Abstract
Novel rehabilitation interventions have improved motor recovery by induction of neural plasticity in individuals with stroke. Of these, Music-supported therapy (MST) is based on music training designed to restore motor deficits. Music training requires multimodal processing, involving the integration and co-operation of visual, motor, auditory, affective and cognitive systems. The main objective of this study was to assess, in a group of 20 individuals suffering from chronic stroke, the motor, cognitive, emotional and neuroplastic effects of MST. Using functional magnetic resonance imaging (fMRI) we observed a clear restitution of both activity and connectivity among auditory-motor regions of the affected hemisphere. Importantly, no differences were observed in this functional network in a healthy control group, ruling out possible confounds such as repeated imaging testing. Moreover, this increase in activity and connectivity between auditory and motor regions was accompanied by a functional improvement of the paretic hand. The present results confirm MST as a viable intervention to improve motor function in chronic stroke individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although mortality rates have been reduced in high-income countries, stroke is still the second most common cause of death worldwide (Feigin et al. 2014) and the third cause of disability-adjusted life-years (Murray et al. 2012). More than 50 % of individuals suffering a stroke have a residual motor deficit, especially affecting the upper extremities (Roger et al. 2012). Among the multiple other possible consequences of stroke, mood changes and cognitive dysfunction are quite common (Nys et al. 2007).
Recent human and animal studies have indicated that the adult brain has considerable potential for functional reorganization. Specifically, cortical map changes can occur in response to experience and learning, or in the course of recovery from injuries or degeneration processes (Buonomano and Merzenich 1998; Munte et al. 2002). Indeed, recovery from hemiparesis after stroke is associated with reorganization of the human brain (Cramer 2008). Several studies have reported abnormal motor activation after stroke, including bilateral activation of primary motor areas (Johansen-Berg et al. 2002) or enhanced activity in non-primary motor regions, such as the premotor cortex (PMC) and the supplementary motor area (SMA; Seitz et al. 1998; Weiller et al. 1993). There is a complex relationship between motor recovery after stroke and the interplay between primary, pre and supplementary motor areas. The ipsilesional PMC has been suggested to support primary motor areas in order to subserve motor function after stroke (Kantak et al. 2012; Schulz et al. 2015). Motor recovery has also been related to enhanced ipsilesional connectivity between the SMA and primary motor regions (Rehme et al. 2011). Interestingly, better motor outcomes in rehabilitation have been shown to induce an increase of activity in ipsilesional motor regions and a decrease of activation in contralesional motor areas (Johansen-Berg et al. 2002; Marshall et al. 2000; Dong et al. 2006). Thus, decrease of contralesional activity can be seen as a marker for clinical improvement. In this vein, analysis of functional connectivity—i.e., the functional integration of several specialized areas which subserve a particular brain function, measured as statistical dependencies among those segregated regions (Friston 2011)—complements traditional univariate fMRI analysis approaches and aids to delineate stroke-related changes and the effect of interventions (Grefkes and Fink 2011).
This generally accepted view of the adult brain as a changing and adapting functional and structural core has motivated the design of novel rehabilitative interventions to boost stroke recovery and improve impairment. In this context, newly developed therapies have proven to be more effective that standard therapeutic approaches (Taub et al. 2002; Langhorne et al. 2011). A premier example is constraint-induced therapy (CIT), which forces the use of the affected arm over extended periods of time in a variety of motor tasks and produces clinically significant improvements of motor function, along with neuroplastic changes (Wittenberg et al. 2003).
In this vein, music listening and training has been proposed as a potential rehabilitation tool (Särkämö et al. 2013). Indeed, in the last decades, music therapy as a clinical intervention for neurological populations has been used to induce benefits in motor function (e.g., gait; Bradt et al. 2010; Thaut et al. 1993, 1996; Hurt et al. 1998), mood (Särkämö et al. 2008; Magee and Davidson 2002) and a broad variety of cognitive deficits such as visuo-spatial neglect (Bernardi et al. 2015), aphasia (Cohen 1992; Cohen and Ford 1995; Zumbansen et al. 2014) and even consciousness disorders (O’Kelly et al. 2013; Boyle and Greer 1983). Therefore, music therapy is proposed as a treatment that targets different domains in stroke and other neurological diseases such as Parkinson, multiple sclerosis or neurodegenerative disorders (Thaut 2015). This idea is based on numerous evidences showing that music playing appears to be a particularly strong inductor of neural plasticity (Pantev and Herholz 2011; Wan and Schlaug 2010; Munte et al. 2002; Francois et al. 2015; Strait and Kraus 2014), requiring the processing and integration of multimodal information (auditory, visual and sensorimotor information). Music training has been shown to induce long-lasting structural and functional changes in several brain areas, including the sensorimotor cortex (Schlaug 2001; Hyde et al. 2009), auditory regions (Schulze et al. 2009; Seither-Preisler et al. 2014), visual–spatial brain areas (Gaser and Schlaug 2003), the corpus callosum (Hyde et al. 2009; Schlaug et al. 1995) and the hippocampus (Herdener et al. 2010). In addition, fast plastic changes induced by music learning have also been observed in motor-related brain regions (Bangert et al. 2006; Baumann et al. 2007; Meyer et al. 2007; Lahav et al. 2007; Rosenkranz et al. 2007). Specifically, professional pianists showed enhanced fMRI activity in not only primary motor, but also in the PMC and the SMA when listening to known melodies (Bangert et al. 2006; Baumann et al. 2007). Moreover, the PMC was also activated when passively listening to melodies that were trained during 5 days (Lahav et al. 2007).
In this context, the Music-Supported Therapy (MST) has been developed with the aim of inducing motor recovery after stroke (Schneider et al. 2007). MST requires an electronic keyboard and an electronic drum set to train fine (keyboard) and gross (drums) movements. Several studies have demonstrated significant benefits of MST in acute patients (Schneider, et al. 2007; Rodriguez-Fornells et al. 2012), exceeding those of dose-equivalent CIT (Schneider et al. 2010). Moreover, these effects also extend to chronic stroke (Rojo et al. 2011). MST is based on four principles: (i) massive repetition and exercising of simple finger and arm movements (Langhorne et al. 2011); (ii) auditory-motor coupling and integration, reinforcement of motor effects due to immediate auditory feedback (Bangert et al. 2006; Zatorre et al. 2007); (iii) shaping, adapting the training according to the individual progress; and (iv) emotion-motivation effects, due to the playfulness and emotional impact of music and the acquisition of a new skill.
Regarding these four principles, the hypothesis of auditory–motor coupling relies on the assumption that music performance is supported by rapid feedforward and feedback loops which coordinate auditory and motor information (e.g., an accurate mapping between a note and the motor movement required to play that note; Rodriguez-Fornells et al. 2012). Feedforward information (a model of the note to be played) might be transferred from the primary auditory cortex in the superior temporal gyrus (STG) to the PMC, in order to facilitate the well-trained motor responses associated to a particular note. On the other hand, an internal representation of the motor output being performed could travel back to the STG in order to evaluate its suitability to play a specific note. In an fMRI study in which healthy non-musicians listened to music, we found strong functional connections between premotor and supplementary motor regions, the STG and the inferior frontal gyrus (IFG; Rodriguez-Fornells et al. 2012). Interestingly, the SMA—an area which has been related to the learning, planning and production of motor sequences and motor control movement (Biswal et al. 1995; Picard and Strick 2001; Chen and Wise 1996)—emerged as a central hub of connectivity on the auditory motor network engaged by music listening (Rodriguez-Fornells et al. 2012).
Concerning the emotion-motivation effects of music, cortical plasticity can be enhanced by the motivational or behavioral relevance of the intervention (Buonomano and Merzenich 1998). In this sense, the emotional effects induced by music listening and learning might also aid the rehabilitation intervention by engaging the reward-learning network (Rodriguez-Fornells et al. 2012). Interestingly, passive music listening after stroke has also proven to induce improvements in several cognitive and mood domains (Särkämö et al. 2008, 2014).
The present study sought to explore the neurophysiological mechanisms involved in MST. With that aim and, as an extension of the previous studies in acute patients, we evaluated the effects of MST in a sample of twenty individuals with chronic stroke with slight to moderate upper-extremity hemiparesis. An extensive evaluation protocol was carried out, comprising functional and structural MRI, standard and kinematic motor assessment, neuropsychological and mood evaluation and transcranial magnetic stimulation (TMS; the results from the TMS and kinematic part have been presented in a different article; Amengual et al. 2013). A healthy control group matched for age, sex and education was evaluated also in two different time-points using the same battery of evaluations. The use of this control group is important in neuroimaging studies in order to control for repeated imaging testing (Johansen-Berg 2012).
Based on the hypothesis that auditory-motor coupling contributes to the beneficial effects of MST, we expected to observe an increase in functional connectivity and brain activity between auditory and motor regions after MST in the chronic stroke group, concomitant with no differences in the control group. Following previous positive effects of MST in acute stroke patients (Schneider et al. 2007; Schneider et al. 2010; Rodriguez-Fornells et al. 2012; Rojo et al. 2011) we also expected a functional improvement of the affected arm, together with a decrease of activation of the contralesional sensorimotor and premotor regions. Finally, based on the general effects of music listening on cognitive and emotional functions (Särkämö and Soto 2012; Särkämö et al. 2008), we also anticipated effects of therapy on cognitive and emotional domains in the chronic stroke group. Thus, a beneficial effect elicited by this therapeutic approach over motor function as well as over mood state was expected.
