Abstract
Dendritic cells (DCs) are the most professional antigen-presenting cells of the mammalian immune system. They are able to phagocytize, process antigen materials, and then present them to the surface of other cells including T lymphocytes in the immune system. These capabilities make DC therapy become a novel and promising immune-therapeutic approach for cancer treatment as well as for cancer vaccination. Many trials of DC therapy to treat cancers have been performed and have shown their application value. They involve harvesting monocytes or hematopoietic stem cells from a patient and processing them in the laboratory to produce DCs and then reintroduced into a patient in order to activate the immune system. DCs were successfully produced from peripheral, umbilical cord blood-derived monocytes or hematopoietic stem cells. In this research, we produced DCs from human menstrual blood-derived monocytes. Briefly, monocytes were isolated by FACS based on FSC vs. SSC plot from lysed menstrual blood. Obtained monocytes were induced into DCs by a two-step protocol. In the first step, monocytes were incubated in RPMI medium supplemented with 2% FBS, GM-CSF, and IL-4, followed by incubation in RPMI medium supplemented with α-TNF in the second step. Our data showed that induced monocytes had typical morphology of DCs, expressed HLA-DR, HLA-ABC, CD80 and CD86 markers, exhibited uptake of dextran-FITC, stimulated allogenic T cell proliferation, and released IL-12. These results demonstrated that menstrual blood can not only be a source of stromal stem cell but also DCs, which are a potential candidate for immune therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dendritic cells (DCs) were firstly discovered by Steinman and Cohn (1973). Until now, many studies had been performed to identify the origin, phenotypes, and functions of DCs as well as their subtypes. DCs are one of antigen-presenting cells. They act as messengers between the innate and adaptive immunity.
In the body, DCs originated from hematopoietic bone marrow progenitor cells. In the differentiation process, these progenitor cells initially transform into immature dendritic cells (imDCs). These cells are characterized by high endocytic activity and low T-cell activation. They can engulf viruses and bacteria in the surrounding environment through pattern recognition receptors and toll-like receptors (TLRs) are one of them. ImDCs probably also originated from monocytes, a type of leukocytes which circulate throughout the human body. When recognizing the suitable signals, monocytes will turn into either DCs or macrophages.
In vitro DCs can be successfully generated from monocytes or CD34-positive hematopoietic stem cells (HSCs) from bone marrow, peripheral blood, and umbilical cord blood (Reid et al. 1990; 1992; Caux et al. 1992; Bender et al. 1996; Romani et al. 1996; Rosenzwajg et al. 1996; Strunk et al. 1996; Morse et al. 1997; Lutz et al. 1999; Thurner et al. 1999; Kyung et al. 2004). A widely used procedure is to induce monocytes or HSCs into imDCs by plating them in a tissue culture flask and treating with interleukin 4 (IL-4) and granulocyte-macrophage colony-stimulating factor (GM-CSF) for 1 wk. Further treatment with tumor necrosis factor alpha (α-TNF) helps imDCs differentiate into mature DCs.
DC therapy for cancer treatment is based on the use of DCs to present tumor antigens to naïve T cells. Subsequently, T cells trigger tumor-specific immune response. In this strategy, monocytes or HSCs are firstly harvested from umbilical cord blood, bone marrow, or peripheral blood from patients and induced to DCs. In a synchronous manner, tumors are isolated from patients. DCs are then primed with antigen juice. Lastly, DCs presenting tumor-specific antigens are transplanted into patients to cause immune response to attack tumors (Steinman and Dhodapkar 2001). DC therapy can be used to treat not only cancers but also persistent infection and autoimmune diseases (Nestle et al. 1998; Lodge et al. 2000; Byrne and Halliday 2002; Jin-Kun et al. 2002; Akbar et al. 2004; Onji 2004; Ding et al. 2010).
