ABSTRACT
BACKGROUND
“Difficult visits” are common in primary care and may contribute to primary care provider (PCP) career dissatisfaction and burnout. Patient requests occur in approximately half of primary care visits and may be a source of clinician–patient miscommunication or conflict, contributing to perceived visit difficulty.
OBJECTIVE
We aimed to determine associations between types of patient requests and PCP-perceived visit difficulty.
DESIGN
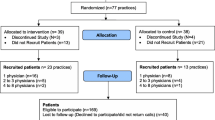
This was an observational study, nested in a multicenter randomized trial of depression engagement interventions.
SUBJECTS
We included 824 patient visits within 135 PCP practices in Northern California occurring from June 2010 to March 2012.
MAIN MEASURES
PCP-perceived visit difficulty was quantified using a three-item scale (relative visit difficulty, amount of effort required, and amount of time required; Cronbach’s α = 0.81). Using linear regression, the difficulty scale (score range 0–2 from least to most difficult) was modeled as a function of: patient requests for diagnostics tests, pain medications, and specialist referrals; PCP perception of likely depression or likely substance abuse; patient sociodemographics, comorbidity, depression; PCP characteristics and practice setting.
RESULTS
Patients requested diagnostic tests, pain medications, and specialist referrals in 37.2, 20.0 and 30.0 % of visits, respectively. After adjustment for patient medical and psychiatric complexity, perceived difficulty was significantly higher when patients requested diagnostic tests [parameter estimate (PE) 0.11, (95 % CI: 0.03, 0.20)] but not when patients requested pain medications [PE −0.04 (95 % CI: −0.15, 0.08)] or referrals [PE 0.04 (95 % CI: −0.07, 0.25)].
CONCLUSIONS
PCP-perceived visit difficulty is associated with patient requests for diagnostic tests, but not requests for pain medications or specialist referrals. In this era of “choosing wisely,” PCPs may be challenged to respond to diagnostic test requests in an evidence-based manner, while maintaining the provider–patient relationship and PCP career satisfaction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Primary care providers (PCPs) typically will experience 10 to 15 % of patient encounters as difficult.1,2 For PCPs, these visits may trigger feelings of anger, frustration, and despair,3,4 potentially leading to emotional exhaustion and burnout.5,6 Difficult encounters frustrate patients as well as providers. Compared to other patients, patients leaving difficult visits are more likely to have unmet expectations and to feel dissatisfied with their care.7 They are also more likely to report unresolved symptoms during short-term follow-up.1
Prior studies have shown that medical and psychiatric complexities are associated with PCP perceived visit difficulty.1,2,7–10 However, little is known about how patient requests influence perceived difficulty independent of such complexity. Patient requests for diagnostic testing or treatment occur in approximately half of primary care visits.11 PCPs often accede to these requests,12,13 and request fulfillment is associated with higher patient satisfaction.11,14,15 Yet PCPs do not fulfill up to one-third of patient requests,11 and they may even decline requests in ways that do not meet patients’ informational or emotional needs.16 In addition, because patient requests may lead to patient–PCP miscommunication or PCP perception that the patient is demanding or controlling,3 requests may introduce conflict and tension into the encounter, regardless of whether they are fulfilled. Patient requests for opiate pain medication may be especially likely to foster conflict during primary care encounters,17–19 and requests for diagnostic tests may introduce tension if the requested test is not recommended by clinical guidelines, such as neuroimaging for uncomplicated headache.20
In this study, we analyzed data from a randomized controlled trial of an intervention to enhance depression recognition and management in primary care. We assessed the relationship between specific types of patient requests and PCP-perceived visit difficulty. We hypothesized that after adjusting for physical and psychiatric complexities, patient requests for diagnostic tests, referrals to specialists, and pain medications would be associated with increased perceived difficulty.