Material and methods
Participants
Twenty right-handed individuals with chronic stroke (17 men, 59.1 ± 9.04 years old) participated in the present study. All study participants suffered from a slight to moderate impairment of motor function of one upper extremity resulting from a stroke (10 left-sided, 30.5 ± 25.2 months after stroke). Individuals with chronic stroke were recruited from Hospital Universitari de Bellvitge and Hospital de l’Esperança in Barcelona. The study was approved by the Ethics committee of the University of Barcelona and the Hospital Universitari de Bellvitge. All methods were carried out in accordance with the approved ethical guidelines. Written informed consent was obtained from all participants. The following inclusion criteria were applied: (i) hemiparesis resulting from a stroke (ischemic or hemorrhagic) at least 6 months before the enrolment into the study, (ii) age from 30 to 75 years, (iii) individuals with chronic stroke had to be able to move the affected arm and the index finger without help from the healthy side, achieving an upper score on the Medical Research Council (MRC) Scale for Muscle Strength above 3 (which reflects active movement against gravity), and (iv) an overall Barthel Index over 50 (maximum possible score 100). Study participants were excluded in case they met one of the following criteria: (i) prior or subsequent symptomatic stroke, (ii) severe perceptual or cognitive deficits revealed by neuropsychological testing (Mini-Mental State Examination score of 23 or less; Short Token test score of 28 or less; positive result in the Visual neglect Albert test) and (iii) previous expertise in playing music. Demographic and clinical information for the chronic stroke group are presented in Table 1.
Fourteen right-handed healthy participants (12 men, 56 ± 9.6 years old) with no history of previous stroke or other neuropsychiatric disorders served as a control group, which was matched in terms of gender, age and educational level with the chronic stroke group (overall school attendance: 9.4 ± 5.3 years for the chronic stroke group and 9.6 ± 5.7 years for the control group). None of the controls had previous expertise in playing music. Right-handedness of all participants in this study was assessed using the Edinburgh handedness inventory.
Procedures
The chronic stroke group received extensive cognitive, motor and MRI assessment prior and after the MST intervention. The control group was assessed twice as well, with the two sessions separated by the same interval of time (approximately 1 month and a half) as the two evaluations performed in the chronic stroke group. The motor, cognitive and mood assessments and the interventions were performed by different researchers. The intervention was carried out by neuropsychologist specialized in the use of musical training in neurorehabilitation. Although fidelity was not formally monitored, all participants received MST using a manualized protocol. However, the person administering the neuropsychological tests was not blind with respect to the pre/post condition.
Music-supported therapy (MST)
Each individual with chronic stroke received 20 MST sessions of 30 min over a 4 week period. In a previous study in which MST was first applied to a group of individuals with acute stroke (Schneider et al. 2007), 15 MST sessions of 30 min were administered to each participant, with significant behavioral improvements in speed, precision and smoothness of movements of the affected hand. Based on these results, in the present study we decided to extend the number of sessions from 15 to 20 in order to enhance the chances for an effect of the therapy. It is important to note that our participants were individuals with chronic stroke who, in spite of having received conventional rehabilitation therapies during the acute stage of their disease, still had motor deficits. Notice also that at the chronic stage, motor function is relatively stable and spontaneous behavioral gains have already reached a plateau level (Cramer 2008). However, although motor function is typically stable at this chronic stage, therapy-induced gains are still possible (Schaechter 2004). Two different input devices were used: a digital and portable keyboard (CTK-810/WK110, Casio Europe GmbH, Norderstedt, Germany) and an electronic drum set (Roland drum system, TD-6KW, Roland Corporation, Hamamatsu, Japan) comprising 8 pads (20 cm of diameter), to improve fine and gross motor movements, respectively. The drum pads (numbered from 1 to 8) were used to produce keyboard (G, A, B, C, D, E, F, G’) rather than drum-sounds. Every time a drum pad was hit, it produced a fixed keyboard note. In a similar vein, the keyboard was arranged in such a way that only 8 white keys (C, D, E, F, G, A, B, C’) could be played by the participant. This offered the advantage of an input device taxing fine motor skills (keyboard) and another taxing gross motor skills (drum set), while keeping the auditory output constant.
For drum training, study participants were seated on a chair without armrests in front of the 8 drum pads. Each exercise was first played by the therapist and was subsequently repeated by the individual with chronic stroke. Participants had to hit the different pads with the affected hand (using only the hand; no drum sticks were used). The therapist stood behind the participant and gave support for the affected extremity if necessary. Similarly, for keyboard training, study participants were seated in front of the keyboard with the therapist standing next to them (on the affected side). Again, an exercise was first performed by the therapist and then repeated by the participant. Physical support was given by the therapist when necessary (i.e. in case of more severe hemiparesis or in the first sessions). Depending on the affectation, the therapist helped the study participant by accompanying the movement of the most affected fingers, or by raising the hand by the wrist/elbow in order to allow the participant to do the fine movement of the fingers without wasting all the energy in the gross control of the arm.
Following previous guidelines (Schneider et al. 2007), a modular training with stepwise increase of complexity was used. The therapy was manualized and comprised different levels varying in the number of tones, materials (single tones, scales, parts of songs, songs), velocity and order of playing. As stated, the difficulty of training was adapted to the needs of each individual. Every participant started by playing single tones and only continued to the next level of difficulty when he/she was able to successfully complete this task. If not, the task was repeated. In the next levels, individuals were required to use an increasing number of pads/keyboard keys until they were able to play all eight tones in different sequences. The most complex levels required participants to play parts of popular songs with the affected hand. With regard to the songs, materials were adapted from the original version of the MST (which had been designed for a German population) to include popular Spanish music which was well-known to the participants. Thus, the songs were pre-selected by the investigators based on their familiarity. Indeed, all participants reported to be familiar with the musical pieces before the beginning of the therapy.
Motor function evaluation
To examine motor functions, the following tests were employed: (i) Action Research Arm Test (ARAT), which is used to test fine and gross manual dexterity of the upper extremities within four subtests: grasp, grip, pinch, and gross movement (maximum score, 57); (ii) Arm Paresis Score (APS) which includes seven simple tasks for the affected hand alone and both hands together (e.g., opening a jar of jam, drawing a line, drinking water from a glass; maximum score, 7); (iii) Box and Block Test (BBT) which measures gross manual dexterity and consists of a box with 2 compartments and 150 cubes. Study participants were requested to grasp one cube at a time and transport it from one compartment to the other within 1 min. Both, healthy and paretic extremities were evaluated; (iv) Nine Hole Pegboard Test (9HPT) which assesses fine motor dexterity and consists of picking up nine rods (32 mm long, 9 mm diameter) and placing them into holes of 10 mm diameter as fast as possible; (v) Barthel index, which measures performance of activities of daily living and mobility (maximum score, 100).
Neuropsychological evaluation
The neuropsychological battery included tests for global cognitive integrity, working memory, attention, verbal memory (parallel versions were applied in the different evaluations to minimize practice effects), executive functions, visual neglect, comprehension and speed of information processing.
Three cognitive screening tests were performed only before the first evaluation: the Mini-Mental State Examination to exclude dementia, the Short Token test to evaluate language comprehension, and the Visual neglect Albert test to evaluate visual neglect deficits.
Attention and working memory were evaluated with the digit span subtest from the Wechsler Adult Intelligence Scale III (WAIS-III). Verbal memory was assessed using the Rey Auditory Verbal Learning Test. Executive functions were evaluated with the color-word condition of the Stroop task (Stroop PC), an extra index (Stroop C-PC; calculated by subtracting the value of the color-word condition to the color naming condition) and the Trail Making test. Speed of processing was assessed with the color (Stroop C) and word (Stroop P) naming conditions of the Stroop task and with a computerized simple and complex reaction time task.
Mood and quality of life (QOL) evaluation
Mood and QOL were also evaluated in both individuals with chronic stroke and controls using the Beck Depression Inventory Scale, the Positive and Negative Affect Scale, and the apathy evaluation scale. The Stroke Specific Quality of Life Scale, the Health survey questionnaire SF36 and the Self-Assessment Manikin Scale (daily evaluation of mood) were administered to the chronic stroke group only.
Statistical analysis
Statistical analysis was performed using SPSS 18.0 software (SPSS Inc, Chicago, USA). The significance of demographic differences between individuals with chronic stroke and controls were tested with the Pearson chi-square test (2 × 2 tables) for nominal variables or with t-tests for quantitative variables. Between group and within-group differences (post-treatment vs. pre-treatment) in neuropsychological and motor evaluation tests and Mood and QOL questionnaires were analyzed using t-tests (two-independent sample t-test for between-group differences, and paired sample t-test for within-group differences). To measure the recovery in the cognitive domains due to the effect of the therapy, a mixed 2 × 2 repeated measures analysis of variance (ANOVA) with Time-Point as a within-subjects factor (first and second evaluation) and Group as a between-subjects factor (chronic stroke and control) was also used. We did not use ANOVAs for the motor results due to the presence of ceiling effects in the control group. To try to control for the effect of the variability in the number of individuals in each group, non-parametric Mann–Whitney U tests were also calculated (working on the session differences when needed) for behavioral data comparing the chronic stroke and control groups.
MRI experimental design
Three individuals with chronic stroke were not included in the MRI protocol due to MRI incompatibilities, two were unable to perform the MRI experiment due to claustrophobia, and one disagreed to be included in the MRI protocol. Thus, fourteen of the individuals with chronic stroke and all 14 participants from the control group were examined twice.