As applications using DCs are increasing significantly, sufficient DC production becomes more imperative. DC sources from umbilical cord blood and bone marrow provide many advantages but also inevitable drawback. For instance, only few people had their own umbilical cord preserved or patients in many reported cases with severe bone marrow suppression could not provide enough immune cells for transplantation. In this study, we investigated production of DCs from menstrual blood, a novel cell source for DC therapy.
Menstrual blood is a highly renewable source. Every month, endometrium can be thickened 5–7 mm and provide 40–60 ml of blood (McLennan and Rydell 1965). Menstrual blood is recognized as an abundant source of cells that can notably differentiate into several lineages. There are several reports indicating that endometrium contains a cell population which have replicating ability and pluripotent differentiation potential similar to bone marrow-derived stem cells (Schwab et al. 2005; Du and Taylor 2007; Gargett 2007; Schwab and Gargett 2007; Wolff et al. 2007). We realize that menstrual blood also includes hematopoietic stem cells and is a plentiful supply of monocytes which are precious material to produce DCs for DC therapy.
Material and Methods
Menstrual blood collection
Menstrual blood was obtained from healthy women. All donors must have signed an agreement with our laboratory prior to donation. To collect menstrual blood, a female volunteer inserted provided menstrual cup in place of a tampon. This cup could be retained for 2–3 h to collect next samples since every woman normally gave two to three times of the menstrual fluid. Blood fluid then was cautiously transferred into 15-ml Falcon tube containing 2 ml of PBS supplemented five times antibiotic/mycotic solution (Sigma-Aldrich, St Louis, MO.). This tube was kept on ice and quickly moved to the laboratory. This sample was tested for bacterial and fungal contamination. Only the samples negative with both bacteria and fungi were further processed.
Isolation of monocytes and CD4+ T cells
Blood which passed all contamination and quality tests was lysed with PharmLyse solution (BD BioSciences, San Jose, NJ) to eliminate erythrocytes. Mixtures of remaining cells were fractionated by carefully layering suspension over Ficoll-Paque and centrifuging at 1,800 rpm for 10 min. Afterwards, mononuclear cell segment in the interphase of tube was obtained. This segment was analyzed with a FACSCalibur using CellQuest Pro software to locate monocyte population based on FSC versus side scatter (SSC) diagram. For isolation of CD4+ T cells, mononuclear cell segments were stained with anti-CD4-fluorescein isothiocyanate (FITC) antibody (Santa Cruz Biotechnology, Santa Cruz, CA) and analyzed through flow cytometer. CD4+ T cells were considered as a sub-population expressing FITC fluorescent signal on SSC versus FL1 diagram. Monocytes and CD4+ T cell population were isolated by catcher tube based cell sorter in FACSCalibur cytometer (BD Bioscience). Sorted populations were re-evaluated for their purification level. Only the samples with a purity of >95% were used for further research.
Cell culture and differentiation
Monocytes were differentiated into dendritic cells by a two-step protocol. In the first step, monocytes (5 × 105cells/ml) were cultured in the RPMI 1640 medium (Sigma-Aldrich) supplemented with 10% heat-inactivated FBS, l-glutamine, HEPES, 50 mM 2-ME, 100 U/ml penicillin and 100 μg/ml streptomycin (Sigma-Aldrich), 20 ng/ml IL-4, 10 ng/ml GM-CSF (Santa Cruz Biotechnology) in 5–6 d to produce imDCs. Culture medium was changed every 3 d until the end of experiment. In the second step, TNF-α (50 ng/ml; Santa Cruz Biotechnology) was added to the culture medium at day 5 and cells were incubated for further 24 h.
