Abstract
Epithelial inflammation and eosinophil infiltration are crucial for the pathogenesis of asthma. Many inflammatory mediators, such as YKL-40, interleukin −5 (IL-5), granulocyte-macrophage colony-stimulating factor (GM-CSF), and eotaxin, are important for the development of allergic airway inflammation. This study is aimed at investigating the impact of treatment with ovalbumin (OVA) on the levels of those inflammatory mediators in primarily cultured mouse tracheal epithelial cells. Mouse tracheal epithelial cells were isolated and identified by immunofluorescent staining; the isolated mouse tracheal epithelial cells expressed cytokeratins. Treatment with OVA for 24 or 48 h significantly increased the relative levels of YKL-40, IL-5, GM-CSF, and eotaxin mRNA transcripts and YKL-40, IL-5, GM-CSF, and eotaxin proteins secreted in the supernatants of cultured cells, as compared with that in the untreated control cells (P < 0.01, P < 0.05, respectively). The levels of YKL-40 expression were correlated positively with the levels of IL-5, GM-CSF, and eotaxin expression in the OVA-treated cells. These data indicated that treatment with OVA simultaneously enhanced YKL-40, IL-5, GM-CSF, and eotaxin expression in the cultured mouse tracheal epithelial cells in vitro. These inflammatory mediators may synergistically contribute to the pathogenesis of allergic inflammation, and this study may help to understand the role of YKL-40 in the pathogenesis of asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epithelial inflammation and eosinophil infiltration are crucial for the pathogenesis of asthma. Currently, the pathogenesis of asthma is not fully understood. The airway epithelium acts as a mechanical barrier and an active interface between the inner and outer environments, and can directly expose to environmental irritants, allergens, and noxious stimuli associated with airway inflammation (Holgate et al. 2009; Fahy and Locksley 2011; Holgate 2011). These noxious substances can activate epithelial cells to produce a large of proinflammatory mediators, such as interleukin (IL)-5 (Kouro and Takatsu 2009; Fahy and Locksley 2011), granulocyte–macrophage colony-stimulating factor (GM-CSF) (Wu et al. 2011; Mir-Kasimov et al. 2012), and eotaxin (Ben et al. 2008; Zhou et al. 2012). These inflammatory mediators can stimulate the proliferation, differentiation, activation, and chemoattraction of various inflammatory cells in the airway mucosa, where inflammatory cells interact with epithelial cells, leading to airway inflammation and epithelial cell damage (Hamid and Tulic 2009; Holgate 2011). However, little is known about whether an allergen can simultaneously induce the expression of multiple cytokines and chemokines in epithelial cells.
YKL-40, also known as chitinase-3-like protein 1, is a glycoprotein secreted by macrophages, chondrocytes, neutrophils, synovial cells, and epithelial cells (Mizoguchi 2006; Bussink et al. 2007; Chupp et al. 2007; Funkhouser and Aronson 2007). A previous study has shown that high levels of serum YKL-40 are associated with an increased risk of the development of asthma, and the levels of serum YKL-40 are correlated positively with the severity of asthma and the thickness of the subepithelial basement membrane (Chupp et al. 2007). Furthermore, the levels of serum YKL-40 are correlated negatively with pulmonary function (Chupp et al. 2007). Apparently, YKL-40 is an inducer of Th2 responses and crucial for the development of asthma (Chupp et al. 2007). YKL-40 enhances Th2 responses by increasing IL-13 or IL-5 production and inhibiting T cell apoptosis as well as supporting cell survival. YKL-40 and Th2 cytokines can also further positively feedback-regulated YKL-40 production by regulating cell death responses or alternative macrophage activation (Lee and Elias 2010). However, it is unclear whether the YKL-40 expression is associated with IL-5, GM-CSF, and eotaxin expression in tracheal epithelial cells.
