ABSTRACT
BACKGROUND
The use of electronic health records (EHR) is widely recommended as a means to improve the quality, safety and efficiency of US healthcare. Relatively little is known, however, about how implementation and use of this technology affects the work of clinicians and support staff who provide primary health care in small, independent practices.
OBJECTIVE
To study the impact of EHR use on clinician and staff work burden in small, community-based primary care practices.
DESIGN
We conducted in-depth field research in seven community-based primary care practices. A team of field researchers spent 9–14 days over a 4–8 week period observing work in each practice, following patients through the practices, conducting interviews with key informants, and collecting documents and photographs. Field research data were coded and analyzed by a multidisciplinary research team, using a grounded theory approach.
PARTICIPANTS
All practice members and selected patients in seven community-based primary care practices in the Northeastern US.
KEY RESULTS
The impact of EHR use on work burden differed for clinicians compared to support staff. EHR use reduced both clerical and clinical staff work burden by improving how they check in and room patients, how they chart their work, and how they communicate with both patients and providers. In contrast, EHR use reduced some clinician work (i.e., prescribing, some lab-related tasks, and communication within the office), while increasing other work (i.e., charting, chronic disease and preventive care tasks, and some lab-related tasks). Thoughtful implementation and strategic workflow redesign can mitigate the disproportionate EHR-related work burden for clinicians, as well as facilitate population-based care.
CONCLUSIONS
The complex needs of the primary care clinician should be understood and considered as the next iteration of EHR systems are developed and implemented.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The use of electronic health records (EHR) is widely recommended as a means to improve the quality, safety and efficiency of US health care. Some studies point to potential EHR-related quality and safety gains due to increased adherence to guideline-based care,1,2 more complete documentation,3,4 and fewer medical errors.5,6 Efficiency gains have been shown to result from electronic ordering7,8 and from improved access to clinical information,9,10 which can reduce redundant services. Despite these potential benefits of EHR use, research has also shown variable impact of EHR use on efficiency, and thus on the workload burdens experienced by health care workers. Studies conducted in large health systems and hospital settings have documented both increased work hours for clinicians as well as more efficient delivery of clinical care, along with the unintended creation of new work and potential safety problems following EHR implementation.1,3,11–19 A systematic review of EHR impact on efficiency concluded that “the goal of decreased documentation time is not likely to be fulfilled, especially for physicians.”
Relatively little is known, however, about the impact of EHR use on work and work burdens in the smaller, unaffiliated primary care practices where most primary care is currently delivered.20–23 Additionally, there is limited data on how EHR-related work burdens are distributed among the various members of the healthcare team within these practices, with most studies focusing exclusively on the work of either physicians12,15,24 or nurses.25,26 One systematic review found EHR use to be more efficient for documentation by nurses than by physicians, but did not distinguish between types of clinical settings.10 We found no studies assessing EHR effects on the work of non-clinical staff.
Given the current emphasis on team-based care models for primary care, understanding the impact of EHR use on the work of all members of the practice team is essential for determining how new tasks, such as those associated with panel management or population-based care approaches, can best be integrated into these settings. In this paper, we report our observations of EHR use on clinician and staff workload in small, independent, community-based primary care practices.
METHODS
This analysis is part of a multi-method study, conceptually informed by The Primary Care Change Model27 and the Technology Acceptance Model,28–34 to understand how EHRs are used in small, independent primary care practices.
Seven physician-owned, single specialty primary care practices in the northeastern U.S. participated in this study. (See Table 1). Two initial practices were selected from a group of 22 practices that had participated in prior studies. Chart audit data were used to select one high performing and one lower performing practice, using a quality composite score that combined process and intermediate outcomes of chronic disease care and preventive care. Both of these first two practices had been using the same EHR system for approximately 10 years. To explore changes in work burden over the course of EHR implementation, we then included a high and low performing practice that had implemented an EHR more recently. For the rest of the sample, efforts were made to recruit practices that varied in terms of care quality and time since implementation.