Immune phenotype analysis of DCs by flow cytometry
Induced cells were washed two times with PBS supplemented with 1% BSA (Sigma-Aldrich). The Fc receptor on the cell surface was blocked using IgG (Santa Cruz Biotechnology) on ice for 15 min. Cells were stained for 30 min at 4°C with the following antibodies conjugated with FITC: anti-HLA-DR, anti-HLA-DQ, anti-CD40, anti-CD80, and anti-CD86 (BDBiosciences Pharmingen, San Diego, CA). After washing, cells were analyzed with FACSCalibur flow cytometer (BD Bioscience). To determine the efficiency of differentiation of monocytes, we evaluated the percentage of cells positive with CD80 and CD86 markers. The percentage of cells that were positive with both markers was considered as differentiating efficiency. This evaluation criterion was based on properties of mature dendritic cells which would express both markers. The experiment was repeated five times. The average value was defined as the efficiency of this process. To assess the co-expression of two markers, we used the anti-CD80 and anti-CD86 antibodies conjugated with different dyes (CD80-PE and CD86-PerCP) to make dual-platform analysis.
Dextran-FITC uptake assay
To measure the phagocytic capacity of DCs, 5 × 104 cells were incubated with Dextran-FITC (0.1 mg/ml; Sigma-Aldrich) in 100 μl of culture medium at 37°C and 0°C which served as negative control for 4 h. Cells were washed with cold PBS supplemented with 1% BSA four times before flow cytometry analysis. Phagocytosis ability of DCs was assessed by the appearance of cell populations expressing FITC fluorescent signal.
Stimulation of CD4+ T lymphocyte proliferation
The assessment was performed in the different groups with the ratio of DC/lymphocytes as follows: 0.25:100, 0.5:100, 1:100, 2:100, and 8:100. Control groups are DC + PHA (phytohemagglutinin, Sigma-Aldrich, St Louis, MO), PHA, and PHA + lymphocytes. PHA concentration is 50 mg/L. The experiment was conducted on 96 wells (Nunc, Roskilde, Denmark) and repeated four times.
MTT assay to measure the ability of lymphocyte proliferation
Twenty microliters of MTT (5 g/L; Sigma-Aldrich) was added into each well of 96-well plates, followed by incubation for 4 h, and addition of 150 μl of DMSO (Sigma-Aldrich). Plates were then mixed well for 10 min until the crystals dissolved completely. Absorption values (A-value) for each well was measured at a wavelength of 490 nm using micro-plate reader DTX 880 (Beckman Coulter, GmbH, Krefeld, Germany). An offset value of A and absorption value of control group (DC + PHA) would reflect lymphocyte proliferation. An offset value of absorption in lymphocyte + PHA and PHA group showed proliferation of lymphocytes in the control group. All results were analyzed by Staraphic 7.0 software.
Quantity of production of cytokines/chemokines
To detect the secretion of cytokines, monocytes after induction with GM-CSF and IL-4 were further induced with TNF-α (in the second step) as described above in culture medium in 24-well plates for 24 h. Supernatant was collected and frozen at −80°C until analysis. The quantity of cytokine IL-12 in the supernatant was determined by ELISA kit (BD Bioscience) and read on a DTX 880 (Beckman Coulter, CA).
Results
Induced cells expressed phenotypic characteristics of DCs.
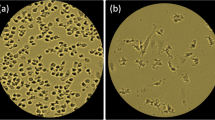
Through observing cultured cells, we noticed that monocytes formed small groups similar with the culture of monocytes from human bone marrow or umbilical cord blood (Inaba et al. 1992a, b; Romani et al. 1994; Sallusto and Lanzavecchia 1994). These small groups adhered weakly to flask surface at day 2 and became compact at day 5. Most of the cells had expanding cytoplasm and small dendrite-like structure (Fig. 1c, d ).
Morphologically, the differentiated cells shared some characteristics of DCs. These cells had relatively uniform shape with large heterogeneity of nuclei, many mitochondria and vacuoles, and relatively few particles in the cytoplasm. Cell shape is comparable to DCs produced from umbilical cord blood or bone marrow but very different from the mononuclear cells (Fig. 1). Likewise, the results to show surface marker expression from flow cytometry displayed that immune phenotype of induced cells and DC isolated from fresh umbilical cord blood are the same. These cells expressed HLA-DQ, HLA-DR, CD86, and CD80. The percentage of positive cells that expressed both CD80 and CD86 was 68.92 ± 2.59% (n = 5; Fig. 2).
