ABSTRACT
BACKGROUND
Only 38 % of young adults with hypertension have controlled blood pressure. Lifestyle education is a critical initial step for hypertension control. Previous studies have not assessed the type and frequency of lifestyle education in young adults with incident hypertension.
OBJECTIVE
The purpose of this study was to determine patient, provider, and visit predictors of documented lifestyle education among young adults with incident hypertension.
DESIGN
We conducted a retrospective analysis of manually abstracted electronic health record data.
PARTICIPANTS
A random selection of adults 18–39 years old (n = 500), managed by a large academic practice from 2008 to 2011 and who met JNC 7 clinical criteria for incident hypertension, participated in the study.
MAIN MEASURES
The primary outcome was the presence of any documented lifestyle education during one year after meeting criteria for incident hypertension. Abstracted topics included documented patient education for exercise, tobacco cessation, alcohol use, stress management/stress reduction, Dietary Approaches to Stop Hypertension (DASH) diet, and weight loss. Clinic visits were categorized based upon a modified established taxonomy to characterize patients’ patterns of outpatient service. We excluded patients with previous hypertension diagnoses, previous antihypertensive medications, or pregnancy. Logistic regression was used to identify predictors of documented education.
KEY RESULTS
Overall, 55 % (n = 275) of patients had documented lifestyle education within one year of incident hypertension. Exercise was the most frequent topic (64 %). Young adult males had significantly decreased odds of receiving documented education. Patients with a previous diagnosis of hyperlipidemia or a family history of hypertension or coronary artery disease had increased odds of documented education. Among visit types, chronic disease visits predicted documented lifestyle education, but not acute or other/preventive visits.
CONCLUSIONS
Among young adults with incident hypertension, only 55 % had documented lifestyle education within one year. Knowledge of patient, provider, and visit predictors of education can help better target the development of interventions to improve young adult health education and hypertension control.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Hypertension is the leading cause of preventable death in the United States.1 Among young adults (18–39 year olds),2 approximately 9 % of men and 7 % of women have hypertension, defined as having a systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, taking antihypertensive medication, or being told twice by a physician or other medical professional that one has hypertension.3 Young adults have lower hypertension control compared to ≥ 40 year olds; the prevalence of control among young adults is only 38 % compared to ≥ 50 % in middle-aged and older adults.2 – 4
The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)5 and recent guideline updates6 , 7 identify lifestyle modifications as a critical first-line step to hypertension control.5 – 7 Recommended lifestyle modifications include: weight loss in overweight and obese individuals, adoption of the Dietary Approaches to Stop Hypertension (DASH) plan, dietary sodium reduction, physical activity, and moderation of alcohol intake.5 , 8 Tobacco cessation is recommended for overall cardiovascular risk reduction.5 Lifestyle modifications are effective in improving hypertension control,9 – 11 reducing cardiovascular risk,12 and enhancing antihypertensive medication efficacy.
Despite the benefits of lifestyle modifications, previous research suggests that few middle-aged and older adults with hypertension receive physician education, with most rates < 50 %.13 – 21 However, most previous studies are cross-sectional with limited longitudinal follow-up; there are no studies assessing lifestyle education in populations with incident hypertension. The development of incident hypertension is an important “teachable moment”22 to educate about the adoption and maintenance of lifestyle modifications. In a clinical environment with competing time demands,23 – 25 an understanding of lifestyle education patterns, as well as how visit types (i.e., acute, chronic, preventive) influence such education, are needed to develop targeted hypertension interventions. Therefore, the purpose of this study was to determine the presence of any documented lifestyle education in an electronic health record system for young adults with incident hypertension, and to identify patient, provider, and visit predictors of receiving documented education.
