T. E., Mackay, C. E., et al. (2006). Tract-based spatial statistics: voxelwise analysis of multi-subject diffusion data. NeuroImage, 31(4), 1487–1505. doi:10.1016/j.neuroimage.2006.02.024.
Stein, M. B., & McAllister, T. (2009). Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. The American Journal of Psychiatry, 166(7), 768–776. doi:10.1176/appi.ajp.2009.08101604.
Taber, K. H., Hurley, R. A., Haswell, C. C., Rowland, J. A., Hurt, S. D., Lamar, C. D., & Morey, R. A. (2015). White matter compromise in veterans exposed to primary blast forces. The Journal of Head Trauma Rehabilitation, 30(1), E15–E25. doi:10.1097/2FHTR.0000000000000030.
Tsourtos, G., Thompson, J. C., & Stough, C. (2002). Evidence of an early information processing speed deficit in unipolar major depression. Psychological Medicine, 32(2), 259–265 http://www.ncbi.nlm.nih.gov/pubmed/11866321.
Watts, R., Thomas, A., Filippi, C. G., Nickerson, J. P., & Freeman, K. (2014). Potholes and molehills: bias in the diagnostic performance of diffusion-tensor imaging in concussion. Radiology, 272(1), 217–223. doi:10.1148/radiol.14131856.
Wechsler, D. (1997). Wechsler Memory Scale (Third ed.). San Antonio: Psychological Corporation.
White, T., Schmidt, M., & Karatekin, C. (2009). White matter “potholes” in early-onset schizophrenia: a new approach to evaluate white matter microstructure using diffusion tensor imaging. Psychiatry Research: Neuroimaging, 174(2), 110–115. doi:10.1016/j.pscychresns.2009.04.014.
Wrocklage, K. M., Schweinsburg, B. C., Krystal, J. H., Trejo, M., Roy, A., Weisser, V., et al. (2016). Neuropsychological functioning in veterans with posttraumatic stress disorder: associations with performance validity, comorbidities, and functional outcomes. Journal of the International Neuropsychological Society: JINS, 22(4), 399–411. doi:10.1017/S1355617716000059.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted according to the principles expressed in the Declaration of Helsinki and approved by Brigham and Women’s Hospital institutional review board. All participants provided written, informed consent
Funding
CL was supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Doctoral Award, which was awarded in support of his PhD in clinical psychology from the University of Ottawa. The authors would like to acknowledge the following grants that, in part, supported this work: W81XWH-08-2-0159 (Imaging core PI: Shenton, Consortium PI: Stein, Site PIs: George, Grant, Marx, McAllister, and Zafonte).
Conflict of interest
The authors declare they have no conflicts of interest.
Electronic supplementary material
ESM 1
(DOCX 95 kb)
Rights and permissions
About this article
Cite this article
Lepage, C., de Pierrefeu, A., Koerte, I.K. et al. White matter abnormalities in mild traumatic brain injury with and without post-traumatic stress disorder: a subject-specific diffusion tensor imaging study. Brain Imaging and Behavior 12, 870–881 (2018). https://doi.org/10.1007/s11682-017-9744-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-017-9744-5