Two different paradigms were employed. First, a Motor task which required sequential movements with the index and middle fingers of both hands was used. The task consisted of four active blocks of 20 s of hand movement and 20 s of rest for the left hand, and another 4 for the right hand (i.e., an ABAB design with A being stimulation and B rest). This task has been previously used to induce robust motor cortex fMRI activity in a chronic stroke individual (Rojo et al. 2011). In this task, participants had one response pad in each hand, which included two buttons. They were requested to press one button with the index finger and the other with the middle finger alternatively. Participants had to repeat this two-button sequence at their own pace during the active motor blocks, alternating each hand across blocks. This sequence was selected due to its simplicity, in order to control for possible learning effects across scans. Before entering the scanner participants completed a training block to ensure that the task was done properly. The buttons in the pad were connected to LEDs outside the scanner. Thus, participants’ performance was monitored to ensure that the task was done properly and without mirror movements in the non-used hand during each active block. In the Music task, participants had to passively listen to short pieces (15 s of music followed by 15 s of rest) of familiar (trained during the rehabilitation therapy) and unfamiliar (not trained during rehabilitation therapy) songs. Three blocks of familiar and unfamiliar songs were randomly presented (e.g., ABCBCBAB, with A, B and C being familiar, rest and unfamiliar pieces, respectively). The musical pieces were counterbalanced between conditions. This task has been previously used to induce strong fMRI activity within auditory-motor areas both in a chronic stroke individual (Rojo et al. 2011) and also in healthy participants (Rodriguez-Fornells et al. 2012).
Data acquisition
Images were acquired with a 3 T whole-body MRI scanner (Siemens Magnetom Trio, Clinic Hospital, Barcelona). High resolution structural images [magnetization-prepared, rapid-acquired gradient echoes (MPRAGE), 240 slices, TR = 2300 ms, TE = 3 ms, 1 mm isotropic voxels] followed by functional images (echo planar T2*-weighted gradient echo sequence, TR = 2000 ms, TE = 29 ms, slice thickness = 4 mm, 3.5 × 3.5 mm in-plane resolution, no gap) were acquired. Each functional run consisted of 176 volumes for the Motor task and 94 for the Music task. Each volume comprised 32 axial slices aligned to the plane intersecting the anterior and the posterior commissure. Stimuli were played using the Presentation Software (www.neurobs.com) through MR compatible headphones, which helped to reduce scanner noise during rest periods, and MR-compatible goggles.
fMRI data analysis
Data were analyzed using the Statistical Parameter Mapping software (SPM8, Wellcome Department of Imaging Neuroscience, University College, London, UK, www.fil.ion.ucl.ac.uk/spm/). Preprocessing included realignment, segmentation, normalization and smoothing with an 8 mm Gaussian kernel. Unified Segmentation (Ashburner and Friston 2005) with medium regularization and cost function masking was applied (Brett et al. 2001). To define the cost function masks, N.R (who had previous experience in lesion definition in stroke; Rodriguez-Fornells et al. 2012; Rojo et al. 2011) created binary masks of the lesioned areas by manually depicting the precise boundaries of the lesion directly into the T1 image (Crinion et al. 2007; Andersen et al. 2010; Ripolles et al. 2012). The MRIcron software package (http://www.cabiatl.com/mricro/mricron/index.html) was used to do the lesion tracing (Rorden and Brett 2000). This cost function masks in native space were used, along with, Unified Segmentation, to obtain the registration parameters needed to normalize the participants’ structural and functional MRI images to MNI space. In addition, the lesion masks defined in native space (containing 1 for lesion and 0 for healthy tissue) were also normalized. Finally, these normalized binary lesion maps were added together to generate an overlap map. We flipped the functional and anatomical data of chronic stroke individuals with right-hemispheric lesions about the mid-sagittal plane in order to perform group analyses with all 14 participants (Cheng et al. 2014; Nair et al. 2007; Wei et al. 2013). This basically allowed us to consider all chronic individuals as having had a left-hemispheric stroke.
For both the Motor and the Music tasks, the statistical evaluation was based on a least-square estimation using the general linear model. The lesioned areas were included in the fMRI analysis. The different conditions were modeled with a box-car regressor waveform convolved with a canonical hemodynamic response function. Data were high-pass filtered (to a maximum of 1/128 Hz) and serial autocorrelations were estimated using an autoregressive model [AR(1) model]. Confounding factors from head movement were also included in the model. Thus, a block-related design matrix was created including the conditions of interest (Motor task: Sequence Affected hand, Sequence Unaffected hand and Rest; Music task: Trained music, Untrained music and Rest). After model estimation, main effects for each condition were calculated. For the Motor task, two main contrasts were calculated: Sequence Affected hand vs. Rest and Sequence Unaffected hand vs. Rest. For the Music Task we explored two main contrasts: Music (Trained and Untrained) vs. Rest, to check for general musical effects; and Trained vs. Untrained music, to check for specific effects of the MST intervention.
First level contrasts were entered into a 2 (Group) × 2 (Time-Point) ANOVA (motor: Sequence Unaffected hand vs. Rest and Sequence Affected hand vs. Rest; music: Music vs. Rest and Trained vs. Untrained music). Thus, four 2 (Group) × 2 (Time-Point) ANOVAs were computed. Results were restricted to four ROIs based on previous studies on auditory-motor coupling (Bangert et al. 2006; Lahav et al. 2007; Zatorre et al. 2007), which included: (i) superior and middle temporal gyri and Heschl gyrus, (ii) inferior and middle frontal gyrus (iii) SMA and (iv) the precentral and postcentral gyri. ROIs were created for both the affected and the healthy hemisphere using the toolbox Wfu pickatlas (Maldjian, et al. 2003; Maldjian et al. 2004). All activations are reported in Tables at an uncorrected p < 0.005 threshold with 20 voxels of cluster extent. It has been shown that combined intensity and cluster size thresholds such as the ones used in this manuscript produce a desirable balance between false positives and false negatives (Types I and II errors, respectively; Lieberman and Cunningham 2009). Thus, only brain structures identified in Tables at the selected threshold (p < 0.005, k = 20) were labeled in Figures and are further commented on the manuscript. Only for illustrative purposes, Figures were created using a p < 0.01 uncorrected threshold. Anatomical and cytoarchitectonical areas were identified using the Automated Anatomical Labeling Atlas (Tzourio-Mazoyer et al. 2002) included in the xjView toolbox (http://www.alivelearn.net/xjview8/).
Functional connectivity
Functional connectivity for the fMRI music dataset was assessed using a ROI-based analysis on both hemispheres. Four different regions were selected per hemisphere, as before, based on previous studies (Bangert et al. 2006; Lahav et al. 2007; Zatorre et al. 2007), although for this functional connectivity analysis the areas were more constrained: (i) primary auditory cortex (including only Brodmann areas 41 and 42 and Heschl gyrus), (ii) inferior frontal gyrus , (iii) SMA and (iv) the precentral gyrus which—based on increased evidence emerging from both animal and human research indicating that reorganization following injury to primary motor areas might involve the premotor cortex (Kantak et al. 2012)—included premotor and primary motor areas (Brodmann areas 6 and 4). The activation pattern obtained for the Trained Music vs. Rest contrast of each group and each fMRI session was masked with the defined ROIs. Individual time course series were extracted for voxels surviving a p < 0.05 uncorrected threshold in each ROI. In this manner, we selected only the voxels showing an effect in each participant, capturing the possible variability in activation between individuals. Subsequently, the time course of each voxel was low-pass filtered (cutoff = 0.08 Hz) and its linear trend was removed. Finally, the extracted time courses from each ROI were averaged (computing the mean value of all voxels within each ROI at each of the 94 scanned volumes for the Music task, yielding 94 mean BOLD values), obtaining 4 (PAC, IFG, SMA, PRG) mean BOLD responses per fMRI session and hemisphere. Then, using the MATLAB toolbox for functional connectivity (Zhou et al. 2009), correlations between the mean BOLD response of each pair of ROIs were calculated (Prat et al. 2007) and subsequently transformed to a normal distribution using Fischer’s z transform (Barber et al. 2012; Lopez-Barroso et al. 2013). Six different measures of the strength and synchrony of the connection between the selected areas per hemisphere were obtained (PAC-SMA, PAC-IFG, PAC-PRG, PRG-SMA, PRG-IFG, IFG-SMA).
A 6 (Connection) × 2 (Group) × 2 (Time-Point) ANOVA was calculated for each hemisphere. We focused on a Group × Time-Point interaction that might show that functional connectivity was increased for the affected hemisphere after MST therapy. For significant interactions and in order to assess between which specific areas of the affected hemisphere functional connectivity was significantly enhanced after MST, paired t-tests were planned for each correlation pair in the chronic stroke group. An FDR-corrected p < 0.05 threshold was used to control for those multiple paired t-tests.
Results
For the clinical, motor, cognitive and mood and quality of life data, results are given, unless otherwise noted, for 20 individuals with chronic stroke and 14 matched controls. The fMRI results are provided for 14 chronic stroke individuals (three study participants with stroke were not included in the MRI protocol due to MRI incompatibilities, two were unable to perform the MRI experiment due to claustrophobia and one disagreed to be included in the MRI protocol) and 14 matched healthy controls.