METHODS
Sample
This study was approved by the University of Wisconsin-Madison Health Sciences Institutional Review Board with a waiver of consent. For our sample, we first identified 18–39 year olds who met established criteria from the Wisconsin Collaborative for Healthcare Quality (WCHQ)26 , 27 for being “currently managed” in a large, Midwestern, multi-disciplinary academic group practice between 1 January 2008 and 31 December 2011. Per WCHQ criteria, patients had to have ≥ 2 billable office encounters in an outpatient, non-urgent, primary care setting, or one primary care and one office encounter in an urgent care setting (regardless of diagnosis code), in the 3 years prior to study enrollment, with at least one of those visits in the prior 2 years.28 Patient records were then evaluated for the first date that JNC 7 blood pressure criteria for a hypertension diagnosis5 were met. Blood pressure eligibility criteria were based on electronic health record data: a) ≥ 3 elevated outpatient blood pressure measurements (systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg) from three separate dates, ≥ 30 days apart but within a 2-year span5; or b) 2 elevated blood pressures (systolic blood pressure ≥ 160 mmHg or diastolic blood pressure ≥ 100 mmHg),29 , 30 ≥ 30 days apart but within a 2-year period. The blood pressures did not need to be from billable encounters. If more than one blood pressure was taken at a visit, the average was used.5 A total of 33,974 adults met both JNC 7 and WCHQ currently managed criteria (Fig. 1).
The 365 days prior to study enrollment was the “baseline period” to assess patients’ baseline comorbidities and utilization. To achieve a sample with incident hypertension, patients were excluded if they had a diagnosis of hypertension in the baseline based on the Tu criteria31 , 32 or a previous antihypertensive medication prescription(s).31 Patients who were pregnant were excluded one year before, during, and one year after pregnancy using a modified Manson approach.33 Applying these exclusion criteria, 4,023 young adult patients met criteria for incident hypertension and met guideline criteria for hypertension management. From this population, 500 young adults were randomly selected for manual electronic health record abstraction. A sample size of 500 records was selected, to have at least ten charts per predictor and at least 10 % of young adults with incident hypertension34 , 35 to ensure a feasible and clinically relevant study population.
Electronic Health Record Abstraction
Each face-to-face ambulatory visit that occurred within one year (365 days) after a patient met criteria for incident hypertension was manually abstracted. Historical visits used to determine eligibility were not abstracted; they did not need to be billable encounters and likely had limited documentation. Abstracted visits were from the following clinics: Internal Medicine, Family Medicine/Family Practice, Pediatrics/Adolescent Medicine, Obstetrics/Gynecology, Cardiology, Endocrinology, Nephrology, and Rheumatology. Specialties that included potentially sensitive information (e.g., Infectious Disease, Psychiatry), Geriatrics, and clinics that did not require blood pressure documentation at every visit since 2007 (e.g., Allergy, Surgical specialties) were excluded.
All clinical staff encounter notes (i.e., medical assistants, nurses, nurse practitioners, physician assistants, educators, physicians, resident/fellow trainees, etc.) and patients’ after-visit instructions were manually abstracted to assess for any documented education. Education topics included exercise, alcohol use, stress management/stress reduction, DASH diet, low salt/sodium, weight reduction, or tobacco cessation. Each encounter was also assessed for general lifestyle terms (e.g., “heart-healthy changes”, “lifestyle changes”), notation of educational handouts and/or websites provided, and/or patient refusal of education. The presence/absence of a family history of hypertension and/or premature coronary artery disease was abstracted.36 The abstraction protocol was created by the authors based on previously published methodology37 , 38 and clinical expertise.
Two trained medical abstractors used a standardized approach to optimize reliability.39 A 10 % random re-abstraction was performed after every 100 patients. Abstractors convened face-to-face at least bi-monthly to discuss re-abstraction items with low reliability so that consensus could be reached. This approach resulted in inter-rater agreement of > 95 % for 29 components, 85–94 % for two components, and 71–76 % for three components (i.e., general lifestyle term, tobacco cessation, and family history). A consensus was reached when the two abstractors did not agree.
Explanatory Variables
Patient-related explanatory variables to identify barriers to hypertension education were obtained from clinical and administrative data from the academic group practice, including: age, sex, marital status, baseline tobacco use, body mass index (BMI), and JNC 7 hypertension stage (Stage 1: 140–159/90–99 mmHg; Stage 2: ≥ 160/100 mmHg). Patients’ comorbidities, including hyperlipidemia,40 diabetes mellitus,41 and a combined variable of anxiety42 and/or depression43 , 44 were assessed using established algorithms. Baseline study year was included to assess secular trends in education documentation. We used the Johns Hopkins Adjusted Clinical Group (ACG) Case-Mix System (version 10.0) to assess morbidity burden based on patient baseline age, gender, and disease patterns.45 Additional utilization measures included the total number of clinic visits during the abstraction period.