METHODS
Design
Data for this observational study were derived from a multicenter, randomized controlled trial evaluating interventions to enhance patient awareness and engagement regarding depression.21 The study design has been previously described in detail.21,22 The trial included a stratified sample of depressed and non-depressed patients who were randomized to one of two patient-level depression engagement interventions or a control intervention, all of which were delivered in primary care offices immediately prior to previously scheduled follow-up visits for various reasons (i.e., not solely for depression care). There were no physician-level interventions. Post-visit data were collected from PCPs regarding the content of index visits, including whether patients requested diagnostic tests, specialty referrals, or pain medications, and PCP ratings of visit difficulty. The current study examined cross-sectional associations between PCP ratings of visit difficulty and patient requests, adjusting for patient, PCP, and system factors previously associated with or suspected to influence patient requests or perceived visit difficulty, including medical and psychiatric comorbidity and suspected substance abuse.1,7–9,11,14,15 Study visits occurred from June 2010 through March 2012.
Setting and Participants
The study was approved by the Institutional Review Boards at each study site. Study sites included academic practices, community-based multispecialty group practices, Veterans Affairs (VA) facilities, and clinics affiliated with the Kaiser Permanente health maintenance organization (HMO). Patients and PCPs were recruited from primary care clinics in six health systems located in Sacramento and San Francisco, CA.
PCPs were clinicians in family practice or general internal medicine practice, including attending physicians, certified nurse practitioners, and resident physicians. For each PCP, staff recruited by telephone up to 12 adult patients with upcoming appointments. Patients were excluded if they did not read and understand English or could not interact with a touchscreen computer. Patients were screened for depression using the Patient Health Questionnaire-9 (PHQ-9), which yields a continuous measure of depressive symptom burden ranging from 0 to 27.23 Patients with significant depression symptoms were oversampled. Although the PHQ-9 was used in sampling and study interventions were designed to facilitate discussion of depressive symptoms, PHQ-9 results were not reported to PCPs.
Perceived Difficulty
After each study visit, PCPs completed a brief questionnaires that included three consecutive questions related to visit difficulty. PCPs were specifically asked:
Compared to your average patient visit, how would you rate this visit in terms of:
-
…the amount of time required?
-
…the amount of effort required?
-
…the degree to which you found the visit difficult?
PCPs responded to each question on a three-point Likert scale (less than average, about average, or greater than average). We used these three items to generate a scale based on the average item response (range 0–2 from least to most difficult). To verify whether the three items measured a single latent construct, we performed exploratory factor analysis and examined factor loadings, eigenvalues, and scree plots. We also checked the assumptions required for creating summated rating scales by examining item-rest correlations and item-rest plots.24 These analyses all suggested that item responses to the three questions reflected a single latent construct. Regression analyses used the continuous summary scale (Cronbach’s α = 0.81).
Patient Requests and Visit Content
Patient requests and visit content were assessed by surveying patients and PCPs post-visit with brief questionnaires. In patient questionnaires, patients indicated whether they had asked or suggested that their doctor: 1) order laboratory tests or x-rays; 2) prescribe medications for pain, sleep, or depression; or 3) refer them to mental health specialists or other specialists.
In PCP questionnaires, PCPs indicated whether it was “likely or somewhat likely,” “uncertain,” or “unlikely or somewhat unlikely” that the patient had each of the following: 1) a “serious, undiagnosed medical condition”; 2) “clinically significant depression”; and 3) “alcohol or drug addiction or abuse.” If a PCP indicated that a condition was either “likely or somewhat likely” or “uncertain,” we defined in analyses that the condition was viewed by the PCP as “possible.” PCPs also indicated whether they prescribed an opiate analgesic during the visit.
Other patient characteristics
Patient sociodemographic variables were determined from pre-visit enrollment surveys, including age, sex, race/ethnicity, and educational status. Patient chronic disease burden was measured as a count of eight conditions identified by PCPs on post-visit questionnaires (i.e., hypertension; diabetes; heart disease; paralysis or stroke; chronic musculoskeletal pain; mental health condition or disorder; chronic abdominal complaints; or other chronic condition). Depressive symptom burden was categorized based on the pre-visit PHQ-9.
PCP and Practice Characteristics
In baseline written questionnaires, PCPs reported age, sex, and average number of visits per half-day. Practices were classified as HMO, academic, VA, or multispecialty group practice. The latter group consisted of community-based practices affiliated with the University of California, Davis Health System or Sutter Health in the greater Sacramento, CA area.