In this study, we employed mouse tracheal epithelial cells as a model to test the impact of treatment with OVA on the levels of YKL-40, IL-5, GM-CSF, and eotaxin expression and determined the potential relationship among these inflammatory mediators in vitro. We found that OVA enhanced YKL-40, IL-5, GM-CSF, and eotaxin expression simultaneously in mouse tracheal epithelial cells in vitro. We discussed the implications of our findings.
Material and Methods
Mice.
Female and male C57BL/6N mice at 5–8 wk of age were obtained from the Animal Experiment Center of Nantong University and housed in a specific pathogen-free facility with free access to normal chow and water. The experimental protocols were approved by the animal, ethics, and gene recombination experiment safety management committee of the Institute of Medical Science, Nantong University.
Isolation and culture of tracheal epithelial cells.
Airway epithelial cells were isolated and cultured, as described previously (Davidson et al. 2000) with minor modifications. Briefly, mice were sacrificed and their tracheas were dissected out. After being washed with cold Dulbecco's modified Eagle medium containing nutrient mixture F-12, the tracheae tissues were cut into small pieces and digested with collagenase at 37°C overnight with gently shaking. The prepared single cells (3–5 × 107 cells/10 cm2) were cultured and submerged in bronchial epithelial cell growth medium (BEGM, Clonetics, Walkersville, MD) supplemented with bovine pituitary extract (52 μg/ml; Sigma, St. Louis, MO), transferrin (10 μg/ml; Sigma), human recombinant EGF (0.5 ng/ml; Chemicon, Temecula, CA), hydrocortisone (0.5 μg/ml; Lianshuo, Shanghai, China), epinephrine (0.5 μg/ml; Solarbio, Beijing, China), insulin (5 μg/ml; Sigma), penicillin–streptomycin mixture (100 U/ml; Gibco BRL, Grand Island, NY) at 37°C in 5% CO2. Three days later, the suspended cells were removed by washing three times. The adherent epithelial cells were then continuously cultured for 3–5 wk. After reaching confluency, the cells were digested with trypsin/EDTA for 5 min at 37°C and diluted 1:2 at each passage. These tracheal epithelial cells (passage 3) were collected and then used for this study.
Immunofluorescence assay.
Primary mouse tracheal epithelial cells were cultured in 24-well coverslip chambers overnight. The cells were fixed with 4% paraformaldehyde in PBS, permeabilized with 0.3% Triton-X-100 (Sigma) for 15 min, and blocked with 1% BSA for 2 h. Subsequently, the cells were incubated with primary antibodies: Pan cytokeratin (1:300, BM0030, Boster, Wuhan, China) at 4°C for 18 h. After being washed, the bound antibodies were detected with FITC-labeled goat anti-mouse IgG (1:40, BA1101, Boster) at room temperature for 2 h and co-stained with DAPI (C1005, Beyotime Biotechnology, Nantong, China), followed by mounting on slides. The immunofluorescent staining was analyzed using a Leica laser scanning spectral confocal microscope.
ELISA.
Primary mouse tracheal epithelial cells (8 × 105 cells/well) were treated in triplicate with, or without, 200 μg/ml of OVA (Sigma) for 24 or 48 h, as described previously (Okamoto et al. 2009). Their supernatants were harvested and the concentrations of YKL-40, IL-5, eotaxin, and GM-CSF in the supernatants were measured using cytokine-specific ELISA kits (R&D Systems, Minneapolis, MN), according to the manufacturers' instruction. The limitation of detection for YKL-40, IL-5, eotaxin, or GM-CSF ELISA is 5 μg/L, 1, 2, or 15 ng/L, respectively.
Western blot analysis.
