Abstract
Summary
Osteoporosis in elderly men is an under-recognized problem. In the current study, we intend to look at the performance of two risk assessment tools [OSTA and MORES] for the diagnosis of osteoporosis. Osteoporosis was seen in 1/4th of elderly men at spine and 1/6th of them at femoral neck. Both risk assessment tools were found to have good sensitivity in predicting osteoporosis at spine and femoral neck with good area under curve (AUC).
Purpose
This study attempts to look at the performance of osteoporosis self-assessment tool for Asians (OSTA) and male osteoporosis risk estimation score (MORES) for predicting osteoporosis in south Indian rural elderly men.
Methods
Five hundred and twelve men above 65 years of age from a south Indian rural community were recruited by cluster random sampling. All subjects underwent detailed clinical, anthropometric, and bone mineral density measurement at lumbar spine and femoral neck using dual-energy X-ray absorptiometry scan. A T score ≤ − 2.5 was diagnostic of osteoporosis. Scores for OSTA and MORES were calculated at various cut offs, and their sensitivities and specificities for predicting osteoporosis were derived.
Results
The prevalence of osteoporosis was found to be 16% at femoral neck and 23% at spine. OSTA with a cut-off value of ≤2 predicted osteoporosis with a sensitivity and specificity at lumbar spine of 94 and 17% and at femoral neck of 99 and 18%. The area under ROC curve for OSTA index for spine was 0.716 and for femoral neck was 0.778. MORES with a cut-off value of ≥6 predicted osteoporosis at spine with a sensitivity of 98% and specificity of 15%, and at femoral neck, they were 98 and 13%, respectively. The area under ROC curve for MORES for spine was 0.855 and for femoral neck was 0.760.
Conclusion
OSTA and MORES were found to be useful screening tools for predicting osteoporosis in Indian elderly men. These tools are simple, easy to perform, and cost effective in the context of rural Indian setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis in men is an under-recognized public health problem in an Indian context. Its incidence is showing a rising trend due to an increase in the life expectancy [1]. There is an increased risk of morbidity and mortality among the elderly people with an osteoporotic fracture, the risk being more in men when compared to women [2]. About 100 million Indian men are above the age of 50 years. Two third of this population is in the rural areas of India [3]. The prevalence of osteoporosis in men with age above 50 years, in various parts of India has been reported from 8 to 25% [4–6].
Measurement of the bone mineral density (BMD) by dual energy X-ray absorptiometry (DXA) scan is considered as the gold standard test for the determining bone strength and also is the best predictor for assessing the risk of fractures [7, 8]. There are about 300–350 DXA scanners available in India and most of them are located in cities. They are expensive and not accessible to most of the rural population. So, there is a need for usage of more simple screening tools for assessment of the osteoporosis risk. There are simple screening tools incorporated with various risk factors which have been used in other countries to predict the risk of osteoporosis, like body weight criterion (BWC), Garvan fracture risk calculator (GARVAN), male osteoporosis screening tool (MOST), osteoporosis Self-Assessment Tool for Asians (OSTA), and male osteoporosis risk estimation score (MORES) [9–11]. Recently, a study from north India documented a poor sensitivity for FRAX when compared to OSTA as a screening tool for the assessment of the risk of osteoporosis [11]. There is paucity of studies in this regard from the rural elderly population of India. So, we attempted to study the predictive ability of two screening tools (OSTA and MORES) in assessing the risk of osteoporosis in rural south Indian men.
Materials and methods
This was a cross sectional study conducted over a period of 1 year from Jan 2015–Dec 2015. Ambulatory men with age more than 65 years from three villages of Vellore district of Tamil Nadu in southern part of India were recruited in the study by cluster random sampling. Written informed consent was taken from all the subjects enrolled in the study. The study protocol was approved by the Institutional Ethics Review Board.
Men with a history of hyperthyroidism, hyperparathyroidism, hypogonadism, malabsorption, chronic liver disease or renal disease, and those on medications such as antiretroviral therapy, anti-tuberculous therapy, or anticonvulsants which can affect the bone health were excluded. Subjects with prior diagnosis of osteoporosis or history of treatment for osteoporosis were also excluded. The details of the subject with respect to demographics, detailed medical history, and anthropometry including height and weight were noted by a trained social worker. Height was measured on wall mounted stadiometer and weight on a digital weighing scale.