Patients were assigned to the provider they saw most frequently in outpatient face-to-face Evaluation & Management visits, as reported in professional service claims.28 Models also included each provider’s specialty, classified as Primary Care (Internal Medicine, Family Practice/Family Medicine, Pediatrics/Adolescent Medicine, Obstetrics/Gynecology) or Specialty Care (Endocrinology, Cardiology, Nephrology, Rheumatology), age, and gender, which were obtained from the provider group’s human resource office and/or the American Medical Association (AMA) 2011 Masterfile data.
Visits were categorized using a modified established taxonomy by Fenton et al.23 to characterize patients’ patterns of outpatient service. Each ICD-9 code from the outpatient visits was categorized into one of seven major diagnostic categories: acute diseases, chronic diseases, symptoms and ill-defined conditions, mental illnesses, vision and hearing disorders, dermatologic diseases, and preventive care/pregnancy-related conditions.23 Visits could be coded for multiple categories. Given the study’s smaller sample size, the categories were modified to include acute, chronic, and other. Fenton defined a chronic disease as recurrent and lasting for more than 3 months.23 The “other” category was defined by merging the five sub-categories (symptoms and ill-defined conditions, mental illness, vision and hearing disorders, dermatologic diseases, and preventive care).23
Statistical Analysis
Analyses were conducted using SAS 9.1.3 (SAS Institute, Inc., Cary, NC) and Stata/MP 12.1 (StataCorp LP; College Station, TX). Categorical variables were summarized using percentages. Continuous variables were summarized using means (SD). We compared patient, provider, and clinic visit descriptive characteristics based on the presence of documented education using Chi-square and Wilcoxon rank-sum tests. Multivariable logistic regression models were estimated at two levels: patient-level and visit-level. At the patient-level, models estimated adjusted odds ratios (ORs) and 95 % confidence intervals (CIs) for patient and provider predictors of documented lifestyle education, with robust estimates of the variance that account for clustering. In a sensitivity analysis, logistic models were re-analyzed clustered on individual provider; the independent predictors did not differ (data not shown). At the visit level, models were clustered by patient-estimated odds ratios and 95 % confidence intervals for documented education by visit type (i.e., acute, chronic, other), after adjusting for patient and provider factors.
RESULTS
Sample Characteristics
The majority of young adults (Table 1) with incident hypertension were male (62 %), obese or morbidly obese (63 %), and had a family history of hypertension and/or premature coronary artery disease in a first-degree relative (53 %). Overall, 55 % (n = 275) had at least one encounter with documented lifestyle education during the one-year abstraction period. There were a total of 396 different providers. There were few referrals for separate visits to dieticians/nutritionists (n = 19; 3.8 %).
Among patients that received education, 50 % (n = 138) had less than or equal to two visits with education during one year of follow-up, 24 % (n = 66) had three to four visits, and 26 % (n = 71) had greater than or equal to five visits. Only four (0.8 %) had documented refusal of lifestyle education. Compared to adults without documented education (Table 1), those with education were on average more likely to receive an initial hypertension diagnosis and/or an initial antihypertensive prescription during the study period, have a family history of hypertension and/or coronary artery disease, a higher BMI, and lower ACG risk index. Males were less likely to have documentation than females. There were no significant differences in documented education between patient age, marital status, race/ethnicity, tobacco use, hypertension stage, comorbidities, or provider specialty.
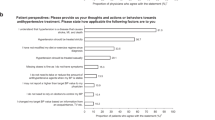
Among counseled patients (Fig. 2), exercise was the most frequently documented topic (64 %), followed by low-fat/other dietary topics (55 %). Examples of other dietary topics include portion control and the Mediterranean diet. Among current tobacco users, 71 % had documented cessation education. Low sodium/DASH diet education was documented among only 25 % of counseled young adults.
Percentage of 18–39 year olds with incident hypertension receiving documented lifestyle education by topic (among counseled patients, n = 275). *Tobacco cessation education was only among current tobacco users, †Other Diet: Examples include low fat, low cholesterol, Mediterranean diet, etc., ‡DASH = Dietary Approaches to Stop Hypertension diet, §General lifestyle = education mentioned in electronic health record, details unknown.
