Abstract
Summary
In a community-dwelling elderly cohort, dysmobility syndrome was associated with elevated odds of morphometric vertebral fracture or any prevalent fracture, independent of age and covariates. Dysmobility syndrome improved discrimination for fracture when added to the FRAX score.
Introduction
Dysmobility syndrome was coined to indicate patients with impaired musculoskeletal health. Data on the association of dysmobility syndrome with prevalent morphometric vertebral fracture (VF) in elderly persons are limited.
Methods
A total of 1369 community-dwelling elderly subjects (mean age 71.6 years; women 66%) were analyzed. Dysmobility syndrome was defined as ≥ 3 components among falls, low lean mass, high fat mass, osteoporosis, low grip strength, and low timed get-up-and-go performance. VF was defined as a ≥ 25% reduction in the height of vertebral bodies in plain radiographs. Modified cutpoints of each component at which elevate the odds of fracture were investigated using receiver-operating characteristics analysis. Net reclassification improvement (NRI) and integrated discrimination index (IDI) were calculated to assess additive discriminatory value of dysmobility syndrome over FRAX.
Results
The prevalence of VF and any fracture composite of VF and non-VF was 16% and 25%, respectively, increasing according to number of dysmobility components (from 0 to 5; VF 10–35%; any fracture 16–45%). Dysmobility syndrome was associated with elevated odds of VF (adjusted OR [aOR] 1.52, 95% CI 1.08–2.15) or any fracture (aOR 1.46, 95% CI 1.07–1.98) but no longer with non-VF (aOR 1.31, 95% CI 0.86–1.98) in multivariate model, whereas modified definition showed robust association with non-VF (aOR 1.79, 95% CI 1.23–2.60). Dysmobility syndrome improved discrimination for prevalent fracture when added to FRAX (NRI 0.25, 95% CI 0.13–0.37; IDI 0.020, 95% CI 0.014–0.026).
Conclusions
Dysmobility syndrome was associated with elevated odds of morphometric VF in community-dwelling older adults, independent of age and covariates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures are a major health burden imposing substantial morbidity and mortality in the elderly [1, 2]. Although T-score-based diagnosis of osteoporosis based on bone mineral density (BMD) testing has provided a pragmatic concept for identifying persons at a risk of fractures, it has been recognized that not only bone loss but also other factors such as muscle loss, obesity, and propensity for falls should be combined to properly reflect a singular condition that requires fracture prevention [3]. In this context, Binkley et al. proposed a new concept, dysmobility syndrome, to indicate patients with impaired musculoskeletal health [4]. Dysmobility syndrome was defined as the presence of three or more components among falls in the preceding year, slow gait speed, low grip strength, osteoporosis, sarcopenia, and high fat mass, and this concept was analogous to the scheme of metabolic syndrome in cardiovascular diseases [4].
In prior studies, dysmobility syndrome was associated with an increased risk of mortality in older adults [5, 6]. Concerning fracture, subjects with dysmobility syndrome had a higher prevalence of self-reported prior fracture and history of falls than those without dysmobility syndrome in a cohort of Caucasian older adults [4]. Postmenopausal women with a history of the previous fracture had elevated odds of having dysmobility syndrome [7]. Further, the presence of dysmobility syndrome was associated with an increased risk of incident fracture in men, independent of the FRAX (fracture risk assessment) score [8]. Although these studies suggested the potential utility of dysmobility syndrome for identification of individuals with a high risk of fracture, data on the association of dysmobility syndrome and its components with morphometric vertebral fracture (VF), an indicator for treatment and a strong predictor for future fracture, in community-dwelling elderly persons are limited [9].
In this study, we aimed to investigate whether the presence of dysmobility syndrome and its components are associated with elevated odds of morphometric VF in a community-based elderly cohort. We further investigated optimal cutpoint for each dysmobility component at which increases the odds of fracture.
