ABSTRACT
Background
Most health insurance organizations reimbursed both video and audio-only (i.e., phone) visits during the COVID-19 pandemic, but may discontinue phone visit coverage after the pandemic. The impact of discontinuing phone visit coverage on various patient subgroups is uncertain.
Objective
Identify patient subgroups that are more probable to access telehealth through phone versus video.
Design
Retrospective cohort.
Patients
All patients at a U.S. academic medical center who had an outpatient visit that was eligible for telehealth from April through June 2020.
Main Measures
The marginal and cumulative effect of patient demographic, socioeconomic, and geographic characteristics on the probability of using video versus phone visits.
Key Results
A total of 104,204 patients had at least one telehealth visit and 45.4% received care through phone visits only. Patient characteristics associated with lower probability of using video visits included age (average marginal effect [AME] −6.9% for every 10 years of age increase, 95%CI −7.8, −4.5), African-American (AME −10.2%, 95%CI −11.4, −7.6), need an interpreter (AME −19.3%, 95%CI −21.8, −14.4), Medicaid as primary insurance (AME −12.1%, 95%CI −13.7, −9.0), and live in a zip code with low broadband access (AME −7.2%, 95%CI −8.1, −4.8). Most patients had more than one factor which further reduced their probability of using video visits.
Conclusions
Patients who are older, are African-American, require an interpreter, use Medicaid, and live in areas with low broadband access are less likely to use video visits as compared to phone. Post-pandemic policies that eliminate insurance coverage for phone visits may decrease telehealth access for patients who have one or more of these characteristics.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Telehealth is the use of telecommunications technology (e.g., video visits, telephone visits) to diagnose, treat, and manage health. During the COVID-19 pandemic, telehealth use surged as a result of the need for social distancing and the introduction of federal and state regulatory and insurance changes.1 As a result, approximately 1.3 million Medicare patients received care via telehealth in April 2020, compared to 11,000 just over 1 month prior.2 One key change was that audio-only telehealth (referred to as “phone visit” in this paper) was permitted. Prior to the COVID-19 pandemic, most insurance organizations required providers to perform telehealth using both real-time video and audio. Medicare and many commercial insurance programs temporarily waived the requirement for video so that patients without video-enabled devices, sufficient data to complete a video session, or adequate Internet access could receive medical care while reducing their COVID-19 exposure risk. While most stakeholders agree that video visit coverage should remain after the COVID-19 pandemic, there is disagreement on whether phone visit coverage should continue.3,4,5 In fact, the Medicare program announced that they will discontinue coverage for phone visits after the COVID-19 pandemic.6 On one hand, opponents of continuing phone visit coverage argue that phone visits limit the ability of a clinician to deliver high-quality care. On the other hand, proponents of continuing phone visit coverage argue that phone visits are an essential option for patients who lack access to video-enabled devices.
Because telehealth was not routinely used prior to the COVID-19 pandemic, little is known about the characteristics of patients who rely on phone visits versus those who can use video visits. Given the widespread prevalence of smartphones, it is plausible that most patients, or their caregivers, can perform video visits.7,8 However, even with a smartphone or device capable of connecting via video, they may not have sufficient data and a survey reported that 26.3% of Medicare patients lacked digital access in their homes.9 Furthermore, prior research has shown that older patients and racial minorities tend to have less engagement with portal engagement, which may be a prerequisite for video visit use.10 Understanding the characteristics of patients who relied on phone visits during the COVID-19 pandemic is important to prevent post-pandemic policymaking that inadvertently leads to reduced access to care. Access to care, as outlined by Andrulis, is the centerpiece in the elimination of socioeconomic disparities in health.11
Recent evidence from the COVID-19 pandemic does, in fact, show lower access to telehealth, particularly video visits, for patients with characteristics such as older age, Black race, Spanish as primary language, and lower household income.12,13,14 However, these studies focused on adult patients and used billing data. We add to this evidence by delineating patient characteristics associated with video versus phone visits based on successful video visit connection and for patients of all ages. Furthermore, because many patients will have more than one risk factor that impacts their probability of using video visits, we estimate the cumulative risk of these individual patient characteristics.
METHODS
Data Sources and Study Population
We performed a retrospective review of outpatient encounters across all specialties at Michigan Medicine, the University of Michigan’s Health System, from April 1, 2020, through June 30, 2020. This period overlaps with the Michigan stay-at-home-order, which impacted access to care. During this time, healthcare providers minimized in-person outpatient services and provided telehealth whenever possible. Using the Michigan Medicine scheduling and billing databases, Epic Clarity (Epic Systems, Madison, WI), we extracted all patient encounters for evaluation and management visits, annual wellness visits, post-operative visits, and other visits types (e.g., psychotherapy visits, disease self-management visits, nutrition visits, counseling/educational visits, consultations, and screening visits) that were eligible for telehealth according to the March 2020 COVID-19 telehealth expansion.15 There were no exclusion criteria applied.