Clinical and lesion data
Table 1 shows demographics and clinical data. There were no statistically significant differences between chronic stroke and control groups in age [t(32) = 0.943, p > 0.353; Mann–Whitney U = 113, p > 0.344], education [t(32) = −0.126, p > 0.900; Mann–Whitney U = 137.5, p > 0.922] or gender [X 2(1) = 0.003, p > 0.954].
Motor evaluation
In individuals with chronic stroke, significant improvements between post and pre therapy evaluations were found for the Box and Block Test [BBT; t(18) = 3.18, p < 0.005, one stroke participant did not complete both the pre and post testing due to fatigue] and the global score of the Action Research Arm Test [ARAT; t(19) = 3.853, p < 0.001] and three of its subtests [grasp, t(19) = 3.067, p < 0.006; grip, t(19) = 2.399, p < 0.027; gross movement, t(19) = 3.390, p < 0.003; see Fig. 1a]. The result for the pinch subtest approached significance [t(19) = 2.030, p > 0.057]. For the ARAT test, it is considered that a change of 10 % (5.7 points) of the maximum score (57 points) can be considered clinically relevant (van der Lee et al. 2001). However in six out of the twenty chronic stroke participants, the minimal clinically importance difference (MCID) could not be applied, as they scored above or equal to 52 points in the ARAT test performed pre intervention. Eight out of the fourteen remaining chronic stroke participants did obtain the MCID for the ARAT test. The Arm Paresis Score (APS) and the Nine Hole Pegboard Test (9HPT) did not show significant improvements. Regarding the control group, no statistical differences were observed between evaluations (for APS and ARAT all control participants scored with maximum values).
a Results of motor behavior tests pre and post-MST (mean, standard error of the mean, SEM) for the chronic stroke (SG) and control group (CG). Motor tests include: Nine Hole Pegboard Test (9HPT), Box and Block Test (BBT), Arm Paresis Score (APS) and Action Research Arm Test (ARAT). A significant improvement after therapy was observed in the BBT and ARAT for the chronic stroke group. Significant differences between groups were also observed before and after therapy in the 9HPT, the BBT and the ARAT test (see Results). No SEM is shown in controls for the APS and ARAT tests because all the participants scored with maxim values (ceiling effect). b Daily assessments of mood (pleasure and arousal) during each therapy session (intra-individual normalized Z mean values ± SEM) for the chronic stroke group. A significant improvement was observed along the course of the therapy. c Results of the Mood questionnaires (Mean, SEM) for the chronic stroke and control group. A significant reduction in depressive symptoms post-MST (2nd evaluation) is observed in the chronic stroke group when compared to pre-therapy evaluations (1st evaluation). A significant improvement was also observed for the positive affect but not the negative affect scales (PANAS). No differences were observed for the control group. SG chronic stroke group, CG control group. ***p < 0.001, **p < 0.005
Prior to the intervention, there were significant differences between chronic stroke and control participants for all motor tests, except the APS [9HPT, t(32) = −5.584, p < 0.001, Mann–Whitney U = 2.5, p < 0.001; BBT, t(31) = −7.488, p < 0.001, Mann–Whitney U = 7 , p < 0.001; ARAT, t(32) = −3.695, p < 0.001, Mann–Whitney U = 21, p < 0.001; APS, t(32) = −1.914, p > 0.065, Mann–Whitney U = 98, p > 0.148; Fig. 1a]. After therapy, significant group differences remained for the 9HPT [t(32) = −5.059, p < 0.001, Mann–Whitney U = 14, p < 0.001], the BBT [t(31) = −6.959, p < 0.001, Mann–Whitney U = 8.5, p < 0.001] and the ARAT [t(32) = −2.775, p < 0.009, Mann–Whitney U = 28, p < 0.001]. The scores for the APS remained non-significant [t(32) = −1.49, p > 0.146, Mann–Whitney U = 105, p > 0.231].
Cognitive performance
There were significant improvements in the chronic stroke group after the therapy in the domain of attention, speed of processing and rate of learning (see Table 2). In the control group no differences were observed between sessions. For several measures, significant group differences emerged between individuals with chronic stroke and controls in the 2 × 2 ANOVA reflecting a general cognitive impairment in the chronic stroke group (see Table 2, group effect; non-parametric analyses also showed the same significant group differences, see Supplemental Table 1). A significant Group × Time interaction was found for the rate of learning of the Rey Auditory Verbal Learning Test (RAVLT; also significant for the non-parametric analysis, see Supplemental Table 1).
Mood and quality of life (QOL)
The Self-Assessment Manikin Scale (SAM, daily evaluation of mood) in individuals with chronic stroke during the therapy (see Fig. 1b) showed a significant effect of MST sessions in arousal [linear trend: F(1361) = 31.7, p < 0.001] and valence [linear trend, F(1361) = 9.50, p < 0.006]. A positive effect of therapy on mood was corroborated by the Beck Depression Inventory [BDI; t(17) = −3.532, p < 0.003, two stroke participants did not complete the pre or post testing due to fatigue] and the positive affect items of the Positive and Negative Affect Scale [PANAS; t(17) = 3.715, p < 0.002, two stroke participants did not complete the pre or post testing due to fatigue; Fig. 1c], with an increase in the chronic stroke group. The Stroke Specific Quality of Life Scale (SS-QOL), showed significant pre-post differences on the domain of Familiar Role [t(15) = 2.515, p < 0.024] and Personality [t(15) = 2.8, p < 0.013, four stroke participants did not complete the pre or post testing due to fatigue]. No significant differences were found in the apathy evaluation scale and in health survey questionnaire SF36. No significant differences were obtained in the control group in any test (Fig. 1c).
fMRI motor task
Participants completed a simple motor task inside the scanner (sequentially tapping with their index and middle finger a two-button pad) with the left or right hand (only one hand was used during each active motor block). In the control group, the motor Sequences > Rest contrast revealed, for both hands, activation of the supplementary motor area (SMA) and the precentral and postcentral gyri contralateral to the movement, as well as small portions of the ipsilateral precentral gyrus (Fig. 2a and Supplemental Table 2). In individuals with chronic stroke, movements of the unaffected hand, led to similar activations as those seen in controls. However, a more bilateral pattern of activity was found for the affected hand, as, prior to therapy, extensive activations were bilaterally present in the pre- and postcentral gyri (Fig. 2b). While for the control group no significant differences were found between the first and the second session of either hand, chronic stroke individuals showed decreased fMRI activity in the contralesional precentral gyrus [Brodmann Area (BA) 6] of the affected hand [significant 2 (Group) × 2 (Time-Point) interaction: t(26) = 3.34; 22 voxels; MNI coordinates = 50–12 58; see Fig. 2c]. No significant interaction was found for the unaffected hand. This results show that activity in the contralesional precentral gyrus was significantly reduced after the MST intervention.
Enhanced group-level fMRI-signals for the motor Sequence versus Rest contrast of the affected hand. Neurological convention is used. Data from chronic stroke individuals with right-hemispheric lesions were flipped to the left. All statistical maps are thresholded at a p < 0.01 uncorrected threshold for illustrative purposes. Only areas reported in Tables at a p < 0.005 uncorrected threshold are labeled in this Figure, with MNI coordinates at the bottom left of each slice. a Right hand motor activations for the control group during the first and second time-points (see also Supplemental Table 2). b Motor activations for the affected limb (right hand) for the chronic stroke group before and after MST (see also Supplemental Table 2). A lesion overlap map indicating the number of chronic stroke individuals showing damage at a particular voxel is shown in purple-blue-green (there were no voxels in which more than 4 participants had a lesion). c Group (Chronic Stroke > Control) × Time-Point (Pre-MST > Post-MST) interaction showing that the motor activity induced at the right precentral gyrus (ipsilateral to the movement) was reduced in individuals with chronic stroke due to MST intervention. Bar graphs on the right indicate mean beta values with standard error of the mean (grey for chronic stroke, white for controls). Prec precentral gyrus, Post postcentral gyrus, SMA supplementary motor area, MST music supported therapy, L left hemisphere
fMRI music listening
Inside the scanner, participants listened to short pieces of songs trained or not trained during the MST intervention (for the control group, no songs were trained and thus, no differences between trained and untrained activations were expected). For the control group, listening to Music (Trained and Untrained) vs. Rest elicited a bilateral activation pattern comprising auditory (superior temporal and Heschl gyri) and motor areas (precentral gyrus, premotor cortex, SMA, postcentral gyrus) as well as the inferior frontal gyrus (see Fig. 3a and Supplemental Table 3) at both time-points (no differences were found between sessions). However, a different pattern was observed in the chronic stroke group: although activations in auditory areas were comparable to those of controls for the first evaluation, no activity was found for the precentral gyrus of the affected hemisphere and the SMA bilaterally (Fig. 3b, Supplemental Table 3). Nonetheless, the Music (Trained and Untrained) vs. Rest contrast after the MST intervention showed activations in the precentral gyrus and the IFG of the affected hemisphere as well as the SMA bilaterally (Fig. 3b, Supplemental Table 3). Moreover, when assessing the Trained > Untrained contrast after MST intervention, the chronic stroke group was the only one showing significant activations in motor-related areas (precentral gyrus, premotor cortex, SMA), auditory areas and the IFG in both the affected and unaffected hemispheres (Fig. 3c, Table 3).