Differentiated DCs from monocytes were in vitro functional
Antigen phagocytosis. For functional analysis, we measured in vitro the phagocytosis ability of DCs. Phagocytosis activity was assessed by measuring the ability of cells that can consume dextran-FITC. Our data showed that monocytes after induction increased their phagocytosis ability from 6.1 ± 2.5% to 48.3 ± 14.9% (p = 0.05). Meanwhile, it was only 5.1 ± 1.3% (n = 3) in the group where cells were cultured in the medium without GM-CSF, IL-4, and TNF-α. In addition, cells cultured at 0°C could not engulf dextran-FITC (Figs. 3 and 4).
Induced monocytes stimulated T lymphocytes
The expression of CD80 and CD86 on the surface of the DCs associated with the activity of activated T lymphocytes. Results showed that induced DCs from monocytes with cytokines GM-CSF, IL-4, and TNF-α triggered T cell proliferation. Figure 5 proved that the activity of DCs had statistically significant difference compared to control group (p < 0.05) and augmented when DC concentration increased (p < 0.05).
A-values (Fig. 5) are offset of OD (Optical Density) values measured in the control samples (lymphocyte + PHA) and experimental groups. Because PHA is the strongest stimulant of lymphocytes, OD value of control sample is the greatest. Therefore, A-value is smaller if the growth capacity of experimental cells is higher. In a similar manner, A-value is larger if the ability to stimulate by DC is lower. Through experimental results, we found that DCs differentiated from monocytes of menstrual blood had the ability to stimulate lymphocyte cells in vitro. This ability depended on the ratio of mixing between DCs and lymphocyte cells. The more DCs were added, the more lymphocytes were stimulated.
Activity of stimulating lymphocyte proliferation is a critical characteristic of DCs in vivo. This feature helps to enhance immunity in cancer treatment, thus is a key point for success of application. This activity of DCs was also demonstrated in the DC derived from umbilical cord blood CD34-positive cells (Miralles et al. 1998), human monocytes from the bone marrow (Reid et al. 1992; Mayordomo et al. 1995; Marta et al. 1999; Carine and Shevach 2005). The activity of DCs in this study is consistent if compared with those differentiated from umbilical cord blood CD34-positive cells (Ferlazzo et al. 2000; de Vries et al. 2002; Kyung et al. 2004).
Induced monocytes produced IL-12
To determine the mechanism of activated T cell proliferation, this study evaluated secretion of interleukin after inducing. IL-12 is the most important interleukin in the activation of T lymphocytes. In fact, DC cells always interact with other cells in the body. This interaction can be direct by cell–cell communication based on the interaction of surface proteins as described above through B7 (CD80 or CD86) with CD28 on lymphocytes or occurs in a greater distance through cytokines. Typically, DC cells after induction with antigens would produce IL-12 (Reis e Sousa et al. 1997). IL-12 is a signal to induce CD4+ T cells into Th1 phenotype. Then, it activates the immune system to attack antigens that were presented by DCs. IL-12 quantity analyzed by ELISA (Fig. 6) showed that there was a statistically significant difference (p < 0.5) between monocytes with and without cytokine treatment.
Discussion
DCs are the most professional antigen-presenting cells in our body. Unlike macrophages, they have capability to present antigens not only to T cells but also to B and natural killer (NK) cells. Within our biological system, DCs can be differentiated by hematopoietic stem cells. These stem cells are firstly induced into immature DCs (imDCs). When there is any stimulation by risk factors through TLRs, imDCs will phagocytose small portions of membrane of those inducers through a process called nibbling. Subsequently, small fragments are processed and sent to present at their cell surface using major histocompatibility complex (MHC) molecules. At this step, DC maturation is completed.