Primary mouse tracheal epithelial cells (8 × 105 cells/well) were treated in triplicate with, or without, 200 μg/ml of OVA for 24 or 48 h, and the cells were harvested, followed by lyzing in lysis buffer. After quantification of protein concentrations using a NanoPhotometerTM kit (IMPLEN, Westlake Village, CA), the cell lysates (20 μg/lane) from the different groups of cells were subjected to sodium dodecyl sulfate polyacrylamide gel electrophoresis on 10% polyacrylamide gel and transferred onto polyvinylidine difluoride membranes (Millipore, Billerica, MA). The membranes were blocked in 5% BSA and incubated with primary antibodies against YKL-40 (1:200, Bios, Beijing, China) or tubulin (1:5,000, Bioworld Technology, St. Louis, MN) for 16 h at 4°C. After being washed, the bound antibodies were detected with horseradish peroxidase-conjugated secondary antibodies (1:1,000, Beyotime Biotechnology) and visualized using the ultra-enhanced chemiluminescence Western blotting detection reagents (Beyotime Biotechnology). The relative levels of YKL-40 to β-tubulin were analyzed by densimetric scanning using the ImageJ software and calculated first by normalizing to the control.
Reverse transcription-polymerase chain reaction and polymerase chain reaction.
Total RNA was extracted from epithelial cells that had been treated with, or without, OVA for 48 h using the TRIzol reagent (Invitrogen, Carlsbad, CA), according to the manufacturers' instruction. After quantification, one portion of the total RNA (3 μg) was transcribed reversely in triplicate into cDNA using the First-Strand cDNA synthesis kit (Roche, Mannheim, Germany), following the standard protocol. The relative levels of YKL-40, IL-5, eotaxin, and GM-CSF mRNA transcripts to the control GAPDH were determined by semiquantitative PCR using Taq master mix (2×; OMEGA, Norcross, GA) and specific primers. The sequences of primers are shown in Table 1. Amplifications were performed at 95°C for 2 min and subjected to 40 cycles of 95°C for 30 s, 60°C for 30s, and 72°C for 30s, followed by extension at 72°C for 10 min. The PCR products were analyzed by 2% agarose gel containing Gold View (Solarbio). The relative levels of each target gene mRNA transcripts to the control GAPDH were determined by densimetric analysis and calculated by first normalizing to the control GAPDH.
Statistical Analysis
Data are presented as the means ± SEM. The difference among groups was analyzed by one-way or two-way ANOVA and Student's t tests using SPSS software, version 18.0 (SPSS, Chicago IL) or Graph Pad Prism 5. The potential correlation between two measures was assessed using Pearson correlation analysis. A P value of <0.05 was considered statistically significant.
Results
Identification of murine primarily cultured tracheal epithelial cells.
The cultured tracheal epithelial cells were stained with anti-pan cytokeratins and FITC-goat anti mouse IgG, and examined under a fluorescent microscope. Approximately, 95% of the cultured cells were stained by anti-pan cytokeratins, a family of intermediate filaments in epithelial cell cytoskeleton in Fig. 1. These data indicated that majority of cultured cells had the features of epithelial cells.
Immunofluorescent analysis of the isolated mouse tracheal epithelial cells. The primarily cultured tracheal epithelial cells from C57BL/6N mice were fixed, permeabilized, and incubated with mouse antibodies against pan cytokeratins. After being washed, the bound antibodies were detected with FITC-labeled goat anti-mouse IgG (green) and co-stained with DAPI (blue), followed by analysis using a confocal microscope. Data shown are representative images (magnification ×400) from three separate experiments. Scale bars indicate 200 μm.
Expression of YKL-40 in ovalbumin-treated tracheal epithelial cells.
Next, we examined the impact of treatment with OVA on the levels of YKL-40 expression in tracheal epithelial cells. Mouse tracheal epithelial cells were treated with, or without, OVA (200 μg/ml) for 24 or 48 h. The relative levels of YKL-40 mRNA transcripts to the control GAPDH were detected by RT-PCR. As shown in Fig. 2, the relative levels of YKL-40 mRNA transcripts in the OVA-treated cells were significantly higher than that in the control cells without OVA treatment (P < 0.01), and the stimulatory effects of OVA appeared to be time-dependent (P < 0.05, Fig. 2a, b ). A similar pattern of YKL-40 protein was detected in the cultured cells and their supernatants (Fig. 2c–e ), as determined by Western blot and ELISA. Collectively, our data indicated that treatment with OVA enhanced YKL-40 expression in mouse tracheal epithelial cells in vitro.
