Abstract
The interconnection between moral distress, moral sensitivity, and moral resilience was explored by constructing two hypothetical scenarios based on a recent Swedish newspaper report. In the first scenario, a 77-year-old man, rational and awake, was coded as “do not resuscitate” (DNR) against his daughter’s wishes. The patient died in the presence of nurses who were not permitted to resuscitate him. The second scenario concerned a 41-year-old man, who had been in a coma for three weeks. He was also coded as “do not resuscitate” and, when he stopped breathing, was resuscitated by his father. The nurses persuaded the physician on call to resume life support treatment and the patient recovered. These scenarios were analyzed using Viktor Frankl’s existential philosophy, resulting in a conceivable theoretical connection between moral distress, moral sensitivity, and moral resilience. To substantiate our conclusion, we encourage further empirical research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
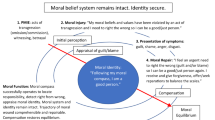
Moral agency in health care practice is fundamentally a dynamic, inter-relational process that is prompted by moral sensitivity—an awareness of the moral implication in making a decision on behalf of another human being (Lützén et al. 2006). Moral action is followed by personal and professional reflection, justification, and accountability for the decision made (Edwards et al. 2011; Peter 2011). From a relational ethics perspective, moral agency not only consists of cognitive ability and emotional capacity but also is demonstrated in an attitude of respect for the other (Bergum and Dossetor 2005). Although these personal capacities may be present, moral agency is not always an easy task when value conflicts occur and moral imperatives stand in opposition to one another. The bioethical principled approach to ethical decision-making has not fully recognized that these moral imperatives are grounded in a relational context, which all clinical settings invariably are. Contradictory views within the interdisciplinary team and between family members can result in situations with no consensus or satisfactory decision. Making a decision on withholding treatment, limiting autonomy, or going through with prenatal testing are only a few examples of situations that perpetually occur in medical and nursing practice. Although support models for ethical decision-making are available, there is empirical evidence that illustrates that these situations are a precursor to moral distress in many clinical settings (Rodney et al. 2002; Woods 2005). We raise the question: Does the absence of moral distress indicate detachment from the ethical issue or can a person find meaning and develop moral resilience despite being repeatedly involved in ethically complex situations?
Aim and Focus
Empirical studies (Lazzarin, Biondi, and Di Mauro 2012; Wilkinson 1987) substantiate that moral distress is prevalent in many health care contexts and may be increasing due to the complexity of ethical decision-making. One feature of ethical decision-making, regardless of context, is that the actions taken invariably affect the provision of good care. A second feature is that both patients and their family are affected by the decision made, especially when patients have limited autonomy or capacity to make their own decisions. Thus, our aim in this paper is to cast a light on moral distress by reflecting on the relationship between moral sensitivity, moral distress, and moral resilience as interrelated components of moral agency. We use Viktor E. Frankl’s idea of meaning (1961, 1978, 1997) as a philosophical frame to our discussion because we feel that this focus may give theoretical depth in understanding the relationship between moral sensitivity, moral resilience, and moral distress. Our analysis is based on two scenarios that involve withdrawing life support treatment in the context of an intensive care unit. We do not refer to Frankl’s applied psychology or “logotherapy,” which serves as a tool for psychotherapy concerning existential issues that have by tradition been attended to by those who undertake pastoral care. First, we review the main characteristics of moral distress, moral sensitivity, and moral resilience.
Conceptual Framework
Moral Distress
Stress refers to any event in the environment that strains or exceeds the adaptive resources of an individual or a shared system. This involves both the person’s cognitive appraisal of the demand and the individual’s resources to cope with the request, as well as his or her physical and emotional reactions to the situation (Theorell and Karasek 1996). Empirical research on moral distress in health care has contributed to an understanding of the complexity of ethical decision-making for all persons involved (Corley et al. 2001; Gallagher 2010; Lützén and Ewalds-Kvist 2012; Vogel Smith 1996). When events and demands threaten a person’s most important values and fundamental assumptions about the world (Simon 1997) this threat is accompanied by a feeling of not being in control. Lack of control causes stress and, if placed within the framework of bioethics, moral distress arises when one knows the right thing to do for the Other but institutional control or constraint make it nearly impossible to pursue the right course of action (Jameton 1984). These constraints can either be factual, for example, shortage of staff, or self-defined inabilities to act, such as lack of knowledge or power to resist or pursue what one believes to be right according to one’s own convictions (Lazzarin, Biondi, and Di Mauro 2012). According to Wilkinson (1987), moral distress represents a psychological disequilibrium experienced when a person makes a moral decision but does not act upon it. Russell (2012) summarizes four comprehensive attributes of moral distress: negative feelings, powerlessness, conflicting loyalties, and uncertainty. A number of secondary attributes were also identified such as ineffective advocacy, the inability to reduce pain and suffering, patient dehumanization, and competing values.