Methods
Study design and participants
The Korean Urban-Rural Elderly (KURE) study is an ongoing, prospective, longitudinal cohort study on aging and various health outcomes in community-dwelling elderly persons [10]. We recruited our subjects from the residents of three urban districts of Seoul and one rural area of Incheon, Korea, who were 65 years or older, through local government health facilities, promotional posters, or random home visits. In the baseline period (2012–2015), a total of 3517 subjects participated in the study. Among them, we analyzed 1493 subjects enrolled in 2014 and 2015 in this study because body composition measurement using bioimpedance analysis (BIA) became available as a routine measurement in 2014. All subjects underwent interviewer-assisted health-related questionnaire surveys, anthropometric measurements, laboratory tests, dual-energy x-ray absorptiometry (DXA; QDR 4500A; Hologic, Waltham, MA, USA), BIA (InBody 720; Biospace Co., Ltd., Seoul, Korea), and physical performance tests including the timed get-up-and-go (TUG) test. The exclusion criteria for this study were as follows: active inflammatory status with elevated high-sensitivity C-reactive protein (> 8 mg/L, n = 47) or elevated white blood cell count (> 15,000 cells/mm3, n = 2), presence of any active cancer (n = 49), any missing study variable value (n = 19), or subjects with combined two criteria (n = 7). Data from 1369 subjects remained in the final analysis.
Fracture assessment
Morphometric VF was defined, using semiquantitative visual assessment, as a > 25% reduction in any measured vertebral height (anterior, middle, or posterior) in lateral thoracolumbar radiographs obtained using DXA by two experts in a blinded manner [10,11,12,13]. Any inconsistency was adjudicated by a third radiologist reviewer with > 10 years of experience. Non-VF was assessed using interviewer-assisted questionnaires, after excluding fracture attributable to major trauma; falling from a place higher than standing height; fracture before age 40 years; and fracture in the fingers, skull, face, and toes. Any fracture was defined as a composite outcome of morphometric VF and non-VF.
Dysmobility syndrome
We used the definition of dysmobility syndrome as described previously [14]. Dysmobility syndrome was defined as the presence of ≥ 3 of the following six factors: falls in the preceding year, low grip strength (< 30 kg in men, < 20 kg in women), osteoporosis (T-score ≤ − 2.5 at any site in the lumbar spine, femoral neck, or total proximal femur in DXA evaluation), low TUG performance (12 s or longer), low lean mass (appendicular skeletal muscle mass/height2 < 7.0 kg/m2 in men and < 5.7 kg/m2 in women in BIA), and high fat mass (> 30% for men and > 40% for women in BIA) [4, 14, 15]. The cutpoint for low lean mass measured using BIA was determined according to the Asian Working Group for Sarcopenia (AWGS) guideline [16]. In addition, we developed a modified definition of dysmobility syndrome using optimal cutpoint for each dysmobility component derived from this cohort.
Covariates
Nutritional status was assessed using the Mini-Nutritional Assessment-Short Form categories, as follows: normal 12–14 points, at risk of malnutrition 8–11 points, and malnourished 0–7 points [17]. The International Physical Activity Questionnaire-Short Form was used to grade physical activity as the following health-enhancing physical activity levels: active, minimally active, and inactive [18]. Data on self-reported physician-diagnosed hypertension, diabetes, degenerative arthritis, and hospitalization for any cause during the preceding year were collected using interviewer-assisted questionnaires. Cognitive impairment was defined as a score of < 24 in the Mini-Mental State Examination (Korean version) [19]. After an overnight fast, blood samples were drawn in the morning and stored at − 80 °C until the time of analysis in a central laboratory (SCL Diagnostics, Seoul, Korea). Anemia was defined as hemoglobin level < 13 and < 12 g/dL in men and women, respectively [20]. The Chronic Kidney Disease-Epidemiology equation was used to calculate the estimated glomerular filtration rate. FRAX score (10-year probability [%] of a major osteoporotic fracture) was calculated using clinical risk factors and femur neck BMD for all participants using the algorithm available online at http://www.shef.ac.uk/FRAX (South Korea version, version 3.11). High FRAX score threshold was defined as > 20% of 10-year probability of major osteoporotic fracture.
