ABSTRACT
In clinical practice, repetitive navigated transcranial magnetic stimulation (rTMS) is of particular interest for non-invasive mapping of cortical language areas. Yet, rTMS studies try to detect further cortical functions. Damage to the underlying network of visuospatial attention function can result in visual neglect—a severe neurological deficit and influencing factor for a significantly reduced functional outcome. This investigation aims to evaluate the use of rTMS for evoking visual neglect in healthy volunteers and the potential of specifically locating cortical areas that can be assigned for the function of visuospatial attention. Ten healthy, right-handed subjects underwent rTMS visual neglect mapping. Repetitive trains of 5 Hz and 10 pulses were applied to 52 pre-defined cortical spots on each hemisphere; each cortical spot was stimulated 10 times. Visuospatial attention was tested time-locked to rTMS pulses by a landmark task. Task pictures were displayed tachistoscopically for 50 ms. The subjects’ performance was analyzed by video, and errors were referenced to cortical spots. We observed visual neglect-like deficits during the stimulation of both hemispheres. Errors were categorized into leftward, rightward, and no response errors. Rightward errors occurred significantly more often during stimulation of the right hemisphere than during stimulation of the left hemisphere (mean rightward error rate (ER) 1.6 ± 1.3 % vs. 1.0 ± 1.0 %, p = 0.0141). Within the left hemisphere, we observed predominantly leftward errors rather than rightward errors (mean leftward ER 2.0 ± 1.3 % vs. rightward ER 1.0 ± 1.0 %; p = 0.0005). Visual neglect can be elicited non-invasively by rTMS, and cortical areas eloquent for visuospatial attention can be detected. Yet, the correlation of this approach with clinical findings has to be shown in upcoming steps.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Repetitive navigated transcranial magnetic stimulation (rTMS) is increasingly used for mapping of cortical functions (Hauck et al. 2015a; Krieg et al. 2015; Pascual-Leone et al. 1991; Picht et al. 2013). Researchers appreciate the combination of non-invasiveness and high spatial accuracy (Ille et al. 2015; Kim et al. 2014). As a “virtual lesion” technique, rTMS can mimic functional deficits transiently by impairing the performance during a certain task, thus detecting cortical areas that can be assigned for the certain function, e.g., language (Pascual-Leone et al. 1991). In clinical practice, it already serves as a tool for pre-surgical language mapping for neurosurgeons, and preclinical studies also investigate its use for mapping of further neuropsychological functions.
Visual neglect is a severe neurological deficit that is often observed after right-hemispheric stroke, but also described as a consequence of various other left- and right-hemispheric brain injuries, including glioma resection (Bonato 2012; Sanai et al. 2012). There are several theories about the neuronal structures involved in visuospatial attention processing (Corbetta et al. 2005; Heilman 1980; Kinsbourne 1977); the latest studies give promising insights in white matter pathways (Lunven et al. 2015; Suchan et al. 2014; Umarova et al. 2014); all agree on one thing, that we are dealing with a complex network of cortical spots interacting via both intra- and inter-hemispheric subcortical structures (Bartolomeo et al. 2012; Duecker and Sack 2014).
The clinical importance of this network becomes apparent from the fact that, especially in patients with chronic rather than early-recovered neglect, functional outcome and quality of life are significantly reduced (Jehkonen et al. 2000; Jehkonen et al. 2006; Katz et al. 1999). Thus, we require reliable mapping tools to understand better the anatomical correlates of visuospatial attention, potentially to find new treatment options on the one hand and to create accurate cortical maps of visual neglect-eloquent areas for resection planning prior to glioma surgery on the other hand (Corbetta et al. 2005; Fierro et al. 2006; Sack 2010).
This study was designed to detect cortical areas in healthy volunteers that can be assigned for the function of visuospatial attention by mimicking its corresponding functional deficit: visual neglect.
Hence, this study aims to answer the following hypotheses:
-
1)
rTMS is able to evoke visual neglect-like deficits in healthy volunteers by an adapted version of the landmark task during tachistoscopic test conditions
-
2)
rTMS can specifically locate cortical areas enrolled in visuospatial attention processing
-
3)
our results correspond to the current literature.
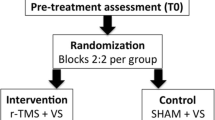
Material and methods
Structure and definitions
In the following paragraphs we will outline study design and data collection step by step. In advance we want to define one term used to describe error occurrences: Throughout the text, “error rate” (ER) will describe the number of induced errors per number of applied rTMS pulse trains, pooled across all stimulated subjects. Further explanations are provided below.
Subjects
The study was conducted on 10 healthy subjects, 5 women and 5 men, with a median age of 24 years (range 21 to 31 years). Inclusion criteria were pure right-handedness (Edinburgh handedness inventory score > 40) and age > 18 years. Exclusion criteria were general MRI or TMS exclusion criteria (pacemaker, cochlear implant, deep brain stimulation) as well as previous seizures or any other neurological or neuropsychological deficits (Rossi et al. 2009).
Ethics
The local ethics committee approved our experimental protocol in accordance with the Declaration of Helsinki (registration number: 223/14). All subjects gave their written informed consent prior to the MRI examination.
MR imaging
Before rTMS mapping, the subjects underwent MR imaging by use of a 3 Tesla MRI scanner with eight-channel phased-array head coil (Achieva 3 T, Philips Medical Systems, Amsterdam, The Netherlands B.V.). The scanning protocol contained a T2-weighted FLAIR sequence (TR: 12,000 ms, TE: 140 ms, voxel size: 0.9 × 0.9 × 4 mm3, acquisition time: 3 min) and a T1-weighted 3-D gradient echo sequence without intravenous contrast administration (TR: 9 ms, TE: 4 ms, 1 mm3 isovoxel covering the whole head, acquisition time: 6 min 58 s). We then transferred the three-dimensional dataset to our rTMS system using the DICOM standard.
