Abstract
Platelet-rich plasma (PRP) is an emerging therapeutic application because PRP contains various growth factors that have beneficial effects on tissue regeneration and engineering. Mesenchymal stem cells and PRP derived from peripheral blood have been well studied. In this study, we investigated the effects of PRP derived from human umbilical cord blood (UCB-PRP) on proliferation, alkaline phosphatase (ALP) activity, and osteogenic differentiation of stem cells from human exfoliated deciduous teeth (SHEDs), dental pulp stem cells (DPSCs), and periodontal ligament stem cells (PDLSCs). Three types of dental stem cells were primarily isolated and characterized by flow cytometric analysis. Dental stem cells were exposed to various concentrations of UCB-PRP, which resulted in the proliferation of dental stem cells. Treatment with 2% UCB-PRP resulted in the highest level of proliferation. The ALP activity of DPSCs and PDLSCs increased following treatment with UCB-PRP in a dose-dependent manner up to a concentration of 2%. ALP activity decreased with higher concentration of UCB-PRP. The effects of UCB-PRP on calcium deposition were similar to those on proliferation and ALP activity. Treatment with 2% UCB-PRP resulted in the highest calcium depositions in DPSCs and PDLSCs; however, treatment with 1% UCB-PRP resulted in the highest calcium deposition in SHEDs. The concentrations of platelet-derived growth factor-AB and transforming growth factor-β1 in UCB-PRP were investigated and found to be comparable to the amounts in peripheral blood. Overall, UCB-PRP had beneficial effects on the proliferation and osteogenic differentiation of dental stem cells. Determination of the optimal concentration of UCB-PRP requires further investigation for clinical applications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Human umbilical cord blood (UCB) is a source of hematopoietic stem cells and progenitor cells. The frequency of hematopoietic stem cells and progenitor cells in UCB is greater than the frequency in bone marrow and peripheral blood (Broxmeyer 2005). Recently, it was shown that UCB contains various types of stem cells such as mesenchymal stem cells (MSCs) (Erices et al. 2000), multipotent adult progenitor cells (Kogler et al. 2004; Lee et al. 2004), unrestricted somatic stem cells (Kogler et al. 2004), and endothelial progenitor cells (Ingram et al. 2004). The lymphocytes in UCB are functionally immature (Dimitriou et al. 1998; Paloczi 1999) and UCB-derived progenitor cells can be maintained in long-term culture for more than 16 wk, suggesting the presence of very primitive hematopoietic cells (Dimitriou et al. 1998). In addition, use of human UCB as a stem cell source has several advantages over other cell sources, for example, human UCB is abundant and can be obtained with non-invasive methods that raise none of the ethical issues related to other human adult stem cell sources (Gluckman 2009).
Platelet-rich plasma (PRP) contains a high concentration of human platelet growth factors in a small volume of plasma. The growth factors are obtained by lysing platelet bodies through temperature-shock or activating platelets to release growth factors. PRP contains platelet-derived growth factor (PDGF), basic fibroblast growth factor, vascular endothelial growth factor, insulin-like growth factor-1, and transforming growth factor-β (TGF-β) (Okuda et al. 2003; Doucet et al. 2005). These growth factors are involved in wound healing and the repair of mineralized tissue. Emerging literature demonstrates the beneficial effects of PRP in chronic non-healing tendon injuries including lateral epicondylitis, plantar fasciitis, and cartilage degeneration. The increasing need for clinical use of PRP necessitates more controlled studies and further understanding of PRP (Sampson et al. 2008). Substantial heterogeneity exists in the studies with regard to patient populations, study designs, PRP preparation techniques, outcome measures, and observation periods (Plachokova et al. 2008).
The effects of PRP on the proliferation and differentiation of MSCs derived from bone marrow (Doucet et al. 2005) have been well studied. However, in dental research, periodontal ligament cells are the most common source used in studies of the effects of PRP on proliferation and differentiation in vitro (Plachokova et al. 2008). In order to enhance wound healing in the dental clinic, PRP was used to provide growth factors in high concentrations to surgical wounds obtained from bone grafting, periodontal defects, sinus augmentation, oral-maxillofacial reconstructions, and bone formation in extraction sockets (Nikolidakis and Jansen 2008).
