Abstract
The beta-adrenergic antagonist propranolol benefits some social and communication domains affected in autism spectrum disorder (ASD), and these benefits appear to be associated with increased functional connectivity (FC) in the brain during task performance. FC is implicated in ASD, with the majority of studies suggesting long distance hypo-connectivity combined with regionally specific local hyper-connectivity. The objective in the current investigation was to examine the effect of propranolol on FC at rest and determine whether ASD-specific effects exist. Participants with and without ASD attended three sessions in which propranolol, nadolol (a beta-adrenergic antagonist that does not cross the blood-brain barrier), or placebo were administered. Resting-state fMRI data were acquired, and graph theory techniques were utilized to assess additional aspects of FC. Compared to placebo, propranolol administration was associated with decreased FC in the dorsal medial prefrontal cortex subnetwork of the default mode network and increased FC in the medial temporal lobe subnetwork, regardless of diagnosis. These effects were not seen with nadolol suggesting that the alterations in FC following propranolol administration were not exclusively due to peripheral cardiovascular effects. Thus, beta-adrenergic antagonism can up- or down- regulate FC, depending on the network, and alter coordinated functional activation in the brain. These changes in information processing, as demonstrated by FC, may mediate some of the clinical and behavioral effects of beta-adrenergic antagonism previously reported in patients with ASD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a behaviorally defined disorder characterized by impairments in social communication and the presentation of stereotyped interests and repetitive behaviors early in life (APA 2013). ASD is one of the most common neurodevelopmental disorders with recent estimates suggesting 1 in 68 children in the United States meet diagnostic criteria (CDC 2014). The underlying neuropathology and effects on neuronal activity in ASD are still being elucidated as well as their impact on intervention. As such, current pharmacological treatments are primarily directed at managing secondary manifestations (Myers et al. 2007). Although there is currently no pharmacological intervention for the core symptoms of ASD, the noradrenergic system is implicated in some of these secondary manifestations and may be a salient treatment target for some individuals.
Individuals with ASD often exhibit comorbid diagnoses that are associated with the noradrenergic system, such as attention deficit/hyperactivity disorder (ADHD) (Leyfer et al. 2006) or anxiety (White et al. 2009), as well as secondary symptoms, such as autonomic nervous system dysfunction (Ming et al. 2005). Individuals with ASD also exhibit heightened sympathetic nervous system arousal (Hirstein et al. 2001; Kushki et al. 2013; Ming et al. 2005) and stress reactivity (Corbett et al. 2006; Corbett et al. 2010) as well as potentially higher peripheral levels of norepinephrine (NE) and other stress hormones (Tordjman et al. 1997; Lake et al. 1977). Whereas ASD in general may not be driven by a NE mechanism, these secondary manifestations suggest that targeting the noradrenergic system may provide some clinical benefit. For example, case series studies of beta-adrenergic antagonists in individuals with ASD have reported diminished aggressiveness and improved socialization and communication (Ratey et al. 1987). Single dose psychopharmacological challenge studies have also reported benefits in verbal problem solving (Beversdorf et al. 2008), semantic fluency (Beversdorf et al. 2011), working memory (Bodner et al. 2012), and social reciprocity (Zamzow et al. 2016). These benefits may result from modulation of central nervous system (CNS) mechanisms that alter information processing in the brain.
Increased NE release in the CNS binds lower affinity beta-adrenergic (G-coupled) receptors to alter coordinated functional activation of neuronal clusters in the brain (Berridge and Waterhouse 2003; Sara 2009), or functional connectivity (FC) (Friston 1994), in order to enhance sensory processing. At the neural circuit level, NE enhances sensitivity to the dominant signal (Hasselmo et al. 1997) and suppresses sensitivity to inputs from weaker associative activity (Hasselmo et al. 1997; Alexander et al. 2007; Campbell et al. 2008). These shifts may be beneficial for the flight-or-flight response but could also impair some aspects of cognitive processing by altering bottom-up signal to noise within neuronal clusters (Hasselmo et al. 1997) as well as top-down attentional control from the prefrontal cortex (Arnsten 2009). Conversely, the administration of beta-adrenergic antagonists (i.e., propranolol) modulates FC shifts in the brain following NE release (Hermans et al. 2011), presumably altering information processing by decreasing sensory dominance and allowing increased prefrontal cortex regulation of network activity, which may be particularly beneficial for individuals with ASD.
A general consensus has emerged from studies investigating functional networks in ASD regarding potential global hypo-connectivity between spatially disparate regions and perhaps local hyper-connectivity between anatomically neighboring regions (Kana et al. 2007; Anderson et al. 2010; Just et al. 2007; Wass 2011), suggesting altered information processing in the brain. However, it is important to note that the presence of atypical FC compared to controls differs across studies, which may be due to methodological differences across investigations (Müller et al. 2011). When present, alterations in FC are often associated with clinical manifestations of the disorder (Just et al. 2007), raising the possibility that pharmacological modulation of FC might correspond to a clinical benefit. Within this context, previous research has shown that following administration of beta-adrenergic antagonists, individuals with ASD exhibit increased FC between regions related to semantic and associative processing during an associative processing task (Narayanan et al. 2010). However, the effects of beta-adrenergic antagonism on FC in individuals with ASD have only been investigated regarding task-based connectivity in individuals diagnosed with the disorder. Expanding the investigation into the effects of beta-adrenergic antagonism to resting-state connectivity and including a non-ASD control group will allow assessment of the generality of these effects.
The default mode network (DMN) is of particular interest in the study of resting state fMRI because the DMN is the primary network activated during passive states (Raichle et al. 2000) and dissociates from other networks during cognitive processing tasks (Raichle et al. 2000; Buckner et al. 2008). Additionally, the DMN is believed to be involved with internal mentation such as constructing self-relevant decisions, mental imagery, and future-oriented thought (Buckner et al. 2008). Accordingly, the DMN has received considerable attention in its potential role in dysfunctions associated with psychiatric disorders such as ASD (Broyd et al. 2009). Investigations of resting state FC in individuals with ASD generally report hypoconnectivity between some regions comprising the DMN (Assaf et al. 2010; Cherkassky et al. 2006; Kennedy and Courchesne 2008; Monk et al. 2009; von dem Hagen et al. 2013; Weng et al. 2010; Washington et al. 2014), consistent with previous underconnectivity theories of ASD (Just et al. 2004; Cherkassky et al. 2006); however, increased connectivity between DMN regions (Lynch et al. 2013; Monk et al. 2009) and the DMN and visual and motor networks have also been reported (Washington et al. 2014), suggesting relevant differences depending on the regions being evaluated. Connectivity differences across these reports may be related to functional network structure (topology) of the DMN because the DMN appears to be comprised of multiple subnetworks including a midline core, a dorsal medial prefrontal cortex (dMPFC) subnetwork, and a medial temporal lobe (MTL) subnetwork that exhibit specific patterns of activation based on cognitive demands (Andrews-Hanna et al. 2010). The MTL subnetwork is preferentially activated during episodic future-oriented decision-making (Schacter et al. 2007); whereas the dMPFC subsystem is preferentially activated during evaluation of present mental states (Denny et al. 2012). Our objective in the current investigation was to examine whether beta-adrenergic antagonism differentially impacts FC of the MTL and dMPFC subnetworks of the DMN in individuals with ASD and whether these effects differ compared to typically-developing controls.