Navigated rTMS mapping
Experimental setup
The rTMS mapping was performed with a Nexstim eXimia System Version 4.3. with the NEXSPEECH® module (Nexstim Oy, Helsinki, Finland). The system operates with a stereotactic camera to link the subject’s head (registered via anatomical landmarks and marked by a “tracker” headband) with the 3-D MRI dataset as an anatomical reference. Thus, while moving the stimulation coil across the head, the induced electric field inside the brain is visualized in real-time in the 3-D MRI reconstruction and we can stimulate selected brain regions accurately (Krieg et al. 2013; Picht et al. 2013; Ruohonen and Karhu 2010; Sollmann et al. 2014). The visuospatial task was set by use of NEXSPEECH software, providing a time-locked delivery of visual stimuli and applied rTMS pulses. Visual stimuli were presented on a 15-in. video screen; the screen was installed centrally to the subject’s body midline at a viewing distance of approximately 24 in. (nose to screen). For later analysis, the subject’s performance was recorded on video (Lioumis et al. 2012).
Mapping parameter
This approach being a pilot study to evaluate general feasibility and gain experience we required a stimulation protocol easy to handle and preferably familiar to the examiners. Thus, we adapted our protocol from reports on rTMS language mapping (Picht et al. 2013; Sollmann et al. 2015c; Tarapore et al. 2013), similar to another pilot study on calculation function by our group that has been published recently (Maurer et al. 2015a). Stimulation intensity was adjusted in each subject to its individual resting motor threshold (RMT), which was determined as described earlier by various groups (Krieg et al. 2012). We determined the RMT for the right and left abductor pollicis brevis muscles reflecting the motor cortex excitability for the left and right hemisphere, respectively. According to our protocol, rTMS mapping was performed at 100 % RMT. Two subjects reported significant pain, and we decreased the intensity to 80 % RMT, not to confound the subjects’ task performance with discomfort (Epstein 1996; Lioumis et al. 2012). Each rTMS stimulation train consisted of 10 pulses delivered at a repetition frequency of 5 Hz; each train thereby lasted 1800 ms. Pulse onset and appearance of the visual stimulus were triggered synchronously according to recent data on rTMS language mapping (Krieg et al. 2014; Sollmann et al. 2015b; Tarapore et al. 2013).
Visual stimuli
To test the subject’s function of visuospatial attention, we chose a line bisection judgment task. We adapted the “landmark task” originally used in patients to measure the perceptual component of neglect (Harvey et al. 1995). Visual stimuli were designed as white background-pictures with black horizontal lines bisected by a black vertical landmark (Fig. 1). The vertical transection bar (height 29 mm, width 1 mm) was positioned middle-centered on the screen and to the subject’s midline. The horizontal - left and right - line segments (width 1 mm) varied in length from 31 mm to 150 mm. Our task set consisted of 72 different pictures. In 24 pictures the line was bisected symmetrically with an equal length of the left and right segment, and in 48 pictures the line was bisected asymmetrically, to the right (with a longer left segment) or rather left (with a longer right segment). As described in previous studies, we decided to present the task pictures tachistoscopically with a display time of 50 ms (Fierro 2000; Salatino et al. 2014). The inter-picture-interval (IPI) was set to 3000 ms; two consecutive pictures were therefore separated by a black screen for 2950 ms. The order of pictures was randomized. On each picture the subject was asked to report whether the presented line appeared to be longer left, longer right, or equal in length by naming the appropriate selection orally (Fierro 2000). To familiarize subject and task setting, we conducted a baseline session before rTMS stimulation (Lioumis et al. 2012; Sollmann et al. 2015c). Baseline conditions equaled the outlined mapping conditions; baseline performance was recorded on video. We discarded all wrongly or hesitantly named pictures. In all cases, these were the first pictures presented; due to the short display time of 50 ms subjects needed to accommodate to situation and task set-up. We then made up a personalized task set for each volunteer for the following mapping.
Stimulation points and mapping procedure
Our mapping template contained 52 cortical spots per hemisphere, distributed to brain areas by use of the cortical parcellation system (CPS; Fig. 2, Table 1) (Corina et al. 2005). As reported recently, some brain regions could not be stimulated because stimulation is known to trigger unacceptable pain, i.e., the orbital part of the inferior frontal gyrus (orIFG), polar and anterior frontal regions (polFG, aSFG, aMFG), the polar temporal gyri (polTG) and the anterior middle temporal gyrus (aMTG). The inferior temporal gyrus (ITG) was not stimulated because stimulation is known not to trigger comparable effects due to increased distance to the skull and decreased stimulation intensity in the brain (Hauck et al. 2015a; Krieg et al. 2013). We anatomically identified the spots within both hemispheres in each subject’s 3-D MRI reconstruction and tagged them as stimulation points prior to each volunteer’s mapping. First, the baseline session was performed as mentioned above, then the mapping session was conducted as follows: Each hemisphere was stimulated twice, taking it in turns and starting with the left hemisphere; each stimulation point was stimulated 5 times, thus 10 times in total. For a maximal field induction the stimulation coil was placed tangentially to the skull in anterior-posterior field orientation (Epstein 1996; Lioumis et al. 2012; Miranda 2013).