Ethical decision-making in clinical practice seen from a relational ethics perspective involves respecting the views of the patient, the family, and professionals who are involved in a specific situation. Vogel Smith (1996) elucidated the inter-related processes of ethical reasoning and ethical conduct in terms of “deliberation” and “integration.” Deliberation refers to nurses’ process of reasoning and engages different factors that affect ethical decision-making. Integration stands for the implementation of nurses’ decisions in clinical practice. Personal factors such as nurses’ values, convictions, experiences, knowledge, and skills in addition to contextual factors such as opinions and expectations of other nurses, doctors, and family as well as rules and routines, procedures, and guidelines specific to wards all play a vital role in both processes (Goethals, Gastmans, and Dierckx de Casterle 2010).
In morally conflicting situations, the commitment to professional values and experiencing meaning in all patient care is threatened (Lützén 1993). We also know that distress can be reduced or prevented by a feeling of personal control as well as a trusting and supportive environment (Mirowsky and Ross 1986). A supportive environment has the potential to deal with distress in interpersonal dialogue (Olson 1998; Pendry 2007). For example, sharing one’s feelings concerning a morally distressing situation with the professional team creates an open atmosphere that nourishes moral reflection and promotes moral agency.
Recent research suggests that the intensity of the feeling of moral distress can vary according to two factors: moral sensitivity and the moral climate in the organization (Lützén et al. 2010). The first factor, moral sensitivity, describes a positive personal attribute—an awareness of the moral nature in an encounter with a person who, because of certain circumstances, is in a vulnerable position. The second factor pertains to the organizational structure that generates norms for behavior, documented as rules and regulations, with which the individual worker must abide in order to continue employment (Olson 1998; Victor and Cullen 1988). Norms dictate behavior that can either lead to an open climate in which a dialogue is undertaken and support is given to resolve ethical problems or the opposite (Olson 1998). Moral distress can occur if a person’s moral sensitivity is hampered by, for example, a climate that does not recognize the need for discussion about ethical issues in daily practice (Lützén et al. 2010). Complex decisions such as infringement of a patient’s autonomy or making priorities in acute or critical care over time can lead to moral distress (Blanchette and Manco-Johnson 2010; Coppola et al. 2011). Yet, we note that in current research on moral distress emphasis is placed on determining levels of structural empowerment and the association between moral distress and structural empowerment among nurses. Structural empowerment refers to the ability to access sources of power (DeKeyser Ganz et al. 2012), thus there may exist a theoretical relationship between these concepts.). In general, structural empowerment may relate to moral distress (Peter, Lerch Lunardi, and Macfarlane 2004). Issues related to end-of-life concerns were especially distressing to nurses. Intensity and frequency of moral distress are correlated, but intensity might contain an element of moral residue, where feelings of moral distress intensity are retained while perceptions of frequency are not (Peter, Lerch Lunardi, and Macfarlane 2004). However, the environment in which nurses practice strongly influences ethical norms and social practice. Therefore, structural empowerment, as an aspect of the work environment, is related to moral distress. However, in a health care system that is controlled by physicians who are the main sources of information, nurses might feel empowered in their own units but may feel disconnected from the general hospital environment according to research by DeKeyser Ganz et al. (2012).