Patient, Provider, and Visit Predictors of Documented Lifestyle Education
After adjustment (Table 2), in the patient-level model, predictors of increased odds of documented education included a family history of hypertension and/or premature coronary artery disease (OR 1.96; 95 % CI 1.28–2.98) or baseline hyperlipidemia (OR 2.25; 95 % CI 1.09–4.65). Males (OR 0.48; 95 % CI 0.29–0.80) had decreased odds of documented education. Patients with the highest clinic visit tertile (≥ 5 visits) during the abstraction period had decreased odds of documented education (OR 0.48; 95 % CI 0.27–0.86) compared to those in the lowest tertile (≤ 2 visits). Patient age and baseline study year were not significant predictors. In this patient-level analysis, provider factors (age, specialty, and sex) did not independently predict documented education.
Visit-level analyses (Table 3) evaluated the effect of visit type on documented education. After adjustment, chronic disease visits demonstrated higher odds of documented lifestyle education (OR 2.36; 95 % CI 1.68–3.32) compared to acute or other visits. Patient predictors identified in the patient model (Table 2) remained significant in visit analysis. At the visit level, Primary Care visits, compared to subspecialty visits, had increased odds of documented lifestyle education, and providers in the highest age tertile had lower odds of documented education.
DISCUSSION
To our knowledge, this is the first study to evaluate the documentation of lifestyle education in the electronic health record among young adults with incident hypertension. Among the 500 young adults, only 55 % (n = 275) had any documented hypertension education within one year of meeting criteria for incident hypertension; 23 % (n = 115) received an initial hypertension diagnosis and/or an initial antihypertensive prescription within one year. Overall, 22 % (n = 110) did not have any documentation (i.e., lack of documented education, diagnosis, and treatment), emphasizing a lack of hypertension awareness.
Previous studies documented some providers’ hesitancy to prescribe potentially lifelong antihypertensive medication.46 Therefore, we hypothesized that within one year, young adults that did not receive a hypertension diagnosis or antihypertensive medication would receive lifestyle education. Our results highlight that, in contrast, a significant number of young adults do not have any documented management of their hypertension, while others receive a hypertension diagnosis with lifestyle education (+/- pharmacotherapy). This gap in care between young adults likely contributes to low hypertension control.
Our demographics demonstrated that young adult males are more likely to have hypertension compared to females, similar to the National Health and Nutrition Examination Survey (NHANES).3 However, despite a higher prevalence of hypertension among males, females were 33 % more likely to have documented education. Our findings conflict with studies conducted in predominantly older adults, which demonstrate either no significant differences in lifestyle education according to patient gender, or that males are more likely to receive weight loss education compared to females.18 , 47 We additionally found that provider gender was not an independent predictor of documented education. The influence of provider gender on documented education is unclear. Studies have demonstrated no significant difference in education among provider gender; in other studies, female providers deliver more gender-specific preventive services.48 – 50 Overall, our results may reflect gender differences in young adult patient initiatives for lifestyle modifications.
Among patients that received education, exercise and tobacco cessation were the most frequent topics. We previously demonstrated that current tobacco use decreased the likelihood of receiving a new hypertension diagnosis by 24 %.31 Per this current study, the majority of current tobacco users with incident hypertension are receiving cessation education. However, hypertension follow-up visits are needed for continued education and guideline-based care.5 In our study, only 25 % of counseled patients received DASH diet education. This may reflect our population’s demographic composition (18 % non-White). Although guidelines recommend sodium reduction for all hypertensive patients, the low-sodium/DASH plan has demonstrated greater blood pressure reduction in African-Americans.5 Our providers’ focus on weight reduction and low-fat diets likely reflects high obesity rates.