Analyses
Analyses were conducted with STATA (Version 13.1, StataCorp, College Station, TX) and accounted for the sampling design (oversampling of patients with higher PHQ-9 scores). For descriptive analyses only, we categorized visits with scale values of 0 to 0.333 as “less difficult,” 0.667 to 1.333 as “average difficulty,” and 1.667 to 2 as “difficult.” We chose these cut-points because item responses for two of three questions were “less than average” when scale values were 0 to 0.333 and “greater than average” for two of three questions when scale values were 1.667 to 2. We compared visit characteristics by PCP reporting using bivariate analyses (chi-squared tests and analyses of variance, as appropriate).
We performed linear regression using generalized estimating equations (GEE) to model the continuous perceived difficulty scale as a function of patient, PCP, and practice characteristics, and visit content. GEE models used a Gaussian distribution and an identity link with perceived difficulty included as a scale (ranging from 0 to 2). Parameter estimates (PEs) from the GEE models estimate the extent to which difficulty varied on this scale with unit changes in independent variables. The GEE models allowed adjustment for the nesting of patients within PCPs and practices. To assess how the impact of requests and visit content were modified by other covariates, we first fit a model that included only patient requests and whether opiates were prescribed during a visit (Model 1). We then sequentially added patient sociodemographics (Model 2), patient comorbidity and diagnoses considered possible (Model 3), and physician and practice characteristics (Model 4). All models also adjusted for the study arm.
RESULTS
Our study included 867 patients attending primary care visits with 135 PCPs (129 physicians and six nurse practitioners). PCP responses to items on visit difficulty were available for 824 patient visits. Complete patient-level data were available for 788 visits (95.6 %), and complete patient-level and provider-level data were available for 748 visits (90.7 %). The average number of visits per PCP was 6.2 (range: 1-12). Patients requested diagnostic tests in 37.2 % of visits, pain medications in 20.0 %, and specialist referrals in 30.0 % (Table 1). Based on our scale measure, PCPs perceived most visits to be of average difficulty (69.4 %), but considered 16.4 % to be difficult. In bivariate analyses, visit difficulty was significantly associated (p < 0.05) with the following: the number of chronic conditions; PHQ-9 score; patient requests for diagnostic tests; opiate prescriptions; physician consideration that a serious undiagnosed condition, depression, or substance abuse was possible; the number of patients seen per half-day; and practice setting (Table 1).
In a model including only requests and opiate prescriptions (Table 2, Model 1), patient requests for diagnostic tests and opiate prescriptions were each associated with significantly greater perceived visit difficulty, but patient requests for pain medications or specialist referrals were not (Table 2, Model 1). Addition of patient sociodemographic factors did not substantively modify these associations (Table 2, Model 2).
After the addition of patient comorbidity and diagnoses considered possible (Table 2, Model 3), opiate prescriptions were no longer significantly associated with perceived difficulty, although both greater PHQ-9 and PCP perception that depression or substance abuse was possible were each associated with greater perceived difficulty. Higher count of chronic conditions was also associated with greater difficulty. PCP perception that a serious, undiagnosed medical condition was possible or likely was not significantly associated with greater difficulty.
With the addition of PCP characteristics (Table 2, Model 4), patient requests for diagnostic tests remained significantly associated with greater perceived difficulty ([parameter estimate (PE) = 0.11 (95 % CI: 0.03, 0.20); p = 0.012], along with the chronic condition count, PHQ-9 score, and the PCP perceptions that depression or substance abuse were possible. In addition, PCPs in multispecialty group practice perceived statistically significantly greater visit difficulty than PCPs in the HMO reference group. Adjusted visit difficulty did not significantly differ across randomized study arms.
Using predicted margins from fitted GEE models, we found that visit difficulty increased similarly with diagnostic test requests among patients stratified by depression severity as measured by the PHQ-9. Associations between patient and visit characteristics and perceived difficulty were also similar in multivariate analyses of the sample of visits without missing provider-level data (n = 788) (results of sensitivity analyses available from authors).