Primary Outcome
The primary outcome was the probability of using video-based telehealth. To assess this outcome, we first categorized patients by whether they had received any telehealth or only in-person care. Patients who had telehealth were further divided into those with any video visits (suggesting video capability) and those with only phone visits (suggesting no video capability or preference for audio-only). We were able to reliably estimate whether the telehealth was video-based or audio-only by using a combination of scheduling data, billing data, and a variable that specifically identified whether a successful video connection occurred. For example, encounters scheduled as video visits, but had an unsuccessful video connection, were classified as phone visits. Our phone visit cohort did not use any video visits during the entire study period.
We assessed our primary outcome across a range of demographic, geographic, and socioeconomic variables. We obtained demographic information about each patient—including age, self-reported gender, self-identified race and ethnicity, need for an interpreter, primary insurance status, and home zip code—from the electronic medical record. We linked patient zip codes to geographically linked socioeconomic variables including rurality, broadband access, median household income, poverty, and the Digital Divide Index. Specifically, we used a list of zip codes from Federal Office of Rural Health Policy programs to identify patients with a rural zip code.16 Using the 2018 American Community Survey, we linked patient zip codes to census tract-specific estimates on median household income, the percentage of households living below the poverty threshold, and the percentage of households with broadband access.17 The Digital Divide Index combines multiple measures of broadband infrastructure, broadband adoption, and socioeconomic factors associated with technology uptake in order to more fully characterize the digital divide, with a higher score correlating with higher digital divide.18
Statistical Analysis
For each patient demographic, socioeconomic, and geographic characteristic, we calculated the proportion of patients who used video versus phone-only. We then used a multivariable logistic regression to determine the relative and cumulative effect of demographic, socioeconomic, and geographic variables on the probability of using video visits compared to phone visits. The outcome of video-based telehealth use yi for patient i was related to the patient- and geographic-specific independent variables x = xi, x2, …, xk and α the sample average via the formula below to study each independent variable’s effect on outcome while adjusting for other independent variables’ effect.
Patient-specific independent variables included age, gender, race and ethnicity, need for an interpreter, and primary insurance status. Geographic-specific independent variables included rurality, poverty, and broadband access. We translated estimated logits to a predicted probability of outcome using the formula \( \mathrm{Predicted}\ \mathrm{probability}=\frac{\exp \left(\mathrm{logit}\right)}{1+\exp \left(\mathrm{logit}\right)} \)and the car package in R.19,20 Estimated logits were obtained by using the regression coefficients estimated, including α and β, while inputting x for values representing the illustrative scenario. Since video-based telehealth use was not a rare event among our study sample, we reported the partial effect of each variable in terms of the estimated absolute difference, in lieu of odds ratios. This is more specifically the change in predicted probability of video-based telehealth use on each unit change in the independent variable of interest. Average marginal effects (AME) were estimated by holding all other variables constant using the margins package in R.21 An average marginal effect estimate of 0% indicates no effect; a negative estimate, for example −10%, indicates a 10-percentage-point lower video-use rate when compared to the reference group, and vice versa.
All analyses were performed using SAS Software Version 9.4 (SAS Institute Inc., Cary, NC, USA) and R Version 3.6.3 (The R Foundation for Statistical Computing). This study was deemed exempt from review by the University of Michigan’s institutional review board (HUM00191243).
RESULTS
Study Population
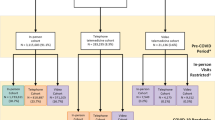
We identified 148,997 unique patients who had 266,350 outpatient visits to Michigan Medicine from April 1, 2020, to June 30, 2020. We found that 44,793 patients (30.1%) had only in-person visits (did not engage in telehealth) and 104,204 patients (69.9%) utilized at least one telehealth visit during the study period. In Appendix Table 1, we report the quartile ranges for our geographic, zip-code based factors (median household income, households below poverty, households with broadband access, digital divide index). Of all telehealth users, 45.4% received care via phone visits only, while 54.6% completed at least one video visit during the study period. The demographic, socioeconomic, and geographic makeup of our video visits and phone visits cohorts are summarized in Table 1.