Sum of errors. This figure illustrates the distribution of error rates per stimulated cortical spot (on average, pooled across all subjects) for the left (a) and the right hemisphere (b). Respective subject rates (number of positive subjects out of 10 stimulated subjects) are presented separately, for the left (c) and the right hemisphere (d)
Leftward errors. Distribution of leftward error rates per cortical spot (on average, pooled across all subjects) within the left (a) and the right hemisphere (b). Respective subject rates (number of positive subjects out of 10 stimulated subjects) are presented separately, for the left (c) and the right hemisphere (d)
Rightward errors. Distribution of rightward error rates per cortical spot (on average, pooled across all subjects) within the left (a) and the right hemisphere (b). Respective subject rates (number of positive subjects out of 10 stimulated subjects) are presented separately, for the left (c) and the right hemisphere (d)
Evaluation of discomfort
Eventually, the subject was asked to quantify discomfort and pain during rTMS stimulation. We differentiated between the temporal muscle area and all other parts of the head surface (convexity); rating was made by a visual analogue scale (VAS) from 0 to 10, with 0 representing no pain, and 10 representing maximal pain.
RTMS data analysis
rTMS data were analyzed in a two-step process (Ille et al. 2015; Lioumis et al. 2012). At first, we evaluated the video-recorded task performance blinded to stimulation sites. Each response was linked with the subject’s baseline response to the respective Picture. Errors were categorized as follows:
-
1)
No-response errors: The subject did not answer at all or stated in any other way not to feel certain. No-response errors in terms of a noticeable speech arrest were discarded; vague cases were talked over with the subject and if remaining unclear discarded as well.
-
2)
Leftward errors: The subject overestimated the left line segment or rather underestimated the right line segment.
-
3)
Rightward errors: The subject overestimated the right line segment or rather underestimated the left line segment.
Additionally, the volunteer’s face was analyzed on video to check if eye blinks, pain, or muscle stimulation impaired the result. All such errors were systematically discarded, also if co-occurring with an induced visuospatial deficit. In a second step, we related errors with stimulated cortical spots. For every spot we gathered information about the number of effective stimulations and the number of particular error types during stimulation; we computed the total number of errors (as the sum of all types of errors), and labeled the spot “positive” if at least 1 out of 10 stimulations elicited any error. We then looked at each spot from two different perspectives:
-
1)
Number of errors per stimulation at this spot, pooled across all subjects (error rate (ER) = number of errors per number of stimulations)
-
2)
Number of subjects, for which this spot is labeled “positive” (subject rate = number of positive subjects out of 10 stimulated subjects).
Statistics
Results are presented as mean ± standard deviation (SD). We compared the ER of both hemispheres by use of the Mann-Whitney U test and ER within one hemisphere by use of the Wilcoxon matched-pairs signed rank test. To analyze the categorical outcome of “positive” spots, we performed a Chi-square test. For all tests a p-value <0.05 was considered significant (GraphPad Prism 6.0, La Jolla, CA, USA).
Results
Mapping characteristics
We determined a mean RMT of 34.9 ± 8.9 % maximal stimulator output for the left hemisphere and of 34.5 ± 8.2 % for the right hemisphere (p = 0.9274; Table 2). Due to reported pain, we reduced the stimulation intensity after RMT determination in two cases (marked with an asterisk). Yet, the electric field strength on cortical level was higher than 55 V/m at all times and we did not observe any effect on error occurrence or frequency in these subjects compared to the whole collective as observed previously (Picht et al. 2013). All subjects tolerated the mapping well; mean discomfort was comparable for both hemispheres. During baseline testing 94.3 ± 4.1 % of the pictures were answered correctly, and the individual mapping task set consisted of 68 pictures on average. The number of baseline errors did not correlate with the number of errors during mapping conditions.
Sum of errors
First, we looked at the error category “sum of errors.” It contains all errors in summary without regard to the particular type of error.
Comparison of the two hemispheres
Error occurrence for the two hemispheres was comparable (p = 0.2314). Pooled across all subjects, 5122 stimulations of the left hemisphere could elicit 163 errors, equivalent to a mean total ER of 3.2 ± 1.6 %. Concerning the right hemisphere, we observed 182 errors during 5126 stimulations (ER of 3.6 ± 1.7 %). Subject rates per cortical spot ranged from 0 to 6 positive out of 10 stimulated subjects within the left hemisphere and from 0 to 5 within the right hemisphere (p = 0.6445; Tables 3 and 4).
Left hemisphere
Referenced to cortical spots, we observed a mean total ER (pooled across all subjects) between 0 % and 7 %. Best ER were obtained for the aSMG (spot no. 32) and the dLOG (spot no. 49), for the SPL (spot no. 48) and for the vPrG (spot no. 23) (Fig. 3a, Online Resource 1). Subject rates are presented separately (Fig. 3c, Online Resource 1). The most convenient co-occurrence of a high ER on average and a high subject rate (i.e., a high number of subjects contributing to the error count) was observed for cortical spots within the aSMG and the dLOG (Figs. 3a and c).
Right hemisphere
Mean total ER ranged from 0 % to 8 %. The highest rates (pooled across all subjects) occurred within middle frontal and pre-central gyri (spots no. 13, 17, and 21), within the opIFG (spot no. 10), the pMTG (spot no. 43), and the polLOG (spot no. 51) (Fig. 3b, Online Resource 2). Subject rates are presented respectively (Fig. 3d, Online Resource 2), and they coincide best with high ER spots in the frontal lobe.
Distribution of leftward and rightward errors
To differ between leftward and rightward attention processing, we looked at the particular types of error. Particular ER tend to be relatively small; however, some differences show statistical significance.