Data Collection
Experienced field researchers, using observation templates and an interview guide, spent approximately 9–14 days over a 4–8 week period in each practice, observing practice members using their EHR, conducting informal and in-depth interviews, and collecting documents related to EHR implementation and use. Additionally, a multidisciplinary team of three researchers conducted a series of “patient pathways,” in which patients were followed from the beginning to the end of their visit to identify how EHR use was incorporated into the visit.35
Research team meetings were held weekly during the data collection process to guide data collection within a site, inform subsequent practice selection, and monitor data saturation. Observational field notes were typed and then read by the principal investigator at regular intervals, and audio-recorded interviews were professionally transcribed and checked for accuracy. All documents were de-identified and imported into ATLAS.ti™—a qualitative analysis software program. The Institutional Review Boards of UMDNJ-Robert Wood Johnson Medical School and Oregon Health & Science University approved this study.
Data Analysis
We used a grounded theory approach (an inductive process of identifying themes as they emerge from the data),36 which resulted in our code book of more than 50 codes. Data from two practices were read aloud and coded by an analysis group of seven investigators. Data from the remaining practices were then distributed to five group members for coding. Codes were merged into a single database and several immersion-crystallization cycles37 were conducted, in which tagged segments of text were examined to look for patterns across practices and to develop a more robust understanding of EHR use. Three consultants, with expertise in health information technology use in primary care and human factors engineering, provided consultation during the analysis process.
RESULTS
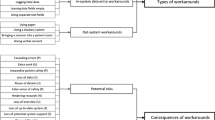
Based on our observations and reported perceptions of practice members, we found that EHR use impacted the work of practice members differently, depending on their role in the practice. Across all practices, EHR use typically reduced work burdens for both clinical and administrative support staff. In contrast, most clinicians reported that EHR use increased their work burdens, primarily by increasing the effort required for maintaining adequate clinical documentation.
Impact on Staff Work
Decreased Staff Work
EHR use in practices typically reduced work burdens for clinical and administrative staff by improving how patients are checked in and roomed, how staff document their work, and how communication occurs with patients and providers. Work burdens were reduced through improved chart availability, simultaneous chart accessibility, and improved communication.
Check-in and Rooming
One of the important sources of decreased work burden for check-in and rooming tasks involved chart availability. Many practice staff members praised their EHR for eliminating the time-consuming tasks of retrieving, filing and searching for paper charts. A nurse in Practice 2 (P2) recalled:
Literally one Wednesday a month, all personnel would systematically go through all the charts to find all the misplaced charts, as well as if there was any chart missing from sequence… [Since] we’re in computers, we no longer have to do that. Misplacing of charts [doesn’t] happen, which is a beautiful thing.
EHR use allowed staff to electronically track when patients had arrived, and to quickly find patient demographic information, problem and medication lists, immunization records, previous visit records, vital signs, as well as lab and other test results, without having to take the time to search through a paper chart.
I think it’s great… Everything’s accessible to you right there. You don’t have to go searching page by page through a folder to find what you want… Like I said, workflow got faster, a lot easier, because everything’s accessible to you. (Medical assistant in P1)
For clinical support staff with access to the EHR during the rooming process, it served as a cognitive tool to help them elicit the right patient information. As a medical assistant (MA) in Practice 7 pointed out, the use of EHR templates for data collection “helps to keep us on track.”
Staff Charting
Use of an EHR also reduced staff work burdens by allowing simultaneous chart accessibility. This feature had the greatest impact on staff charting, since staff no longer had to wait until clinicians were finished with a paper chart to complete their work. A front desk staffer in Practice 7 pointed out that this eliminated the pile-up of tasks, “so you’re not really here at the end of the day trying to go through all these paper things … that had to be charted.”