Characterization of YKL-40 expression. The tracheal epithelial cells were treated with, or without, OVA for the indicated time periods. The relative levels of YKL-40 mRNA transcripts to the control GAPDH were determined by RT-PCR (a), and the data were semiquantitatively analyzed by desimetric scanning (b). The relative levels of YKL-40 protein to control β-tubulin were determined by Western blot assay (c–d). Finally, the concentrations of YKL-40 in the supernatants of cultured epithelial cells were determined by ELISA (e). Data are representative images or expressed as the mean ± SEM of different groups of cells from three separate experiments. *P < 0.05; **P < 0.01 versus the untreated control cells.
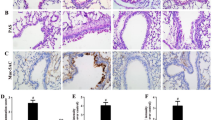
Expression of IL-5, GM-CSF, and eotaxin in the ovalbumin-treated tracheal epithelial cells.
IL-5, GM-CSF, and eotaxin are usually upregulated within the tracheal epithelial tissues of asthmatic subjects, and they are crucial for the recruitment of inflammatory infiltrates during the pathogenesis of airway inflammation (Finkelman et al. 2010; Fortin et al. 2010; Nakagome and Nagata 2011). We further examined the impact of OVA treatment on the levels of IL-5, GM-CSF, and eotaxin expression in mouse tracheal epithelial cells. Following treatment with OVA for 24 or 48 h, the relative levels of IL-5, GM-CSF, and eotaxin mRNA transcripts were determined by RT-PCR. As shown in Figs. 3a, b , treatment with OVA for either 24 or 48 h significantly enhanced the levels of IL-5, GM-CSF, and eotaxin mRNA transcripts in tracheal epithelial cells, related to that in the untreated control cells, and the levels of eotaxin, but not IL-5 and GM-CSF, mRNA transcripts in the cells treated with OVA for 48 h were significantly higher than that in the cells treated with OVA for 24 h (P < 0.01), a trend of time-dependent.
Characterization of IL-5, GM-CSF and Eotaxin expression. The tracheal epithelial cells were treated with, or without, OVA for the indicated time periods. The relative levels of IL-5, GM-CSF and Eotaxin mRNA transcripts to the control GAPDH were determined semi-quantitative RT-PCR (a) and semi-quantitatively analyzed by densimetric scanning (b). The concentrations of IL-5, GM-CSF and Eotaxin in the supernatants of cultured epithelial cells were determined by ELISA (C-E). Data are representative images or expressed as the mean ± SEM of different groups of cells from three separate experiments. * P < 0.05; ** P < 0.01 vs. the untreated control cells.
ELISA analysis revealed that treatment with OVA for either 24 or 48 h also significantly increased the concentrations of IL-5, GM-CSF, and eotaxin in the supernatants of cultured tracheal epithelial cells (P < 0.05, Fig. 3c–e ). Together, our data clearly demonstrated that treatment with OVA enhanced IL-5, GM-CSF, and eotaxin expression in primarily cultured mouse tracheal epithelial cells in vitro.
Further analyses indicated that the levels of YKL-40 expression were correlated positively with the levels of IL-5 (r = 0.847, P < 0.0001; Fig. 4a ), GM-CSF (r = 0.869, P < 0.0001; Fig. 4b ), and eotaxin (r = 0.923, P < 0.0001; Fig. 4c ) in the cultured mouse tracheal epithelial cells. Therefore, OVA treatment enhanced the YKL-40, IL-5, GM-CSF, and eotaxin expression simultaneously in mouse tracheal epithelial cells.
The correlation analysis. The potential correlations between the levels of YKL-40 and the concentrations of IL-5, GM-CSF, and eotaxin in the supernatants of cultured tracheal epithelial cells were analyzed using the Pearson correlation analysis. Data are the mean values of YKL-40 levels against the values of IL-5, GM-CSF, and eotaxin in individual wells of cells tested. a, The correlation between the levels of YKL-40 and IL-5. b, The correlation between the levels of YKL-40 and GM-CSF. c, The correlation between the levels of YKL-40 and eotaxin.