Moral Sensitivity
Lützén’s initial studies on moral sensitivity were based on interviews with nurses employed in closed psychiatric units for adults suffering from mental illness requiring long-term care (Lützén 1993; Lützén and Nordin 1993a, b, 1994). The nurses, who expressed moral sensitivity, first identified and described situations that they viewed as “ethical” in nature because of the patient’s vulnerability. In all of these situations, the nurses were concerned about maintaining the patient’s autonomy. However, the nurses also valued their professional obligation that decisions made should be aimed at maintaining the integrity of the patient. In response to the question, “How do you know what is the right decision?” the nurses answered that it was an “inner voice” or a “gut feeling.” This response led to exploring phenomenological ethics, with its origin in the concept of “moral sense” that can be traced to the British moral philosophers in the 17th century, referred to as “sentimentalists” who suggested that moral distinctions originate in the sentiment and not in reason alone (Almer 1939). The “moral sense” was thought to close the gap between moral knowledge and moral behavior by providing a motive for action. Shaftesbury (1671–1713) was the first British philosopher to develop the idea of the “moral sense.” He argued that in order for “man” to be virtuous “he” must be capable of reflecting on his (sic!) “actions” and “affections” (Gill 2006). Hutcheson was aligned to some degree with Shaftesbury’s theory of the function of (moral) reflection and claimed that moral “ideas” are derived from “the” moral sense through which “pleasures and pains” or good versus evil are generated (Almer 1939). Translated into modern vocabulary, perhaps “pleasures” can refer to a good or “clean” conscience and “pains” to a bad conscience. These feelings of pleasures and pains accompanied with bodily or emotional reactions bring us closer to the concept of moral (dis)stress.
Modern phenomenological ethicists, foremost Tymieniecka, extended the idea of the moral sense by suggesting that the “benevolent sentiment” functions in the inter-subjective interpretation of conflicting situations: “It is the benevolent sentiment at work, introducing ultimately the moral axis of right or wrong that establishes the inter-subjective life-sharing” (Tymieniecka 1986, 34). Further, Tymieniecka refers to the “evaluative process” where the benevolent sentiment presents itself (1986, 35). In short, in this decision-making process, judgments do not only concern a moral act based on approbation (praise, approval) or disapprobation without benevolence toward the other being present. That is, moral agency is manifested by benevolence and moral responsibility for the well-being of all living beings (Tymieniecka 1986).
In research on nurses’ moral decision-making in mental health care, moral sensitivity was described as an immediate understanding of a patient’s vulnerable situation as well as an awareness of the moral implications of decision-making on his or her behalf (Lützén 1993; Lützén et al. 2006). However, the opposite could also happen: weakening of moral sensitivity in which the focus shifts from the vulnerable other to oneself and to self-defensive actions and arguments, even to covering one’s tracks. In a supportive ethical climate, where the sentiments of, and discussions about, moral demands can be shared in the interprofessional team, a realistic potential for enactment of moral agency exists. Hence, moral sensitivity refers to a subjective insight into what should be done while moral agency answers how this should be accomplished. Nevertheless, there are circumstances that prevent both the what and the how, on which we will focus in this paper.
Moral Resilience and Existential Analysis
Viktor Frankl (1959, 1961, 1978, 1997) conceived a meaning-oriented philosophy, named logotherapy/existential analysis (from the Greek logos meaning “meaning”). He argued that the search for meaning in life is the primary motivational force in human beings and comprises three philosophical and psychological concepts: (a) Freedom of Will, where freedom is defined as the realm of determining one’s own life within the limits of a given possibility; (b) Will to Meaning: Human beings are not only free, but free to do something—explicitly, to achieve goals and purposes; (c) Meaning in Life: Humans are urged, on the basis of their freedom and responsibility, to develop the best possible in themselves and in the world by perceiving and realizing the meaning of the moment in each and every situation. These meaning possibilities, although objective in nature, are connected to the exact situation and person and are therefore constantly shifting (Batthyany n.d.). In times of trauma and existential crisis, the attribution of meaning serves as moderator of unpleasant feelings and is crucial for explaining the differences in people’s vulnerability to stressors (Simon 1997).
Viktor Frankl is a paramount example of a person equipped with moral resilience—a concept that can be defined as a distinctive sense that life is meaningful under every condition. He validated his own conclusion that even in the most absurd, painful, and dehumanized situation, life has potential meaning and, therefore, even suffering can be meaningful when one cannot remove or change the cause of distress. Despair means suffering without meaning. Frankl focuses on the will to meaning as opposed to Adler’s will to power or Freud’s will to pleasure. A crisis of meaninglessness provokes an existential vacuum or a feeling of emptiness. Meaning was the leitmotif of Frankl’s works. In his book Man’s Search for Meaning, published in the late 1950s, he communicated moral resilience as a man forced to live as an inmate in a concentration camp but who chose to live a meaningful life even under extreme conditions. In 1997, Frankl completed his works on moral resilience by publishing Man’s Search for Ultimate Meaning and claimed that true existential meaning stems out of three sources: (1) accomplishments and creative activities such as solving a problem or creating something; (2) experiencing something or someone inspiring such as the beauty of nature, the love for a spouse or family member, or the value of a close friend; and (3) identifying value in unavoidable suffering.