Recently, banking of cord blood as a hematopoietic stem cell source has become widely accepted and commercially feasible. During the process of banking cord blood, mononuclear cells are stored and red blood cells and plasma are usually discarded. Therefore, the plasma in cord blood can be another source of PRP. The effects of PRP on dental stem cells derived from dental pulp have not been well studied. Moreover, the use of UCB-derived PRP (UCB-PRP) was elusive. In this study, we investigated the effects of human UCB-PRP on the proliferation and osteogenic differentiation of human dental stem cells, which are stem cells from human exfoliated deciduous teeth (SHEDs), dental pulp stem cells (DPSCs), and periodontal ligament stem cells (PDLSCs). Various concentrations of UCB-PRP were examined and found to induce the proliferation and osteogenic differentiation of these dental stem cells. Our data show that treatment with 2% UCB-PRP induces high levels of proliferation and osteogenic differentiation in SHEDs, DPSCs, and PDLSCs. UCB-PRP contained similar levels of growth factors compared to peripheral blood-derived PRPs.
Materials and Methods
Platelet-rich plasma preparation.
Approval for the use of human UCB was obtained from the School of Dentistry, Seoul National University Institutional Review Board (approval number S-D20080007). Before and after PRP preparation, the platelet count in whole blood and PRP was assessed. For the preparation of PRP, 50–100 mL of human UCB was centrifuged at 150×g for 15 min at room temperature. Harvested PRP was stored at −80°C until use. Frozen PRP was rapidly thawed at 37°C and centrifuged at 900×g for 30 min at 4°C to remove platelet bodies.
Measurement of TGF-β and PDGF levels in PRP.
To quantitate the amount of PDGF-AB and TGF-β1 in UCB-PRP, Quantikine enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems, Minneapolis, MN) were used according to the manufacturer’s instructions. All sample measurements were performed in duplicate. The minimal detection limits of these assay kits reported by the manufacturer are 1.7 pg/mL for PDGF-AB and 7 pg/mL for TGF-β1.
Cell culture.
Deciduous teeth and adult molars were delivered in Hank’s balanced salt solution (Welgene, Dae-gu, Korea) supplemented with 3% antibiotics/antimycotics (Gibco, Grand Island, NY) at 4°C. Adult dental pulps were extracted after the crown of the tooth was removed using a dental high-speed unit. Deciduous dental pulps were gently extracted with tweezers, and periodontal ligaments were gently separated from the surface of the root. Dental pulps and periodontal ligaments were minced in 1 mg/mL of collagenase type I and 2.4 mg/mL of dispase (Gibco) at 37°C for 1 h. Single-cell suspensions were plated and maintained in minimum essential medium alpha (α-MEM; Hyclone, Road Logan, UT) supplemented with 15% fetal bovine serum (FBS; Hyclone), 2 mM l-glutamine, 100 μM ascorbic acid 2-phosphate (Sigma–Aldrich, St. Louis, MO), and 1% antibiotics/antimycotics. The medium was changed every 3 d, and the cells were sub-cultured at 70% confluency. At each passage, cells were counted and photographed using an inverted microscope (Nikon Eclipse TS 100; Nikon, Tokyo, Japan).
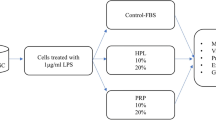
To determine the effects of UCB-PRP on the proliferation of SHEDs, DPSCs, and PDLSCs, cells were plated at 1 × 104 cells per well in a 24-well plate. Beginning the next day, cells were maintained in α-MEM supplemented with 5% FBS with 0%, 2%, 5%, or 10% PRP for 3 d. Each day, cells were counted using a hemocytometer.
Flow cytometry.
Cells were detached and washed with PBS supplemented with 2% FBS. The following antibodies were used: FITC-conjugated mouse anti-human CD14, CD31, CD44, and CD45; phycoerythrin (PE)-conjugated mouse anti-human CD29, CD73, and CD117; PE/Cy5-conjugated mouse anti-human CD90; allophycocyanin (APC)-conjugated mouse anti-human CD34; HLA-DR (all from BD PharMingen, San Jose, CA); APC-conjugated mouse anti-human CD105 (eBioscience, San Diego, CA); and biotin-conjugated mouse anti-human HLA class I (BD PharMingen). From 1 × 105 to 5 × 105 cells were incubated with primary antibodies for 30 min on ice. After washing, secondary antibody was applied for 30 min on ice. After washing, cells were fixed with 4% paraformaldehyde at 4°C before analysis. Fluorescence intensity was measured on a FACSCalibur (BD PharMingen), and data were analyzed using FLOWJO software (Tree Star Inc., Ashland, OR).