Enhanced group-level fMRI-signals for the music task. Neurological convention is used. Data from chronic stroke individuals with right-hemispheric lesions were flipped to the left. All statistical maps are thresholded at a p < 0.01 uncorrected threshold for illustrative purposes. Only areas reported in Tables at a p < 0.005 uncorrected threshold are labeled in this Figure, with MNI coordinates at the bottom left of each slice. a Music (Trained and Untrained) > Rest contrast for the first and second time-points of the control group (see also Supplemental Table 3). b Music (Trained and Untrained) > Rest contrast for the pre and post therapy sessions of the chronic stroke group (see also Supplemental Table 3). c Trained > Untrained music contrast for the post MST session of the chronic stroke group (the only one showing significant effects, see also Table 3). Prec precentral gyrus, SMA supplementary motor area, IFG inferior frontal gyrus, STG superior temporal gyrus, HG heschl gyrus, MST music supported therapy, L left hemisphere
To test whether the extensive training of musical pieces during the therapy had specific effects in individuals with chronic stroke compared to controls, we carried out a 2 × 2 factorial analysis. For the Music (Trained and Untrained) > Rest contrast, only four voxels at the precentral gyrus of the affected hemisphere were found [BA 6; t(26) = 3.05, p < 0.0026; 4 voxels; MNI coordinates = −64 0 30]. However, regarding the Trained > Untrained music contrast, while no significant differences between sessions were found for the control group, chronic stroke individuals showed enhanced fMRI activity after MST in auditory and motor regions, mainly in the affected hemisphere [significant 2 (Group) × 2 (Time-Point) interaction in the precentral gyrus (BA 6), the primary auditory cortex (STG), the inferior frontal gyrus and the SMA of the affected hemisphere, and in the primary auditory cortex (STG) of the non-affected hemisphere; see Fig. 4 and Table 3]. Thus, music training induced a clear increase in the fMRI activation of auditory and motor areas of the affected hemisphere in individuals with chronic stroke. As no changes were observed in the control group, test repetition cannot account for the present findings.
Group (Chronic Stroke > Control) × Time-Point (Post-MST > Pre-MST) interaction for the Trained > Untrained music contrast, showing MST interventional effects. Neurological convention is used. Data from chronic stroke individuals with right-hemispheric lesions were flipped to the left. Bar graphs indicate mean beta values with standard error of the mean (grey for chronic stroke, white for controls). All statistical maps are thresholded at a p < 0.01 uncorrected threshold for illustrative purposes. Only areas reported in Tables at a p < 0.005 uncorrected threshold are labeled in this Figure, with MNI coordinates at the bottom left of each slice. Prec precentral gyrus, SMA supplementary motor area, IFG inferior frontal gyrus, HG heschl gyrus, MST music supported therapy, L Left hemisphere
Functional connectivity in the auditory-motor network
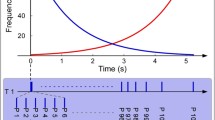
Functional connectivity was assessed using a region of interest (ROI) analysis on both hemispheres. Four different regions were selected (i) primary auditory cortex (PAC), (ii) IFG, (iii) SMA and (iv) the precentral gyrus (PRG). Results are shown in Fig. 5. For the unaffected hemisphere, no significant Group × Time-Point interaction was found [F(1,26) = 0.332, p > 0.57]. However, while no differences between sessions were found for the control group, chronic stroke individuals showed a significant increase in functional connectivity of the affected hemisphere [2 (Group) × 2 (Time-Point) interaction: F(1,26) = 10.360, p < 0.003]. This suggests (see third row in Fig. 5) that there was a general increment in functional connectivity in the affected hemisphere of the chronic stroke group after MST therapy. Indeed, paired t-tests FDR-corrected for multiple comparisons showed that functional connectivity was significantly higher post-therapy for SMA-PRG [t(13) = 4.13, p < 0.002], PRG-IFG [t(13) = 3.22, p < 0.007] and also PAC-SMA [t(13) = 2.59, p < 0.022] in the affected hemisphere of the chronic stroke group.
Mean functional connectivity (Fisher’s z-transformed) within the auditory-motor network (selected ROIs: SMA—supplementary motor area; PRG precentral gyrus, IFG inferior frontal gyrus, PAC primary motor cortex). Data from chronic stroke individuals with right-hemispheric lesions were flipped to the left. Results are shown for both hemispheres (affected hemisphere on the left column; unaffected hemisphere on the right) and time-points (dashed line for pre-MST/time-point 1; solid line for post-MST/time-point 2) of the control group (first row), and the chronic stroke group (second row). The connections showing a significant increase in functional connectivity after MST therapy are depicted in red. The third row shows the mean functional connectivity for each group and time-point averaged by all connections. Notice the increase of functional connectivity in the different auditory-motor pathways of the affected hemisphere involved in music listening in the chronic stroke group (bottom-left). L left hemisphere, R right hemisphere. ***p < 0.005, **p < 0.01, *p < 0.05
As an interaction effect could be either due to a dysfunctional connectivity in the individuals with chronic stroke prior to the therapy or to a genuine effect of MST (which only the chronic stroke group received) on connectivity, two-sample t-tests between groups were carried out for the two time-points, only for the affected hemisphere. Before therapy, functional connectivity was significantly lower in individuals with chronic stroke for SMA-PRG [t(26) = 3.50, p < 0.002], PRG-IFG [t(26) = 3.74, p < 0.001] and PAC-IFG [t(26) = 2.84, p < 0.01]. In contrast, no significant differences were observed between controls and individuals with chronic stroke after the MST intervention on any connection, suggesting that, in the individuals with chronic stroke, a dysfunctional auditory-motor network was restored to normal functional levels after MST therapy.
Discussion
In the present study, we investigated the changes in brain activity observed after the application of MST in a group of individuals with chronic stroke with slight to moderate motor residual deficits. First of all, chronic stroke individuals showed significant improvement in motor and cognitive function and also a reduction in depressed and negative mood symptoms after the MST therapy (see Fig. 1). Interestingly, when listening to music (trained and untrained) after MST, individuals with chronic stroke showed enhanced fMRI activity in the premotor cortex (PMC) and the SMA (see Fig. 3b). Furthermore, also after MST and for the musical pieces that had been trained compared to those which had been not, chronic stroke participants showed enhanced fMRI activity in several auditory and motor regions, replicating previous findings from studies in healthy participants (see Figs. 3c and 4; Bangert et al. 2006; Lahav et al. 2007). In addition, activity in motor regions ipsilateral to the affected limb (when participants performed a motor task) was significantly reduced after the application of the MST (see Fig. 2). Finally, the increased functional connectivity observed in the chronic stroke group for the auditory-motor network after MST, suggests that the therapy restored its default dynamics (Fig. 5). Crucially, no differences between sessions were seen in the control participants with regard to the activation of auditory and motor regions (including the superior temporal lobe, ventral PMC, SMA, sensorimotor areas and the IFG), or in terms of functional connectivity when listening to music (Fig. 5, top row). It is important to note that the described co-activation of motor and auditory areas reported in healthy individuals with no previous expertise in playing music, replicates previous results (Bangert et al. 2006; Rodriguez-Fornells et al. 2012). It has to be kept in mind that in this study, we have used songs well-known to all participants since their early childhood. For such songs, strong motor representations (e.g., clapping, dancing, singing) can be assumed (with the corresponding enhancement of BOLD activity in these areas), even if a participant is not experienced with playing music.
The functional connectivity analysis of the Music task showed that, in individuals with chronic stroke, connectivity between three pairs of regions changed significantly after the therapy: SMA-PRG, PRG-IFG and PAC-SMA (Fig. 5). Interestingly, the SMA and the precentral gyrus were the regions showing the most prominent MST effects in our study (Figs. 3c, 4 and 5). The SMA, located in the medial aspect of Brodmann’s area 6 and extending to the medial wall, has been related to the selection, initiation, planning, production and both implicit and explicit learning of motor sequences and also to bimanual motor control (Picard and Strick 2001; Hikosaka et al. 1996; Penhune and Steele 2012; Chen and Wise 1996). Moreover, the SMA is directly connected to the primary motor and premotor cortices and has direct connections to motor neurons of the corticospinal tract (Dum and Strick 1991; Bates and Goldman-Rakic 1993). The involvement of premotor regions and the SMA in the reorganization of the sensorimotor cortex observed in this manuscript is corroborated by animal studies on the effects of brain damage in functional reorganization (Dancause et al. 2005; Nudo et al. 1996). For example, it has been observed that primary motor damage can provoke both the diversion of fibers and also the growth of novel brain connections (intracortical sprouting) from the ventral premotor cortex to the primary somatosensory cortex (Dancause et al. 2005), thus providing a substrate for motor functional recovery. This rewiring and remapping of motor representations might be especially important in new training experiences, as it is the case in music learning (Wan and Schlaug 2010).