The gap between our real and ideal selves creates a healthy tension or stress that keeps us inspired and mentally well. We can choose within ourselves to attribute meaning to every situation, which helps us to be morally resilient: “The one thing you can’t take away from me is the way I choose to respond to what you do to me.” In the early 1940s after Frankl married, the Nazis forced the young couple to abort their child and deported them to ghettos and concentration camps where he came down with typhoid fever. To escape death, he kept himself awake during the nights by reconstructing his book manuscript that he had been working on prior to this. When Frankl returned to Vienna, he learned that his family members died in the gas chambers (Viktor Frankl Institute n.d.). Despite these hardships, Frankl believed that by offering paths to finding existential meaning to other persons, his own life would become meaningful. Bartone (2006) refers to meaning in Frankl’s sense and suggests that many people show remarkable resilience and remain mentally healthy despite severe stress levels. One potential pathway to enhance moral resilience is to foster hardiness, that is, to encourage a distinctive sense that life is meaningful. On the other hand, Bartone identifies risk factors for morally non-resilient behavior in the context of modern military operations that include “isolation, ambiguity, powerlessness, boredom, and danger” (2006, 134). Resilient people typically interpret experience as (a) interesting and worthwhile overall (meaningful); (b) something they can exert control over (we can choose our attitudes toward unavoidable suffering); and (c) valuable, challenging, and presenting opportunities from which to learn and grow (logotherapeutic).
Withdrawing Life-Supporting Treatment—Two Scenarios
The idea of existential meaning as related to resilience can be transferred to the intensive care environment, since critical decisions and professional responsibility provide opportunities for individual choices in deciding and doing what one believes to be right for oneself and others (Rodney et al. 2002; Russell 2012; Woods 2005). Bartone’s (2006) risk factors for non-resilience or frustration of meaning are, among others, “ambiguity and powerlessness.” If moral resilience is defined as a distinctive sense that life is meaningful under every condition, two recent cases within the Swedish health care system may call this definition into question. In the intensive care unit, nurses are the ones most present at the patient’s bedside, taking orders from the physicians, meeting the family, and showing understanding for the family’s hope for the survival of their loved one. These nurses meet dying and death, almost on a daily basis, and at times may feel that they could have done more for the patient. However, according to the results of an extensive review of the role of nurses in intensive care, it is questionable to what extent nurses perceive that they have a legitimate role in end-of-life decision-making (Adams et al. 2011).
End-of-life decision-making is becoming increasingly complex, involving difficult decisions such as whether to initiate or discontinue life support (Adams et al. 2011). Medical advancement has, in many Western countries, made it possible to prolong life. However, the practice of end-of-life decision-making and the extent of involvement of family or collaboration with the critical care team may vary. In an extensive study of six European countries, the characteristics of end-of-life decisions were investigated (van der Heide et al. 2003). The results reveal that when the patient was mentally competent, end-of-life decisions were discussed with the patient and relatives most frequently in the Netherlands and least frequently in Italy and Sweden. For both competent and incompetent patients, more than 50 percent of decisions were discussed with neither patient nor relatives. Given that this study is 10 years old, with data probably collected at least one year prior to publication, it is useful to compare these results with a Canadian court ruling that states: “withdrawal of life support is a plan of treatment requiring consent” of the substitute decision-makers (cited in Cooper, Chidwick, and Sibbald, 2011, 467). According to the current guidelines for life support treatment in Sweden, prior to making a decision to withdraw or withhold life support treatment, the physician should consult with a colleague. Moreover, the family should be informed and their wishes respected (National Board of Health and Welfare 2011).Footnote 1
Presently the practice of “coding” is used in Sweden to communicate and alert (mainly) nursing staff as to whether life support treatment should be given or not. For example, when “0-DNR” is written in a patient’s chart, this indicates that no cardiopulmonary resuscitation is to take place in case of heart failure. The code, or the decision prior to coding, is to be made by the attending physician when he or she judges that treatment only prolongs suffering and the patient’s condition inevitably leads to death. In the national Swedish guidelines for terminating life-sustaining treatment, the physician should consult with at least one colleague. Moreover, the physician should even consult with other staff who participated in the care of the patient. All significant information should be recorded such as what attitudes the patient and relatives have with regard to not initiating or continuing life-sustaining treatment. Neither age nor the mental state of a patient is a judicially justifiable reason to withdraw or withhold treatment or care. Even if the physician has medical evidence and judicial support to justify end-of-life decisions, a decision on the termination of life-sustaining treatment should be preceded by documented ethical considerations (SMER 2011). In order to illustrate how withdrawal of life support can be experienced as morally distressing by nursing staff and family, we constructed two hypothetical scenarios inspired by two current articles in a Swedish newspaper.Footnote 2 These two cases are constructed with the aim to integrate previous work done on moral distress. However, there are some notable gaps of which the reader should be aware. We have no substantive evidence that the nurses and others involved in these two cases actually experienced moral distress. Our conjectures regarding the experience of moral distress are drawn from theoretical knowledge, discussed in this paper, and relevant empirical research. Our analyses should be seen as theoretical possibilities that could be useful in guiding further empirical research.