Individuals with ASD and matched controls were administered (a) propranolol, a CNS and peripheral nervous system (PNS) beta-adrenergic antagonist; (b) nadolol, a PNS only beta-adrenergic antagonist; and (c) placebo across three separate visits. Nadolol served as a control for the PNS effects of beta-adrenergic antagonism because it does not cross the blood-brain barrier yet yields identical peripheral physiological effects as propranolol. Heart rate and blood pressure were measured to assess the PNS effects of beta-adrenergic antagonism, and resting-state fMRI data were acquired to assess the CNS effects. We hypothesized that individuals with ASD would exhibit significantly lower FC, particularly for the dMPFC subnetwork, compared to unaffected individuals in the placebo condition; however, the MTL subnetwork may exhibit hyperconnectivity due to increased MTL-based processing in some individuals (Lynch et al. 2013). Following propranolol administration, we hypothesized that individuals with ASD would exhibit significantly increased FC, particularly for the dMPFC subnetwork, compared to placebo, and that these changes would be greater than controls. We also hypothesized that individuals with the lowest FC estimates following placebo administration would show the largest changes in FC from propranolol because up-regulation of NE signaling modulates network dynamics and beta-adrenergic antagonism may mitigate these effects allowing greater functional integration of the DMN.
Methods
Participants
Fifteen individuals with ASD, confirmed from clinical report and the Autism Diagnostic Interview-Revised (Le Couteur et al. 2003), with a full-scale IQ (FSIQ) of at least 80 and aged between 15 and 35 years were recruited from the University of Missouri Thompson Center for Autism and Neurodevelopmental Disorders. IQ was estimated with the Wechsler Abbreviated Scale of Intelligence (Wechsler 1999), and demographic information (e.g. ethnicity, years of education, and socio-economic status) were collected with questionnaires. A control sample of 15 healthy individuals without ASD was recruited from the surrounding community. The ASD and control groups were matched for gender, age, FSIQ and handedness. Participants in the control group did not have any previous major medical or psychiatric diagnoses and were not currently taking any psychoactive medications. No subjects were taking drugs affecting the noradrenergic system at the time of assessment. All participants were consented in accordance with the University of Missouri Health Sciences Institutional Review Board.
Drug administration
Participants attended three sessions, counterbalanced for drug order, in which propranolol, nadolol, or placebo were administered orally in a blinded manner. Sessions were separated by at least 24 h. A dose of 40 mg propranolol was administered because this dose was previously shown to be sufficient to benefit cognitive flexibility for those struggling to complete difficult problems (Campbell et al. 2008) and also benefits individuals with ASD during cognitive processing tasks (Beversdorf et al. 2008; Beversdorf et al. 2011; Bodner et al. 2012; Zamzow et al. 2016). Whereas larger doses of either propranolol or nadolol, on average 225 mg, benefit additional clinically-relevant domains such as aggression (Ratey et al. 1987), lower doses appear sufficient to provide general cognitive benefits for high-functioning individuals with ASD. A dose of 50 mg nadolol was administered because it yields similar heart rate and blood pressure changes as 40 mg propranolol (Beversdorf et al. 2002), but does not cross the blood-brain barrier. Drug administration was followed by wait times for peak effects: 60, 90 or 120 min for propranolol, placebo and nadolol, respectively. Heart rate, blood pressure, and self-report anxiety, as assessed by the Beck Anxiety Inventory (BAI) (Beck et al. 1988), were measured before drug administration, at peak effects, and following testing. Difference scores between baseline and each subsequent time point for these measures were computed for further analysis. Researchers were blinded during data processing to participant diagnostic group and treatment condition.
MRI acquisition
Following the proper wait time for peak drug effects, MRI was carried out at the University of Missouri’s Brain Imaging Center utilizing a Siemens 3 T Trio scanner (Siemens, Malvern, PA) and standard 8-channel head coil. Structural T1-weighted 3D MR images were acquired for anatomical localization (MPRAGE, TR = 1920 ms, TE = 2.92 ms, Flip Angle = 9 degrees, FOV = 256 × 256, matrix size = 256 × 256, 1 mm3 resolution with sagittal acquisition) and functional T2*-weighted images were acquired to measure the blood oxygenation level dependent (BOLD) response (EPI, TR = 2200 ms, TE = 30 ms, Flip Angle = 90 degrees, FOV = 256 × 256, matrix size = 64 × 64, 35 ACPC-aligned slices at 4 mm3 resolution) during 5 min of passive rest in which the participant (with eyes open) viewed a blank screen with a cross-hair fixation point.
MRI preprocessing
Preprocessing of fMRI data consisted of slice timing correction, rigid body realignment, intensity normalization, brain extraction, and registration to the structural T1-weighted image with the FMRIB Software Library (FSL) (Jenkinson et al. 2012; Smith et al. 2004). To account for spurious fluctuations in the BOLD response (Fox and Raichle 2007), translation and rotation parameters (x, y, z, pitch, roll, and yaw) from realignment as well as the average BOLD signals from the whole brain, ventricles, white matter, and their temporal derivatives were regressed out of the timeseries data with the REST toolkit (Song et al. 2011). Temporal band-pass filtering (0.01 < f < 0.08 Hz) was also applied. The fMRI data were then motion-corrected as motion can substantially influence FC analyses (Van Dijk et al. 2012; Power et al. 2012) and is of particular importance in the assessment of neurodevelopmental populations. BOLD acquisitions were scrubbed for excess motion and signal intensity using in-house MATLAB programs (The Mathworks, Inc., Natick, MA). Any acquisitions that exceeded two standard deviations from the within-subject within-run mean for any translation, rotation, or intensity parameter or exceeded motion of more than 2 mm in any direction were removed.