Alkaline phosphatase activity.
Cells were plated at 1 × 104 cells per well in a 24-well plate. Beginning the next day, cells were maintained in 5% FBS, 50 μg/mL ascorbic acid (Sigma–Aldrich), 1 μM dexamethasone (Sigma–Aldrich), 10 mM β-glycerophosphate (Sigma–Aldrich), and 0%, 1%, 2%, or 5% UCB-PRP for 3 d. Alkaline phosphatase (ALP) activity was assayed with a QuantiChrom™ Alkaline Phosphatase Assay Kit (DALP-250; BioAssay System, CA) according to the manufacturer’s protocol. ALP activities were normalized based on protein concentrations, which were determined using the BCA protein assay kit (Pierce, Rockford, IL).
In vitro osteogenic differentiation and Alizarin Red staining.
For osteogenic differentiation, cells were cultured until they reached confluency and then maintained in α-MEM supplemented with 5% FBS, 10 mM β-glycerophosphate, 50 μg/mL l-ascorbic acid 2-phosphate, 1 μM dexamethasone, and 0%, 1%, 2%, or 5% UCB-PRP for 21 d. Medium was changed every 3 d. To visualize calcium deposits for the detection of mineralization, cells were fixed with 4% paraformaldehyde and stained with 2% Alizarin Red (Sigma–Aldrich).
In order to quantitatively determine the amount of calcium minerals, Alizarin Red was de-stained with 10% cetylpyridinium chloride (Sigma–Aldrich) in 10 mM sodium phosphate for 30 min at room temperature. The concentration of calcium minerals was determined by measuring absorbance at 570 nm on a multi-plate reader (Bio-Rad, Hercules, CA).
Results
Morphology and immunophenotypes of SHEDs, DPSCs, and PDLSCs.
SHEDs, DPSCs, and PDLSCs that were primarily isolated grew very well and showed typical fibroblast-like morphology. The cells became almost confluent at 5 to 7 d and were then sub-cultured. SHEDs, DPSCs, and PDLSCs had slightly different morphologies from each other, for example, DPSCs and PDLSCs were more elongated and bipolar, whereas SHEDs were slightly polygonal (Fig. 1A, C, E ). Their morphologies were maintained through sub-culturing. To characterize SHEDs, DPSCs, and PDLSCs, the expression status of surface markers was examined using FACS. The results showed that SHEDs, DPSCs, and PDLSCs were all positive for MSC markers such as CD29, CD44, CD73, CD90, CD105, and HLA-I; however, they did not express hematopoietic lineage markers such as CD14, CD34, CD45, CD117, and HLA-DR, or the endothelial marker, CD31 (Fig. 1B, D, F ). In addition, SHEDs, DPSCs, and PDLSCs were differentiated in osteogenic and adipogenic induction conditions (data not shown). Analysis of the differentiated cells indicated that SHEDs, DPSCs, and PDLSCs have MSC characteristics.
Morphology and flow cytometry of SHEDs, DPSCs, and PDLSCs. SHEDs, DPSCs, and PDLSCs were photographed and characterized at passage 3. DPSCs (C) and PDLSCs (E) showed bipolar fibroblast-like morphology, but SHEDs (A) were slightly polygonal. FACS analysis showed that SHEDs (B), DPSCs (D), and PDLSCs (F) were positive for mesenchymal markers (CD29, CD44, CD73, CD90, and CD105) and negative for an endothelial marker (CD31) and hematopoietic markers (CD14, CD34, CD45, CD117, and HLA-DR).
The effects of UCB-PRP on the proliferation of SHEDs, DPSCs, and PDLSCs.
The effects of UCB-PRP on the proliferation of SHEDs, DPSCs, and PDLSCs were examined at different concentrations of UCB-PRP (Fig. 2). Treatment with UCB-PRP for 24 h resulted in no significant difference in the level of cell proliferation; however, after 72 h, significant differences in cell proliferation among the groups treated with different concentrations of UCB-PRP were observed. Treatment with 2% UCB-PRP for 72 h resulted in the highest proliferation rate in SHEDs, DPSCs, and PDLSCs; however, treatment with higher concentrations of UCB-PRP resulted in a decreased proliferation rate at 72 h. These data suggest that there is an optimal concentration of UCB-PRP for the induction of proliferation, and the effect of UCB-PRP is similar among different dental stem cells. We conducted other assays with 1%, 2%, and 5% UCB-PRP.