We demonstrated important positive and negative patient predictors of documented lifestyle education. Young adults with hyperlipidemia or a family history of hypertension/premature coronary artery disease each demonstrated significantly increased odds of documented education. Piette and Kerr51 found that concordant comorbid conditions (e.g., dyslipidemia, hypertension) may positively influence guideline-based treatment. Patients with concordant risk factors are more likely to have hypertension education.18 In our study, the presence of diabetes mellitus, although a concordant condition, was not a significant predictor; this may be due to a smaller sample size (4.2 % of total population). Young adults in the highest visit tertile (≥ 5 visits) had a 27 % lower likelihood of documented education. This likely reflects patients with multiple complex conditions resulting in frequent visits with competing demands.52
Chronic disease management visits were more likely to have documented lifestyle education compared to acute or other (including Preventive) visits. This supports our discussion above that some concordant diagnoses are associated with greater guideline-based care. In previous research among adolescents (11–21 year olds), more diet and exercise education occurred during acute visits compared to well-care visits.53 We were able to examine all visit types (acute, chronic, and other). Almost 50 % of our population had mixed visit types (acute +/- chronic +/- other), again highlighting the likelihood of competing demands. Visits with lifestyle education have demonstrated longer mean visit lengths.14 Stange et al. concluded that one minute is the realistic average amount of time primary care providers have to commit to prevention education in a typical office visit.54 Given previously reported obesity trends in the United States55 and in this population, young adults with hypertension will likely have more than one cardiovascular risk factor, requiring recurrent lifestyle education for multiple comorbidities. Interventions including team-based care may address competing clinical demands and improve lifestyle education.56
Despite their limitations, narrative notes by healthcare providers have been a primary source of information on providing lifestyle education.57 However, relying solely on medical record documentation can result in falsely low true counseling rates; for example, providers only using verbal education without documentation would not be captured. To improve our sensitivity, we abstracted all documentation from physician and non-physician providers (e.g. registered nurses, medical assistants) during the encounter. Although our measure of lifestyle counseling may under-report the true prevalence, patient characteristics will likely not differ, and thus our predictors of counseling are likely valid. Any counseling prior to meeting study eligibility would not have been captured. However, historical visits were up to two years prior to study entry, and would not reflect documented management of young adults after meeting hypertension diagnostic criteria.
Although this study included a single Midwestern healthcare system, it is one of the ten largest physician practice groups in the United States. The inclusion of patient demographic, comorbidity, and utilization data, as well as provider and clinic data, improves the generalizability and clinical applicability of our data. However, since only 12 % of patients were treated by specialists, this data may be more applicable to Primary Care. Although ambulatory blood pressures were not available to confirm the diagnosis of hypertension, lifestyle education is widely applicable for the prevention and treatment of hypertension. During our study, education reminders/check boxes were not embedded in the electronic health record to support education documentation. Yet, our findings are consistent with previous studies using video recordings and direct research nurse observations that also demonstrated sub-optimal education rates (9–77 %).47 , 58 Other potential limitations include recall bias and documentation variability; however, previous studies with survey data and manual paper chart abstraction13 are subject to similar bias,59 , 60 and audio recording14 has its own limitations.57 In addition, we did not examine the frequency of documentation between physicians and non-physicians (e.g., nurse practitioners/physician assistants). This study could not evaluate education quality, but highlights common topics primary care providers discuss with young adults. Qualitative analysis is needed to evaluate providers’ self-efficacy in young adult education.
Conclusions
Among young adults with incident hypertension, only 55 % had documented lifestyle education. Patient, provider, and visit characteristics predict documented education. Healthcare system interventions empowering additional clinical staff for health coaching and lifestyle education may address some of these barriers.
REFERENCES
Kochanek KD, Xu J, Murphy SL, Minino AM, Kung HC. Deaths: preliminary data for 2009. Natl Vital Stat Rep. 2011;59:1–51.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–50.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292.
Yoon PW, Gillespie CD, George MG, Wall HK. Control of hypertension among adults—National Health and Nutrition Examination Survey, United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2012;61:19–25.
Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72.
James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507–20.
Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;16:14–26.
Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension. 2006;47:296–308.
Mattila R, Malmivaara A, Kastarinen M, Kivela SL, Nissinen A. Effectiveness of multidisciplinary lifestyle intervention for hypertension: a randomised controlled trial. J Hum Hypertens. 2003;17:199–205.
Miller ER 3rd, Erlinger TP, Young DR, et al. Results of the Diet, Exercise, and Weight Loss Intervention Trial (DEW-IT). Hypertension. 2002;40:612–8.
Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503.
Ketola E, Sipila R, Makela M. Effectiveness of individual lifestyle interventions in reducing cardiovascular disease and risk factors. Ann Med. 2000;32:239–51.
Ardery G, Carter BL, Milchak JL, et al. Explicit and implicit evaluation of physician adherence to hypertension guidelines. J Clin Hypertens (Greenwich). 2007;9:113–9.
Bell RA, Kravitz RL. Physician counseling for hypertension: what do doctors really do? Patient Educ Couns. 2008;72:115–21.
Booth AO, Nowson CA. Patient recall of receiving lifestyle advice for overweight and hypertension from their General Practitioner. BMC Fam Pract. 2010;11:8.
Egede LE, Zheng D. Modifiable cardiovascular risk factors in adults with diabetes: prevalence and missed opportunities for physician counseling. Arch Intern Med. 2002;162:427–33.