Communication
Staff reported that communicating with clinicians throughout the day via their EHR’s electronic messaging function was especially efficient and convenient. For instance, in Practice 5, we observed all practice members routinely checking their electronic in-boxes because the clinician would answer staff questions and forward requests, tasks and information to them between patient visits. The receptionist in Practice 5 emphasized the positive impact of this new way of communicating, by recalling the past:
It took more time [before we got an EHR]. You had to write everything out. You had to wait for [the clinician] in the hallway to ask him questions . . . once he would answer the message, they had to type up the telephone message and stick it onto the paper and put it in their paper chart. (P5, Front Desk, Interview)
She then contrasted it with their current process of communicating with the physician electronically through their EHR:
We communicate like this all day long . . . I like the way we just go back and forth with him [through] messages; you don’t have to constantly be searching for him. It’s quick. … He can do it between patients . . . so we never really wait real long for any kind of messages.
Use of an EHR also facilitated more efficient staff communication with patients. Because charts could be so easily accessed, staff members were often able to answer patient questions immediately and minimize callbacks.
Increased Staff Work
While EHR use typically reduced work for staff there were some instances in which EHR use created more work for staff.
Inadequate Infrastructure
Inadequate infrastructure was a common cause of additional work for staff. Examples included: limited EHR access, resulting from the purchase of too few user licenses (P1 and P2), an insufficient number of computers (P1 and P3), and use of multiple, poorly integrated software programs rather than one integrated EHR (P4). These conditions often required staff to double-document patient information, cut and paste from one program to another, and in some cases, they had to do work during their personal time to accommodate limitations on EHR access.
Limited Interconnectivity
Limited interconnectivity with other health care organizations also created additional work for staff. All practices experienced varying degrees of unreliability from the software bridges that linked the two major laboratories in the region to practices’ EHR. Faulty transmission of electronic lab results was common and in some practices (P2, P4 and P7), a staff member would cross-check all EHR data with paper-based results. Limited interconnectivity also meant that diagnostic test results, consultation letters, hospital reports, and nursing home correspondence were all transmitted to practices by mail or fax. While the incoming documents/reports themselves are not new, the new mode of information exchange and storage has created new tasks for practice staff.
Expanded MA Role
Increased work was not always negative. In Practice 6, the MA role was expanded to include a variety of panel management of chronic disease and preventive health tasks that had previously been performed by clinicians. The MA followed clear protocols to complete tasks such as populating preventive flow sheets, tracking lab results, addressing patient requests (e.g., protocol-driven lab orders and referrals), managing patient registries, contacting patients for preventive and chronic care follow-ups, and, in some cases, documenting an initial patient history at the beginning of a patient visit. While these tasks created more work for the MA, the increased responsibilities and the title of “panel manager” were a source of pride and job satisfaction.
Impact on Clinician Work
While EHR use typically reduced work burdens for administrative and clinical support staff, the impact on clinician work was more variable. For most clinicians, EHR use increased the amount and complexity of work involved in medical record keeping, had a mixed impact on work related to ordering or reviewing lab results and on chronic disease and preventive care-related tasks, and decreased work burdens relating to prescribing. All clinicians appreciated having immediate access to patient charts and the convenience of intra-office messaging.
Charting
Clinicians in all but Practice 6 reported that electronic charting was more time consuming than paper record keeping and that this extra work created longer work days, often after hours at home.
The reasons clinicians identified for this increased work burden include: poorly designed interfaces, the process of selecting diagnosis codes during each visit, and the loss of “short hand” documentation that had been used in paper charting. In addition, EHR use often created cognitive interruptions that made charting more difficult. A clinician in Practice 3 described the problem, as related to his particular EHR:
[T]he acquisition of a medical history used to be very conversational: ‘What medical problems have you had?’ ‘I’ve had heart disease all my life and I had bypass surgery and then I had two stents placed…’ [Now I have to] say, ‘Hold on, I’m just taking your medical history now.’ I [have to] close this window and open another window to get the surgical history… So the conversation flow is dictated by the chart… it creates obstacles towards documenting the information.
Additional factors that influenced charting burdens for clinicians included the reliability of access to their EHR (i.e., Internet connectivity, sufficient user licenses) and individual computer skills and typing speeds.