The Probability of Video Visits Versus Phone Visit Use by Demographic, Socioeconomic, and Geographic Characteristics
We observed differences in the use of video versus phone by demographic, socioeconomic, and geographic characteristics. The most notable difference was age. As age increased, we observed less use of video visits compared to phone visits, with the proportion of phone-only users increasing linearly with age (Fig. 1). In total, 46.1% of patients aged 51–55 relied on phone visits compared to 54.3% of patients aged 61–65 and 63.8% of patients aged 71–75. Other notable differences included race (53.6% of self-identified Black or African-American patients used phone visits compared to 37.9% of Asian), need for interpreter (65.5% of patients who needed an interpreter for their appointments used phone visits compared to 45.1% of patients who did not), and rural zip code (50.9% of patients who lived in a rural zip code used phone visits compared to 44.7% of those who did not). Additional trends in the proportion of phone and video use according to other patient characteristics and geographic variables are displayed in Figures 2 and 3.
Using the multivariable regression analysis to hold other patient factors constant, we found that each 10-year increase in age was associated with an average decrease of 6.9% (95% CI −7.8, −4.5) in the probability of using video visits. Additionally, patients who needed an interpreter were 19.3% (95%CI −21.8, −14.4) less probable to have had a video visit, and Black or African-American patients were on average 10.2% (95%CI –11.4, –7.6) less probable to receive care via video visit compared to those who identified as white or Caucasian. Patients with Medicaid as their primary insurance and those living in rural zip codes and zip codes with lower broadband access were also less probable to have had a video visit. Figure 4 and Appendix Table 2 display the average marginal effect of each demographic, socioeconomic, and geographic characteristic that we evaluated on the absolute change in probability of video visit use among our study population.
Average marginal effects of patient and geographic variables on the probability of being a video visit user, adjusted for other patient and geographic factors. Please refer to Appendix Table 2 for the values corresponding to the quartiles of geographic variables. Error bars show the 95% confidence interval for the estimated average marginal effects. Source: Michigan Medicine institutional data April 1, 2020, through June 30, 2020. American Community Survey 2018 5-years estimates.
Cumulative Effect of Demographic, Socioeconomic, and Geographic Characteristics
To understand the cumulative effect of multiple characteristics on the probability of being a video visit user, we generated predicted probabilities for several patient scenarios, displayed in Figure 5. For example, an 18-year-oldEnglish-speaking white male who does not have Medicaid as primary insurance has a predicted probability of having participated in a video visit of 90%. A 65-year-old, but otherwise similar individual, has a predicted probability of only 50% for having participated in a video visit. A 65-year-old, who is on Medicaid, has an even lower predicted probability of video use of 37%. Finally, if this 65-year-old Medicaid patient needs an interpreter, the probability that she will have had a video visit is reduced to 19%. Across our entire study population, the mean predicted probability for a video visit was 55% (53% median) (Appendix Figure 1).
DISCUSSION
We found that during the COVID-19 pandemic, nearly half of patients who used telehealth did so through phone visits alone. We found that phone visit use was more probable among patients who were older, needed an interpreter, identified as Black or African-American, lived in a rural area, or had Medicaid as their primary insurance. Many patients had multiple risk factors that further reduced their probability of utilizing video visits. Collectively, these findings suggest that phone visits are an important way for many patient subgroups to establish care remotely.
Our finding that nearly half of telehealth users completed phone visits, as opposed to video visits, is consistent with emerging studies during the COVID-19 pandemic. For example, two studies during the early months of the COVID-19 pandemic revealed that approximately 50% of patients who used telehealth did so through the use of phone visits.13,14 Furthermore, our findings that age, race, primary language, insurance status, and geography play an important role in access to video visits is supported by these two studies and prior research on patient portal enrollment.9,13,14,22 For instance, a study by Walker et al. found that both older inpatients and African-American inpatients engaged with a tablet-based patient portal approximately 40% less than young patients or white patients.9 Similarly, a nationally representative survey found that 63% of respondents had not used a patient portal in the prior year with predictors of non-use including male gender, Medicaid insurance, lack of a regular doctor, and lower educational attainment.22 Our study goes beyond the prior and current literature in this area by demonstrating the cumulative effect of factors on the probability of using video visits.