Comparison of the two hemispheres
We observed left- and rightward deficits during the stimulation of both hemispheres. The number of leftward errors was comparable for the two hemispheres (p = 0.3877; Figs. 4a and c, Tables 3 and 4). Pooled across all subjects, we obtained a mean leftward ER of 2.0 ± 1.3 % for the left hemisphere and a mean leftward ER of 1.7 ± 1.3 % for the right hemisphere (Tables 3 and 4). Subject rates for leftward errors varied for cortical spots of both hemispheres comparably (p = 0.1292; Figs. 4c and d, Tables 3 and 4). Rightward errors occurred significantly more often during stimulation of the right hemisphere than during stimulation of the left hemisphere (ER 1.6 ± 1.3 % vs. 1.0 ± 1.0 %, p = 0.0141; Figs. 5a and b, Tables 3 and 4). Yet, subject rates for rightward errors were comparable between both hemispheres (p = 0.5034; Figs. 5c and d, Tables 3 and 4).
Left hemisphere
After stimulation of the left hemisphere, we observed predominantly leftward errors (p = 0.0005; Fig. 6a, Table 3, Online Resource 1). In addition, some cortical spots presented higher rightward ER, especially in anterior parietal regions (spots no. 32, 33, 36, 40, and 44; Figs. 5a and 6a).
Right hemisphere
Stimulation of the right hemisphere elicited leftward and rightward errors to a similar extent (p = 0.6836; Fig. 6b, Table 4, Online Resource 2). ER of both types varied from 0 % to 5 %. Although not statistically significant, we observed a noticeable trend of rightward errors being cumulatively distributed to the frontal lobe (Figs. 5b and 6b).
Discussion
NTMS-based mapping of visuospatial attention function
The first goal of this study was to show that rTMS can mimic visual neglect in healthy volunteers (Duecker and Sack 2014; Fierro 2000; Sack 2010); we successfully evoked visual neglect-like deficits in all examined subjects. The observed effects equate contralesional, or rather ipsilesional, visual neglect depending on the combination of stimulated (i.e., thus virtually lesioned) hemisphere and elicited type of error. Leftward errors (equal to right-sided visuospatial attention deficits) during stimulation of the left hemisphere correspond to classical contralesional visual neglect, as do rightward errors (or left-sided deficits) for stimulation of the right hemisphere. Leftward errors during stimulation of the right hemisphere and rightward errors during stimulation of the left hemisphere, on the other hand, are in line with ipsilesional visual neglect. In this study, rTMS could imitate contralesional and ipsilesional visual neglect (Figs. 4 and 5, Tables 3 and 4) and we were able to link the effects accurately to cortical areas by means of the neuronavigation system which is—at least to our knowledge—the first time to be reported.
Landmark task design and tachistoscopic testing
In recent years, neuroscientists entered into a discussion about the term of visuospatial attention and neglect (Bartolomeo et al. 2007; Corbetta and Shulman 2011; de Haan et al. 2012; Karnath and Rorden 2012). They require the separation of particular components of attention processing (spatial vs. non-spatial, goal directed vs. stimulus driven, subject centered vs. object centered, etc.) and call on researchers to distinguish between tasks demanding these components to a different extent. Besides, in a review on visuospatial tasks for diagnosing visual neglect patients, Bonato et al. discusses a couple of compensation mechanisms (fixation, reorienting, etc.) masking existent deficits; they consequently propose the construction of tasks more demanding and sensitive than paper-and-pencil-tasks (Bonato 2012). In this study, we therefore tested visuospatial, object-centered attention processing by embedding an adapted version of the landmark task into a tachistoscopic test setting, as already used before (Fierro 2000). The short display time of 50 ms prevents eye scanning and fixation, thus increasing sensitivity. Generally, we can rate our setup as feasible and effective. However, ER during baseline and mapping conditions were considerably small; hence, one should consider increasing difficulty by minimizing the differences between left and right line segments. At the same time, we should keep in mind that this study examined a cohort of young and healthy subjects; a patient study might not be feasible at a higher difficulty level, which is what we are basically aiming for. The chosen combination provided an adequate visuospatial task design for this study and made it possible to sensitively map visuospatial object-centered attention.
Results in comparison to the current literature
There are several theories about the functional mechanisms of visuospatial attention processing. Kinsbourne (1977) and Heilman (1980) were the first to outline the role of parietal regions and interhemispheric differences and interactions; over time, more and more studies put frontal and temporal regions into play: Corbetta and Shulman (2002, 2011) concluded a dynamic model of frontoparietal intrahemispheric circuits. They distinguished between a dorsal network including superior and posterior parietal and superior frontal regions (represented in both hemispheres to a similar extent) and a ventral network including the temporoparietal junction (TPJ) and inferior frontal regions (represented dominantly within the right hemisphere).
Literature on the hemispheric asymmetries is very rarely balanced; most studies on visuospatial attention focus on the right hemisphere (Sack 2010). The prevalence of visual neglect might be higher after damage to the right rather than the left hemisphere, but the severity after left hemispheric damage shows comparable sequelae (Suchan et al. 2012). To paint a total picture of the underlying mechanisms, though, it is crucial to examine both hemispheres in a comparable way. Besides, apparent from case reports on visual neglect in its diverse shapes and coherences, we have to assume that the network shows highly individual differences (Kwon et al. 2011; Sacchetti et al. 2015; Shinoura et al. 2009). This study included a considerably homogenous cohort with no participants driving the results; hence we could show good agreement in particular regions. In the following paragraphs, we will discuss these findings in relation to the current literature.