DISCUSSION
Within diverse primary care practices, PCP-perceived visit difficulty was associated with patient requests for diagnostics tests, but not with patient requests for pain medications or specialist referrals. Results are consistent with prior research showing that PCPs perceive visits to be more difficult when patients have greater chronic disease burden, clinically significant depression, and substance abuse disorders.1,2,7–9 Our study extends this literature by showing that patient requests for diagnostic tests remain significantly associated with visit difficulty even after controlling for these important patient characteristics. Additionally, after adjustment for other factors, including PCP perception of the likelihood of depression or a substance abuse disorder, perceived difficulty was not associated with the prescription of opioid analgesics during visits.
In multivariate analyses, patient requests for diagnostic tests were statistically significantly associated with perceived difficulty, but is the observed difference also clinically significant? A request for a diagnostic test was associated with an increase in perceived difficulty as large as either an increase from 0 to 3 chronic illnesses or an increase in PHQ-9 from a normal level (0–4) to a level indicative of moderate depression (10–14).23 If requests for diagnostic tests augment perceived difficulty to a similar extent as the above changes in chronic disease or depressive symptoms, then the increase in perceived difficulty associated with test requests would seem not only statistically significant, but also clinically important.
In weighted analyses, requests for diagnostic tests occurred in 37.2 % of visits—a frequency similar to a prior study of requests in primary care.11 Requests for diagnostic tests were associated with increased difficulty even after adjusting for PCP belief in the possibility of a serious, undiagnosed condition. This suggests that requests for diagnostic tests pose difficulties to PCPs that go beyond the diagnostic uncertainties that the requested tests are supposed to address. Patient requests for specialty referrals and pain medications also occurred commonly, but even without adjustment for other factors (including PCP perceived likelihood of depression or substance abuse), these requests were not significantly associated with PCP perceived difficulty. Opiate prescriptions were associated with perceived difficulty, an association that became nonsignificant with adjustment for clinical characteristics.
Several factors may contribute to the difficulty of diagnostic test requests. First, prior research shows that about one-third of patient requests for diagnostic tests are not fulfilled, although request fulfillment enhances patient satisfaction.11 Clinicians increasingly face pressure to enhance patient satisfaction in the context of time-constrained visits.25 When a patient requests a test that is not consistent with clinical guidelines or standards of care, PCPs may face an uncomfortable dilemma: whether to acquiesce to the request or attempt to explain why the test is not recommended. The latter may risk dissatisfying the patient if the explanation does not address patients’ informational and emotional needs.16 Additionally, PCPs may worry about the malpractice risks of not ordering diagnostic tests,26 or may have an unsure grasp of the downsides of requested testing, including the risk of false-positive or false-negative results or the discovery of incidental findings requiring further evaluation. Lastly, PCPs may perceive test requests as a challenge to their authority.
The challenge of responding to patient requests for low-value tests may be particularly vexing for PCPs. We are unaware of interventions that have been shown to be effective in facilitating PCP–patient communication regarding low-value or inappropriate tests. The Kaiser Permanente health system has disseminated a theoretically grounded PCP communication workshop that emphasizes “Four Habits to Effective Communication.”27 If implemented in a conscientious manner, the four habits may foster patient-centered interactions in which care plans are collaboratively crafted to address patients’ concerns and expectations within a whole-person context. While such a patient-centered approach is a conceptually promising means of addressing patient requests for low-value diagnostic tests,28 the impact of such an approach on PCP perceived difficulty and low-value test ordering warrants rigorous evaluation.
In our analysis, perceived difficulty was associated with a PCP’s belief that depression was possible or likely, independent of depressive symptoms as measured by the PHQ-9. In other words, PCP perception of depression may augment visit difficulty, regardless of the severity of depressive symptoms. If they perceive that the patient is depressed, PCPs may feel compelled to obtain further history and diagnostic information and to advocate a plan for addressing the problem. Further, greater depression symptom burden (i.e., higher PHQ-9) was associated with greater difficulty independent of PCP perception of depression, suggesting that patient behaviors associated with depressive illness (e.g., psychomotor retardation, somatization) may complicate primary care encounters even when not recognized as depression-related.