There are many potential reasons why we noted patient differences in the use of phone visits versus video visits. First, barriers to accessing technology, such as lack of tech literacy, inadequate tech support, and decreased digital access, defined as having a connected device and Internet, may have impacted rates of phone visit versus video visit use. Income and geography play a role in digital access.10 Differences in portal enrollment may have been an additional barrier as portal use is required to access video visits at our institution. Portal enrollment may be an indicator of a patient’s comfort level with and ability to access technology. It is worth noting that while there are disparities in access to telehealth in specific populations, including rural and low-income, the COVID-19 pandemic increased overall access to and utilization of telehealth at the population level. Second, patient preference may play a role. For example, a survey of adults 65 years and older reported that 67% felt that quality of care received through telehealth is not equal to in-person care. Therefore, some patients may view the use of telehealth as temporary and be less motivated to invest effort in learning how to use video visits.23 Finally, it is important to note that the appropriateness of in-person, video, and phone visits may vary by health conditions and type of visit. For example, heart murmur assessments may require in-person visits, while mental health visits can likely be accomplished via phone or video visits. Evaluating a surgical wound may not be appropriate for a phone visit, but acceptable for a video visit in place of an in-person appointment.
There are several limitations to this study. First, the study was conducted at a single academic medical center, limiting generalizability. However, we had a very large sample and diverse patient population. Second, clinical details about individual patients were not available in our dataset. While these clinical details may have impacted the decision to use video or phone, it is unlikely that clinical differences alone drove the demographic, socioeconomic, and geographic differences we observed in this study. Third, we could not assess successful video visit connections that may have occurred outside of the electronic medical record. However, based on our knowledge of how video visits were conducted at our institution, the frequency of these alternative video visits was negligible. Lastly, patients may have relocated from their primary residence during the pandemic, affecting the accuracy of our zip code data, which was used as a surrogate for several factors. While this may have affected information on broadband access and Digital Divide Index, the home zip code is likely still accurate for factors such as median household income and poverty.
It is important for clinician practices and policymakers to consider that, while telehealth may improve access to care for many patients, it may also further widen disparities in care.24 Our findings support emerging literature that, despite the increasing use of smartphones and wider availability of Internet connectivity, many patients still depended on phone visits for access to care during COVID-19. Maintaining insurance coverage to phone visits will be important if policymakers want all patients to have an option to access their healthcare providers remotely. Moving forward, research in this area should include qualitative research to understand why some patients use phone visits versus video visits for medical care and the clinical effectiveness of phone and video visits for specific conditions and specialties.
Data Availability
Study protocol: Available from Dr. Ellimoottil (e-mail, cellimoo@med.umich.edu). Dataset: Not available.
REFERENCES
MEDICARE TELEMEDICINE HEALTH CARE PROVIDER FACT SHEET [Internet]. [cited 2020 Sep 6]. Available from: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed November 8, 2021
Verma S. Early Impact Of CMS Expansion Of Medicare Telehealth During COVID-19 [Internet]. Health Affairs Blog. 2020 [cited 2020 Oct 5]. Available from: https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/. Accessed November 8, 2021
Jaklevic, M.C.(2020) Telephone Visits Surge During the Pandemic, but Will They Last? JAMA, 324(16), 1593-1595.
Consumers expect expanded telehealth to remain post-COVID-19, survey finds. Healthcare Financial Management Association [Internet]. [2021 Jul 13]. Available from: https://www.hfma.org/topics/news/2020/07/consumers-expect-expanded-telehealth-to-remain-post-covid-19%2D%2Dsu.html. Accessed November 8, 2021
Dyrda L, Drees J, Adams K. 12 health system execs outline post-pandemic telehealth strategy. Becker’s Hospital Review [Internet]. 2020 Sep 11; Available from: https://www.beckershospitalreview.com/telehealth/12-health-system-execs-outline-post-pandemic-telehealth-strategy.html. Accessed November 8, 2021
Centers for Medicare & Medicaid Services. Medicare Program; CY 2021 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies; Medicare Shared Savings Program Requirements; Medicaid Promoting Interoperability Program Requirements for Eligible Professionals; Quality Payment Program; Coverage of Opioid Use Disorder Services Furnished by Opioid Treatment Programs; Medicare Enrollment of Opioid Treatment Programs; Electronic Prescribing for Controlled Substances for a Covered Part D Drug; Payment for Office/Outpatient Evaluation and Management Services; Hospital IQR Program; Establish New Code Categories; Medicare Diabetes Prevention Program (MDPP) Expanded Model Emergency Policy; Coding and Payment for Virtual Check-in Services Interim Final Rule Policy; Coding and Payment for Personal Protective Equipment (PPE) Interim Final Rule Policy; Regulatory Revisions in Response to the Public Health Emergency (PHE) for COVID-19; and Finalization of Certain Provisions from the March 31st, May 8th and September 2nd Interim Final Rules in Response to the PHE for COVID-19 [Internet]. Vol. 85, Federal Register. 2020. p. 84472–5377. Available from: https://www.federalregister.gov/d/2020-26815. Accessed November 8, 2021
Demographics of Mobile Device Ownership and Adoption in the United States [Internet]. [cited 2020 Aug 28]. Available from: https://www.pewresearch.org/internet/fact-sheet/mobile/. Accessed November 8, 2021
Demographics of Internet and Home Broadband Usage in the United States [Internet]. [cited 2020 Aug 28]. Available from: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Accessed November 8, 2021
Roberts ET, Mehrotra A. Assessment of Disparities in Digital Access Among Medicare Beneficiaries and Implications for Telemedicine. JAMA Internal Medicine [Internet]. 2020 [cited 2020 Aug 28]; Available from: https://doi.org/10.1001/jamainternmed.2020.2666
Walker DM, Hefner JL, Fareed N, Huerta TR, McAlearney AS. Exploring the Digital Divide: Age and Race Disparities in Use of an Inpatient Portal. Telemedicine and e-Health. 2020;26(5):603–13.