General error occurrence and cortical distribution
In contrast to other studies, we tested cortical spots of the whole left and right hemisphere (Fig. 2), and observed effects during stimulation over all lobes (Fig. 3) (Brighina et al. 2002; Fierro 2000). Between both hemispheres, we found regional differences. Within the left hemisphere, we especially want to point to anterior parietal spots (aSMG) and more posterior parietal or rather occipital spots of the SPG and the dLOG (Figs. 3a and c, Table 3). The role of parietal spots corresponds well with previous (non-navigated) TMS studies (Duecker and Sack 2014; Fierro 2000; Salatino et al. 2014), and with the original theories in general, as described above (Heilman 1980; Kinsbourne 1977). Frontal positive spots were observed in the SFG, IFG, and vPrG (Figs. 3a and c, Table 3). Referring to Corbetta superior spots within the human frontal eye field (FEF) might be part of a dorsal network (Corbetta and Shulman 2002).
Within the right hemisphere, parietal spots were slightly more common in superior and middle parietal regions; i.e. the dorsal parts of the anG and the aSMG, as well as the mPoG (Figs. 3b and d, Table 4). Additionally, one occipital spot showed an unexpected high ER (pooled across all subjects), which might be explained as a direct effect on the visual cortex. Particularly striking were posterior temporal spots of the pSTG and pMTG and frontal spots of the MFG, the mPrG, and the opIFG (Figs. 3b and d). Again referring to Corbetta, these regions accord especially well with their proposed right-lateralized ventral network, including right TPJ and right ventral frontal areas (Corbetta and Shulman 2002; Corbetta and Shulman 2011).
Distribution of leftward and rightward errors
Overall, reports on ipsilesional neglect are less common than those on classical contralesional neglect. In this study, we were able to mimic both types of attention shift by stimulation of both hemispheres (Fig. 6, Tables 3 and 4); and yet, rightward errors (or left-sided neglect) occurred significantly more often during stimulation of the right hemisphere, according to a contralesional neglect (Figs. 5b and d), than during stimulation of the left hemisphere (that would parallel ipsilesional neglect, Figs. 5a and c).
The observed rightward errors within the left hemisphere (corr. to ipsilesional neglect) were mainly distributed to anterior parietal regions (Figs. 5a and c); interestingly, Salatino et al. found the same in a TMS study on parietal hot spots (Salatino et al. 2014). Apart from that, during stimulation of the left hemisphere, we elicited primarily leftward errors and thus contralesional neglect (Figs. 4a and c, Fig. 6a, Table 3), well in accordance with all major theories (Corbetta and Shulman 2002; Heilman 1980; Kinsbourne 1977).
For the right hemisphere, it was more difficult to differentiate between higher leftward or rather rightward error occurrences (Fig. 6b, Table 4). Generally, we observed both, a finding that Roux et al. also confirmed in a patient study by direct cortical stimulation (Roux et al. 2011). However, rightward errors (corr. to contralesional neglect) had a particular share in ventral frontal regions (Figs. 5b and d, Fig. 6b), while leftward errors (corr. to ipsilesional neglect) were spread over all lobes (Figs. 4b and d, Fig. 6b).
Limitations
Despite these encouraging results and the accordance to current literature, we should also consider limitations of this study. First of all, this study was designed as a pilot study to evaluate general feasibility. With our main focus on the wide-ranged examination of both hemispheres and the analysis of summary data, we had to simplify our stimulation protocol and accept a number of basic limitations. The use of a fixed mapping template and the strictly anterior-posterior coil orientation need to be particularly mentioned. As confirmed by Sollmann et al., variations in stimulation site or coil angulation certainly could have changed our results; yet, anterior-posterior orientation is the current standard for rTMS examinations since it has shown reliable results in navigated and non-navigated rTMS studies on language, neglect and calculation function (Sollmann et al. 2015b). In addition, we had to reduce the stimulation intensity in two of our subjects. Yet, the electric field strength on cortical level was above 55 V/m at all times, which is known to be sufficiently effective in rTMS language mapping (Picht et al. 2013). Accordingly we did not find any effect on mapping performance and error occurrence in these subjects compared to the other subjects of the cohort.
One could question the significance of our results in respect to a rather small and obviously young cohort and small ER. A low mean age minimizes the generalizability without question; the examination of a larger diverse collective would be appropriate to investigate the general applicability. Yet, all our subjects were healthy, without any medication, and without any neurological pathology (e.g. subcortical ischemic changes), and thus beneficially homogenous. Certainly, there is a discrepancy between the assumption of highly individual distribution of cortical networks (and their suggestibility) and the analysis of individual data in summary. Furthermore, our stimulation protocol did not include any specific test-retest evaluation of positive spots. However, we observed good accordance of ER and subject rates in particular regions. With a number of 10 subjects, this study took a first step of evaluation. So, we should consider the general results with this background, and we should pay special attention to the significant ones.
As one final crucial point, we want to address the missing controls. We cannot answer if any errors were due to other effects than the local disturbance of neuronal tissue by rTMS; for example, impaired concentration, eye movements, etc. To filter these unintended effects, a control trial by sham stimulation or inclusion of an eye tracking device should be considered in future studies. Furthermore, some studies raise the issue whether rTMS also has remote effects on functional networks; i.e. cortical structures that are connected to the site of stimulation via subcortical fiber tracts. Better understanding of these interactions might explain—among others—the discrepancy between leftward and rightward attention processing within one hemisphere. For example, combined fMRI/TMS studies allow the visualization of local and distal rTMS effects by concurrent use of fMRI, a design that has already been used before (Ricci et al. 2012; Ruff et al. 2008).