Discussion
YKL-40 plays a vital role in airway inflammation and remodeling (Chupp et al. 2007), and higher levels of YKL-40 are detected in patients with inflammatory diseases (Kawada et al. 2007; Kucur et al. 2007; Lee et al. 2011). A recent study has shown that higher levels of circulating YKL-40 are present in patients with asthma (Ober et al. 2008), although its role remains controversial (Specjalski and Jassem 2011). Given that inflammation in the airway epithelial cells is crucial for the development and progression of asthma, we examined the impact of treatment with OVA on the expression of YKL-40, IL-5, GM-CSF, and eotaxin in primarily cultured tracheal epithelial cells in vitro. We found that treatment with OVA significantly upregulated YKL-40 expression in tracheal epithelial cells in a time-dependent manner. Furthermore, treatment with OVA enhanced the IL-5, GM-CSF, and eotaxin expression in tracheal epithelial cells in vitro. More importantly, the levels of YKL-40 expression were correlated positively with the levels of IL-5, GM-CSF, and eotaxin in the OVA-treated epithelial cells. These data clearly demonstrated that treatment with OVA simultaneously enhanced the expression of proinflammatory mediators in the tracheal epithelial cells. Our findings suggest that OVA may interact with some unknown factors/receptors to activate the downstream signals and in turn promote the expression of proinflammatory mediators in mouse tracheal epithelial cells. However, the mechanisms underlying the regulatory effect of OVA remain to be further investigated.
Eosinophilic infiltration is a hallmark of allergic inflammation in mouse models of asthma and human patients (Akuthota and Weller 2012; Molfino 2012; Petsky et al. 2012) and is associated with epithelial damage (Gong et al. 2012; Lambrecht and Hammad 2012). The airway epithelial cells can secrete inflammatory mediators, such as eotaxin, IL-5, and GM-CSF, which are potent chemotactic factors for the recruitment of eosinophils through the CCR3 receptor, contributing to airway inflammation. Furthermore, these mediators can also recruit the inflammatory progenitor cells into the inflammatory site (Allakhverdi et al. 2009; Allakhverdi and Delespesse 2012). It is notable that the levels of YKL-40 are associated with the degrees of eosinophil infiltration in asthmatic patients (Ober et al. 2008) and that YKL-40 can stimulate the migration of IL-4+ eosinophils and basophils into the inflammatory lungs (Reese et al. 2007). We found that treatment with OVA simultaneously enhanced YKL-40, IL-5, GM-CSF, and eotaxin expression in tracheal epithelial cells. These data suggest that YKL-40 may participate in the network of inflammatory mediators that regulate eosinophil-mediated airway inflammation and contribute to the pathogenesis of asthma. We are interested in further investigating the regulatory roles of these inflammatory mediators in the allergic airway inflammation-mediated epithelial damage in vivo. Therefore, our findings may provide new insights into the pathogenesis of asthma.
In summary, our data suggest that YKL-40 may be an active player in the process of airway inflammation-mediated epithelial damage. Future studies are necessary to illustrate whether YKL-40 can enhance IL-5, GM-CSF, and eotaxin expression and the potential mechanisms by which an allergen enhances the production of inflammatory mediator in the tracheal epithelial cells.
References
Akuthota P.; Weller P. F. Eosinophils and disease pathogenesis. Seminars in hematology 49: 113–119; 2012.
Allakhverdi Z.; Comeau M. R.; Smith D. E.; Toy D.; Endam L. M.; Desrosiers M.; Liu Y. J.; Howie K. J.; Denburg J. A.; Gauvreau G. M.; Delespesse G. CD34+ hemopoietic progenitor cells are potent effectors of allergic inflammation. J Allergy Clin Immunol 123: 472–478; 2009.