Statistical analysis
Data are presented as means ± standard deviations or as numbers (percentages). The characteristics of study participants were compared according to the presence of dysmobility syndrome by using an independent t test or chi-square test. The presence of a trend between the prevalence of fracture and the number of dysmobility components was tested using the Cochran-Armitage test for trend. Univariate logistic models were created to test the association between each component of dysmobility syndrome with a prevalent fracture. Receiver operating characteristics (ROC) curve was used to determine the optimal cutpoint at which each component of the dysmobility syndrome increases the odds of any fracture by Youden index [21]. The relative odds of any fracture, morphometric VF, or non-VF according to the presence of dysmobility syndrome were assessed by multivariate logistic models adjusted for age, sex, hospitalization in the preceding year, and serum albumin level. p values for dysmobility syndrome as an independent variable in multivariate logistic models were corrected for multiple testing with Bonferroni method. To investigate the additive discriminatory value of dysmobility syndrome over FRAX score, net reclassification improvement index (NRI) and integrated discrimination index (IDI) were calculated for any prevalent fracture, VF, and non-VF [22]. Statistical significance level was set at two-sided p < 0.05. All statistical analyses were performed with STATA 14.0 (Stata Corp, College Station, TX, USA).
Results
Characteristics of study participants
Among a total of 1369 subjects (mean age 71.6; women 66%), dysmobility syndrome was present in 273 subjects (20%; Table 1). The prevalence of the components of dysmobility syndrome (osteoporosis, low grip strength, falls in the preceding year, low lean mass, high fat mass, and low TUG performance) was significantly higher in persons with dysmobility syndrome than in those without (p < 0.001 for all). Subjects with dysmobility syndrome had an older age; a higher prevalence of malnutrition, diabetes, and degenerative arthritis; and more frequent hospitalizations during the preceding year. Elevated serum alkaline phosphatase and decreased albumin levels were observed in subjects with dysmobility syndrome, with small but discernable differences.
Prevalence of fracture
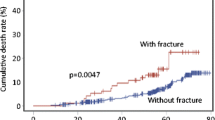
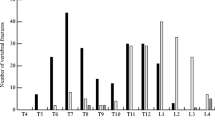
Any prevalent fracture composite of morphometric VF (n = 222, 16%) and non-VF (n = 147, 10%) was present in 333 (24%) subjects among the overall participants, with a higher prevalence in subjects with dysmobility syndrome than in those without (36% vs. 21%, p < 0.001; Table 1). A higher prevalence of both VF (25% vs. 14%, p < 0.001) and non-VF (16% vs. 9%, p = 0.017) was observed in subjects with dysmobility syndrome. Figure 1 shows the stepwise increase of prevalence of any fracture, VF, and non-VF from 0 to ≥ 5 components (any fracture 15–45%; VF 10–35%; non-VF 6–15%; p for trend < 0.05 for all).
Individual components of dysmobility syndrome and fracture
Among the individual components of dysmobility syndrome, low grip strength, poor performance in TUG test, falls in the preceding year, low lean mass, and osteoporosis were associated with elevated odds of any fracture, whereas high body fat percentage was not in univariate analyses (Table 2). The association of each component of the dysmobility syndrome with morphometric VF was significant, except for the association of fat mass with VF. Low grip strength, falls, and osteoporosis were significant factors associated with non-VF.
Modified definition of dysmobility syndrome with optimal cutpoint determination
Optimal cutpoint of each component for predicting elevated odds of any fracture was investigated using Youden index calculated from the ROC curve. Cutpoint for low grip strength (in men < 31 kg [sensitivity/specificity 0.41/0.74]; in women < 20 kg [0.50/0.65]) and high fat mass (in men ≥ 31% [0.11/0.85]; in women ≥ 41% [0.18/0.86]) closely approximated to the cutpoint used in this study (conventional definition). Modified cutpoint for low lean mass (in men ASM/ht2 < 7.8 kg/m2 [0.80/0.38]; in women ASM/ht2 < 6.2 kg/m2 [0.61/0.50]), low TUG performance (≥ 10.5 s [0.44/0.64]), and osteoporosis (in men, T-score ≤ − 1.6 [0.57/0.70]; in women, T-score ≤ − 2.2 [0.67/0.52] at any site in the lumbar spine, femoral neck, or total proximal femur) yielded higher prevalence of dysmobility syndrome (38% vs. 20%) compared to conventional definition.