Future implications and challenges
This study may be considered a pilot study for further research. For example, it would be interesting to design a comparative study with different stimulation frequencies to further analyze inhibiting vs. exciting rTMS effects (Epstein 1996; Hauck et al. 2015b; Miranda 2013). Apart from that, investigations on visuospatial attention and visual neglect increasingly focus on subcortical network components; i.e., intra- and inter-hemispheric white matter fiber tracts. Diffusion tensor imaging (DTI) affords an opportunity to visualize changes of these network structures in patients over the course of post-stroke recovery or chronification (Lunven et al. 2015; Umarova et al. 2014). On the other hand, DTI fiber tracking (DTI FT) in healthy subjects can visualize regular connections and interactions (Suchan et al. 2014). A promising outlook for future analysis afford latest approaches in nTMS-based DTI FT (Sollmann et al. 2015a); the idea here is to use nTMS-mapped cortical spots as specific origins for the visualization of fiber tracts. However, apart from basic research, rTMS mapping of visuospatial attention may also have clinical benefits, such as accurate preoperative cortical maps in brain tumor patients undergoing neurosurgical resection. Additionally, several studies already successfully used therapeutic rTMS to reduce visual neglect in stroke patients (Brighina et al. 2003; Fierro et al. 2006; Koch et al. 2012). Corbetta et al. (2005) described neglect as the combination of “structural changes at the locus of injury” and supplementary “physiological changes in distant but functionally related brain areas”; the aim of rehabilitation treatment, therefore, is a rebalancing of the partially damaged network. Previous approaches broadly targeted the parietal cortex. rTMS mapping could provide more accurate cortical maps and thus specific sites for therapeutic rTMS application.
Conclusions
To finally answer our hypotheses, we may say that rTMS is a feasible tool to evoke visual neglect-like deficits in healthy volunteers. Based on our task setting, we could specifically locate cortical components of the visuospatial attention network, and our results accord well to the current scientific literature.
Abbreviations
- dti:
-
Diffusion tensor imaging
- er:
-
Error rate
- fef:
-
Frontal eye field
- fmri:
-
Functional magnetic resonance imaging
- ft:
-
Fiber tracking
- ipi:
-
Inter-picture-interval
- mri:
-
Magnetic resonance imaging
- rmt:
-
Resting motor threshold
- ntms:
-
Navigated transcranial magnetic stimulation
- rtms:
-
Repetitive navigated transcranial magnetic stimulation
- tms:
-
Transcranial magnetic stimulation
- tpj:
-
Temporoparietal junction
- sd:
-
Standard deviation
- vas:
-
Visual analogue scale
- 3-d:
-
Three-dimensional
References
Bartolomeo, P., Thiebaut de Schotten, M., Duffau, H., 2007. Mapping of visuospatial functions during brain surgery: A new tool to prevent unilateral spatial neglect. Neurosurgery, 61, e1340.
Bartolomeo, P., de Schotten, M. T., & Chica, A. B. (2012). Brain networks of visuospatial attention and their disruption in visual neglect. Frontiers in Human Neuroscience, 6, 110.
Bonato, M. (2012). Neglect and extinction depend greatly on task demands: a review. Frontiers in Human Neuroscience, 6, 195.
Brighina, F., Bisiach, E., Oliveri, M., Piazza, A., La Bua, V., Daniele, O., & Fierro, B. (2003). 1 Hz repetitive transcranial magnetic stimulation of the unaffected hemisphere ameliorates contralesional visuospatial neglect in humans. Neuroscience Letters, 336, 131–133.
Brighina, F., Bisiach, E., Piazza, A., Oliveri, M., La Bua, V., Daniele, O., & Fierro, B. (2002). Perceptual and response bias in visuospatial neglect due to frontal and parietal repetitive transcranial magnetic stimulation in normal subjects. Neuroreport, 13, 2571–2575.
Corbetta, M., & Shulman, G. L. (2002). Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews. Neuroscience, 3, 201–215.
Corbetta, M., & Shulman, G. L. (2011). Spatial neglect and attention networks. Annual Review of Neuroscience, 34, 569–599.
Corbetta, M., Kincade, M. J., Lewis, C., Snyder, A. Z., & Sapir, A. (2005). Neural basis and recovery of spatial attention deficits in spatial neglect. Nature Neuroscience, 8, 1603–1610.
Corina, D. P., Gibson, E. K., Martin, R., Poliakov, A., Brinkley, J., & Ojemann, G. A. (2005). Dissociation of action and object naming: evidence from cortical stimulation mapping. Human Brain Mapping, 24, 1–10.
Duecker, F., Sack, A.T., 2014. The hybrid model of attentional control: New insights into hemispheric asymmetries inferred from TMS research. Neuropsychologia, 74, 21–9.
Epstein, C.M., 1996. Optimum stimulus parameters for lateralized suppression of speech with magnetic brain stimulation. Neurology, 47, 1590–3.
Fierro, B., 2000. Contralateral neglect induced by right posterior parietal rTMS in healthy subjects. Neuroreport, 11, 1519–21.
Fierro, B., Brighina, F., & Bisiach, E. (2006). Improving neglect by TMS. Behavioural Neurology, 17, 169–176.
de Haan, B., Karnath, H. O., & Driver, J. (2012). Mechanisms and anatomy of unilateral extinction after brain injury. Neuropsychologia, 50, 1045–1053.
Harvey, M., Milner, A. D., & Roberts, R. C. (1995). An investigation of hemispatial neglect using the landmark test. Brain and Cognition, 27, 59–78.
Hauck, T., Tanigawa, N., Probst, M., Wohlschlaeger, A., Ille, S., Sollmann, N., Maurer, S., Zimmer, C., Ringel, F., Meyer, B., & Krieg, S. M. (2015a). Stimulation frequency determines the distribution of language positive cortical regions during navigated transcranial magnetic brain stimulation. BMC Neuroscience, 16, 5.