In each of these scenarios the patient was coded by the physician, not by the patient or family, as “not to continue life-support treatment.” The first patient was a 77-year-old man whose general condition was very poor but who fought to survive although the physician denied him life-sustaining care. The patient’s daughter telephoned the evening before he passed away and asked the nurses to do all they could for her father. Yet, because of the physician’s order, the nurses could do nothing but stand and watch him die. The second patient was a 41-year-old man who was in a coma as a result of a drug reaction. Despite the parents seeing signs that their son was regaining consciousness, the physician made the decision not to resuscitate. The nurses were not permitted to do anything and the oxygen and defibrillator were removed from his room. However, when the patient’s heart stopped, his father applied cardiopulmonary resuscitation (CPR) and his breathing commenced. After much persuasion, the nurses and the patient’s parents managed to convince the physician who was on call to resume life-sustaining treatment. This patient is now fully recovered and has returned to his family and work.
Analysis of the Scenarios
These scenarios raise the question of whether the nurses enacted moral agency or not. It seems that the guidelines formalize what could be considered a moral responsibility concerning the termination of a person’s life and the persons who will be left in mourning. Our interpretation is that the nurses who could not “do anything” may have felt morally perplexed and thus deeply distressed in their professional meaning—they would in Bartone’s words have felt “ambiguity and powerlessness” and would be subject to moral distress.
If we draw on Frankl’s (1961, 1969, 1978) work to analyze the two scenarios, we propose that moral resilience is a personal and cultural strategy of attributing existential meaning to a dreadful event—a mental stamina even transcending a sense of failure in not being able to act upon one’s moral sensitivity. In order to connect meaning to the patient’s death, it should not be passed on and forgotten. The daughter’s situation of having lost her father and not having her wishes respected would certainly leave her with a feeling of distrust in the treatment and care given. It is important to show empathy and respect for her experience. She was not present when her father died and may need to regain her trust in the health care system. The nurses, however, were present and may see the patient’s death as their failure. The physician, by owning the decision, needs to explain to the daughter and the nursing staff the reasons for withdrawing life-support treatment. Encouraging interdisciplinary dialogue with the goal of understanding each other’s moral and professional responsibility is a way to create an atmosphere in which moral resilience can be fostered.
Looking at the second scenario, in which the patient’s father resuscitated his son, the nurses acted upon what they considered the right thing to do. Frankl’s (1978, 35–38) claim that true meaning stems, for example, out of solving a problem can be applied in this situation. After the son regained his breathing function, the nurses acted upon their conviction to give good care, took control, and persuaded the doctor to cancel his decision not to administer life support treatment to the 41-year-old man. The nurses respected the inimitability and sacredness of life, which means that their professional endeavor made moral sense.
Conclusion
Our aim in this paper was to explore moral distress by reflecting on the relationship between moral sensitivity, moral distress, and moral resilience as interconnected components of moral agency. By using Viktor Frankl’s existential analysis as a metaphorical compass, we embarked on a journey that was more complex than we had anticipated. Viewing “meaning” as closely connected to moral resilience, we created and analyzed two hypothetical cases inspired by two real-life incidents reported in a daily Swedish newspaper. We are also aware that important facts may have been missed by the journalistic reporting on these incidents. Nevertheless, we think that our hypothetical cases are educational and fruitful when investigated from the angle of Frankl’s existential analysis with reference to moral sensitivity, moral distress, and moral resilience. We conclude that a person’s moral sensitivity arouses unpleasant feelings that can be described as moral distress in circumstances in which they are not able to enact their moral agency. By experiencing meaning in similar situations and outcomes as portrayed in the present scenarios, moral distress could be limited. This may be achieved through interdisciplinary dialogue as well as by showing respect for the family’s and, if possible, the patient’s, own wishes. Relational engagement enhances moral resilience by encouraging the distinctive sense that life is meaningful under all conditions.