In the mature stage, DCs express CD80 (B7.1), CD86 (B7.2), and CD40. These are essential co-receptors to stimulate T cell activity. By the expression of mentioned co-receptors, DCs have the power to provoke memory T and naïve T cells as well as other forms of T cells. Hence, appearance of these surface proteins is prerequisite for DCs to perform their functions in activating other immune cells. Numerous studies which created DCs from monocytes or hematopoietic stem cells from umbilical cord blood, bone marrow, or peripheral blood succeeded in enhancing the expressivity of these markers (Romani et al. 1996; Reddy et al. 1997; Reis e Sousa et al. 1997; Ferlazzo et al. 2000; Zheng et al. 2000; Goriely et al. 2001; Liu et al. 2002). In this current report, we proved that our DCs also expressed similar proteins with CD80 and CD86 as examples. This is the evidence to conclude that induced cells have the capacity to excite other cells in the immune system, especially naïve T and memory T cells.
The point can be proved by our results of investigation in the ability of DCs to activate T cell. Obviously, in the experiment to stimulate CD4+ T cells by induced monocytes, we could see remarkable T cell proliferation when DCs were co-cultured with CD4+ T cells extracted from blood samples. Furthermore, T cell increase was dosage-dependent when same amount of T cells was mixed with variable numbers of DCs. This trend was led by direct interaction between DCs and CD4+ T cells through CD80 and CD86 co-receptors.
However, it is known that stimulation of DCs on T cells is not only through direct interaction but also in a far distance by cytokine signal which is released by DCs. In our body, IL-12, one of important interleukins, is produced either by DCs or by macrophages and B cells. IL-12 initiates differentiation of naïve T into Th0 and then into Th1 and Th2 cells. IL-12 also plays a pivotal role in activities of NK and T cells. It intensifies toxicity by NK cells and CD8+ T cells. Fortunately, DCs from menstrual blood can do a good job in releasing IL-12. Data from this study indicated that induced DCs with a suitable cocktail of cytokines had a significant elevation in IL-12 secretion. This evidence again supports our conclusion about authenticity of DCs from menstrual blood.
Not only did induced DCs from menstrual blood have DC-like shape and ability to activate T cells, they also had the capacity of phagocytosis and antigen presentation, which are indispensable for DCs to perform their functions in immune therapy. In this report, we showed feasible phagocytosis by DCs through dextran uptake assay. After 120 min of incubation with dextran, 47.78% of DCs have taken dextran and expressed strong fluorescent signal. Additionally, we observed that cells after induction expressed MHC II (HLA-DR and HLA-ABC). This is a critical protein complex which serves as co-receptors and antigen-presenting region. The expression of HLA-DR and HLA-ABC along with phagocytosis ability after induction indicated that DCs from menstrual blood can phagocytize, process, and present antigens at the cell surface with MHC II proteins.
Hence, we created functional DCs with all typical characteristics of normal DCs. Those are DC-like shape, ability to phagocytize, process, and present antigens to stimulate other cells in immune system, especially T cells through direct cell–cell interaction or IL-12 secretion in far distance.
Due to masterful capability in antigen presentation, DCs were widely used to treat cancer diseases. Clinical trials utilizing DCs to initiate a specific immune reaction have been conducted to treat lung, skin, prostate, and kidney cancers. Nowadays, common DC sources can be achieved from bone marrow, peripheral blood, and recently, from umbilical cord blood. Though production of DCs from those origins is relatively simple, some disadvantages need to be considered. Noticeably, limitedness of monocytes or HSCs obtained by those methods can greatly reduce efficiency of application. Large-scale production of DCs from those sources for repeated transplantation which is required for older or weak patients grouped in late stage or end-stage diseases will be a real hindrance. Moreover, umbilical cord blood preservation is still not commonplace within contemporary society. From this point of view, we expect that menstrual blood can be a potential substitute for DC source. In the current study, we realized that cell population which was positive for both CD80 and CD86 reached 68.92 ± 2.59% after induction. Generally, every month, a woman can give 40–60 ml of menstrual blood, which was previously considered as a sanitary waste. This amount of blood is approximately similar to the volume we can get from one aspiration of umbilical cord blood or bone marrow. As a result, enormous amounts of DCs are produced since 450–720 ml of menstrual blood can be gained each yr.