The effects of various concentrations of UCB-PRP on the proliferation of SHEDs, DPSCs, and PDLSCs. SHEDs (A), DPSCs (B) and PDLSCs (C) were seeded at a density of 5,000 cells/cm2. The next day, cells were cultured with 0%, 2%, 5%, or 10% UCB-PRP. After 3 d of treatment, the cells were counted. As shown, treatment with 2% UCB-PRP resulted in the highest proliferation of SHEDs, DPSCs, and PDLSCs.
The effects of UCB-PRP on the ALP activity of SHEDs, DPSCs, and PDLSCs.
The ALP activity of SHEDs, DPSCs, and PDLSCs in response to different UCB-PRP concentrations is indicated in Fig. 3. The ALP activity of SHEDs treated with 2% UCB-PRP was slightly increased. In DPSCs, treatment with 2% and 5%UCB-PRP markedly increased ALP activity. In PDLSCs, ALP activity strikingly increased when the cells were treated with 1% or 2% UCB-PRP. Taken together, treatment with 1% or 2% UCB-PRP resulted in the greatest effect on ALP activity in various dental stem cells, but treatment with concentrations higher than 2% UCB-PRP resulted in a decrease in ALP activity. These results are consistent with the observed effects of UCB-PRP on cell proliferation.
The effects of various concentrations of UCB-PRP on ALP activity. SHEDs, DPSCs, and PDLSCs were cultured under osteogenic differentiation conditions with various concentrations of UCB-PRP for 3 d. Cells were harvested and assayed for ALP activity. As shown, treatment with 2% UCB-PRP resulted in the highest ALP activity in SHEDs (A), DPSCs (B), and PDLSCs (C). Data are shown as mean ± SD (n = 3). AU and N/I represent arbitrary unit and no induction, respectively.
The effects of UCB-PRP on the osteogenic differentiation of SHEDs, DPSCs, and PDLSCs.
To determine the functional effects of UCB-PRP, we conducted in vitro osteogenic differentiation analyses with various concentrations of UCB-PRP. After 21 d of treatment with UCB-PRP, the number of calcium deposits stained by Alizarin Red strikingly increased (Fig. 4A ). The quantitative determinations of calcium deposits are shown in Fig. 4B–D . Treatment with 1% or 2% UCB-PRP showed the greatest effects on calcium deposition in SHEDs, DPSCs, and PDLSCs. These data suggest that treatment with 2% PRP results in the greatest induction of ALP activity and osteogenic differentiation in our culture conditions.
In vitro osteogenic differentiation and calcium quantitation. SHEDs, DPSCs, and PDLSCs were cultured under osteogenic differentiation conditions with various concentrations of UCB-PRP for 21 d. After fixation, calcium deposits were stained with Alizarin Red (A). To quantitate the calcium content, Alizarin Red was extracted with 10% cetylpyridinum chloride, and absorbance at 570 nm was determined. As shown, treatment with 2% UCB-PRP resulted in the highest amount of calcium deposition in SHEDs (B), DPSCs (C), and PDLSCs (D). Data are shown as mean ± SD (n = 3). AU and N/I represent arbitrary unit and no induction, respectively.
Platelet counts and growth factor concentrations in UCB-PRP.
The platelet counts and growth factor concentrations in UCB-PRP are shown in Table 1. Platelet counts ranged from 128 × 106 to 253 × 106 platelets/mL with a mean value of 205 ± 59 × 106 platelets/mL. In contrast, platelet counts in fresh UCB ranged from 94 × 106 to 194 × 106 platelets/mL with a mean value of 149 ± 45 × 106 platelets/mL. The concentrations of PDGF-AB and TGF-β1 in UCB-PRP were 35,135 ± 14,506 and 24,998 ± 7,427 pg/mL, respectively. These results indicate that the number of platelets in UCB following two-step centrifugation was less than that previously obtained from peripheral blood samples (Okuda et al. 2003; Doucet et al. 2005). By contrast, UCB-PRP and peripheral blood contained comparable levels of PDGF-AB and TGF-β1. In summary, we found that platelets in UCB are well concentrated and that UCB is a more effective source of PRP than peripheral blood.