Heymann AD, Gross R, Tabenkin H, Porter B, Porath A. Factors associated with hypertensive patients' compliance with recommended lifestyle behaviors. Isr Med Assoc J. 2011;13:553–7.
Mellen PB, Palla SL, Goff DC Jr, Bonds DE. Prevalence of nutrition and exercise counseling for patients with hypertension. United States, 1999 to 2000. J Gen Intern Med. 2004;19:917–24.
Moeller MA, Snelling AM. Health professionals' advice to Iowa adults with hypertension using the 2002 Behavioral Risk Factor Surveillance System. Am J Health Promot. 2006;20:392–5.
Valderrama AL, Tong X, Ayala C, Keenan NL. Prevalence of self-reported hypertension, advice received from health care professionals, and actions taken to reduce blood pressure among US adults—HealthStyles, 2008. J Clin Hypertens (Greenwich). 2010;12:784–92.
Viera AJ, Kshirsagar AV, Hinderliter AL. Lifestyle modification advice for lowering or controlling high blood pressure: who's getting it? J Clin Hypertens (Greenwich). 2007;9:850–8.
Tsiantou V, Pantzou P, Pavi E, Koulierakis G, Kyriopoulos J. Factors affecting adherence to antihypertensive medication in Greece: results from a qualitative study. Patient Prefer Adherence. 2010;4:335–43.
Fenton JJ, Von Korff M, Lin EH, Ciechanowski P, Young BA. Quality of preventive care for diabetes: effects of visit frequency and competing demands. Ann Fam Med. 2006;4:32–9.
Zulman DM, Kerr EA, Hofer TP, Heisler M, Zikmund-Fisher BJ. Patient-provider concordance in the prioritization of health conditions among hypertensive diabetes patients. J Gen Intern Med. 2010;25:408–14.
Jaén CR, Stange KC, Nutting PA. Competing demands of primary care: a model for the delivery of clinical preventive services. J Fam Pract. 1994;38:166–71.
Hatahet MA, Bowhan J, Clough EA. Wisconsin Collaborative for Healthcare Quality (WCHQ): lessons learned. WMJ. 2004;103:45–8.
Sheehy A, Pandhi N, Coursin DB, et al. Minority status and diabetes screening in an ambulatory population. Diabetes Care. 2011;34:1289–94.
Thorpe CT, Flood GE, Kraft SA, Everett CM, Smith MA. Effect of patient selection method on provider group performance estimates. Med Care. 2011;49:780–5.
Myers MG, Tobe SW, McKay DW, Bolli P, Hemmelgarn BR, McAlister FA. New algorithm for the diagnosis of hypertension. Am J Hypertens. 2005;18:1369–74.
Schmittdiel J, Selby JV, Swain B, et al. Missed opportunities in cardiovascular disease prevention?: low rates of hypertension recognition for women at medicine and obstetrics-gynecology clinics. Hypertension. 2011;57:717–22.
Johnson HM, Thorpe CT, Bartels CM, et al. Undiagnosed hypertension among young adults with regular primary care use. J Hypertens. 2014;32:65–74.
Tu K, Campbell NR, Chen ZL, Cauch-Dudek KJ, McAlister FA. Accuracy of administrative databases in identifying patients with hypertension. Open Med. 2007;1:e18–26.
Manson JM, McFarland B, Weiss S. Use of an automated database to evaluate markers for early detection of pregnancy. Am J Epidemiol. 2001;154:180–7.
Gearing RE, Mian IA, Barber J, Ickowicz A. A methodology for conducting retrospective chart review research in child and adolescent psychiatry. J Can Acad Child Adolesc Psychiatry. 2006;15:126–34.
Harrell FE Jr, Lee KL, Matchar DB, Reichert TA. Regression models for prognostic prediction: advantages, problems, and suggested solutions. Cancer Treat Rep. 1985;69:1071–77.
Scheuner MT, Wang SJ, Raffel LJ, Larabell SK, Rotter JI. Family history: a comprehensive genetic risk assessment method for the chronic conditions of adulthood. Am J Med Genet. 1997;71:315–24.
Fluker SA, Whalen U, Schneider J, et al. Incorporating performance improvement methods into a needs assessment: experience with a nutrition and exercise curriculum. J Gen Intern Med. 2010;25:S627–33.