Allakhverdi Z.; Delespesse G. Hematopoietic progenitor cells are innate Th2 cytokine-producing cells. Allergy 67: 4–9; 2012.
Ben S.; Li X.; Xu F.; Xu W.; Li W.; Wu Z.; Huang H.; Shi H.; Shen H. Treatment with anti-CC chemokine receptor 3 monoclonal antibody or dexamethasone inhibits the migration and differentiation of bone marrow CD34 progenitor cells in an allergic mouse model. Allergy 63: 1164–1176; 2008.
Bussink A. P.; Speijer D.; Aerts J. M.; Boot R. G. Evolution of mammalian chitinase (−like) members of family 18 glycosyl hydrolases. Genetics 177: 959–970; 2007.
Chupp G. L.; Lee C. G.; Jarjour N.; Shim Y. M.; Holm C. T.; He S.; Dziura J. D.; Reed J.; Coyle A. J.; Kiener P.; Cullen M.; Grandsaigne M.; Dombret M. C.; Aubier M.; Pretolani M.; Elias J. A. A chitinase-like protein in the lung and circulation of patients with severe asthma. N Engl J Med 357: 2016–2027; 2007.
Davidson D. J.; Kilanowski F. M.; Randell S. H.; Sheppard D. N.; Dorin J. R. A primary culture model of differentiated murine tracheal epithelium. Am J Physiol Lung Cell Mol Physiol 279: L766–778; 2000.
Fahy J. V.; Locksley R. M. The airway epithelium as a regulator of Th2 responses in asthma. Am J Respir Crit Care Med 184: 390–392; 2011.
Finkelman F. D.; Hogan S. P.; Hershey G. K.; Rothenberg M. E.; Wills-Karp M. Importance of cytokines in murine allergic airway disease and human asthma. J Immunol 184: 1663–1674; 2010.
Fortin M.; Wagner J. G.; Brault J.; Harkema J. R.; Renzi P. M.; Paquet L.; Ferrari N. Spatial and temporal expression of CCR3 and the common beta chain of the IL-3, IL-5, and GM-CSF receptor in the nasal epithelium and lymphoid tissues in a rat model of allergic rhinitis. Cytokine 52: 194–202; 2010.
Funkhouser J. D.; Aronson Jr. N. N. Chitinase family GH18: evolutionary insights from the genomic history of a diverse protein family. BMC Evol Biol 7: 96; 2007.
Gong J. H.; Shin D.; Han S. Y.; Kim J. L.; Kang Y. H. Kaempferol suppresses eosinophil infiltration and airway inflammation in airway epithelial cells and in mice with allergic asthma. J Nutr 142: 47–56; 2012.
Hamid Q.; Tulic M. Immunobiology of asthma. Annual review of physiology 71: 489–507; 2009.
Holgate S. T. The sentinel role of the airway epithelium in asthma pathogenesis. Immunol Rev 242: 205–219; 2011.
Holgate S. T.; Roberts G.; Arshad H. S.; Howarth P. H.; Davies D. E. The role of the airway epithelium and its interaction with environmental factors in asthma pathogenesis. Proc Am Thorac Soc 6: 655–659; 2009.
Kawada M.; Hachiya Y.; Arihiro A.; Mizoguchi E. Role of mammalian chitinases in inflammatory conditions. Keio J Med 56: 21–27; 2007.
Kouro T.; Takatsu K. IL-5- and eosinophil-mediated inflammation: from discovery to therapy. International immunology 21: 1303–1309; 2009.
Kucur M.; Isman F. K.; Karadag B.; Vural V. A.; Tavsanoglu S. Serum YKL-40 levels in patients with coronary artery disease. Coron Artery Dis 18: 391–396; 2007.
Lambrecht B. N.; Hammad H. The airway epithelium in asthma. Nat Med 18: 684–692; 2012.
Lee C. G.; Da Silva C. A.; Dela Cruz C. S.; Ahangari F.; Ma B.; Kang M. J.; He C. H.; Takyar S.; Elias J. A. Role of chitin and chitinase/chitinase-like proteins in inflammation, tissue remodeling, and injury. Annual review of physiology 73: 479–501; 2011.