Standard space regions of interest (ROIs) from the Automated Anatomical Labeling (AAL) method (Tzourio-Mazoyer et al. 2002) were converted to each participant’s native space, and average timeseries were extracted from each ROI. The use of anatomically-defined regions, in contrast to functionally-defined ROIs, standardizes segmentation of the brain allowing cross-subject comparison and comparison across studies, which is the primary reason the AAL has been commonly utilized in previous investigations (Bullmore and Bassett 2011). Regions comprising the DMN, as defined by Andrews-Hanna et al. (2010), were overlaid with the template to determine the best-approximated corresponding AAL ROIs and are shown in Fig. 1. The dMPFC and MTL subnetworks of the DMN exhibit strong within-network connectivity and weaker between-network connectivity; however, regions comprising both subnetworks exhibit strong connectivity with the midline core. Thus, regions comprising the midline core are affiliated with both subnetworks comprising the DMN and were included in both subnetworks for further analysis.
To account for covariance and allow for assessment of unique FC, partial correlation matrices containing all possible ROI pairs were generated for each participant and each condition, and then transformed with Fischer’s r-to-z. Self-connections were removed and negative correlations were set to zero. Negative correlations were removed from further analysis because false negative correlations may be introduced by removal of the global signal during preprocessing (Van Dijk et al. 2010; Weissenbacher et al. 2009).
Graph theory analyses
Graph theory techniques were also utilized to assess additional properties of functional networks in the brain. A graph is a mathematical representation of a network and consists of a set of nodes, ROIs, and a set of edges (i.e., functional connections between nodes). Graph theory has been applied previously to assess networks in the brain and allows comparison between normal and pathological states (Guye et al. 2010). Most importantly, graph theory provides an assessment of different aspects of functional networks, such as network topology (Bullmore and Sporns 2009), expanding on previous FC investigations in ASD. For example, lower local and higher global efficiency have been previously reported in individuals with ASD (Rudie et al. 2013), suggesting altered functional network dynamics beyond just strength of coordinated activation.
Weighted partial correlation matrices were utilized and each matrix cell was divided by the mean across all cells in order to standardize the matrix and control for the effects of FC magnitude differences across participants and drug conditions. Graph metrics that were calculated using the Brain Connectivity Toolbox (Rubinov and Sporns 2010) are shown in Table 1. Clustering coefficient (C) and local efficiency (Elocal) are metrics that assess aspects of local network processing by examining the efficiency with which information can pass through clusters within the network based on the number of shared connections between ROIs. Characteristic path length (L) and global efficiency (Eglobal) are metrics that assess aspects of global network processing by examining the efficiency with which information can pass through the entire network based on the shortest possible paths between ROIs.
Statistical analyses
One ASD participant was unable to complete the study due to an adverse reaction to the imaging environment (anxiety) and one additional ASD participant was removed following motion correction. These subjects’ matched controls were subsequently removed, and statistical analyses were conducted on the remaining sample of 13 individuals with ASD and 13 individually matched controls. The effect of beta-adrenergic antagonism on the PNS (heart rate and blood pressure) was first assessed with one-sample t-tests comparing the difference from baseline to peak effects to determine whether participants exhibited a significant physiological response following drug administration. Diagnostic group and drug condition comparisons were then conducted. Analyses included: (1) a one-way ANOVA between groups for continuous demographic variables (age, IQ, and years of education) and a χ2 (chi-squared) for categorical demographic variables (gender, ethnicity, handedness, and family income), (2) a 2 × 3 repeated measures MANOVA between diagnostic groups and within drug conditions for the difference from baseline to peak effect and ending time points for cardiovascular and anxiety measures [heart rate, blood pressure (systolic and diastolic), and BAI], and (3) a set of six (one for the whole brain, one for the bilateral DMN, and one each for the right and left lateralized dMPFC and MTL subnetworks) 2 × 3 repeated measures MANOVAs between groups and within drug conditions for mean FC and graph metrics (C, L, Eglobal, Elocal). Although groups were matched for age, cortical development could affect drug response. Thus, alterations in FC were also examined for potential influences of age by splitting individuals into younger (≤ 21) and older (> 21) groups and assessing potential drug x age group interactions.
Analyses were carried out with IBM SPSS Statistics Software (IBM 2013). Due to the small sample size and pilot nature of this investigation, correction for multiple comparisons was only completed across drug conditions, which may increase Type I error but will allow hypothesis generation for future investigations. Follow-up paired samples t-tests or independent samples t-tests were conducted when significance was indicated at the univariate level, and correction for multiple comparisons was completed across drug conditions by controlling for the false discovery rate (FDR) (Benjamini and Hochberg 1995).
Results
Participants
Table 2 illustrates that the ASD and control groups did not significantly differ in age, estimated FSIQ, estimated performance IQ, years of education, gender, ethnicity, handedness or family income, p > 0.05 in all instances. Group differences in estimated verbal IQ (VIQ) approached significance, p = 0.06, as individuals with ASD exhibited lower VIQ on average. (Note that the samples were matched on overall IQ, with the exception of one ASD participant with low average IQ who was matched to a control participant within the average IQ range.)
Cardiovascular and anxiety measures
Cardiovascular and anxiety measure difference scores significantly differed within-subject across drug conditions at the omnibus level due to heart rate changing from baseline to the peak drug effect time point, F(2,48) = 7.00, p = 0.002, η p 2 = 0.23. Heart rate (beats per minute) significantly decreased during placebo (M = −7.85, SD = 9.00), t(25) = 4.45, p < 0.001, d = 1.78, nadolol (M = −16.77, SD = 11.89), t(25) = 7.19, p < 0.001, d = 2.88, and propranolol administration (M = −12.54, SD = 11.17), t(25) = 5.72, p < 0.001 d = 2.29; but decreased significantly more during nadolol compared to placebo, t(25) = 3.70, p = 0.001, g = 0.83, and exhibited a trend towards a greater reduction during propranolol compared to placebo, t(25) = 1.87, p = 0.07, g = 0.46. Thus, there was a significant physiological effect of beta-adrenergic antagonism. The decrease in heart rate after placebo administration was most likely due to the period of quiet rest used to control for wait time effects, as has been previously observed (Beversdorf et al. 2008). Self-reported anxiety did not significantly differ across drug conditions, F(2,48) = 2.05, p = 0.14, or diagnostic groups, F(1,24) = 3.160, p = 0.088, nor did it exhibit a significant drug by group interaction, F(2,48) = 0.417, p = 0.661. The absence of a significant drug-related change in anxiety assessments may have been due to insufficient sensitivity of self-report within the time domain of assessment or difficulty individuals with ASD typically exhibit with self-report of emotional introspection (Hill et al. 2004).