Hauck, T., Tanigawa, N., Probst, M., Wohlschlaeger, A., Ille, S., Sollmann, N., Maurer, S., Zimmer, C., Ringel, F., Meyer, B., & Krieg, S. M. (2015b). Task type affects location of language-positive cortical regions by repetitive navigated transcranial magnetic stimulation mapping. PloS One, 10, e0125298.
Heilman, K. M. (1980). Right hemisphere dominance for attention: the mechanism underlying hemispheric asymmetries of inattention (neglect). Neurology, 30, 327.
Ille, S., Sollmann, N., Hauck, T., Maurer, S., Tanigawa, N., Obermueller, T., Negwer, C., Droese, D., Zimmer, C., Meyer, B., Ringel, F., & Krieg, S. M. (2015). Combined noninvasive language mapping by navigated transcranial magnetic stimulation and functional MRI and its comparison with direct cortical stimulation. Journal of Neurosurgery, 123, 212–25.
Jehkonen, M., Laihosalo, M., Kettunen, J.E., 2006. Impact of neglect on functional outcome after stroke – a review of methodological issues and recent research findings. Restorative Neurology and Neuroscience, 24, 209–15.
Jehkonen, M., Ahonen, J. P., Dastidar, P., Koivisto, A. M., Laippala, P., Vilkki, J., & Molnar, G. (2000). Visual neglect as a predictor of functional outcome one year after stroke. Acta Neurologica Scandinavica, 101, 195–201.
Karnath, H. O., & Rorden, C. (2012). The anatomy of spatial neglect. Neuropsychologia, 50, 1010–1017.
Katz, N., Hartman-Maeir, A., Ring, H., Soroker, N., 1999. Functional disability and rehabilitation outcome in right hemisphere damaged patients with and without unilateral spatial neglect. Archives of Physical Medicine and Rehabilitation, 80, 379–84.
Kim, W. J., Min, Y. S., Yang, E. J., & Paik, N.-J. (2014). Neuronavigated vs Conventional Repetitive Transcranial Magnetic Stimulation Method for Virtual Lesioning on the Broca's Area. . Neuromodulation: Technology at the Neural Interface, 17, 16–21.
Kinsbourne, M. (1977). Hemi-neglect and hemisphere rivalry. Advances in Neurology, 18, 41–49.
Koch, G., Bonni, S., Giacobbe, V., Bucchi, G., Basile, B., Lupo, F., Versace, V., Bozzali, M., & Caltagirone, C. (2012). Theta-burst stimulation of the left hemisphere accelerates recovery of hemispatial neglect. Neurology, 78, 24–30.
Krieg, S. M., Shiban, E., Buchmann, N. H., Gempt, J., Foerschler, A., Meyer, B., & Ringel, F. (2012). Utility of presurgical navigated transcranial magnetic brain stimulation for the resection of tumors in eloquent motor areas. Journal of Neurosurgery, 116, 994–1001.
Krieg, S. M., Sollmann, N., Hauck, T., Ille, S., Foerschler, A., Meyer, B., & Ringel, F. (2013). Functional language shift to the right hemisphere in patients with language-eloquent brain tumors. PloS One, 8, e75403.
Krieg, S. M., Sollmann, N., Tanigawa, N., Foerschler, A., Meyer, B., & Ringel, F. (2015). Cortical distribution of speech and language errors investigated by visual object naming and navigated transcranial magnetic stimulation. Brain Structure & Function, 38, 1320–1324.
Krieg, S. M., Tarapore, P. E., Picht, T., Tanigawa, N., Houde, J., Sollmann, N., Meyer, B., Vajkoczy, P., Berger, M. S., Ringel, F., & Nagarajan, S. (2014). Optimal timing of pulse onset for language mapping with navigated repetitive transcranial magnetic stimulation. NeuroImage, 100, 219–236.
Kwon, J. C., Ahn, S., Kim, S., & Heilman, K. M. (2011). Ipsilesional ‘where’ with contralesional ‘what’ neglect. Neurocase, 18, 415–423.
Lioumis, P., Zhdanov, A., Makela, N., Lehtinen, H., Wilenius, J., Neuvonen, T., Hannula, H., Deletis, V., Picht, T., & Makela, J. P. (2012). A novel approach for documenting naming errors induced by navigated transcranial magnetic stimulation. Journal of Neuroscience Methods, 204, 349–354.
Lunven, M., Thiebaut De Schotten, M., Bourlon, C., Duret, C., Migliaccio, R., Rode, G., & Bartolomeo, P. (2015). White matter lesional predictors of chronic visual neglect: a longitudinal study. Brain, 138, 746–760.
Maurer, S., Tanigawa, N., Sollmann, N., Hauck, T., Ille, S., Boeckh-Behrens, T., Meyer, B., & Krieg, S. (2015a). Non-invasive mapping of calculation function by repetitive navigated transcranial magnetic stimulation. Brain Structure and Function, 28(4), 1–21.
Miranda, P. C. (2013). Physics of effects of transcranial brain stimulation. Handbook of Clinical Neurology, 116, 353–366.
Pascual-Leone, A., Gates, J. R., & Dhuna, A. (1991). Induction of speech arrest and counting errors with rapid-rate transcranial magnetic stimulation. Neurology, 41, 697–702.
Picht, T., Krieg, S. M., Sollmann, N., Rosler, J., Niraula, B., Neuvonen, T., Savolainen, P., Lioumis, P., Makela, J. P., Deletis, V., Meyer, B., Vajkoczy, P., & Ringel, F. (2013). A comparison of language mapping by preoperative navigated transcranial magnetic stimulation and direct cortical stimulation during awake surgery. Neurosurgery, 72, 808–819.