Relative odds of fracture according to the presence of dysmobility syndrome
Among subjects with dysmobility syndrome by conventional definition, the unadjusted OR of any fracture, VF, and non-VF was 2.05 (95% confidence interval [CI] 1.54–2.73), 2.14 (95% CI 1.55–2.95), and 1.85 (95% CI 1.26–2.71; p < 0.01 for all), respectively. After adjustment for covariates in multivariate models (Table 3), the association of dysmobility syndrome with any fracture (aOR 1.46, 95% CI 1.07–1.98, p = 0.048) and VF (aOR 1.52, 95% CI 1.08–2.15, p = 0.048) remained robust, whereas the statistical significance was attenuated for the association with non-VF (aOR 1.31, 95% CI 0.86–1.98, p = 0.588). However, modified definition of dysmobility syndrome was independently associated with any fracture (aOR 1.84, 95% CI 1.42–4.43, p = 0.002), with VF (aOR 1.76, 95% CI 1.29–2.40, p = 0.001), and also with non-VF (aOR 1.79, 95% CI 1.23–2.60, p = 0.006) in multivariate models. C-statistics ranged from 0.66 to 0.69 for multivariate models with dysmobility syndrome by modified definition (for any fracture 0.66 [0.63–0.70]; for VF 0.66 [0.62–0.69]; for non-VF 0.69 [0.64–0.72]).
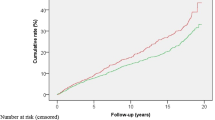
Improved fracture discrimination by dysmobility syndrome over FRAX score
Dysmobility syndrome defined by either conventional or modified definition remained significant predictors of any fracture, VF, and non-VF after adjustment for high FRAX score (major osteoporotic fracture risk > 20%; Table 4). Dysmobility syndrome improved discrimination for prevalent fracture (NRI 0.25 and 0.40 for conventional and modified definition, respectively), VF (NRI 0.27 and 0.39), and non-VF (NRI 0.23 and 0.36; 95% CI for all NRI values > 0) when added to high FRAX score.
Discussion
In this study, we found that dysmobility syndrome and its components were associated with morphometric VF and any prevalent fracture but not with non-VF in community-dwelling elderly persons, independent of age and covariates in multivariate logistic models. Modified cutpoint for dysmobility components was identified in this cohort, which led to the higher prevalence of dysmobility syndrome compared to conventional definition (38% vs. 20%). Both conventional and modified definitions of dysmobility syndrome improved the discriminatory ability for any fracture, VF, and non-VF when added to the FRAX score.
The prevalence of dysmobility syndrome was 20 (conventional) to 38% (modified definition) in this study, which was within the previously reported range in various cohorts (5–34%) [4,5,6, 23, 24]. Currently, three cross-sectional studies have reported the association between dysmobility syndrome and prevalent fracture. The self-reported prior fracture was more common in persons with dysmobility syndrome than in those with sarcopenia diagnosed using various approaches in a Caucasian cohort of 97 community-dwelling older adults [4]. In 121 Italian postmenopausal women, the relative odds of dysmobility syndrome were elevated in subjects with a prior fracture [7]. Meanwhile, in 298 subjects from the Hertfordshire Cohort Study, the association between dysmobility syndrome and self-reported fracture from age 45 years was weak and not statistically significant [23]. However, these findings were mainly based on self-reported fracture data [25]. In this study, dysmobility syndrome showed a robust association with morphometric VF, a strong and significant risk factor for future fracture, and any fracture as a composite of VF and self-reported non-VF in community-dwelling older adults [26].
Although the concept of dysmobility syndrome is still under development, a limitation of this approach is that the proposed components and cutpoint of the syndrome were chosen rather arbitrarily [4]. In this context, we sought to determine optimal cutpoint at which each component of the dysmobility syndrome increases the odds of fracture. A modified cutpoint of dysmobility syndrome had relatively sensitive thresholds compared to conventional definition, which led to the higher prevalence of dysmobility syndrome. Modified dysmobility syndrome showed a stronger association with prevalent fracture and the association remained robust for non-VF, whereas the association of conventional dysmobility syndrome with non-VF was attenuated after adjustment for covariates. Of note, serum albumin also showed a robust association with any fracture, VF, and non-VF, independent of dysmobility syndrome and other covariates. These findings indicate that serum albumin can be considered as one of the candidates for future dysmobility components reflecting nutritional status. Taken together, our findings may support the potential validity of the components incorporated in the current concept of dysmobility syndrome and to reinforce this emerging concept to identify individuals with the high risk of fracture better, which needs to be validated in prospective studies with fracture outcomes.