Our results are also in accord with previous studies showing that improved hand function after rehabilitation therapy is associated with increased activation of ipsilesional motor areas and decreased activation in contralesional regions during movement of the affected hand (Johansen-Berg et al. 2002; Marshall et al. 2000; Dong et al. 2006). Indeed, the chronic stroke group in our sample showed a decrease in contralesional activation of motor and neighboring regions after MST (see Fig. 2b and c) and an improvement on motor tests such as the ARAT and BBT. Importantly, these improvements in motor function are in agreement with previous studies applying MST in subacute stroke patients (Schneider et al. 2007; Schneider et al. 2010; Grau-Sanchez et al. 2013). There is a complex relation between impairment and function in stroke rehabilitation, where impairment usually refers to the symptom at the level of the body structure (i.e., the paresis affecting the mobility of the upper extremity) and function refers to the limitations that the individual with stroke may face when performing specific activities (i.e. the participant cannot move a cube with the affected upper extremity). While in the subacute phase both improvements in function and impairment have been reported (Langhorne et al. 2011), in chronic stages the situation might differ. Indeed, it has been suggested that treatment at later stages may have a greater impact in the improvement of function rather than in the reduction of impairment (Krakauer et al. 2012; Kitago et al. 2013). In accord, in the present study we report improvements in function (measured with the ARAT and the BBT). However, in a previous study using the same cohort of participants (Amengual et al. 2013), we found that participants improved in smoothness and frequency of the movement with the affected hand after MST. Therefore, although we expected MST to mostly improve function, we also found a slight amelioration in impairment, as evidenced by the analysis of movement performance (Amengual et al. 2013).
Finally, recent studies have demonstrated how music influences overall mood and cognitive functions in neurological and healthy participants (Thaut et al. 2005; Särkämö et al. 2014; Särkämö and Soto 2012; Särkämö et al. 2008). In the present study, improvements in cognitive function and a reduction of depressed and negative mood symptoms were observed in individuals with chronic stroke after MST. On the basis of the current study design, we are unable to prove whether these effects were due to the specific characteristics of MST, or were related to more general aspects of the study, such as the interaction with the therapists and the research team. It is important to note, however, that the benefits of music in neurological patients for cognitive recovery and elevation of mood has convincingly been demonstrated (Särkämö et al. 2013).
Our results confirm MST as a viable intervention to produce behavioral, motor and mood improvements—accompanied by changes in brain activity and an increase of functional connectivity between auditory and motor regions—in individuals with chronic stroke. There are three reasons to assume that these changes were induced by MST: i) MST was the only intervention our study participants received; ii) it is unlikely that the reported changes come from spontaneous recovery, as our sample included individuals with chronic stroke (30.5 ± 25.2 months had elapsed since the stroke occurred) where spontaneous behavioral gains have generally reached a plateau (Cramer 2008). Thus, the chronic stage represents a stable phase where changes in brain and motor function are more likely to be associated to the effects of the therapy than to spontaneous recovery (Schaechter 2004); and iii) the results of the healthy control group account for any changes induced by task repetition or by the mere effect of time. On the other hand, although we suggest—given the reported neuroimaging data and especially the functional connectivity results—that the mechanism behind the participants’ recovery could be based on auditory-motor coupling, we cannot unambiguously prove this claim. First, we were unable to directly link (e.g., with music neuroimaging-motor improvement correlations) increases in auditory and motor neural activity during passive listening with motor improvements, probably due to the lack of a large sample within the chronic stroke group. In addition, the lack of an additional stroke control group involved in a different neurorehabilitation program prevents us from ensuring that the mechanism behind the plastic effects observed was, indeed, the coupling between motor and auditory regions. In other words, it is possible that another motor therapy could induce plastic effects in the damaged motor regions so that, in turn, the normal dynamics of the auditory-motor network would be reestablished. Thus, it could be the case that participants who underwent other type of rehabilitation therapy could also show activity in motor, premotor and supplementary motor areas post-intervention when passively listening to music, even though their intervention was not based on stimulating the coupling of auditory and motor regions. Further studies, using for example a control stroke group receiving musical therapy but with a mute piano (Gatti et al. 2014), are needed to ensure which of the reported changes regarding brain activity, functional connectivity, motor behavior, mood and cognition are specifically induced by auditory-motor coupling.
This study also presents a set of limitations that precise further discussion. First, we included a relatively small sample of individuals with chronic stroke with considerable variability in lesion locations (in both left and right hemispheres) and lesion size. In addition, our stroke group was relatively young (mean age was 59 years). Interestingly, a recent review (Gaynor et al. 2014) found that the mean age of stroke participants undergoing rehabilitation studies was 64.3 years, almost 10 years younger than those seen by physicians globally. We speculate that the participants’ willingness or ability (due to the exclusion criteria) to participate in our study resulted in an age bias that is not uncommon in the stroke rehabilitation literature. For example, in a previous study of our group dealing with MST in acute stroke participants which used very similar inclusion and exclusion criteria, the mean age of the study participants was 58 and 54 years for the music and the control stroke group, respectively (Schneider et al. 2007). Further studies, mirroring the age of stroke patients treated in clinical daily practice, should also be conducted in order to replicate the current findings. Regarding the therapy, the number (20) and length (30 min) of the MST sessions is also a critical variable that can be manipulated in future research. In this study, MST has been applied individually but a modified version of the protocol could include sessions in group. Moreover, in a recent study, Villeneuve and colleagues (2014) introduced a new variation in the therapy as MST sessions at the medical center were combined with self-administered sessions performed at home. These modifications in the protocol could make MST more cost-effective. In order to improve participants’ engagement in the therapy, future studies may also consider the musical preferences of patients when selecting the songs trained during the MST. Besides, in our design we did not include a phenomenological qualitative interview aimed at assessing both participants’ experience and the therapeutic role of the interventionist (Forsblom et al. 2009). Subsequent studies should address this question, as the information obtained could ultimately lead to improvements in the way MST is applied. And finally, as stated above, the lack of a chronic stroke group engaged in other rehabilitation therapy limits the impact of our results, as we cannot ensure that audio-motor coupling was the neural mechanism responsible for the reported effects. Future studies using a 3-group design (healthy individuals, chronic stroke with MST, chronic stroke without MST) will be crucial to clearly characterize the neural mechanisms behind MST. Thus, the effects of MST should be studied by doing clinical trials and comparing this treatment to other available therapies (Francois et al. 2015). Well-designed experimental studies and randomized clinical trials will help to provide robust evidence about the specific benefits of MST in the recovery of motor deficits after a stroke. In order to transfer this knowledge to the clinical practice, systematic reviews on the topic (Bradt et al. 2010) are necessary in order to include music therapy as a recommended treatment in international guidelines of stroke rehabilitation (see for an interesting discussion, Magee and Stewart 2015).
In conclusion, this study further strengthens the neurobiological basis of MST by (i) showing its effectiveness in individuals with chronic stroke, (ii) demonstrating an effect of MST on motor-related brain function (i.e. reduction of contralesional activity), similar to other effective neurorehabilitation regimes (iii) showing a MST-induced enhancement in fMRI activity in auditory and motor areas and an increase in functional connectivity among several regions of the auditory-motor network (iv) suggesting that MST has additional non-specific effects on cognitive performance and mood.
References
Amengual, J. L., Rojo, N., de Las Veciana, H. M., Marco-Pallares, J., Grau-Sanchez, J., Schneider, S., et al. (2013). Sensorimotor plasticity after music-supported therapy in chronic stroke patients revealed by transcranial magnetic stimulation. PLoS.One, 8, e61883.
Andersen, S. M., Rapcsak, S. Z., & Beeson, P. M. (2010). Cost function masking during normalization of brains with focal lesions: still a necessity? NeuroImage, 53, 78–84.
Ashburner, J., & Friston, K. J. (2005). Unified segmentation. NeuroImage, 26, 839–851.
Bangert, M., Peschel, T., Schlaug, G., Rotte, M., Drescher, D., Hinrichs, et al. (2006). Shared networks for auditory and motor processing in professional pianists: evidence from fMRI conjunction. NeuroImage, 30, 917–926.
Barber, A. D., Srinivasan, P., Joel, S. E., Caffo, B. S., Pekar, J. J., & Mostofsky, S. H. (2012). Motor “Dexterity”?: evidence that left hemisphere lateralization of motor circuit connectivity is associated with better motor performance in children. Cerebral Cortex, 22, 51–59.
Bates, J. F., & Goldman-Rakic, P. S. (1993). Prefrontal connections of medial motor areas in the rhesus monkey. Journal of Comparative Neurology, 336, 211–228.
Baumann, S., Koeneke, S., Schmidt, C. F., Meyer, M., Lutz, K., & Jancke, L. (2007). A network for audio-motor coordination in skilled pianists and non-musicians. Brain Research, 1161, 65–78.
Bernardi, N.F., Cioffi, M.C., Ronchi, R., Maravita, A., Bricolo, E., Zigiotto, L., et al., (2015). Improving left spatial neglect through music scale playing. Journal of Neuropsychology.
Biswal, B., Yetkin, F. Z., Haughton, V. M., & Hyde, J. S. (1995). Functional connectivity in the motor cortex of resting human brain using echo-planar MRI. Magnetic Resonance in Medicine, 34, 537–541.
Boyle, M. E., & Greer, R. D. (1983). Operant procedures and the comatose patient. Journal of Applied Behavior Analysis, 16, 3–12.
Bradt, J., Magee, W.L., Dileo, C., Wheeler, B.L., and McGilloway, E. (2010). Music therapy for acquired brain injury. Cochrane Database of Systematic Reviews, CD006787.
Brett, M., Leff, A. P., Rorden, C., & Ashburner, J. (2001). Spatial normalization of brain images with focal lesions using cost function masking. NeuroImage, 14, 486–500.
Buonomano, D. V., & Merzenich, M. M. (1998). Cortical plasticity: from synapses to maps. Annual Review of Neuroscience, 21, 149–186.
Chen, L. L., & Wise, S. P. (1996). Evolution of directional preferences in the supplementary eye field during acquisition of conditional oculomotor associations. Journal of Neuroscience, 16, 3067–3081.