Andrulis DP. Access to care is the centerpiece in the elimination of socioeconomic disparities in health. Ann Intern Med. 1998;129(5):412–6.
Chunara R, Zhao Y, Chen J, Lawrence K, Testa PA, Nov O, et al. Telemedicine and Healthcare Disparities: A cohort study in a large healthcare system in New York City during COVID-19 [Internet]. Journal of the American Medical Informatics Association. 2020. Available from: https://doi.org/10.1093/jamia/ocaa217
Rodriguez JA, Betancourt JR, Sequist TD, Ganguli I. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1):21–6.
Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SAM, Nathan AS, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640.
President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak [Internet]. [cited 2021 Feb 8]. Available from: https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak. Accessed November 8, 2021
Federal Office of Rural Health Policy (FORHP) Data Files [Internet]. 2017 [cited 2020 Aug 23]. Available from: https://www.hrsa.gov/rural-health/about-us/definition/datafiles.html. Accessed November 8, 2021
US Census Bureau. Poverty Thresholds. [cited 2020 Aug 23]; Available from: https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html. Accessed November 8, 2021
Digital Divide Index [Internet]. [cited 2020 Aug 23]. Available from: https://pcrd.purdue.edu/2019-digital-divide-index-ddi/
Harrell FE, Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Springer; 2015. 582 p.
Companion to Applied Regression [R package car version 3.0-10]. 2020 [cited 2021 Feb 8]; Available from: https://cran.r-project.org/web/packages/car/index.html. Accessed November 8, 2021
Norton EC, Dowd BE, Maciejewski ML. Marginal Effects-Quantifying the Effect of Changes in Risk Factors in Logistic Regression Models. JAMA. 2019;321(13):1304–5.
Anthony DL, Campos-Castillo C, Lim PS. Who Isn’t Using Patient Portals And Why? Evidence And Implications From A National Sample Of US Adults. Health Affairs. 2018;37(12):1948–54.
Poll: Telehealth visits have skyrocketed for older adults, but some concerns & barriers remain [Internet]. [cited 2021 Feb 8]. Available from: https://ihpi.umich.edu/news/poll-telehealth-visits-have-skyrocketed-older-adults-some-concerns-barriers-remain. Accessed November 8, 2021
Ensuring The Growth Of Telehealth During COVID-19 Does Not Exacerbate Disparities In Care. Health Affairs Blog [Internet]. 2020 8 [cited 2020 Aug 31]; Available from: https://www.healthaffairs.org/do/10.1377/hblog20200505.591306/full/. Accessed November 8, 2021
Code Availability
Statistical code: Available from Dr. Ellimoottil (e-mail, cellimoo@med.umich.edu).
Funding
This study was supported in part by 1 K08 HS027632-01 from the Agency for Healthcare Research and Quality (Ellimoottil), 1T32HL129974 from National Heart, Lung, and Blood Institute (Li). The funding sources did not play a role in the design, conduct, or analysis of the study, or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Institutional Review Board
IRB Exempt Approved – HUM00191243
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations: None.
Supplementary Information
ESM 1
(DOCX 35 kb)
Rights and permissions
About this article
Cite this article
Chen, J., Li, K.Y., Andino, J. et al. Predictors of Audio-Only Versus Video Telehealth Visits During the COVID-19 Pandemic. J GEN INTERN MED 37, 1138–1144 (2022). https://doi.org/10.1007/s11606-021-07172-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07172-y