As compared to PCPs in the HMO reference group, PCPs in multispecialty group practice rated visits as significantly more difficult. In this study, multispecialty group PCPs were affiliated with large medical groups in the urban and suburban Sacramento region, while HMO PCPs practiced within Kaiser Permanente-affiliated clinics in either Sacramento or San Francisco. To our knowledge, there were no major disruptions during the study period that may have transiently increased difficulty in only one of these settings (e.g., new adoption of an electronic medical record). Nevertheless, relatively greater system integration, increased mental health care access, or other contextual factors within the HMO may reduce average visit difficulty for HMO PCPs as compared to PCPs in multispecialty practices. The finding may also be attributable to selection bias arising from the relatively small sample of visits from the HMO setting.
In a prior study that included both PCPs and specialist physicians, chronic pain was one among many factors that contributed to physician frustration during office visits.3 Many have written about the challenges of prescribing opiate analgesics, particularly for patients with chronic, non-malignant pain.19,29,30 In bivariate analyses, both patient requests for pain medications and PCP prescriptions of opiate analgesics occurred more commonly in more versus less difficult visits. However, our multivariate analyses suggest that these associations may be mediated by comorbid mental health disorders, particularly depression and substance abuse disorders. In the absence of suspected depression or substance abuse, PCPs may not find it particularly difficult to manage requests for pain medications.
As with all observational studies, our analysis may be susceptible to unmeasured confounding, limiting causal interpretation. While we believe it is plausible that requests for diagnostic tests may augment perceived difficulty, patients who request diagnostic tests may share personality traits or communication behaviors that increase perceived difficulty independent of test requests. Measurement error may also affect study results. The three items in the difficulty scale have face validity, and in factor analyses, reflected a single underlying construct. The combined scale had high internal consistency and was correlated with similar predictors of difficulty as alternative measures of visit difficulty (e.g., patient psychiatric and medical comorbidity, suspected substance abuse).1,7 Still, study results may have differed had we used a more comprehensive measure of visit difficulty.2 Although the PCP sample was large and from diverse settings, PCP participants may differ from PCPs in other settings in their perceptions of visit difficultly. We also could not assess whether patient requests were for appropriate or inappropriate services. Lastly, confidence limits around some study estimates were wide; our study, for example, cannot exclude a clinically meaningful association between visit difficulty and pain medication requests or opioid prescriptions, although neither factor was statistically significantly associated with difficulty in multivariate analyses.
Among a sample of primary care visits at diverse clinics, PCPs perceived visits to be more difficult when patients had greater chronic illness or depressive symptom burdens. Greater difficulty was also associated with a PCP’s perception that a patient was likely to be depressed or to have a substance abuse problem. In addition, patient requests for diagnostic tests were also associated with greater difficulty, although requests for pain medications or referrals were not. Health care organizations are increasingly tasking PCPs with the dual challenges of choosing wisely in their use of diagnostic tests and therapeutics, while also maintaining high rates of patient satisfaction.31 To achieve these simultaneous goals, PCPs may grapple with the difficult task of responding to patient requests in a manner that both addresses patients’ needs and concerns and prioritizes high-value care.
REFERENCES
Hinchey SA, Jackson JL. A cohort study assessing difficult patient encounters in a walk-in primary care clinic, predictors and outcomes. J Gen Intern Med. 2011;26:588–94.
Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11:1–8.
Levinson W, Stiles WB, Inui TS, Engle R. Physician frustration in communicating with patients. Med Care. 1993;31:285–95.
Bair MJ. Patient encounters of a difficult kind. J Gen Intern Med. 2014;29:1083–4.
Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377–85.
Spickard A Jr, Gabbe SG, Christensen JF. Mid-career burnout in generalist and specialist physicians. JAMA. 2002;288:1447–50.
Jackson JL, Kroenke K. Difficult patient encounters in the ambulatory clinic: clinical predictors and outcomes. Arch Intern Med. 1999;159:1069–75.
Schafer S, Nowlis DP. Personality disorders among difficult patients. Arch Fam Med. 1998;7:126–9.