Cheng, B., Forkert, N. D., Zavaglia, M., Hilgetag, C. C., Golsari, A., Siemonsen, S., et al. (2014). Influence of stroke infarct location on functional outcome measured by the modified rankin scale. Stroke, 45, 1695–1702.
Cohen, N. S. (1992). The effect of singing instruction on the speech production of neurologically impaired persons. Journal of Music Therapy, 29, 87–102.
Cohen, N. S., & Ford, J. (1995). The effect of musical cues on the nonpurposive speech of persons with aphasia. Journal of Music Therapy, 32, 46–57.
Cramer, S. C. (2008). Repairing the human brain after stroke: I. mechanisms of spontaneous recovery. Annals of Neurology, 63, 272–287.
Crinion, J., Ashburner, J., Leff, A., Brett, M., Price, C., & Friston, K. (2007). Spatial normalization of lesioned brains: performance evaluation and impact on fMRI analyses. NeuroImage, 37, 866–875.
Dancause, N., Barbay, S., Frost, S. B., Plautz, E. J., Chen, D., Zoubina, et al. (2005). Extensive cortical rewiring after brain injury. Journal of Neuroscience, 25, 10167–10179.
Dong, Y., Dobkin, B. H., Cen, S. Y., Wu, A. D., & Winstein, C. J. (2006). Motor cortex activation during treatment may predict therapeutic gains in paretic hand function after stroke. Stroke, 37, 1552–1555.
Dum, R. P., & Strick, P. L. (1991). The origin of corticospinal projections from the premotor areas in the frontal lobe. Journal of Neuroscience, 11, 667–689.
Feigin, V. L., Forouzanfar, M. H., Krishnamurthi, R., Mensah, G. A., Connor, M., Bennett, et al. (2014). Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet, 383, 245–254.
Forsblom, A., Laitinen, S., Sarkamo, T., & Tervaniemi, M. (2009). Therapeutic role of music listening in stroke rehabilitation. Annals of the New York Academy of Sciences, 1169, 426–430.
Francois, C., Grau-Sanchez, J., Duarte, E., & Rodriguez-Fornells, A. (2015). Musical training as an alternative and effective method for neuro-education and neuro-rehabilitation. Frontiers in Psychology, 6, 475.
Friston, K. J. (2011). Functional and effective connectivity: a review. Brain Connectivity, 1, 13–36.
Gaser, C., & Schlaug, G. (2003). Brain structures differ between musicians and non-musicians. Journal of Neuroscience, 23, 9240–9245.
Gatti, R., Tettamanti, A., Lambiase, S., Rossi, P., & Comola, M. (2014). Improving hand functional use in subjects with multiple sclerosis using a musical keyboard: a randomized controlled trial. Physiotheraphy Research International.
Gaynor, E. J., Geoghegan, S. E., & O’Neill, D. (2014). Ageism in stroke rehabilitation studies. Age and Ageing, 43, 429–431.
Grau-Sanchez, J., Amengual, J. L., Rojo, N., Veciana de Las, H. M., Montero, J., Rubio, F., et al. (2013). Plasticity in the sensorimotor cortex induced by music-supported therapy in stroke patients: a TMS study. Frontiers in Human Neuroscience, 7, 494.
Grefkes, C., & Fink, G. R. (2011). Reorganization of cerebral networks after stroke: new insights from neuroimaging with connectivity approaches. Brain, 134, 1264–1276.
Herdener, M., Esposito, F., di Salle, F., Boller, C., Hilti, C. C., Habermeyer, B., Scheffler, I., et al. (2010). Musical training induces functional plasticity in human hippocampus. Journal of Neuroscience, 30, 1377–1384.
Hikosaka, O., Sakai, K., Miyauchi, S., Takino, R., Sasaki, Y., & Putz, B. (1996). Activation of human presupplementary motor area in learning of sequential procedures: a functional MRI study. Journal of Neurophysiology, 76, 617–621.
Hurt, C. P., Rice, R. R., McIntosh, G. C., & Thaut, M. H. (1998). Rhythmic auditory stimulation in gait training for patients with traumatic brain injury. Journal of Music Therapy, 35, 228–241.
Hyde, K. L., Lerch, J., Norton, A., Forgeard, M., Winner, E., Evans, A. C., et al. (2009). Musical training shapes structural brain development. Journal of Neuroscience, 29, 3019–3025.
Johansen-Berg, H. (2012). The future of functionally-related structural change assessment. NeuroImage, 62, 1293–1298.
Johansen-Berg, H., Dawes, H., Guy, C., Smith, S. M., Wade, D. T., & Matthews, P. M. (2002). Correlation between motor improvements and altered fMRI activity after rehabilitative therapy. Brain, 125, 2731–2742.
Kantak, S. S., Stinear, J. W., Buch, E. R., & Cohen, L. G. (2012). Rewiring the brain: potential role of the premotor cortex in motor control, learning, and recovery of function following brain injury. Neurorehabilitation and Neural Repair, 26, 282–292.
Kitago, T., Liang, J., Huang, V. S., Hayes, S., Simon, P., & Tenteromano. (2013). Improvement after constraint-induced movement therapy: recovery of normal motor control or task-specific compensation? Neurorehabilitation and Neural Repair, 27, 99–109.
Krakauer, J. W., Carmichael, S. T., Corbett, D., & Wittenberg, G. F. (2012). Getting neurorehabilitation right: what can be learned from animal models. Neurorehabilitation and Neural Repair, 26, 923–931.
Lahav, A., Saltzman, E., & Schlaug, G. (2007). Action representation of sound: audiomotor recognition network while listening to newly acquired actions. Journal of Neuroscience, 27, 308–314.
Langhorne, P., Bernhardt, J., & Kwakkel, G. (2011). Stroke rehabilitation. Lancet, 377, 1693–1702.
Lieberman, M. D., & Cunningham, W. A. (2009). Type I and Type II error concerns in fMRI research: re-balancing the scale. Social Cognitive and Affective Neuroscience, 4, 423–428.
Lopez-Barroso, D., Catani, M., Ripolles, P., Dell’Acqua, F., Rodriguez-Fornells, A., & de Diego-Balaguer, R. (2013). Word learning is mediated by the left arcuate fasciculus. Proceedings of the National academy of Sciences of the United States of America, 110, 13168–13173.
Magee, W. L., & Davidson, J. W. (2002). The effect of music therapy on mood states in neurological patients: a pilot study. Journal of Music Therapy, 39, 20–29.
Magee, W. L., & Stewart, L. (2015). The challenges and benefits of a genuine partnership between music therapy and neuroscience: a dialog between scientist and therapist. Frontiers in Human Neuroscience, 9, 223.
Maldjian, J. A., Laurienti, P. J., Kraft, R. A., & Burdette, J. H. (2003). An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. NeuroImage, 19, 1233–1239.
Maldjian, J. A., Laurienti, P. J., & Burdette, J. H. (2004). Precentral gyrus discrepancy in electronic versions of the Talairach atlas. NeuroImage, 21, 450–455.
Marshall, R. S., Perera, G. M., Lazar, R. M., Krakauer, J. W., Constantine, R. C., & DeLaPaz, R. L. (2000). Evolution of cortical activation during recovery from corticospinal tract infarction. Stroke, 31, 656–661.
Meyer, M., Elmer, S., Baumann, S., & Jancke, L. (2007). Short-term plasticity in the auditory system: differential neural responses to perception and imagery of speech and music. Restorative Neurology and Neuroscience, 25, 411–431.
Munte, T. F., Altenmuller, E., & Jancke, L. (2002). The musician’s brain as a model of neuroplasticity. Nature Review Neuroscience, 3, 473–478.
Murray, C. J., Vos, T., Lozano, R., Naghavi, M., Flaxman, A. D., Michaud, C., et al. (2012). Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 380, 2197–2223.
Nair, D. G., Hutchinson, S., Fregni, F., Alexander, M., Pascual-Leone, A., & Schlaug, G. (2007). Imaging correlates of motor recovery from cerebral infarction and their physiological significance in well-recovered patients. NeuroImage, 34, 253–263.
Nudo, R. J., Wise, B. M., SiFuentes, F., & Milliken, G. W. (1996). Neural substrates for the effects of rehabilitative training on motor recovery after ischemic infarct. Science, 272, 1791–1794.
Nys, G. M., van Zandvoort, M. J., de Kort, P. L., Jansen, B. P., de Haan, E. H., & Kappelle, L. J. (2007). Cognitive disorders in acute stroke: prevalence and clinical determinants. Cerebrovascular Diseases, 23, 408–416.
O’Kelly, J., James, L., Palaniappan, R., Taborin, J., Fachner, J., & Magee, W. L. (2013). Neurophysiological and behavioral responses to music therapy in vegetative and minimally conscious States. Frontiers in Human Neuroscience, 7, 884.
Pantev, C., & Herholz, S. C. (2011). Plasticity of the human auditory cortex related to musical training. Neuroscience and Biobehavioral Reviews, 35, 2140–2154.
Penhune, V. B., & Steele, C. J. (2012). Parallel contributions of cerebellar, striatal and M1 mechanisms to motor sequence learning. Behavioural Brain Research, 226, 579–591.
Picard, N., & Strick, P. L. (2001). Imaging the premotor areas. Current Opinion in Neurobiology, 11, 663–672.