Functional connectivity
Functional connectivity was assessed with average FC as well as graph metric measures to assess global (L, Eglobal) and local (C, Elocal) network processing. Graph metrics at the whole-brain and bilateral DMN levels, respectively, did not significantly differ across drug conditions, F(10,15) = 0.81, p = 0.62, F(10,15) = 0.33, p = 0.96, or diagnostic group, F(5,20) = 0.51, p = 0.77, F(5,20) = 0.76, p = 0.59; and there was no diagnostic group by drug interaction observed, F(10,15) = 0.82, p = 0.62, F(10,90) = 1.03, p = 0.47.
DMPFC subnetwork
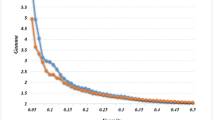
Although there were no observable drug effects at the global level, beta-adrenergic antagonism appeared to alter FC in the DMN subnetworks. There was a strong trend towards a main effect of drug in the left dMPFC subnetwork on FC, F(2,48) = 3.01, p = 0.06, η p 2 = 0.11, and Eglobal, F(2,48) = 3.04, p = 0.06, η p 2 = 0.11. As shown in Fig. 2, FC was significantly lower during propranolol administration (M = 0.21, SD = 0.07) compared to placebo (M = 0.26, SD = 0.07), t(25) = 2.50, p = 0.02, g = 0.70. The difference between propranolol and nadolol (M = 0.25, SD = 0.06) did not reach significance, t(25) = 1.72, p = 0.10, g = 0.60, and there was no difference between placebo and nadolol, t(25) = 0.65, p = 0.52, g = 0.15.
Beta-adrenergic antagonism effects on the DMN during resting state. Average functional connectivity of the dorsal medial prefrontal cortex (dMPFC) and medial temporal lobe (MTL) subnetworks are displayed for the left (dark grey) and right (light grey) hemispheres across placebo, propranolol, and nadolol conditions for all participants regardless of diagnostic group. Error bars represent standard error and significant differences are indicated with (**) and without (*) correction for multiple comparisons
Eglobal was significantly higher during propranolol administration (M = 0.89, SD = 0.12) compared to nadolol (M = 0.82, SD = 0.13), t(25) = 3.18, p = 0.004, g = 0.55, suggesting an increase in the efficiency of information processing across the entire subnetwork; however, there was no difference between propranolol and placebo (M = 0.85, SD = 0.13), t(25) = 1.43, p = 0.17, g = 0.32, nor between nadolol and placebo, t(25) = 0.84, p = 0.41, g = 0.23. As shown in Fig. 3 (A), a greater decrease in FC following propranolol administration was significantly associated with higher baseline FC, as determined by measurement during placebo administration, regardless of diagnostic group, r = −0.65, p < 0.001. Additionally, there was no significant drug x age group interaction comparing propranolol and placebo, F(1,24) = 0.18, p = 0.671, but there was a significant interaction comparing propranolol and nadolol, F(1,24) = 9.06, p = 0.006, which appeared to be due to significantly lower FC during propranolol administration (M = 0.19, SD = 0.06) compared to nadolol in the older group (M = 0.27, SD = 0.06), t(12) = 3.26, p = 0.007, but not in the younger group, t(12) = 0.60, p = 0.557.
The association between baseline FC and change in FC following propranolol administration. Functional connectivity of the (a) dorsal medial prefrontal cortex (dMPFC) subnetwork and (b) medial temporal lobe (MTL) subnetwork are displayed in relation to the change in FC following propranolol administration for individuals with ASD, dark grey diamonds, and controls (CTRL), light grey circles. Correlations are displayed separately for individuals with ASD (solid line) and controls (dashed line) and significant correlations are indicated (*)
FC and graph metrics of interest did not significantly differ between diagnostic groups, F(5,20) = 0.36, p = 0.87, and drug effects did not significantly change based on ASD diagnosis, as evidenced by a lack of a significant drug by diagnostic group interaction, F(10,15) = 0.35, p = 0.95. There was no significant effect of drug condition, group, or drug condition by diagnostic group interaction in FC or graph metrics for the right dMPFC subnetwork (F < 1.05, p > 0.45, in all instances).
MTL subnetwork
Measures of FC within the left MTL subnetwork of the DMN exhibited a trend towards a main effect of drug, F(2,48) = 2.60, p = 0.08, η p 2 = 0.10. As shown in Fig. 2, there was a significant increase in FC during propranolol administration (M = 0.31, SD = 0.09) compared to placebo (M = 0.26, SD = 0.08), t(25) = 2.56, p = 0.017, g = 0.58; but no difference between propranolol and nadolol (M = 0.28, SD = 0.07), t(25) = 1.11, p = 0.28, g = 0.37, or between placebo and nadolol, t(25) = 1.11, p = 0.28, g = 0.26. As can be seen in Fig. 3 (B), a greater increase in FC following propranolol administration was significantly associated with lower baseline FC, as measured during placebo administration, regardless of diagnostic group, r = −0.58, p = 0.002. Additionally, there were no significant drug x age group interactions comparing propranolol and placebo, F(1,24) = 0.88, p = 0.358, or propranolol and nadolol, F(1,24) = 0.28, p = 0.602.
FC and graph metrics of interest did not significantly differ between diagnostic groups, F(5,20) = 1.20, p = 0.35, and drug effects did not significantly change based on ASD diagnosis, as there was no significant drug by diagnostic group interaction F(10,15) = 0.79, p = 0.64. There were also no significant changes in FC or graph metrics of the right MTL subnetwork across drug conditions, F(10,15) = 1.09, p = 0.43, or diagnostic groups, F(5,20) = 0.37, p = 0.86. There was a significant drug by diagnostic group interaction at the omnibus level F(10,15) = 2.62, p = 0.05, η p 2 = 0.64; however, none remained significant at the univariate level, F(2,48) < 1.5, p > 0.05, in all instances.