Discussion
PRP is known to contain various growth factors, including PDGF and TGF-β, which play important roles in hard tissue regeneration (Okuda et al. 2003; Barrientos et al. 2008; Ng et al. 2008). Beneficial roles of PRP in tissue regeneration have been proposed (Mishra et al. 2009). In the dental research field, PRP has been studied as a potential means by which to deliver growth factors to a wound-healing site to promote tissue regeneration. Moreover, use of PRP prepared from a patient’s own blood will likely reduce harmful immune responses. Although the therapeutic effectiveness of PRP is still under investigation, some reports showed a significant increase in bone formation and maturation rates following treatment with PRP.
PRP is commonly prepared from peripheral blood. Apheresis or centrifugation of blood is required to concentrate platelets. In this study, we used a simple two-step centrifugation method to prepare PRP from UCB. The first centrifugation step acquired PRP, and the harvested PRP was stored at −80°C. Before use, PRP was thawed rapidly at 37°C to break platelets and release growth factors from the platelets. The thawed PRP was centrifuged a second time to remove platelet bodies. Through these two steps, we acquired 30–50 mL of PRP from 100 to 150 mL of UCB. We obtained 20.5 ± 5.9 × 104 platelets/μL from 100 to 150 mL of UCB by centrifugation. The concentrations of PDGF-AB and TGF-β1 in UCB-PRP were 35 and 25 pg/μL, respectively. By contrast, Doucet et al. (2005) reported acquisition of approximately 1 × 106 platelets/μL by apheresis and PDGF-AB and TGF-β1 concentrations of 30.9 and 50.8 pg/μL, respectively. Okuda et al. (2003) reported acquisition of 70.9 ± 21.6 × 104 platelets/μL by centrifugation and PDGF-AB and TGF-β1 concentrations of 182.0 ± 75.5 and 140.9 ± 53.5 pg/μL, respectively. In our results, platelet counts were reduced by 1/5 to 1/3, and the growth factor concentrations were lower than the amounts obtained in the above reports. The use of different PRP preparation methods such as apheresis and multi-step centrifugation may explain these differences. Furthermore, the growth factor concentrations in PRP are determined by the efficiency of their release from platelet granules. Although the absolute amount of growth factors in UCB-PRP was less than that described in previous reports, we acquired higher amounts of growth factors relative to platelet counts. Moreover, our cord blood bag contained approximately 50 mL of anti-coagulant, which may dilute the platelets and growth factors released from platelets. These results showed that our UCB-PRP preparation was comparable to previous reports; however, variations existed among our PRP preparations. The amount of anti-coagulant was the same regardless of the use of UCB; therefore, platelet counts and growth factor levels may have differed among the four different UCB samples.
PRP is known to promote proliferation and differentiation of MSCs (Lucarelli et al. 2003; Doucet et al. 2005; Vogel et al. 2006; Kocaoemer et al. 2007). PDGF-AB and TGF-β1 are key growth factors that promote the differentiation of MSCs (Kulterer et al. 2007; Ng et al. 2008). Importantly, single or multiple recombinant peptides did not stimulate the proliferation of MSCs (Kawase et al. 2005). This finding suggests that other components of PRP may affect proliferation. In our results, the highest proliferation of SHEDs, DPSCs, and PDLSCs was observed using 2% UCB-PRP. Treatment with 2% UCB-PRP was expected to result in approximately 0.70 ng/mL of PDGF-AB and 0.50 ng/mL of TGF-β1. The observed growth factor concentrations were less than the levels obtained in peripheral blood in previous reports (Kawase et al. 2005). This result may be explained by the use of 5% FBS in our experiment. We used 5% FBS to acquire reproducible results in the osteogenic differentiation of SHEDs, DPSCs, and PDLSCs.
ALP is a membrane enzyme that hydrolyzes phosphate ions and thereby allows for the formation of hydroxyapatite crystals and promotes mineralization (Stein and Lian 1993), which are representative markers of bone formation. In accordance with proliferation results, treatment with 2% UCB-PRP resulted in the highest ALP activity of SHEDs, DPSCs, and PDLSCs. Although the ALP activity of SHEDs showed a slight increase following culture in osteogenic differentiation medium, calcium deposits were highest following treatment with 1% UCB-PRP. These results are consistent with the results of previous reports (Okuda et al. 2003; Schecroun and Delloye 2004; Kawase et al. 2005).