Prat, C. S., Keller, T. A., & Just, M. A. (2007). Individual differences in sentence comprehension: a functional magnetic resonance imaging investigation of syntactic and lexical processing demands. Journal Cognitive Neuroscience, 19, 1950–1963.
Rehme, A. K., Eickhoff, S. B., Wang, L. E., Fink, G. R., & Grefkes, C. (2011). Dynamic causal modeling of cortical activity from the acute to the chronic stage after stroke. NeuroImage, 55, 1147–1158.
Ripolles, P., Marco-Pallares, J., de Diego-Balaguer, R., Miro, J., Falip, M., Juncadella, et al. (2012). Analysis of automated methods for spatial normalization of lesioned brains. NeuroImage, 60, 1296–1306.
Rodriguez-Fornells, A., Rojo, N., Amengual, J. L., Ripolles, P., Altenmuller, E., & Munte, T. F. (2012). The involvement of audio-motor coupling in the music-supported therapy applied to stroke patients. Annals of the New York Academy of Sciences, 1252, 282–293.
Roger, V. L., Go, A. S., Lloyd-Jones, D. M., Benjamin, E. J., Berry, J. D., Borden, et al. (2012). Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation, 125, e2–e220.
Rojo, N., Amengual, J., Juncadella, M., Rubio, F., Camara, E., Marco-Pallares, et al. (2011). Music-supported therapy induces plasticity in the sensorimotor cortex in chronic stroke: a single-case study using multimodal imaging (fMRI-TMS). Brain Injury, 25, 787–793.
Rorden, C., & Brett, M. (2000). Stereotaxic display of brain lesions. Behavioural Neurology, 12, 191–200.
Rosenkranz, K., Williamon, A., & Rothwell, J. C. (2007). Motorcortical excitability and synaptic plasticity is enhanced in professional musicians. Journal of Neuroscience, 27, 5200–5206.
Särkämö, T., & Soto, D. (2012). Music listening after stroke: beneficial effects and potential neural mechanisms. Annals of the New York Academy of Sciences, 1252, 266–281.
Särkämö, T., Tervaniemi, M., Laitinen, S., Forsblom, A., Soinila, S., Mikkonen, et al. (2008). Music listening enhances cognitive recovery and mood after middle cerebral artery stroke. Brain, 131, 866–876.
Särkämö, T., Tervaniemi, M., & Huotilainen, M. (2013). Music perception and cognition: development, neural basis, and rehabilitative use of music. WIREs Cognitive Science, 4, 441–451.
Särkämö, T., Ripolles, P., Vepsalainen, H., Autti, T., Silvennoinen, H. M., Salli, et al. (2014). Structural changes induced by daily music listening in the recovering brain after middle cerebral artery stroke: a voxel-based morphometry study. Frontiers in Human Neuroscience, 8, 245.
Schaechter, J. D. (2004). Motor rehabilitation and brain plasticity after hemiparetic stroke. Progress in Neurobiology, 73, 61–72.
Schlaug, G. (2001). The brain of musicians. A model for functional and structural adaptation. Annals of the New York Academy of Sciences, 930, 281–299.
Schlaug, G., Jancke, L., Huang, Y., Staiger, J. F., & Steinmetz, H. (1995). Increased corpus callosum size in musicians. Neuropsychologia, 33, 1047–1055.
Schneider, S., Schonle, P. W., Altenmuller, E., & Munte, T. F. (2007). Using musical instruments to improve motor skill recovery following a stroke. Journal of Neurology, 254, 1339–1346.
Schneider, S., Munte, T. F., Rodriguez-Fornells, A., Sailer, M., & Altenmuller, E. (2010). Music-supported training is more efficient than functional motor training for recovery of fine motor skills in stroke patients. Music Perception, 27, 271–280.
Schulz, R., Braass, H., Liuzzi, G., Hoerniss, V., Lechner, P., Gerloff, et al. (2015). White matter integrity of premotor-motor connections is associated with motor output in chronic stroke patients. Neuroimage Clinical, 7, 82–86.
Schulze, K., Gaab, N., & Schlaug, G. (2009). Perceiving pitch absolutely: comparing absolute and relative pitch possessors in a pitch memory task. BMC Neuroscience, 10, 106.
Seither-Preisler, A., Parncutt, R., & Schneider, P. (2014). Size and synchronization of auditory cortex promotes musical, literacy, and attentional skills in children. Journal of Neuroscience, 34, 10937–10949.
Seitz, R. J., Hoflich, P., Binkofski, F., Tellmann, L., Herzog, H., & Freund, H. J. (1998). Role of the premotor cortex in recovery from middle cerebral artery infarction. Archives of Neurology, 55, 1081–1088.
Strait, D. L., & Kraus, N. (2014). Biological impact of auditory expertise across the life span: musicians as a model of auditory learning. Hearing Research, 308, 109–121.
Taub, E., Uswatte, G., & Elbert, T. (2002). New treatments in neurorehabilitation founded on basic research. Nature Review Neuroscience, 3, 228–236.
Thaut, M. H. (2015). The discovery of human auditory-motor entrainment and its role in the development of neurologic music therapy. Progress in Brain Research, 217, 253–266.
Thaut, M. H., McIntosh, G. C., Rice, R. R., Miller, R. A., Rathburn, J., & Brault, J. M. (1993). Effect of rhythmic auditory cuing on temporal stride parameters and EMG patterns in hemiparetic gait of stroke patients. Journal of Neurological Rehabilitation, 7, 9–16.
Thaut, M. H., McIntosh, G. C., Rice, R. R., Miller, R. A., Rathbun, J., & Brault, J. M. (1996). Rhythmic auditory stimulation in gait training for Parkinson’s disease patients. Movement Disorders, 11, 193–200.
Thaut, M. H., Peterson, D. A., & McIntosh, G. C. (2005). Temporal entrainment of cognitive functions: musical mnemonics induce brain plasticity and oscillatory synchrony in neural networks underlying memory. Annals of the New York Academy Sciences, 1060, 243–254.
Tzourio-Mazoyer, N., Landeau, B., Papathanassiou, D., Crivello, F., Etard, O., Delcroix, et al. (2002). Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. NeuroImage, 15, 273–289.
van der Lee, J. H., Beckerman, H., Lankhorst, G. J., & Bouter, L. M. (2001). The responsiveness of the action research Arm test and the Fugl-Meyer assessment scale in chronic stroke patients. Journal of Rehabilitation Medicine, 33, 110–113.
Villeneuve, M., Penhune, V., & Lamontagne, A. (2014). A piano training program to improve manual dexterity and upper extremity function in chronic stroke survivors. Frontiers in Human Neuroscience, 8, 662.
Wan, C. Y., & Schlaug, G. (2010). Music making as a tool for promoting brain plasticity across the life span. The Neuroscientist, 16, 566–577.
Wei, W., Bai, L., Wang, J., Dai, R., Tong, R. K., Zhang, Y., et al. (2013). A longitudinal study of hand motor recovery after sub-acute stroke: a study combined FMRI with diffusion tensor imaging. PLoS One, 8, e64154.
Weiller, C., Ramsay, S. C., Wise, R. J., Friston, K. J., & Frackowiak, R. S. (1993). Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Annals of Neurology, 33, 181–189.
Wittenberg, G. F., Chen, R., Ishii, K., Bushara, K. O., Eckloff, S., Croarkin, E., et al. (2003). Constraint-induced therapy in stroke: magnetic-stimulation motor maps and cerebral activation. Neurorehabilitation and Neural Repair, 17, 48–57.
Zatorre, R. J., Chen, J. L., & Penhune, V. B. (2007). When the brain plays music: auditory-motor interactions in music perception and production. Nature Review Neuroscience, 8, 547–558.
Zhou, D., Thompson, W. K., & Siegle, G. (2009). MATLAB toolbox for functional connectivity. NeuroImage, 47, 1590–1607.
Zumbansen, A., Peretz, I., & Hebert, S. (2014). Melodic intonation therapy: back to basics for future research. Frontiers in Neurology, 5, 7.
Acknowledgments
This work was supported by la Fundació La Marató TV3 (Spain), the DFG and FPU program AP2010-4179 to P.R. We are particularly grateful to all the participants for being part of this study. We want to also thank Clara Medrano, Gemma Torres, Gonçalo Padrao, Laura Merino and Sabine Schneider for their help.
Author contributions
E.A., T.F.M. and A.R.F. designed research; N.R., J.L.A., J.G.S., M.J., L.V., F.R., E.D. and C.G. performed research; P.R., N.R., E.C. and J.M.P. analyzed data; P.R., N.R., E.C., J.M.P., J.L.A., J.G.S., L.V., E.A., T.F.M. and A.R.F wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ripollés P, Rojo N, Grau-Sánchez J, Amengual JL, Camara E, Marco-Pallarés J, Juncadella M, Vaquero L, Rubio F, Duarte E, Garrido C, Altenmuller E, Münte TF and Rodríguez-Fornells A, declare no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, and the applicable revisions at the time of the investigation. Informed consent was obtained from all patients for being included in the study.
Additional information
P. Ripollés and N. Rojo contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 133 kb)
Rights and permissions
About this article
Cite this article
Ripollés, P., Rojo, N., Grau-Sánchez, J. et al. Music supported therapy promotes motor plasticity in individuals with chronic stroke. Brain Imaging and Behavior 10, 1289–1307 (2016). https://doi.org/10.1007/s11682-015-9498-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11682-015-9498-x