Lee C. G.; Elias J. A. Role of breast regression protein-39/YKL-40 in asthma and allergic responses. Allergy Asthma Immunol Res 2: 20–27; 2010.
Mir-Kasimov M.; Sturrock A.; McManus M.; Paine 3rd R. Effect of alveolar epithelial cell plasticity on the regulation of GM-CSF expression. Am J Physiol Lung Cell Mol Physiol 302: L504–511; 2012.
Mizoguchi E. Chitinase 3-like-1 exacerbates intestinal inflammation by enhancing bacterial adhesion and invasion in colonic epithelial cells. Gastroenterology 130: 398–411; 2006.
Molfino N. A. Targeting of eosinophils in asthma. Expert opinion on biological therapy 12: 807–809; 2012.
Nakagome K.; Nagata M. Pathogenesis of airway inflammation in bronchial asthma. Auris, nasus, larynx 38: 555–563; 2011.
Ober C.; Tan Z.; Sun Y.; Possick J. D.; Pan L.; Nicolae R.; Radford S.; Parry R. R.; Heinzmann A.; Deichmann K. A.; Lester L. A.; Gern J. E.; Lemanske Jr. R. F.; Nicolae D. L.; Elias J. A.; Chupp G. L. Effect of variation in CHI3L1 on serum YKL-40 level, risk of asthma, and lung function. N Engl J Med 358: 1682–1691; 2008.
Okamoto M.; Matsuda H.; Joetham A.; Lucas J. J.; Domenico J.; Yasutomo K.; Takeda K.; Gelfand E. W. Jagged1 on dendritic cells and Notch on CD4+ T cells initiate lung allergic responsiveness by inducing IL-4 production. J Immunol 183: 2995–3003; 2009.
Petsky H. L.; Cates C. J.; Lasserson T. J.; Li A. M.; Turner C.; Kynaston J. A.; Chang A. B. A systematic review and meta-analysis: tailoring asthma treatment on eosinophilic markers (exhaled nitric oxide or sputum eosinophils). Thorax 67: 199–208; 2012.
Reese T. A.; Liang H. E.; Tager A. M.; Luster A. D.; Van Rooijen N.; Voehringer D.; Locksley R. M. Chitin induces accumulation in tissue of innate immune cells associated with allergy. Nature 447: 92–96; 2007.
Specjalski K.; Jassem E. YKL-40 protein is a marker of asthma. J Asthma 48: 767–772; 2011.
Wu H.; Suzuki T.; Carey B.; Trapnell B. C.; McCormack F. X. Keratinocyte growth factor augments pulmonary innate immunity through epithelium-driven. GM-CSF-dependent paracrine activation of alveolar macrophages. J Biol Chem 286: 14932–14940; 2011.
Zhou L.; Kawate T.; Liu X.; Kim Y. B.; Zhao Y.; Feng G.; Banerji J.; Nash H.; Whitehurst C.; Jindal S.; Siddiqui A.; Seed B.; Wolfe J. L. STAT6 phosphorylation inhibitors block eotaxin-3 secretion in bronchial epithelial cells. Bioorganic & medicinal chemistry 20: 750–758; 2012.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (no. 30971306), the project of “Six Peaks of Talents” sponsored by Jiangsu Province (2011-WS-060), and Science and Technology Program of Nantong Government (HS 2011010).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Editor: T. Okamoto
Su-qin Ben and Ya-li Qiu contributed equally to this study.
Rights and permissions
About this article
Cite this article
Ben, Sq., Qiu, Yl., Zhou, J. et al. Ovalbumin enhances YKL-40, IL-5, GM-CSF, and eotaxin expression simultaneously in primarily cultured mouse tracheal epithelial cells. In Vitro Cell.Dev.Biol.-Animal 50, 243–250 (2014). https://doi.org/10.1007/s11626-013-9698-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-013-9698-x