The concept of osteoporosis based on BMD has provided a pragmatic paradigm for the detection of persons at risk for fracture. However, it has been recognized that the overdependence on BMD as a sole marker of fracture risk might have, at least partially, contributed to the existing crisis in osteoporosis treatment in which a majority of persons who sustain fractures do not undergo treatment to reduce their future fracture risk [3]. Epidemiologic studies showed that up to half of newly developed fractures occurred in subjects with BMD at a normal or osteopenia level [27, 28]. Although currently available tools for fracture risk prediction such as FRAX provide valuable prognostic information, the performance of individualized fracture risk assessment remains suboptimal [29]. In this study, dysmobility syndrome defined by either conventional or modified cutpoint improved discrimination for any prevalent fracture, VF, and non-VF when added to high FRAX score. These findings suggest the potential additive and complementary value of dysmobility syndrome to the conventional fracture risk assessment tools, although the additive prognostic value of dysmobility syndrome for incident fracture needs to be further confirmed in prospective studies [8].
This study has several limitations. An inference on causality could not be made owing to the cross-sectional study design. Because the participants of the KURE study were recruited based on voluntary application, the potential of healthy volunteer bias cannot be ruled out. The assessments of non-VF were not confirmed by review of x-ray reports, which might have partly contributed to the attenuated association shown for non-VF in our data [25, 30]. BIA-measured lean mass and fat mass were used to define dysmobility syndrome instead of DXA-measured mass in the original definition by Binkley et al. [4]. Although lean mass and fat mass measured using BIA show good agreement with the values measured using DXA, and the cutpoint for BIA-measured lean mass endorsed by the AWGS guideline was used, the BIA method has a small but discernable tendency for overestimating lean mass and underestimating fat mass compared with DXA [16, 31]. Although the consensus for the optimal definition of dysmobility syndrome has not been reached yet, we found that the definitions used in this study showed a robust association with VF or any prevalent fracture despite applying different cutpoints for individual components as a modified definition.
In conclusion, dysmobility syndrome and its components were associated with elevated odds of morphometric VF or any prevalent fracture, independent of age and covariates. Dysmobility syndrome improved discrimination for fracture when added to the FRAX score. The prognostic value of dysmobility syndrome and the optimal cutpoint for its individual components need to be further investigated in a prospective study with incident fracture outcome.
References
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Arch Intern Med 159:1215–1220
Tran T, Bliuc D, van Geel T, Adachi JD, Berger C, van den Bergh J, Eisman JA, Geusens P, Goltzman D, Hanley DA, Josse RG, Kaiser SM, Kovacs CS, Langsetmo L, Prior JC, Nguyen TV, Center JR (2017) Population-wide impact of non-hip non-vertebral fractures on mortality. J Bone Miner Res 32:1802–1810
Binkley N, Blank RD, Leslie WD, Lewiecki EM, Eisman JA, Bilezikian JP (2017) Osteoporosis in crisis: it’s time to focus on fracture. J Bone Miner Res 32:1391–1394
Binkley N, Krueger D, Buehring B (2013) What’s in a name revisited: should osteoporosis and sarcopenia be considered components of “dysmobility syndrome?”. Osteoporos Int 24:2955–2959
Looker AC (2015) Dysmobility syndrome and mortality risk in US men and women age 50 years and older. Osteoporos Int 26:93–102
Lee WJ, Liu LK, Hwang AC, Peng LN, Lin MH, Chen LK (2017) Dysmobility syndrome and risk of mortality for community-dwelling middle-aged and older adults: the nexus of aging and body composition. Sci Rep 7:8785
Iolascon G, Moretti A, Giamattei MT, Migliaccio S, Gimigliano F (2015) Prevalent fragility fractures as risk factor for skeletal muscle function deficit and dysmobility syndrome in post-menopausal women. Aging Clin Exp Res 27(Suppl 1):S11–S16
Buehring B, Hansen KE, Lewis BL, Cummings SR, Lane NE, Binkley N, et al (2018) Dysmobility syndrome independently increases fracture risk in the osteoporotic fractures in men (MrOS) prospective cohort study. J Bone Miner Res. https://doi.org/10.1002/jbmr.3455