Murff HJ, Rothman RL, Byrne DW, Syngal S. The impact of family history of diabetes on glucose testing and counseling behavior in primary care. Diabetes Care. 2004;27:2247–8.
Reisch LM, Fosse JS, Beverly K, et al. Training, quality assurance, and assessment of medical record abstraction in a multisite study. Am J Epidemiol. 2003;157:546–51.
Borzecki AM, Wong AT, Hickey EC, Ash AS, Berlowitz DR. Identifying hypertension-related comorbidities from administrative data: what's the optimal approach? Am J Med Qual. 2004;19:201–6.
Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM. Identifying persons with diabetes using Medicare claims data. Am J Med Qual. 1999;14:270–7.
Marciniak MD, Lage MJ, Dunayevich E, et al. The cost of treating anxiety: the medical and demographic correlates that impact total medical costs. Depress Anxiety. 2005;21:178–84.
Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27.
Fawcett J, Kravitz HM. Anxiety syndromes and their relationship to depressive illness. J Clin Psychiatry. 1983;44:8–11.
Starfield B, Weiner J, Mumford L, Steinwachs D. Ambulatory care groups: a categorization of diagnoses for research and management. Health Serv Res. 1991;26:53–74.
Mitsnefes MM. Hypertension in children and adolescents. Pediatr Clin North Am. 2006;53:493–512.
Milder IE, Blokstra A, de Groot J, van Dulmen S, Bemelmans WJ. Lifestyle counseling in hypertension-related visits--analysis of video-taped general practice visits. BMC Fam Pract. 2008;9:58.
Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33:407–16.
Henderson JT, Weisman CS. Physician gender effects on preventive screening and counseling: an analysis of male and female patients' health care experiences. Med Care. 2001;39:1281–92.
Schmittdiel J, Grumbach K, Selby JV, Quesenberry CP Jr. Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J Gen Intern Med. 2000;15:761–9.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29:725–31.
Krein SL, Hofer TP, Holleman R, Piette JD, Klamerus ML, Kerr EA. More than a pain in the neck: how discussing chronic pain affects hypertension medication intensification. J Gen Intern Med. 2009;24:911–6.
Rand CM, Auinger P, Klein JD, Weitzman M. Preventive counseling at adolescent ambulatory visits. J Adolesc Health. 2005;37:87–93.
Stange KC, Woolf SH, Gjeltema K. One minute for prevention: the power of leveraging to fulfill the promise of health behavior counseling. Am J Prev Med. 2002;22:320–3.
Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS Data Brief. 2012:1–8.
Yarnall KS, Ostbye T, Krause KM, Pollak KI, Gradison M, Michener JL. Family physicians as team leaders: “time” to share the care. Prev Chronic Dis. 2009;6:A59.
Stange KC, Zyzanski SJ, Smith TF, et al. How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patients visits. Med Care. 1998;36:851–67.
Stange KC, Flocke SA, Goodwin MA, Kelly RB, Zyzanski SJ. Direct observation of rates of preventive service delivery in community family practice. Prev Med. 2000;31:167–76.
Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576–8.
Wee CC, McCarthy EP, Davis RB, Phillips RS. Physician counseling about exercise. JAMA. 1999;282:1583–8.
Acknowledgements
Contributors
The authors gratefully acknowledge Patrick Ferguson and Katie Ronk for data preparation, and Colleen Brown for manuscript preparation.
Funders
Research reported in this manuscript was supported by the Health Innovation Program and the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) under award number UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health under award number U54TR000021. Heather Johnson is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number K23HL112907, and also by the University of Wisconsin Centennial Scholars Program of the University of Wisconsin School of Medicine and Public Health. Amy Kind is supported by the National Institute on Aging of the National Institutes of Health under award number K23AG034551, the American Federation for Aging Research, the Atlantic Philanthropies, the Starr Foundation, and the Madison VA Geriatric Research, Education, and Clinical Center. Nancy Pandhi is supported by the National Institute on Aging of the National Institutes of Health under award number K08AG029527. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additional funding for this project was provided by the University of Wisconsin Health Innovation Program and the University of Wisconsin School of Medicine and Public Health from the Wisconsin Partnership Program.
Prior Presentations
None.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, H.M., Olson, A.G., LaMantia, J.N. et al. Documented Lifestyle Education Among Young Adults with Incident Hypertension. J GEN INTERN MED 30, 556–564 (2015). https://doi.org/10.1007/s11606-014-3059-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-014-3059-7