For clinical transplantation of MSCs, three criteria need to be satisfied. First, MSCs must be sufficiently expanded for transplantation. Second, immune rejection should be avoided. Last, xeno-free serum should be used for ex vivo expansion of MSCs. PRP can be used as an alternative to serum in the culture of MSCs (Capelli et al. 2007). To date, peripheral blood has been used for PRP preparation. Cord blood is considered to be a source of adult hematopoietic stem cells. Recently, banking of cord blood has become commercially feasible. Banking requires the removal of red blood cells so that only mononuclear cells are stored. In commercial banking, mononuclear cells are stored with or without autologous plasma after removal of red blood cells. Only the plasma in cord blood is usually discarded. Plasma derived from UCB may be another banking material that can replace animal serum.
In conclusion, PRP is a valuable source of autologous serum and growth factors. We obtained sufficient amounts of growth factors from UCB-PRP. Our data indicate that UCB-PRP may be used to promote the proliferation and osteogenic differentiation of SHEDs, DPSCs, and PDLSCs. The responses to UCB-PRP are different; therefore, the optimal concentration of UCB-PRP should be determined for each cell type. Similar to PRP derived from peripheral blood, UCB-PRP may contain unknown components that have beneficial effects on the proliferation and differentiation of MSCs. For the clinical application of UCB-PRP, more studies such as in vivo transplantation and banking methods are required.
References
Barrientos S.; Stojadinovic O.; Golinko M. S.; Brem H.; Tomic-Canic M. Growth factors and cytokines in wound healing. Wound Repair Regen. 16: 585–601; 2008.
Broxmeyer H. E. Biology of cord blood cells and future prospects for enhanced clinical benefit. Cytotherapy 7: 209–18; 2005.
Capelli C.; Domenghini M.; Borleri G.; Bellavita P.; Poma R.; Carobbio A.; Mico C.; Rambaldi A.; Golay J.; Introna M. Human platelet lysate allows expansion and clinical grade production of mesenchymal stromal cells from small samples of bone marrow aspirates or marrow filter washouts. Bone Marrow Transplant. 40: 785–91; 2007.
Dimitriou H.; Matsouka C.; Perdikoyanni C.; Stiakaki E.; Bolonaki I.; Lydaki E.; Koumantakis E.; Kalmanti M. Phenotypic characteristics of cord blood hemopoietic cells. Leuk. Res. 22: 755–8; 1998.
Doucet C.; Ernou I.; Zhang Y.; Llense J. R.; Begot L.; Holy X.; Lataillade J. J. Platelet lysates promote mesenchymal stem cell expansion: a safety substitute for animal serum in cell-based therapy applications. J. Cell. Physiol. 205: 228–36; 2005.
Erices A.; Conget P.; Minguell J. J. Mesenchymal progenitor cells in human umbilical cord blood. Br. J. Haematol. 109: 235–42; 2000.
Gluckman E. History of cord blood transplantation. Bone Marrow Transplant. 44: 621–6; 2009.
Ingram D. A.; Mead L. E.; Tanaka H.; Meade V.; Fenoglio A.; Mortell K.; Pollok K.; Ferkowicz M. J.; Gilley D.; Yoder M. C. Identification of a novel hierarchy of endothelial progenitor cells using human peripheral and umbilical cord blood. Blood 104: 2752–60; 2004.
Kawase T.; Okuda K.; Saito Y.; Yoshie H. In vitro evidence that the biological effects of platelet-rich plasma on periodontal ligament cells is not mediated solely by constituent transforming-growth factor-beta or platelet-derived growth factor. J. Periodontol. 76: 760–7; 2005.
Kocaoemer A.; Kern S.; Kluter H.; Bieback K. Human AB serum and thrombin-activated platelet-rich plasma are suitable alternatives to fetal calf serum for the expansion of mesenchymal stem cells from adipose tissue. Stem Cells 25: 1270–8; 2007.
Kogler G.; Sensken S.; Airey J. A.; Trapp T.; Muschen M.; Feldhahn N.; Liedtke S.; Sorg R. V.; Fischer J.; Rosenbaum C.; Greschat S.; Knipper A.; Bender J.; Degistirici O.; Gao J.; Caplan A. I.; Colletti E. J.; Almeida-Porada G.; Muller H. W.; Zanjani E.; Wernet P. A new human somatic stem cell from placental cord blood with intrinsic pluripotent differentiation potential. J. Exp. Med. 200: 123–35; 2004.