BMD was assessed using the Hologic DXA QDR 4500 Discovery A machine at the lumbar spine and femoral neck by the same technician with the precision of 2% at both the measured sites (spine and neck of femur). The WHO classification was used for categorization of BMD; lowest T score, osteoporosis ≤−2.5, osteopenia, or low bone mass −1 to −2.5 and normal as >−1 [12]. The OSTA index was calculated for each subject by using the formula [wt (kg) – age (yr)]/5. An OSTA index value of ≤2 was taken for assessment cut off to predict osteoporosis. Various cut off values of OSTA were assessed to predict osteoporosis at spine and femoral neck. MORES takes into account the age, weight, and history of chronic obstructive pulmonary disease (COPD) with each component being allotted point score and the final score (MORES of ≥6 points was considered significant) being the summation of all the components as shown below [13].
Age (years) | Cut off points |
|---|---|
≤55 | 0 |
56–74 | 3 |
≥75 | 4 |
Weight (kgs) | |
≤70 | 6 |
71–80 | 4 |
≥80 | 0 |
COPD present | 3 |
Statistical analysis
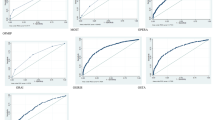
Statistical analysis was done using SPSSv.16. software (IBM Corp., USA). Receiver operating characteristic (ROC) curve was constructed to look at various sensitivities and specificities for 2 screening tools (OSTA and MORES) for the diagnosis of osteoporosis at either site (T score ≤−2.5) or which will better predict osteoporosis. Various cut-offs of OSTA and MORES in relation to sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were estimated.
Results
Five hundred twelve elderly men above the age of 65 years were included in the study. The mean ± SD for age, weight, and BMI were 71.9 ± 5.2 years, 73.6 ± 8.7 kg and 25.8 ± 4.2 kg/m2, respectively. Overall, the prevalence of osteoporosis was 23% at spine and 16% at femoral neck.
An OSTA index with a cut-off of ≤+2 predicted the risk of osteoporosis with a sensitivity of 94% and specificity of 17% at spine and at femoral neck with a sensitivity of 99% and specificity of 18%. The area under ROC curve for OSTA index for spine was 0.716 and for femoral neck was 0.778. Various cut-off values for OSTA and MORES for predicting osteoporosis at spine with their sensitivities, specificities, PPV, and NPV are shown in Fig. 1 and for femoral neck in Fig. 2. The MORES with a cut-off of ≥6 predicted osteoporosis with a sensitivity of 98% and a specificity of 15% at spine, and they were 98 and 13%, respectively, at femoral neck. The area under ROC curve for MORES for spine was 0.855 and for femoral neck was 0.760.
Discussion
To best of our knowledge, it is first study from rural India in elderly men to look at the validity of screening tools (OSTA and MORES) in predicting osteoporosis. About one fifth of men had osteoporosis at spine and one sixth at femoral neck which is comparable to previous studies [4–6]. In our study, OSTA index with a cut-off value of ≤2 and MORES with a cut off value of ≥6 predicted osteoporosis with a good sensitivity at spine and femoral neck at the cost of low specificity. A cut off value of +1 for OSTA had a better specificity (27%) at both sites without compromising sensitivity.
OSTA is a screening tool, although there was no single exact cut-off value which could predict osteoporosis with good sensitivity and specificity. Various cut-off values have been studied with different population and ethnicities and have been validated in various ethnic groups like oriental postmenopausal women [14, 15], elderly Caucasian women [16], US veteran men [17], and elderly Chinese men [18]. A north Indian study showed that OSTA index with a cut-off value ≤2 predicted osteoporosis with a sensitivity of 95.7% and specificity of 33.6% and was better than FRAX [11]. A recent meta-analysis of the studies that look into the performance of OSTA showed that a cut-off threshold of 3 had a sensitivity and specificity of 88 and 55%, respectively [19].
MORES is another validated cost-effective screening tool and was considered superior when compared to FRAX for predicting osteoporosis in men. MORES with a cut-off value of ≥6 in predicting osteoporosis with remarkably high sensitivity shown in our study has been demonstrated previously [10, 13]. Although, MORES has an additional component of COPD, in addition to the age and weight in the criterion, its performance was almost same as OSTA.
Osteoporosis in elderly rural Indian men is an under-recognized public health problem. With the rapid changes in the adaptation of life-style and an increase in the life expectancy, osteoporosis in men will be a major public health issue. Though BMD measurement by DXA scan is considered as gold standard for diagnosis, its utility in developing countries particularly in rural areas is limited because of the lack of availability and high cost of the DXA equipment. Simple cost-effective screening tools will be thus be helpful for the primary care physicians particularly in rural areas, for detecting individuals at risk of osteoporosis and fractures.