Nevertheless, efficacy to produce DCs (68%) from this research is still relatively low indeed. Thus, further studies need to be performed to optimize differentiation efficiency. The ultimate aim is to demonstrate antigen presentation and T cell stimulation as well as therapeutic effects in vivo and in clinical application by induced DCs from menstrual blood.
Therefore, the results from this study showed that menstrual blood is a new and useful source of DCs for research and application.
Conclusion
To conclude, we have successfully created DCs from menstrual blood-derived monocytes in this study. These cells exhibited the basic characteristics of functional DCs such as phagocytosis of antigen, processing antigen and presenting them in MHC II (HLA-DR and HLA-DQ), and stimulating autogenic T lymphocytes through CD80 and CD86 proteins and IL-12. These results will be a premise for the next evaluation as well as their applications in trials.
References
Akbar S. M.; Furukawa S.; Hasebe A.; Horiike N.; Michitaka K.; Onji M. Production and efficacy of a dendritic cell-based therapeutic vaccine for murine chronic hepatitis B virus carrierer. Int J Mol Med 2: 295–9; 2004.
Bender A.; Sapp M.; Schuler G.; Steinman R. M.; Bhardwaj N. Improved methods for the generation of dendritic cells from nonproliferating progenitors in human blood. J Immunol Methods 196: 121–135; 1996.
Byrne S. N.; Halliday G. M. Dendritic cells: making progress with tumour regression? Immunol Cell Biol 6: 520–30; 2002.
Carine Brinster; Shevach E. M. Bone Marrow-Derived Dendritic Cells Reverse the Anergic State of CD4+CD25+ T Cells without Reversing Their Suppressive Function. Journal of Immunology 175: 7332–7340; 2005.
Caux C.; Dezutter-Dambuyant C.; Schmitt D.; Banchereau J. GM-CSF and TNF-alpha cooperate in the generation of dendritic Langerhans cells. Nature 360: 258–261; 1992.
de Vries I. J.; Eggert A. A.; Scharenborg N. M.; Vissers J. L.; Lesterhuis W. J.; Boerman O. C.; Punt C. J.; Adema G. J.; Figdor C. G. Phenotypical and functional characterization of clinical grade dendritic cells. J Immunother 25: 429–439; 2002.
Ding F. X.; Xian X.; Guo Y. J.; Liu Y.; Wang Y.; Yang F.; Wang Y. Z.; Song S. X.; Wang F.; Sun S. H. A preliminary study on the activation and antigen presentation of hepatitis B virus core protein virus-like particle-pulsed bone marrow-derived dendritic cells. Mol Biosyst.; 2010. doi:10.1039/C005222A.
Du H.; Taylor H. S. Contribution of bone marrow-derived stem cells to endometrium and endometriosis. Stem Cells 25: 2082–6; 2007.
Ferlazzo G.; Klein J.; Paliard X.; Wei W. Z.; Galy A. Dendritic cells generated from CD34+ progenitor cells with flt3 ligand, c-kit ligand, GM-CSF, IL-4, and TNF-alpha are functional antigen-presenting cells resembling mature monocyte-derived dendritic cells. J Immunother 1: 48–58; 2000.
Gargett C. E. Uterine stem cells: What is the evidence? Hum Reprod Update 13: 87–101; 2007.
Goriely S.; Vincart B.; Stordeur P.; Vekemans J.; Willems F.; Goldman M.; De Wit D. Deficient IL-12(p35) gene expression by dendritic cells derived from neonatal monocytes. J Immunol 166: 2141; 2001.
Inaba K.; Inaba M.; Romani N.; Aya H.; Degichi M.; Ikehara S.; Muramatsu S.; Steinman R. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med 176: 1693–1702; 1992a.
Inaba K.; Steinman R. M.; Pack M. W.; Aya H.; Inaba M.; Sudo T.; Wolpe S.; Schuler G. Identification of proliferating dendritic cell precursors in mouse blood. J Exp Med 175: 1157–1167; 1992b.