Kulterer B.; Friedl G.; Jandrositz A.; Sanchez-Cabo F.; Prokesch A.; Paar C.; Scheideler M.; Windhager R.; Preisegger K. H.; Trajanoski Z. Gene expression profiling of human mesenchymal stem cells derived from bone marrow during expansion and osteoblast differentiation. BMC Genomics 8: 70; 2007.
Lee O. K.; Kuo T. K.; Chen W. M.; Lee K. D.; Hsieh S. L.; Chen T. H. Isolation of multipotent mesenchymal stem cells from umbilical cord blood. Blood 103: 1669–75; 2004.
Lucarelli E.; Beccheroni A.; Donati D.; Sangiorgi L.; Cenacchi A.; Del Vento A. M.; Meotti C.; Bertoja A. Z.; Giardino R.; Fornasari P. M.; Mercuri M.; Picci P. Platelet-derived growth factors enhance proliferation of human stromal stem cells. Biomaterials 24: 3095–100; 2003.
Mishra A.; Tummala P.; King A.; Lee B.; Kraus M.; Tse V.; Jacobs C. R. Buffered platelet-rich plasma enhances mesenchymal stem cell proliferation and chondrogenic differentiation. Tissue Eng C Meth. 15: 431–5; 2009.
Ng F.; Boucher S.; Koh S.; Sastry K. S.; Chase L.; Lakshmipathy U.; Choong C.; Yang Z.; Vemuri M. C.; Rao M. S.; Tanavde V. PDGF, TGF-beta, and FGF signaling is important for differentiation and growth of mesenchymal stem cells (MSCs): transcriptional profiling can identify markers and signaling pathways important in differentiation of MSCs into adipogenic, chondrogenic, and osteogenic lineages. Blood 112: 295–307; 2008.
Nikolidakis D.; Jansen J. A. The biology of platelet-rich plasma and its application in oral surgery: literature review. Tissue Eng. B Rev. 14: 249–58; 2008.
Okuda K.; Kawase T.; Momose M.; Murata M.; Saito Y.; Suzuki H.; Wolff L. F.; Yoshie H. Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the proliferation of periodontally related cells in vitro. J. Periodontol. 74: 849–57; 2003.
Paloczi K. Immunophenotypic and functional characterization of human umbilical cord blood mononuclear cells. Leukemia 13(Suppl 1): S87–9; 1999.
Plachokova A. S.; Nikolidakis D.; Mulder J.; Jansen J. A.; Creugers N. H. Effect of platelet-rich plasma on bone regeneration in dentistry: a systematic review. Clin. Oral Implants Res. 19: 539–45; 2008.
Sampson S.; Gerhardt M.; Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med 1: 165–74; 2008.
Schecroun N.; Delloye C. In vitro growth and osteoblastic differentiation of human bone marrow stromal cells supported by autologous plasma. Bone 35: 517–24; 2004.
Stein G. S.; Lian J. B. Molecular mechanisms mediating proliferation/differentiation interrelationships during progressive development of the osteoblast phenotype. Endocr. Rev. 14: 424–42; 1993.
Vogel J. P.; Szalay K.; Geiger F.; Kramer M.; Richter W.; Kasten P. Platelet-rich plasma improves expansion of human mesenchymal stem cells and retains differentiation capacity and in vivo bone formation in calcium phosphate ceramics. Platelets 17: 462–9; 2006.
Acknowledgement
This work was supported by Bioteeth Project (no. 20090084043) from the National Research Foundation of Korea grant funded by the Ministry of Education, Science and Technology, Republic of Korea and by Regenomics (no. 20100002086), the nanobiotechnology development program from the National Research Foundation of Korea grant funded by the Ministry of Education, Science and Technology, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor: J. Denry Sato
Jung-Yeon Lee and Hyun Nam equally contributed to this work.
Rights and permissions
About this article
Cite this article
Lee, JY., Nam, H., Park, YJ. et al. The effects of platelet-rich plasma derived from human umbilical cord blood on the osteogenic differentiation of human dental stem cells. In Vitro Cell.Dev.Biol.-Animal 47, 157–164 (2011). https://doi.org/10.1007/s11626-010-9364-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11626-010-9364-5