Discussion
The effects of beta-adrenergic antagonism on FC in individuals with ASD was previously examined during an associative processing task, and propranolol administration was found to increase FC in brain networks underlying this cognitive processing domain (Narayanan et al. 2010). The purpose of the present study was to extend the investigation of beta-adrenergic antagonism effects on FC in individuals with ASD to additional networks implicated in the disorder during resting state fMRI and examine whether there are ASD-specific alterations. Following beta-adrenergic antagonism, FC in the DMN was altered regardless of diagnosis (ASD or non-ASD) and yielded some relevant and contrasting results, depending on the subnetwork. Relative to placebo, propranolol (a lipophilic beta-adrenergic antagonist that crosses the blood brain barrier) was associated with decreased FC in the dMPFC subnetwork and increased FC in the MTL subnetwork. Additionally, individuals with low baseline FC (especially in the MTL subnetwork) typically exhibited an increase in FC following propranolol administration whereas individuals with high baseline FC (especially in the dMPFC subnetwork) typically exhibited a decrease, suggesting that beta-adrenergic antagonism could potentially help maintain FC patterns in the brain. Thus, beta-adrenergic antagonism appears to modulate FC in resting-state networks of individuals with and without ASD.
Beta-adrenergic antagonism in the CNS alters coordinated functional activation between regions in the brain, which is especially relevant considering that NE release in the CNS typically enhances sensitivity to dominant sensory signals (Hasselmo et al. 1997) by down-regulating networks underlying cognitive processing in favor of networks that prompt environmental adaptation (Aston-Jones and Cohen 2005; Valentino and Van Bockstaele 2008; Sara 2009). Within this context, subfield-specific projections from neurons in the locus coeruleus (LC), which are the primary source of NE in the brain, likely contributed to the effects of propranolol on the subnetworks of the DMN. Medial regions of the prefrontal cortex, such as the dMPFC and anterior cingulate cortex, receive dense innervation from the LC (Radley et al. 2008); whereas more lateral regions such as those involved in higher-order cognitive processing (e.g., the dorsal lateral prefrontal cortex) receive less dense innervation. Thus, decreased FC in the dMPFC subnetwork may be due to a shift in prefrontal cortex activation following down-regulation of LC influences. Additionally, the hippocampus has particularly high concentrations of beta-adrenergic receptors (Reznikoff et al. 1986), which typically facilitate memory formation of salient stimuli during stress. Increased FC in the MTL subnetwork following beta-adrenergic antagonism may be due to a shift of MTL regions away from salience based networks and back towards the DMN. Overall, beta-adrenergic antagonism could potentially support cognitive processing by down-regulating the priming effects of NE release on networks underlying attention-shifting and sensory processing and allowing increased associative processing through greater integration within cognitive networks. However, the effects of pharmacologically-mediated shifts in FC of the DMN on cognition have yet to be determined. Further research is necessary to determine how propranolol affects FC in task-related networks during cognitive processing in order to more directly examine the influence of pharmacologically-mediated changes in FC on cognition and behavior.
Although not specific to autism, beta-adrenergic modulation of FC may particularly benefit some individuals with ASD. As previously mentioned, individuals with ASD may exhibit patterns of hypoconnectivity in the DMN (Assaf et al. 2010; Cherkassky et al. 2006; Kennedy and Courchesne 2008; Monk et al. 2009; von dem Hagen et al. 2013; Weng et al. 2010; Washington et al. 2014); however, hyperconnectivity between DMN regions (Lynch et al. 2013; Monk et al. 2009) and no alterations in FC between some DMN regions (Assaf et al. 2010; Kennedy and Courchesne 2008; Monk et al. 2009; von dem Hagen et al. 2013) have also been reported, such as in this sample, suggesting relevant differences across regions and individuals. Nonetheless, it appears that the effects of beta-adrenergic antagonism on subnetworks of the DMN have the potential to mitigate hypo- or hyper- connectivity in some individuals, such as those with low or high baseline FC, and potentially allow increased segregation between subnetworks. This may be particularly relevant for individuals with ASD considering reports of reduced integration within networks and less segregation between networks in the brain (Rudie et al. 2013; Washington et al. 2014) as well as the potential role of DMN in some cognitive domains (Andrews-Hanna et al. 2010) affected in the disorder, such as prospective thought, introspective thought, and Theory of Mind (Lind and Bowler 2010; Graziano and Derefinko 2013; Baron-Cohen 2001). For example, the role of the MTL subnetwork in future-oriented decision-making (Schacter et al. 2007) suggests beta-adrenergic antagonism could potentially allow increased evaluation of future behavior. Additionally, the effects of beta-adrenergic antagonism were localized primarily to the left hemisphere, which potentially supports benefits to language and communication as well as the processing of some social information (Ross et al. 1994; Gotts et al. 2013). Social and communication deficits are core symptoms of ASD, and previous reports have already shown that language-related networks are affected following propranolol administration (Narayanan et al. 2010). Furthermore, individuals with ASD may exhibit a pervasive rightward shift in functional networks associated with multiple cognitive domains (Cardinale et al. 2013), suggesting pharmacologically-mediated alteration of FC in the left hemisphere may potentially be associated with additional cognitive benefits in individuals with ASD.
Limitations
Due to the preliminary nature of our investigation, our sample size was limited, particularly for the comparisons between diagnostic groups. Additionally, the wait time for drug effects allowed heart rate to significantly decrease during the placebo condition compared to baseline. However, the within-subject design allowed us to account for additional individual variation in imaging data and detect differences between drug conditions, which supports our findings that beta-adrenergic antagonism can alter FC in the brain. It is also important to note that although the general lack of differences between propranolol and nadolol suggests that peripheral effects may have contributed to the observed alterations in FC, the lack of differences between nadolol and placebo supports that these alterations were not exclusively due to PNS effects on the BOLD signal. Furthermore, alterations in network efficiency emerged when comparing propranolol and nadolol and the older subjects in this sample exhibited significant FC differences between propranolol and nadolol, further supporting that beta-adrenergic modulation of FC acts (at least partially) through CNS mechanisms. It is of interest that the effects of beta-adrenergic antagonism on FC may differ depending on age, especially in the frontal cortex; however, additional research will be necessary to examine potential developmental differences in drug response.