Jin-Kun Zhang; Jun Li; Hai-Bin Chen; Jin-Lun Sun; Yao-Juan Qu; Juan-Juan Lu. Antitumor activities of human dendritic cells derived from peripheral and cord blood. World J Gastroenterol 1: 87–90; 2002.
Kyung Ha Ryu; Su Jin Cho; Yoon Jae Jung; Ju Young Seoh; Jeong Hae Kie; Sang Hyeok Koh; Hyoung Jin Kang; Hyo Seop Ahn; Hee Young Shin. In Vitro Generation of Functional Dendritic Cells from Human Umbilical Cord Blood CD34+ Cells by a 2-Step Culture Method. International Journal of Hematology 80: 281–286; 2004.
Liu A.; Takahashi M.; Narita M.; Zheng Z.; Kanazawa N.; Abe T.; Nikkuni K.; Furukawa T.; Toba K.; Fuse I.; Aizawa Y. Generation of functional and mature dendritic cells from cord and bone marrow CD34+ cells by two-step culture combined calcium ionophore treatment. J Immunol Methods 261: 49–63; 2002.
Lodge P. A.; Jones L. A.; Bader R. A.; Murphy G. P.; Salgaller M. L. Dendritic cell-based immunotherapy of prostate cancer:immune monitoring of a phase II clinical trial. Cancer Res 60: 829–833; 2000.
Lutz M. B.; Kukutsch N.; Ogilvie A. L.; Rossner S.; Koch F.; Romani N.; Schuler G. An advanced culture method for generating large quantities of highly pure dendritic cells from mouse bone marrow. J Immunol Methods 223: 77–92; 1999.
Marta S. L.; Roters B.; Pers B.; Mehling A.; Luger T. A.; Schwarz T.; Grabbe S. Maturation Stage Correlates with Dendritic Cell Bone Marrow-Derived Dendritic Cells. J Immunol 162: 168–175; 1999.
Mayordomo J. I.; Zorina T.; Storkus W. J.; Zitvogel L.; Celluzzi C.; Falo L. D.; Melief C. J.; Ildstad S. T.; Martin Kast W.; Deleo A. B.; Lotze M. T. Bone marrow-derived dendritic cells pulsed with synthetic tumour peptides elicit protective and therapeutic antitumour immunity. Nature Medicine 1: 1297–1302; 1995.
McLennan C. E.; Rydell A. H. Extent of endometrial shedding during normal menstruation. Obstet Gynecol 26: 605–21; 1965.
Miralles G. D.; Smith C. A.; Whichard L. P.; Morse M. A.; Haynes B. F.; Patel D. D. CD34 + CD38-lin- cord blood cells develop into dendritic cells in human thymic stromal monolayers and thymic nodules. J Immunol 7: 3290–8; 1998.
Morse M. A.; Zhou L. J.; Tedder T. F.; Lyerly H. K.; Smith C. Generation of dendritic cells in vitro from peripheral blood mononuclear cells with granulocyte-macrophage-colony-stimulating factor, interleukin-4, and tumor necrosis factor-alpha for use in cancer immunotherapy. Ann Surg 1: 6–16; 1997.
Nestle F. O.; Alijagic S.; Gilliet M.; Sun Y.; Grabbe S.; Dummer R.; Burg G.; Schadendorf D. Vaccination of melanoma patients with peptide- or tumor lysate-pulsed dendritic cells. Nat Med 4: 328–332; 1998.
Onji. Role of dendritic cells in the immunopathogenesis and therapy of liver diseases. Nihon Rinsho Meneki Gakkai Kaishi 2: 64–76; 2004.
Reddy A.; Sapp M.; Feldman M.; Subklewe M.; Bhardwaj N. A monocyte conditioned medium is more effective than defined cytokines in mediating the terminal maturation of human dendritic cells. Blood 90: 3640–3646; 1997.