Notes
The National Board of Health and Welfare (Socialstyrelsen) is a government agency in Sweden under the Ministry of Health and Social Affairs.
Expressen, June 30, 2011, and August, 26, 2012.
References
Adams, J.A., D.E. Baily Jr., R. Anderson, and S.L. Docherty. 2011. Nursing roles and strategies in end-of-life decision making in acute care: A systematic review of the literature. Nursing Research and Practice. doi:10.1155/2011/527834. Article ID 527834.
Almer, T. 1939. Studier i Shaftesburys filosofi [Studies of Shaftesbury’s philosophy]. Ph.D. diss., University of Lund.
Bartone, P.T. 2006. Resilience under military operational stress: Can leaders influence hardiness? Military Psychology 18(2): 131–148.
Batthyany, A. 2013. What is logotherapy and existential analysis? Viktor Frankl Institut. www.viktorfrankl.org/e/logotherapy.html.
Bergum, V., and J. Dossetor. 2005. Relational ethics: The full meaning of respect. Hagerstown: University Publishing Group Inc.
Blanchette, V.S., and M.J. Manco-Johnson. 2010. Meeting unmet needs in inhibitor patients. Haemophilia 16(3): 46–51.
Cooper, A.B., P. Chidwick, and R. Sibbald. 2011. Court rules that withdrawal of life support is a plan of treatment requiring consent. Canadian Medical Association Journal 183(8): E467. doi:10.1503/cmaj.109-3855.
Coppola, A., M.A. Cerbone, G. Mancuso, M.F. Mansueto, C. Mazzini, and Z. Ezio. 2011. Confronting the psychological burden of haemophilia. Haemophilia 17(1): 21–27.
Corley, M.C., R.K. Elswick, M. Gorman, and T. Clor. 2001. Development and evaluation of a moral distress scale. Journal of Advanced Nursing 33(2): 250–256.
DeKeyser Ganz, F.D., R. Ofra, et al. 2012. Moral distress and structural empowerment among a national sample of Israeli intensive care nurses. Journal of Advanced Nursing 69(2): 415–424.
Edwards, I., C.M. Delany, A.F. Townsend, and L.L. Swisher. 2011. Moral agency as enacted justice: A clinical and ethical decision-making framework for responding to health inequities and social injustice. Physical Therapy 91(11): 1653–1663.
Frankl, V.E. 1959. Man’s search for meaning. Boston: Beacon.
Frankl, V.E. 1961. Die psychotherapie in der praxis: Eine kasuistische einfuhrung fur arzte. Wien: Franz Deuticke.
Frankl, V.E. 1969. The will to meaning: Foundations and applications of logotherapy. New York and Cleveland: The World Publishing Company.
Frankl, V.E. 1978. The unheard cry for meaning. Psychotherapy and humanism. New York: Simon and Schuster.
Frankl, V.E. 1997. Man’s search for ultimate meaning. New York: Perseus Book Publishing.
Gallagher, A. 2010. Moral distress and moral courage in everyday nursing practice. Online Journal of Issues in Nursing 16(2): 8. doi:10.3912/OJIN.Vol16No02PPT03.
Gill, M.B. 2006. Lord Shaftesbury [Anthony Ashley Cooper, 3rd Earl of Shaftesbury]. In The Stanford encyclopedia of philosophy (Winter 2006 Edition), ed. E.N. Zalta, S. Goethals, C. Gastmans, and B. Dierckx de Casterle. http://plato.stanford.edu/entries/shaftesbury/.
Goethals, S., C. Gastmans, and B. Dierckx de Casterle. 2010. Nurses’ ethical reasoning and behaviour: A literature review. International Journal of Nursing Studies 47(5): 635–650.
Jameton, A. 1984. Nursing practice: The ethical issues. Englewood Cliffs: Prentice-Hall.
Lazzarin, M., A. Biondi, and S. Di Mauro. 2012. Moral distress in nurses in oncology and haematology units. Nursing Ethics 19(2): 183–195.