Based on the literature, we had hypothesized that individuals with ASD would exhibit general hypoconnectivity within the DMN and potential hyperconnectivity within the MTL subnetwork compared to unaffected individuals. Considering the region-specific differences in the DMN in ASD and the network-level approach that we applied (i.e., averaging across subnetwork ROIs), it is not entirely surprising that there were no significant baseline differences in FC within our sample. Additionally, the anatomically-defined ROIs utilized in this investigation may have been comprised of multiple functional subunits diluting the ability to assess domain-specific functional clusters. The possible domain specific roles of the DMN subnetworks also suggest that dynamic changes in subnetwork integration could potentially reflect a shift from introspective to prospective contemplation (Andrews-Hanna et al. 2010); however directed investigations into the effects of beta-adrenergic antagonism on internal mentation would be necessary to elucidate the effects of these shifts. The evaluation of mental-state inference performance and FC of the dMPFC subnetwork following propranolol administration would be of particular interest.
Summary
Beta-adrenergic antagonism was previously shown to benefit cognitive processing in individuals with ASD, especially in verbal domains, and increase FC in functional networks associated with verbal processing during task performance. Our findings suggest that the effect of propranolol on FC is more complex than increased FC in individuals with ASD, at least at rest. Beta-adrenergic antagonism may be able to up- or down- regulate specific subnetworks in the brain, such as the DMN, regardless of ASD diagnosis and allow increased integration within functional networks. Thus, pharmacological modulation of coordinated functional activation allowing more efficient information processing may underlie the aforementioned propranolol-mediated benefits to cognitive processing; however, the assessment of FC during cognitive processing tasks, while monitoring performance, will be necessary to further elucidate the effects of beta-adrenergic mediated changes in FC on cognitive outcomes and to further explore individual differences in response. In addition to the aforementioned cognitive and behavioral benefits of propranolol and effects on FC, propranolol also typically has anxiolytic effects and influences the autonomic nervous system, which is particularly relevant for individuals with ASD. Cumulatively, these findings support continued investigation into the effects of beta-adrenergic antagonists on FC in the brain, especially for individuals with ASD.
References
Alexander, J. K., Hillier, A., Smith, R. M., Tivarus, M. E., & Beversdorf, D. Q. (2007). Beta-adrenergic modulation of cognitive flexibility during stress. Journal of Cognitive Neuroscience, 19(3), 468–478.
Anderson, J. S., Druzgal, T. J., Froehlich, A., DuBray, M. B., Lange, N., Alexander, A. L., et al. (2010). Decreased interhemispheric functional connectivity in autism. Cerebral Cortex, 21, 1134–1146.
Andrews-Hanna, J. R., Reidler, J. S., Sepulcre, J., Poulin, R., & Buckner, R. L. (2010). Functional-anatomic fractionation of the brain's default network. Neuron, 65, 550–562.
APA (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-V. VA: Arlington.
Arnsten, A. F. T. (2009). Stress signalling pathways that impair prefrontal cortex structure and function. [10.1038/nrn2648. Nature Reviews. Neuroscience, 10(6), 410–422.
Assaf, M., Jagannathan, K., Calhoun, V. D., Miller, L., Stevens, M. C., Sahl, R., et al. (2010). Abnormal functional connectivity of default mode sub-networks in autism spectrum disorder patients. NeuroImage, 53, 247–256.
Aston-Jones, G., & Cohen, J. D. (2005). An integrative theory of locus coeruleus-norepinephrine function: adaptive gain and optimal performance. Annual Review of Neuroscience, 28, 403–450.
Baron-Cohen, S. (2001). Theory of mind and autism: a review. International review of research in mental retardation, 23, 169–184.
Beck, A. T., Epstein, N., Brown, G., & Steer, R. A. (1988). An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57(1), 289–300.
Berridge, C. W., & Waterhouse, B. D. (2003). The locus coeruleus-noradrenergic system: Modulation of behavioral state and state-dependent cognitive processes. Brain Research Reviews, 42, 33–84.
Beversdorf, D. Q., White, D. M., Chever, D. C., Hughes, J. D., & Bornstein, R. A. (2002). Central beta-adrenergic modulation of cognitive flexibility. Neuroreport, 13(18), 2505–2507.
Beversdorf, D. Q., Carpenter, A. L., Miller, R. F., Cios, J. S., & Hillier, A. (2008). Effect of propranolol on verbal problem solving in autism spectrum disorder. Neurocase, 14(4), 378–383.
Beversdorf, D. Q., Saklayen, S., Higgins, K. F., Bodner, K. E., Kanne, S. M., & Christ, S. E. (2011). Effect of propranolol on word fluency in autism. Cognitive and Behavioral Neurology, 24(1), 11–17.
Bodner, K. E., Beversdorf, D. Q., Saklayen, S. S., & Christ, S. E. (2012). Noradrenergic moderation of working memory impairments in adults with autism spectrum disorder. Journal of the International Neuropsychological Society, 18(03), 556–564.
Broyd, S. J., Demanuele, C., Debener, S., Helps, S. K., James, C. J., & Sonuga-Barke, E. J. S. (2009). Default-mode brain dysfunction in mental disorders: A systematic review. Neuroscience & Biobehavioral Reviews, 33, 279–296.
Buckner, R. L., Andrews-Hanna, J. R., & Schacter, D. L. (2008). The brain's default network: Anatomy, function, and relevance to disease. Ann. N.Y. Acad. Science, 1124, 1–38.
Bullmore, E., & Sporns, O. (2009). Complex brain networks: graph theoretical analysis of structural and functional systems. [10.1038/nrn2575]. Nature Reviews. Neuroscience, 10(3), 186–198.
Bullmore, E. T., & Bassett, D. S. (2011) Brain graphs: graphical models of the human brain connectome. Annual Review of Clinical Psychology, 7(1), 113–140
Campbell, H. L., Tivarus, M. E., Hillier, A., & Beversdorf, D. Q. (2008). Increased task difficulty results in greater impact of noradrenergic modulation of cognitive flexibility. Pharmacology Biochemistry Behavior, 88(3), 222–229.
Cardinale, R. C., Shih, P., Fishman, I., Ford, L. M., & Müller, R. (2013). PErvasive rightward asymmetry shifts of functional networks in autism spectrum disorder. JAMA Psychiatry, 70(9), 975–982.
CDC (2014). Prevalence of autism spectrum disorders among children aged 8 years: autism and developmental disabilities monitoring network, 11 sites, United States, 2010. (Vol. 63, pp. 1–22). MMWR Surveillance Summaries.
Cherkassky, V. L., Kana, R. K., Keller, T. A., & Just, M. A. (2006). Functional connectivity in a baseline resting-state network in autism. Neuroreport, 17(16), 1687–1690.