The clinicians in Practice 6 were the one exception to the general frustration about the extra work involved in electronic charting: they routinely completed their charts in the exam room and voiced no frustration about documentation. An important reason for the different experience of this practice is that the lead physician had invested significant effort in thinking through office work flow and work roles to optimally support the clinical process. This included expanding the MA role, as mentioned in detail above. As a result, clinicians had less documentation to do, and were afforded more time to do it.
Ordering/Reviewing Lab Tests
Ordering and reviewing lab tests contributed to the increased work burden for clinicians, since the order had to be documented in their EHR and then communicated (via paper or electronic messaging) to staff members who then entered the order into a separate system for submission to the lab. Practices had a single dedicated laboratory computer that was not located so that labs could be verbally ordered and entered by staff. There were additional inefficiencies with reviewing results. Some, but not all, laboratories returned results electronically; therefore, practices had to maintain both electronic and paper processes and clinicians often had to look in more than one place to determine whether or not they had received a lab result. There were also delays in the availability of both electronic and paper-based results due to scanning back-ups, as well as unreliability in the lab interface. In those cases where lab results were available as structured data, clinicians reported a positive effect on their workload; it allowed clinicians to view patient trends over time in one glance, thereby eliminating the need to flip through the chart to find lab data over time.
Electronic Prescribing
There was a large amount of variation in how electronic prescribing (e-prescribing) was perceived to affect clinicians’ work, with some clinicians finding that it reduced workload and others finding it more burdensome. This variation was associated with whether or not a practice had a stand-alone e-prescribing program or a program integrated into their EHR. Two practices (P1 and P4) had stand-alone e-prescribing programs, and the clinicians using these programs reported increased work, as they now had to document prescribing information into both systems. A clinician in Practice 4 explained one of the time consuming consequences of this double-documentation: “Sometimes I forget [some of the prescription information] by the time I get back to the other program.” In contrast, for the practices that used an integrated e-prescribing module (P2, P3, P5, P6 and P7), prescribing was quicker and easier. Clinicians in these practices also appreciated that information from the e-prescribing module automatically populated the medication list in the patient’s chart, and that a log of the patient’s history with the medication was created in the process.
Disease Management and Preventive Care
In general, clinicians reported that tasks involved in chronic disease management and preventive care were not well supported by their EHR, and as a result were more time consuming. One explanation for this experience was that data could not be displayed in ways that supported point of care needs. For example, information about immunizations, screening tests, labs, medications, referrals and vitals tended to be stored on separate screens. To locate and review each required that the clinician click through a series of screens that could not be opened simultaneously. In addition, alerts and prompts were either not used or noted to be distracting rather than helpful.
Two practices were notable exceptions to this issue. In one exemplary case (P5), the lead physician chose his EHR primarily because it had a summary panel that provided alerts when specific care is due. After spending considerable time customizing these alerts, he reported that they have allowed his chronic and preventive care to be more thorough and more efficient. In addition, another practice (P6) paid an outside vendor to pull patient data from their EHR and provide it in a summary sheet for each patient to prompt needed care. Clinicians at both of these practices reported less frustration with this aspect of using EHR.
DISCUSSION
Our findings suggest that EHR use affects the work of clinicians and their staff differently, with staff generally experiencing a reduction in work burden and clinicians experiencing a more variable impact. These findings have implications for EHR developers, practice leaders, and those who are invested in helping primary care practices successfully implement EHR, including vendors, regional extension agents, researchers, and policy makers.
EHR developers should focus on supporting clinician charting, disease management and ordering/reviewing tasks, as these are the main sources of increased EHR-related work burden. The differing impact of EHR on staff and clinician work likely has to do with the nature of the work performed by these two groups. Staff work is generally more routinized than clinician work, and therefore tends to be more conducive to the structured format of an electronic system. Clinician work, on the other hand, is characteristically more complex and unpredictable,38 especially in the primary care setting where the range of care is diverse, and the sources and types of information may vary widely.39 Primary care clinicians deliver acute, chronic, and preventive care, and often treat multiple health conditions in a single patient. Consequently, it is more difficult to determine how such care can be best supported by electronic systems. As EHR vendors develop new systems and the next iteration of existing systems, the complex needs of the primary care clinician should be better understood and considered.