Reid C. D. L.; Fryer P. R.; Clifford C.; Kirk A.; Tikerpae J.; Knight S. C. Identification of hematopoietic progenitors of macrophages and dendritic Langerhans cells (DL-CFU) in human bone marrow and peripheral blood. Blood 76: 1139–1149; 1990.
Reid C. D. L.; Stackpole A.; Meager A.; Tikerpae J. Interactions of tumor necrosis factor with granulocyte-macrophage colony-stimulating factor and other cytokines in the regulation of dendritic cell growth in vitro from early bipotent CD34+ progenitors in human bone marrow. J Immunol 154: 2681–2688; 1992.
Reis e Sousa C.; Hieny S.; Scharton-Kersten T.; Jankovic D. In vivo microbial stimulation induces rapid CD40 ligand-independent production of interleukin 12 by dendritic cells and their redistribution to T cell areas. J Exp Med 11: 1819–29; 1997.
Romani N.; Gruner S.; Brang D.; Kampgen E.; Lenz A.; Trockenbacher B.; Konwalinka G.; Fritsch P. O.; Steinman R. M.; Schuler G. Proliferating dendritic cell progenitors in human blood. J Exp Med 180: 83–93; 1994.
Romani N.; Reider D.; Heuer M.; Ebner S.; Kampgen E.; Eibl B.; Niederwieser D.; Schuler G. Generation of mature dendritic cells from human blood - an improved method with special regard to clinical applicability. J Immunol Methods 196: 137–151; 1996.
Rosenzwajg M.; Canque B.; Gluckman C. Human dendritic cell differentiation pathway from CD34+ hematopoietic precursor cells. Blood 87: 535–544; 1996.
Sallusto F.; Lanzavecchia A. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte-macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor. J Exp Med 179: 1109–1118; 1994.
Schwab K. E.; Chan R. W.; Gargett C. E. Putative stem cell activity of human endometrial epithelial and stromal cells during the menstrual cycle. Fertil Steril 84: 1124–30; 2005.
Schwab K. E.; Gargett C. E. Co-expression of two perivascular cell markers isolates mesenchymal stem-like cells from human endometrium. Hum Reprod 22: 2903–11; 2007.
Steinman R. M.; Cohn Z. A. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J Exp Med 5: 1142–62; 1973.
Steinman R. M.; Dhodapkar M. Active immunization against cancer with dendritic cells: the near future. Int J Cancer 4: 459–73; 2001.
Strunk D.; Rappersberger K.; Egger C. Generation of human dendritic cells/Langerhans cells from circulating CD34+ hematopoietic progenitor cells. Blood 87: 1292–1302; 1996.
Thurner B.; Roder C.; Dieckmann D.; Heuer M.; Kruse M.; Glaser A.; Keikavoussi P.; Kampgen E.; Bender A.; Schuler G. Generation of large numbers of fully mature and stable dendritic cells from leukapheresis products for clinical application. J Immunol Methods 223: 1–15; 1999.
Wolff E. F.; Wolff A. B.; Hongling Du; Taylor H. S. Demonstration of multipotent stem cells in the adult human endometrium by in vitro chondrogenesis. Reprod Sci 14: 524–33; 2007.
Zheng Z.; Takahashi M.; Narita M.; Toba K.; Liu A.; Furukawa T.; Koike T.; Aizawa Y. Generation of dendritic cells from adherent cells of cord blood by culture with granulocyte-macrophage colony-stimulating factor, interleukin-4, and tumor necrosis factor-alpha. J Hematother Stem Cell Res 9: 453–464; 2000.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor: Tetsuji Okamoto
Rights and permissions
About this article
Cite this article
Phuc, P.V., Lam, D.H., Ngoc, V.B. et al. Production of functional dendritic cells from menstrual blood—a new dendritic cell source for immune therapy. In Vitro Cell.Dev.Biol.-Animal 47, 368–375 (2011). https://doi.org/10.1007/s11626-011-9399-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-011-9399-2