Lin EH, Katon W, Von Korff M, et al. Frustrating patients: physician and patient perspectives among distressed high users of medical services. J Gen Intern Med. 1991;6:241–6.
Hahn SR, Thompson KS, Wills TA, Stern V, Budner NS. The difficult doctor–patient relationship: somatization, personality and psychopathology. J Clin Epidemiol. 1994;47:647–57.
Kravitz RL, Bell RA, Azari R, Krupat E, Kelly-Reif S, Thom D. Request fulfillment in office practice: antecedents and relationship to outcomes. Med Care. 2002;40:38–51.
Kravitz RL, Epstein RM, Feldman MD, et al. Influence of patients’ requests for direct-to-consumer advertised antidepressants: a randomized controlled trial. JAMA. 2005;293:1995–2002.
Little P, Dorward M, Warner G, Stephens K, Senior J, Moore M. Importance of patient pressure and perceived pressure and perceived medical need for investigations, referral, and prescribing in primary care: nested observational study. BMJ. 2004;328:444.
Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315:1211–4.
Rao JK, Weinberger M, Kroenke K. Visit-specific expectations and patient-centered outcomes: a literature review. Arch Fam Med. 2000;9:1148–55.
Paterniti DA, Fancher TL, Cipri CS, Timmermans S, Heritage J, Kravitz RL. Getting to “no”: strategies primary care physicians use to deny patient requests. Arch Intern Med. 2010;170:381–8.
Dobscha SK, Corson K, Flores JA, Tansill EC, Gerrity MS. Veterans affairs primary care clinicians’ attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med. 2008;9:564–71.
Matthias MS, Parpart AL, Nyland KA, et al. The patient-provider relationship in chronic pain care: providers’ perspectives. Pain Med. 2010;11:1688–97.
Zgierska A, Miller M, Rabago D. Patient satisfaction, prescription drug abuse, and potential unintended consequences. JAMA. 2012;307:1377–8.
You JJ, Gladstone J, Symons S, Rotstein D, Laupacis A, Bell CM. Patterns of care and outcomes after computed tomography scans for headache. Am J Med. 2011;124:58–63 e1.
Kravitz RL, Franks P, Feldman MD, et al. Patient engagement programs for recognition and initial treatment of depression in primary care: a randomized trial. JAMA. 2013;310:1818–28.
Tancredi DJ, Slee CK, Jerant A, et al. Targeted versus tailored multimedia patient engagement to enhance depression recognition and treatment in primary care: randomized controlled trial protocol for the AMEP2 study. BMC Health Serv Res. 2013;13:141.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
McIver JP, Carmines EG. Unidimensional Scaling. Beverly Hills, CA: Sage Publications; 1981.
Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405–11.
Sirovich BE, Woloshin S, Schwartz LM. Too Little? Too Much? Primary care physicians’ views on US health care: a brief report. Arch Intern Med. 2011;171:1582–5.
Stein T, Frankel RM, Krupat E. Enhancing clinician communication skills in a large healthcare organization: a longitudinal case study. Patient Educ Couns. 2005;58:4–12.
Epstein RM, Franks P, Shields CG, et al. Patient-centered communication and diagnostic testing. Ann Fam Med. 2005;3:415–21.
Katz MH. Opioid prescriptions for chronic nonmalignant pain: driving on a dangerous road. JAMA Intern Med. 2013;173:178.
Von Korff M, Kolodny A, Deyo RA, Chou R. Long-term opioid therapy reconsidered. Ann Intern Med. 2011;155:325–8.
Cassel CK, Guest JA. Choosing wisely: helping physicians and patients make smart decisions about their care. JAMA. 2012;307:1801–2.
Acknowledgements
This work was supported by grants 1R01MH079387 (Kravitz) and K24MH072756 (Kravitz) from the National Institute of Mental Health.
Conflicts of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fenton, J.J., Franks, P., Feldman, M.D. et al. Impact of Patient Requests on Provider-Perceived Visit Difficulty in Primary Care. J GEN INTERN MED 30, 214–220 (2015). https://doi.org/10.1007/s11606-014-3082-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3082-8