Our findings should also be useful for practice leaders. They illuminate where suboptimal EHR implementation may be lightening the workload for some practice members and where it may be creating more work for others. Our analysis suggests that because EHR use has been particularly helpful in creating efficiencies in staff work, there may be new opportunities to redistribute work from clinicians to support staff. This finding adds support to a growing body of literature that suggests that redesigning workflow and reconceptualizing work roles to make more extensive use of clinical support staff is important for improved patient care.40–47 There is increasing recognition that a team-care approach is needed in primary care, as the physician-centric model is proving to be insufficient to manage the large burden of chronic illnesses and increasing preventive care recommendations.48–50 The limits of the physician-centric model of care may become even more apparent after small practices adopt an EHR system. Evidence from our two exemplary practices (P5 and P6) suggests that thoughtful implementation and workflow redesign can circumvent the problem of overburdening clinicians, while optimizing use of EHR as a tool to enable population-based care.
There can be, however, a variety of potential barriers to investing in workflow redesign. The most obvious is the time and resource constraints, due to the myriad of pressures often referred to as “hamster healthcare.”51,52 These pressures are intensified during the demands of EHR implementation, and without sufficient resources, practice owners often focus on minimizing the disruption to patient volume during the implementation phase. Another barrier is that recognizing the value of investing in redesign requires a systems-level orientation,53 not typical of either physician leaders or EHR vendors. When vendors do not encourage workflow redesign, they can be implicitly sending the message to practices that such an effort is not important for successful implementation. As long as workflow assessment and redesign remains absent from or peripheral to EHR implementation, practices may need other forms of external help to aid them in accomplishing this. Even longtime EHR users could benefit from such external help. As our data suggests, we cannot assume that just because a practice has been using an EHR system for many years, they are using it effectively or have implemented it optimally. One possible source of support may be the HIT extension centers.38 While extension centers vary regionally, many are conceptualized around supporting new user implementation. In our estimation, supporting meaningful use for existing users is as pressing a need as helping new users with basic implementation.
One of the limitations of our research is that our data come only from the behavior and perspectives of practice members that were working in the practice at the time of the study. This has the potential to skew our findings toward a more favorable view of EHR use, since practice members unable to adapt to EHR use may no longer be working at the practice. We learned of one employee who had been fired soon after the practice implemented an EHR because she resisted using this new tool. There is also the possibility of recall bias, since we depended on practice members’ retrospective accounts of what took place prior to our observation (i.e., recollections of the implementation process or work processes prior to EHR use, etc.) We tried to minimize this by triangulating recollections from several practice members. Our sample is small and geographically limited, thus it is not known how these findings generalize to other settings. Broad generalizability was not the purpose of this study; however, other recent research suggests our findings may indeed generalize to practices in other regions.54
The sample sufficiently highlights important areas where EHR use has affected work burden both positively and negatively, and sets up further research in small primary care practices. For instance, it would be fruitful to specifically study small practices where clinicians report that EHR use has, overall, decreased their work burden. In this way, best practices could be identified that could help to inform a set of guidelines for workflow redesign in small practices using EHR. Such guidelines could be applied in an intervention study in which practices, perhaps with the help of an external facilitator, assess current workflow and develop a tailored workflow for their particular practice to optimize EHR use. Ideally, such a process could be incorporated into the training model that vendors use in EHR implementations in small practices.
REFERENCES
Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med. 2006;144(10):742–752.
Hillestad R, Bigelow J, Bower A. Can electronic medical record systems transform health care? Potential health benefits, savings, and costs. Health Aff (Millwood). 2005;24:1103–1117.
Apkon M, Singhaviranon P. Impact of an electronic information system on physician workflow and data collection in the intensive care unit. Intensive Care Med. 2001;27(1):122–130.
Roukema J, Los R, Bleeker S, Ginneken A, Lei J, Moll H. Paper versus computer: feasibility of an electronic medical record in general pediatrics. Pediatrics. 2006;117:15–21.