Lützén, K. 1993. Moral sensitivity; a study of subjective aspects of the process of moral decision making in psychiatric nursing. Ph.D. diss., Karolinska Institute.
Lützén, K., and B. Ewalds-Kvist. 2012. Moral distress: A comparative analysis of theoretical understandings and inter-related concepts. HEC Forum 24(1): 13–25.
Lützén, K., and C. Nordin. 1993a. Structuring moral meaning in psychiatric nursing practice. Scandinavian Journal of Caring Sciences 7(3): 175–180.
Lützén, K., and C. Nordin. 1993b. Benevolence, a central moral concept derived from a grounded theory of nursing decision making in psychiatric setting. Journal of Advanced Nursing 18(7): 1106–1111.
Lützén, K., and C. Nordin. 1994. Modifying autonomy—a concept grounded in nurses’ experiences of moral decision-making in psychiatric practice. Journal of Medical Ethics 20(2): 101–107.
Lützén, K., V. Dahlqvist, S. Eriksson, and A. Norberg. 2006. Developing the concept of moral sensitivity in health care practice. Nursing Ethics 13(2): 187–196.
Lützén, K., T. Blom, B. Ewalds-Kvist, and S. Winch. 2010. Moral stress, moral climate and moral sensitivity among psychiatric professionals. Nursing Ethics 17(2): 213–224.
Mirowsky, J., and C.E. Ross. 1986. Social pattern of distress. Annual Review of Sociology 12: 23–45.
National Board of Health and Welfare. 2011. Opinion on new regulations and general advice from The National Board of Health and Welfare regarding life-sustaining treatment. Stockholm: The Swedish National Council on Medical Ethics.
Olson, L.L. 1998. Hospital nurses’ perceptions of the ethical climate of their work setting. Journal of Nursing Scholarship 30(4): 345–349.
Pendry, P.S. 2007. Moral distress: Recognizing it to retain nurses. Nursing Economics 25(4): 217–221.
Peter, E. 2011. Fostering social justice: The possibilities of a socially connected model of moral agency. Canadian Journal of Nursing Research 43(2): 11–16.
Peter, E., V. Lerch Lunardi, and A. Macfarlane. 2004. Nursing resistance as ethical action: Literature review. Journal of Advanced Nursing 46(4): 403–416.
Rodney, P., C. Varcoe, J.L. Storch, et al. 2002. Navigating towards a moral horizon: A multisite qualitative study of ethical practice in nursing. Canadian Journal of Nursing Research 34(3): 75–102.
Russell, A.C. 2012. Moral distress in neuroscience nursing: An evolutionary concept analysis. Journal of Neuroscience Nursing 44(1): 15–24.
Simon, R.W. 1997. The meanings individuals attach to role identities and their implications for mental health. Journal of Health and Social Behavior 38(3): 256–274.
SMER (Statens Medicinsk-Etiska Råd). 2011. Review statements: Regulations and general advice on life support and manual on life support. Stockholm: SMER [The National Council on Medical Ethics].
Theorell, T., and R.A. Karasek. 1996. Current issues relating to psychological job strain and cardiovascular disease research. Journal of Occupational Health Psychology 1(1): 9–26.
Tymieniecka, A.-T. 1986. The moral sense and the human person within the fabric of communal life. Analecta Husserliana 20: 3–100.
Van der Heide, A., L. Deliens, K. Faisst, et al. 2003. End-of-life decision-making in six European countries: Descriptive study. Lancet 361(9381): 345–350.
Victor, B., and J.B. Cullen. 1988. The organizational bases of ethical work climates. Administrative Science Quarterly 33(1): 101–126.
Viktor Frankl Institut. No date. Life and work: Chronology. http://www.viktorfrankl.org/e/chronology.html.
Vogel Smith, K.V. 1996. Ethical decision-making by staff nurses. Nursing Ethics 3(1): 17–25.
Wilkinson, J.M. 1987. Moral distress in nursing practice: Experience and effect. Nursing Forum 23(1): 16–29.
Woods, M. 2005. Nursing ethics education: Are we really delivering the good(s)? Nursing Ethics 12(1): 5–18.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lützén, K., Ewalds-Kvist, B. Moral Distress and its Interconnection with Moral Sensitivity and Moral Resilience: Viewed from the Philosophy of Viktor E. Frankl. Bioethical Inquiry 10, 317–324 (2013). https://doi.org/10.1007/s11673-013-9469-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11673-013-9469-0