Corbett, B., Mendoza, S., Abdullah, M., Wegelin, J. A., & Levine, S. (2006). Cortisol circadian rhythms and response to stress in children with autism. Psychoneuroendocrinology, 31(1), 59–68.
Corbett, B., Schupp, C., Simon, D., Ryan, N., & Mendoza, S. (2010). Elevated cortisol during play is associated with age and social engagement in children with autism. Molecular Autism, 1(1), 13.
Denny, B. T., Kober, H., Wager, T. D., & Ochsner, K. N. (2012). A Meta-analysis of Functional Neuroimaging Studies of Self- and Other Judgments Reveals a Spatial Gradient for Mentalizing in Medial Prefrontal Cortex. Journal of Cognitive Neuroscience, 24(8), 1742–1752.
Fox, M. D., & Raichle, M. E. (2007). Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nature Reviews, 8, 700–711.
Friston, K. J. (1994). Functional and effective connectivity in neuroimaging: a synthesis. Human Brain Mapping, 2, 56–78.
Gotts, S. J., Jo, H. J., Wallace, G. L., Saad, Z. S., Cox, R. W., & Martin, A. (2013). Two distinct forms of functional lateralization in the human brain. Proceedings of the National Academy of Sciences, 110(36), E3435–E3444.
Graziano, P., & Derefinko, K. (2013). Cardiac vagal control and children's adaptive functioning: a meta-analysis. Biological Psychology, 94(1), 22–37.
Guye, M., Bettus, G., Bartolomei, F., & Cozzone, P. J. (2010). Graph theoretical analysis of structural and functional connectivity MRI in normal and pathological brain networks. Magnetic Resonance Materials in Physics, 23, 409–421.
Hasselmo, M. E., Linster, C., Patil, M., Ma, D. & Cekic, M. (1997). Noradrenergic suppression of synaptic transmission may influence cortical signal-to-noise. Journal of Neurophysiology, 77(6), 3326–3339.
Hermans, E. J., van Marle, H. J. F., Ossewaarde, L., Henckens, M. J. A. G., Qin, S., van Kesteren, M. T. R., et al. (2011). Stress-related noradrenergic activity prompts large-scale neural network reconfiguration. [10.1126/science.1209603. Science, 334(6059), 1151–1153.
Hill, E., Berthoz, S., & Frith, U. (2004) Brief report: cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. Journal of Autism and Developmental Disorders, 34(2), 229–235
Hirstein, W., Iversen, P., & Ramachandran, V. S. (2001). Autonomic responses of autistic children to people and objects. Proceedings of the Royal Society of London. Series B: Biological Sciences, 268(1479), 1883–1888.
IBM (2013). IBM SPSS Statistics for Macintosh (22 ed.). Armonk, NY: IBM Corp.
Jenkinson, M., Beckman, C. F., Behrens, T. E., Woolrich, M. W., & Smith, S. M. (2012). FSL. NeuroImage, 62, 782–790.
Just, M. A., Cherkassky, V. L., Keller, T. A., & Minshew, N. J. (2004). Cortical activation and synchronization during sentence comprehension in high-functioning autism: evidence of underconnectivity. [10.1093/brain/awh199]. Brain, 127(8), 1811–1821.
Just, M. A., Cherkassky, V. L., Keller, T. A., Kana, R. K., & Minshew, N. J. (2007). Functional and Anatomical Cortical Underconnectivity in Autism: Evidence from an fMRI Study of an Executive Function Task and Corpus Callosum Morphometry. Cerebral Cortex, 17(4), 951–961.
Kana, R. K., Keller, T. A., Minshew, N. J., & Just, M. A. (2007). Inhibitory control in high-functioning autism: decreased activation and underconnectivity in inhibition networks. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't]. Biological Psychiatry, 62(3), 198–206.
Kennedy, D. P., & Courchesne, E. (2008). The intrinsic functinal organization of the brain is altered in autism. NeuroImage, 39(4), 1877–1885.
Kushki, A., Drumm, E., Mobarak, M., Tanel, N., Dupuis, A., Chau, T., et al. (2013). Investigating the autonomic nervous system response to anxiety in children with autism spectrum disorders. PloS One, 8(4), 59730.
Lake, C., Ziegler, M. G., & Murphy, D. L. (1977). Increased norepinephrine levels and decreased dopamine-β-hydroxylase activity in primary autism. Archives of General Psychiatry, 34(5), 553–556.
Le Couteur, A., Lord, C., & Rutter, M. (2003). The autism diagnostic interview-revised (ADI-R). Los Angeles, CA: Western Psychological Services.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36, 849–861.
Lind, S. E., & Bowler, D. M. (2010). Episodic memory and episodic future thinking in adults with autism. Journal of Abnormal Psychology, 119(4), 896.
Lynch, C. J., Uddin, L. Q., Supekar, K., Khouzam, A., Phillips, J., & Menon, V. (2013). Default Mode Network in Childhood Autism: Posteromedial Cortex Heterogeneity and Relationship with Social Deficits. Biological Psychiatry, 74(3), 212–219.
Ming, X., Julu, P., Brimacombe, M., Connor, S., & Daniels, M. (2005). Reduced cardiac parasympathetic activity in children with autism. Brain Dev, 27(7), 509–516.
Monk, C. S., Peltier, S. J., Wiggins, J. L., Weng, S.-J., Carrasco, M., Risi, S., et al. (2009). Abnormalities of intrinsic functional connectivity in autism spectrum disorders. NeuroImage, 47(2), 764–772.
Müller, R. A., Shih, P., Keehn, B., Deyoe, J. R., Leyden, K. M., & Shukla, D. K. (2011). Underconnected, but how? A survey of functional connectivity MRI studies in autism spectrum disorders. Cerebral Cortex, 21(10), 2233–2243.
Myers, S. M., Johnson, C. P., & Disabilities, t. C. o. C. W. (2007). Management of Children With Autism Spectrum Disorders. Pediatrics, 120(5), 1162–1182.
Narayanan, A., White, C., Saklayen, S., Scaduto, M., Carpenter, A., Abduljalil, A., et al. (2010). Effect of propranolol on functional connectivity in autism Spectrum disorder—a pilot study. Brain Imaging and Behavior, 4(2), 189–197.
Power, J. D., Barnes, K. A., Synder, A. Z., Schlaggar, B. L., & Petersen, S. E. (2012). Spurious but systematic correlations in functional connectivty MRI networks arise from subject motion. NeuroImage, 59(3), 2142–2154.