Ricci, R., Salatino, A., Li, X., Funk, A. P., Logan, S. L., Mu, Q., Johnson, K. A., Bohning, D. E., & George, M. S. (2012). Imaging the neural mechanisms of TMS neglect-like bias in healthy volunteers with the interleaved TMS/fMRI technique: preliminary evidence. Frontiers in Human Neuroscience, 6, 326.
Rossi, S., Hallett, M., Rossini, P. M., & Pascual-Leone, A. (2009). Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clinical Neurophysiology, 120, 2008–2039.
Roux, F. E., Dufor, O., Lauwers-Cances, V., Boukhatem, L., Brauge, D., Draper, L., Lotterie, J. A., Demonet, J. F. (2011). Electrostimulation mapping of spatial neglect. Neurosurgery, 69, 1218–31.
Ruff, C. C., Bestmann, S., Blankenburg, F., Bjoertomt, O., Josephs, O., Weiskopf, N., Deichmann, R., & Driver, J. (2008). Distinct causal influences of parietal versus frontal areas on human visual cortex: evidence from concurrent TMS-fMRI. Cerebral Cortex, 18, 817–827.
Ruohonen, J., & Karhu, J. (2010). Navigated transcranial magnetic stimulation. Neurophysiologie Clinique, 40, 7–17.
Sacchetti, D. L., Goedert, K. M., Foundas, A. L., & Barrett, A. M. (2015). Ipsilesional neglect: behavioral and anatomical correlates. Neuropsychology, 29, 183–190.
Sack, A.T., 2010. Using non-invasive brain interference as a tool for mimicking spatial neglect in healthy volunteers. Restorative Neurology and Neuroscience, 28(4), 485–497.
Salatino, A., Poncini, M., George, M. S., & Ricci, R. (2014). Hunting for right and left parietal hot spots using single-pulse TMS: modulation of visuospatial perception during line bisection judgment in the healthy brain. Frontiers in Psychology, 5, 1238.
Sanai, N., Martino, J., & Berger, M. S. (2012). Morbidity profile following aggressive resection of parietal lobe gliomas. Journal of Neurosurgery, 116, 1182–1186.
Shinoura, N., Suzuki, Y., Yamada, R., Tabei, Y., Saito, K., & Yagi, K. (2009). Damage to the right superior longitudinal fasciculus in the inferior parietal lobe plays a role in spatial neglect. Neuropsychologia, 47, 2600–2603.
Sollmann, N., Giglhuber, K., Tussis, L., Meyer, B., Ringel, F., & Krieg, S. M. (2015b). NTMS-based DTI fiber tracking for language pathways correlates with language function and aphasia – a case report. Clinical Neurology and Neurosurgery, 136, 25–28.
Sollmann, N., Ille, S., Obermueller, T., Negwer, C., Ringel, F., Meyer, B., & Krieg, S. M. (2015a). The impact of repetitive navigated transcranial magnetic stimulation coil positioning and stimulation parameters on human language function. European Journal of Medical Research, 20, 47.
Sollmann, N., Tanigawa, N., Ringel, F., Zimmer, C., Meyer, B., & Krieg, S. M. (2014). Language and its right-hemispheric distribution in healthy brains: An investigation by repetitive transcranial magnetic stimulation. NeuroImage, 102(Part 2), 776–788.
Sollmann, N., Tanigawa, N., Tussis, L., Hauck, T., Ille, S., Maurer, S., Negwer, C., Zimmer, C., Ringel, F., Meyer, B., & Krieg, S. M. (2015c). Cortical regions involved in semantic processing investigated by repetitive navigated transcranial magnetic stimulation and object naming. Neuropsychologia, 70, 185–195.
Suchan, J., Rorden, C., & Karnath, H. O. (2012). Neglect severity after left and right brain damage. Neuropsychologia, 50, 1136–1141.
Suchan, J., Umarova, R., Schnell, S., Himmelbach, M., Weiller, C., Karnath, H. O., & Saur, D. (2014). Fiber pathways connecting cortical areas relevant for spatial orienting and exploration. Human Brain Mapping, 35, 1031–1043.
Tarapore, P. E., Findlay, A. M., Honma, S. M., Mizuiri, D., Houde, J. F., Berger, M. S., & Nagarajan, S. S. (2013). Language mapping with navigated repetitive TMS: proof of technique and validation. NeuroImage, 82, 260–272.
Umarova, R. M., Reisert, M., Beier, T. U., Kiselev, V. G., Kloppel, S., Kaller, C. P., Glauche, V., Mader, I., Beume, L., Hennig, J., & Weiller, C. (2014). Attention-network specific alterations of structural connectivity in the undamaged white matter in acute neglect. Human Brain Mapping, 35, 4678–4692.
Acknowledgments
The first author gratefully acknowledges the support of the TUM graduate school.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SK is a consultant for BrainLab AG (Feldkirchen, Germany). Yet, the study was completely financed by institutional grants from the Department of Neurosurgery and the Section of Neuroradiology, and all authors declare to have no conflict of interest affecting this study, nor the materials or methods used, nor the findings specified in this paper.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all patients for being included in the study.
Electronic supplementary material
Online Resource 1
(DOCX 114 kb)
Online Resource 2
(DOCX 111 kb)
Rights and permissions
About this article
Cite this article
Giglhuber, K., Maurer, S., Zimmer, C. et al. Evoking visual neglect-like deficits in healthy volunteers – an investigation by repetitive navigated transcranial magnetic stimulation. Brain Imaging and Behavior 11, 17–29 (2017). https://doi.org/10.1007/s11682-016-9506-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-016-9506-9