Kendler DL, Bauer DC, Davison KS, Dian L, Hanley DA, Harris ST et al (2016) Vertebral fractures: clinical importance and management. Am J Med 129(221):e221–e210
Lee EY, Kim HC, Rhee Y, Youm Y, Kim KM, Lee JM, Choi DP, Yun YM, Kim CO (2014) The Korean urban rural elderly cohort study: study design and protocol. BMC Geriatr 14:33
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D et al (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis: The Study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Lee EY, Lee SJ, Kim KM, Seo DH, Lee SW, Choi HS, Kim HC, Youm Y, Kim CO, Rhee Y (2017) Lower jump power rather than muscle mass itself is associated with vertebral fracture in community-dwelling elderly Korean women. Calcif Tissue Int 100:585–594
Duboeuf F, Bauer DC, Chapurlat RD, Dinten JM, Delmas P (2005) Assessment of vertebral fracture using densitometric morphometry. J Clin Densitom 8:362–368
Hong N, Kim CO, Youm Y, Kim HC, Rhee Y (2018) Low peak jump power is associated with elevated odds of dysmobility syndrome in community-dwelling elderly individuals: the Korean Urban Rural Elderly (KURE) study. Osteoporos Int 29:1427–1436. https://doi.org/10.1007/s00198-018-4466-0
Bischoff HA, Stahelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M et al (2003) Identifying a cut-off point for normal mobility: a comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing 32:315–320
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JSW, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101
Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B (2001) Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J Gerontol A Biol Sci Med Sci 56:M366–M372
Chun MY (2012) Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med 33:144–151
O’Bryant SE, Humphreys JD, Smith GE, Ivnik RJ, Graff-Radford NR, Petersen RC et al (2008) Detecting dementia with the mini-mental state examination in highly educated individuals. Arch Neurol 65:963–967
Anonymous (1968) Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser 405:5–37
Youden WJ (1950) Index for rating diagnostic tests. Cancer 3:32–35
Pencina MJ, Steyerberg EW, D’Agostino RB (2011) Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med 30:11–21
Clynes MA, Edwards MH, Buehring B, Dennison EM, Binkley N, Cooper C (2015) Definitions of sarcopenia: associations with previous falls and fracture in a population sample. Calcif Tissue Int 97:445–452
Hill KD, Farrier K, Russell M, Burton E (2017) Dysmobility syndrome: current perspectives. Clin Interv Aging 12:145–152
Braun BL, Gerberich SG, Sidney S (1994) Injury events: utility of self report in retrospective identification in the USA. J Epidemiol Community Health 48:604–605
Johansson H, Oden A, McCloskey EV, Kanis JA (2014) Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos Int 25:235–241
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20:1813–1819
Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman E et al (2004) Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone 34:195–202
Nguyen TV (2018) Individualized fracture risk assessment: state-of-the-art and room for improvement. Osteoporosis and Sarcopenia 4:2–10
Fleming J, Matthews FE, Brayne C, Cambridge City over-75s Cohort study c (2008) Falls in advanced old age: recalled falls and prospective follow-up of over-90-year-olds in the Cambridge City over-75s Cohort study. BMC Geriatr 8:6
Sun G, French CR, Martin GR, Younghusband B, Green RC, Xie YG, Mathews M, Barron JR, Fitzpatrick DG, Gulliver W, Zhang H (2005) Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am J Clin Nutr 81:74–78
Acknowledgements
We thank all our participants and the technical staff of the KURE study.
Funding
This study was funded by the Research of Korea Centers for Disease Control and Prevention (2013-E63007-01, 2013-E63007-02).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Institutional Review Board (IRB) of Severance Hospital (IRB no. 4-2012-0172), with written informed consent obtained from all participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the IRB and with the 1964 Helsinki Declaration and its later amendments.
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Hong, N., Kim, C.O., Youm, Y. et al. Dysmobility syndrome is associated with prevalent morphometric vertebral fracture in older adults: the Korean Urban-Rural Elderly (KURE) study. Arch Osteoporos 13, 86 (2018). https://doi.org/10.1007/s11657-018-0500-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0500-2