So, the results of this study show that both OSTA and MORES can perform well as screening tools in deciding which subset of subjects needs DXA scan for the assessment for risk of osteoporosis.
Conclusion
OSTA and MORES were better cost effective screening tools in predicting osteoporosis in rural elderly Indian men. However, these results need to be validated by large follow-up cohort studies.
References
Kanis JA, Johnell O, Oden A, Laet CD, Mellstrom D (2004) Epidemiology of osteoporosis and fracture in men. Calcif Tissue Int 75(2):90–99
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390
Mithal A, Bansal B, Kyer CS, Ebeling P (2014) The Asia-Pacific regional audit-epidemiology, costs and burden of osteoporosis in India 2013: a report of international osteoporosis foundation. Indian J Endocrinol Metab 18(4):449–454
Marwaha RK, Tandon N, Garg MK, Kanwar R, Narang A, Sastry A et al (2011) Bone health in healthy Indian population aged 50 years and above. Osteoporos Int 22(11):2829–2836
Shetty S, Kapoor N, Naik D, Asha HS, Prabu S, Thomas N, et al. Osteoporosis in healthy South Indian males and the influence of life style factors and vitamin d status on bone mineral density. J Osteoporos. 10.1155/2014/723238
Agrawal NK, Sharma B (2013) Prevalence of osteoporosis in otherwise healthy Indian males aged 50 years and above. Arch Osteoporos 8:116
U.S. Preventive Services Task Force (2002) Screening for osteoporosis in postmenopausal women: recommendations and rationale. Ann Intern Med 137(6):526–528
Genant HK, Cooper C, Poor G, Reid I, Ehrlich G, Kanis J et al (1999) Interim report and recommendations of the World Health Organization task-force for osteoporosis. Osteoporos Int 10(4):259–264
Chen S-J, Chen Y-J, Cheng C-H, Hwang H-F, Chen C-Y, Lin M-R (2016) Comparisons of different screening tools for identifying fracture/osteoporosis risk among community-dwelling older people. Medicine (Baltimore) 95(20):e3415
Cass AR, Shepherd AJ, Asirot R, Mahajan M, Nizami M (2016) Comparison of the male osteoporosis risk estimation score (MORES) with FRAX in identifying men at risk for osteoporosis. Ann Fam Med 14(4):365–369
Bhat KA, Kakaji M, Awasthi A, Kumar K, Mishra K, Shukla M et al (2016) Utility of osteoporosis self-assessment tool as a screening tool for predicting osteoporosis in Indian men. J Clin Densitom. doi:10.1016/j.jocd.2016.04.005
Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994;843:1–129
Cass AR, Shepherd AJ (2013) Validation of the male osteoporosis risk estimation score (MORES) in a primary care setting. J Am Board Fam Med 26(4):436–444
Koh LK, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP et al (2001) A simple tool to identify asian women at increased risk of osteoporosis. Osteoporos Int 12(8):699–705
Yang Y, Wang B, Fei Q, Meng Q, Li D, Tang H et al (2013) Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporotic vertebral fractures in postmenopausal Chinese women in Beijing. BMC Musculoskelet Disord 14:271
Richy F, Gourlay M, Ross PD, Sen SS, Radican L, De Ceulaer F et al (2004) Validation and comparative evaluation of the osteoporosis self-assessment tool (OST) in a Caucasian population from Belgium. QJM 97(1):39–46
Steuart Richards J, Lazzari AA, Teves Qualler DA, Desale S, Howard R, Kerr GS (2014) Validation of the osteoporosis self-assessment tool in US male veterans. J Clin Densitom 17(1):32–37
Zha X-Y, Hu Y, Pang X-N, Chang G-L, Li L (2015) Diagnostic value of osteoporosis self-assessment tool for Asians (OSTA) and quantitative bone ultrasound (QUS) in detecting high-risk populations for osteoporosis among elderly Chinese men. J Bone Miner Metab 33(2):230–238
Nayak S, Edwards DL, Saleh AA, Greenspan SL (2015) Systematic review and meta-analysis of the performance of clinical risk assessment instruments for screening for osteoporosis or low bone density. Osteoporos Int 26(5):1543–1554
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Satyaraddi, A., Shetty, S., Kapoor, N. et al. Performance of risk assessment tools for predicting osteoporosis in south Indian rural elderly men. Arch Osteoporos 12, 35 (2017). https://doi.org/10.1007/s11657-017-0332-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-017-0332-5