Radley, J. J., Williams, B., & Sawchenko, P. E. (2008). Noradrenergic innervation of the dorsal medial prefrontal cortex modulates hypothalamo-pituitary-adrenal responses to acute emotional stress. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 28(22), 5806–5816.
Raichle, M. E., MacLeod, A. M., Snyder, A. Z., Powers, W. J., Gusnard, D. A., & Shulman, G. L. (2000). A default mode of brain function. PNAS, 98(2), 676–682.
Ratey, J., Bemporad, J., Sorgi, P., Bick, P., Polakoff, S., O'Driscoll, G., et al. (1987). Brief report: open trial effects of beta-blockers on speech and social behaviors in 8 autistic adults. Journal of Autism and Developmental Disorders, 17(3), 439–446.
Reznikoff, G. A., Manaker, S., Rhodes, C. H., Winokur, A., & Rainbow, T. C. (1986). Localization and quantification of beta-adrenergic receptors in human brain. Neurology, 36(8), 1067–1067.
Ross, E. D., Homan, R. W., & Buck, R. (1994). Differential hemispheric lateralization of primary and social emotions implications for developing a comprehensive neurology for emotions, repression, and the subconscious. Cognitive and Behavioral Neurology, 7, 1–19.
Rubinov, M., & Sporns, O. (2010). Complex network measures of brain connectivity: uses and interpretations. [Research Support, Non-U.S. Gov't]. NeuroImage, 52(3), 1059–1069.
Rudie, J. D., Brown, J. A., Beck-Pancer, D., Hernandez, L. M., Dennis, E. L., Thompson, P. M., et al. (2013). Altered functional and structural brain network organization in autism. NeuroImage: Clinical, 2(0), 79–94.
Sara, S. J. (2009). The locus coeruleus and noradrenergic modulation of cognition. [10.1038/nrn2573. Nature Reviews. Neuroscience, 10(3), 211–223.
Schacter, D. L., Addis, D. R., & Buckner, R. L. (2007). Remembering the past to imagine the future: the prospective brain. [10.1038/nrn2213]. Nature Reviews. Neuroscience, 8(9), 657–661.
Smith, S. M., Jenkinson, M., Woolrich, M. W., Beckman, C. F., Behrens, T. E., Johansen-Berg, H., et al. (2004). Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage, 23(Supplement 1), S208-S219.
Song, X.-W., Dong, Z.-Y., Long, X.-Y., Li, S.-F., Zuo, X.-N., Zhu, C.-Z., et al. (2011). REST: A toolkit for resting-state functional magnetic resonance imaging data processing. PloS One, 6(9), E25031.
Tordjman, S., McBride, P. A., Hertzig, M. E., Snow, M. E., Anderson, G. M., Hall, L. M., et al. (1997). Plasma β-endorphin, Adrenocorticotropin hormone, and cortisol in autism. Journal of Child Psychology and Psychiatry, 38(6), 705–715.
Tzourio-Mazoyer, N., Landeau, B., Papathanassiou, D., Crivello, F., Etard, O., Delcroix, N., et al. (2002). Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage, 15(1), 273–289.
von dem Hagen, E. A. H., Stoyanova, R. S., Baron-Cohen, S., & Calder, A. J. (2013). Reduced functional connectivity within and between 'social' resting state networks in autism spectrum conditions. SCAN, 8, 694–701.
Valentino, R. J., & Van Bockstaele, E. (2008). Convergent regulation of locus coeruleus activity as an adaptive response to stress. European Journal of Pharmacology, 583(2–3), 194–203.
Van Dijk, K. R. A., Hedden, T., Venkataraman, A., Evans, K. C., Lazar, S. W., & Buckner, R. L. (2010). Intrinsic functional connectivity as a tool for human connectomics: Theory, properties, and optimization. Journal of Neurophysiology, 103(1), 297–321.
Van Dijk, K. R. A., Sabuncu, M. R., & Buckner, R. L. (2012). The influence of head motion on intrinsic functional connectivity MRI. NeuroImage, 59(2), 431–438.
Washington, S. D., Gordon, E. M., Brar, J., Warburton, S., Sawyer, A. T., Wolfe, A., et al. (2014). Dysmaturation of the default mode network in autism. Human Brain Mapping, 35(4), 1284–1296.
Wass, S. (2011). Distortions and disconnections: disrupted brain connectivity in autism. Brain and Cognition, 75(1), 18–28.
Wechsler, D. (1999). WASI manual. San Antonio: Psychological Corporation.
Weissenbacher, A., Kasess, C., Gerstl, F., Lanzenberger, R., Moser, E., & Windischberger, C. (2009). Correlations and anticorrelations in resting-state functional connectivity MRI: A quantitative comparison of preprocessing strategies. NeuroImage, 47, 1408–1416.
Weng, S.-J., Wiggins, J. L., Peltier, S. J., Carrasco, M., Risi, S., Lord, C., et al. (2010). Alterations of resting state functional connectivity in the default network in adolescents with autism spectrum disorders. Brain Research, 1313(0), 202–214.
White, S. W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229.
Zamzow, R. M., Ferguson, B. J., Stichter, J. P., Porges, E. C., Ragsdale, A. S., Lewis, M. L., et al. (2016) Effects of propranolol on conversational reciprocity in autism spectrum disorder: a pilot, double-blind, single-dose psychopharmacological challenge study. Psychopharmacology, 233(7), 1171–1178
Acknowledgments
We would like to thank all of the individuals and their families that participated in this investigation as well as the faculty and staff at the University of Missouri Brain Imaging Center, Thompson Center for Autism and Neurodevelopmental Disorders, and School of Medicine that were involved in this work. This project was supported by a grant from the Health Resources and Services Administration (1R40MC19926) and the University of Missouri, School of Medicine Mission Enhancement Fund awarded to David Q. Beversdorf.
Disclosures
John P. Hegarty II, Bradley J. Ferguson, Rachel M. Zamzow, Landon J. Rohowetz, Jeffrey D. Johnson, Shawn E. Christ, and David Q. Beversdorf declare that they have no conflict of interest. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hegarty, J.P., Ferguson, B.J., Zamzow, R.M. et al. Beta-adrenergic antagonism modulates functional connectivity in the default mode network of individuals with and without autism spectrum disorder. Brain Imaging and Behavior 11, 1278–1289 (2017). https://doi.org/10.1007/s11682-016-9604-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9604-8