Crossing the Quality Chasm: A New Health System for the 21st Century. . In: Medicine Io, ed. Washington, DC: National Academy Press; 2001.
Bates D, Gawande A. Patient safety: improving safety with information technology. N Engl J Med. 2003;348:2526–2534.
Rosenbloom ST, Talbert D, Aronsky D. Clinicians’ perceptions of clinical decision support integrated into computerized provider order entry. Int J Med Informat. 2004;73(5):433–441.
Khajouei R, Wiereng P, Hasman A, Jaspers M. Clinicians satisfaction with CPOE ease of use and effect on clinicians’ workflow, efficiency and medication safety. Int J Med Informat. 2011;80:297–309.
El-Kareh R, Gandhi TK, Poon EG, et al. Trends in primary care clinician perceptions of a new electronic health record. J Gen Intern Med. 2009;24(4):464–468.
Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc. 2005;12(5):505–516.
Koppel R, Metlay J, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;293(10):1197–1203.
Saitwal H, Feng X, Walji M, Patel V, Zhanga J. Assessing performance of an Electronic Health Record (EHR) using Cognitive Task Analysis. Int J Med Informat. 2010;79:501–506.
Campbell E, Sittig D, Ash J, Guappone K, Dykstra R. Types of unintended consequences related to computerized provider order entry. J Am Med Informat Assoc. 2006;13(5):547–556.
Ash J, Sittig D, Poon E, Guappone K, Campbell E, Dykstra R. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Informat Assoc. 2007;14(4):415–423.
Samaan ZM, Klein MD, Mansour ME, DeWitt TG. The impact of the electronic health record on an academic pediatric primary care center. J Ambul Care Manage. 2009;32(3):180–187.
McAlearney A, Robbins J, Hirschd A, Jorina M, Harropa J. Perceived efficiency impacts following electronic health record implementation: an exploratory study of an urban community health center network. Int J Med Informat. 2010;79:807–816.
Pizziferri L, Kittler AF, Volk LA, et al. Primary care physician time utilization before and after implementation of an electronic health record: a time-motion study. J Biomed Inform. 2005;38(3):176–188.
Lo H, Newmark L, Yoon C, et al. Electronic health records in specialty care: a time-motion study. J Am Med Informat Assoc. 2007;14(5):609–615.
Daniel G, Ewen E, Willey V, Reese C, Shirazi F, Malone D. Efficiency and economic benefits of a payer-based electronic health record in an emergency department. Acad Emerg Med. 2010;17(8):824–833.
Miller R, Sim I, Newman J. Electronic medical records: Lessons from small physician practices. California HealthCare Foundation. 2003:1–27.
Simon SR, Kaushal R, Cleary PD, et al. Physicians and electronic health records: a statewide survey. Arch Intern Med. 2007;167(5):507–512.
Torda P, Han ES, Scholle SH. Easing the adoption and use of electronic health records in small practices. Health Aff (Millwood). 2010;29(4):668–675.
Ross S, Schilling L, Fernald D, Davidson A, West D. Health information exchange in small-to-medium sized family medicine practices: motivators, barriers, and potential facilitators of adoption. Int J Med Informat. 2010;79:123–129.
Overhage J, Perkins S, Tierney W, McDonald C. Controlled trial of direct physician order entry: effects on physicians’ time utilization in ambulatory primary care internal medicine practices. J Am Med Informat Assoc. 2001;14(4):361–371.
DesRoches C, Donelan K, Buerhaus P, Zhonghe L. Registered nurses’ use of electronic health records: findings from a national survey. Medscape J Med. 2008;10(7):164.
LaDuke S. Online nursing documentation: finding a middle ground. JONA. 2001;31(6):283–286.
Cohen D, McDaniel R, Crabtree B. A practice change model for quality improvement in primary care practice. J Healthc Manag. 2004;49(3):155–168.
Davis F. Perceived usefulness, perceived ease of use, and user acceptance of information technologies. MIS Q. 1989;13(3):319–340.
Davis F, Bagozzi P, Warshaw P. User acceptance of computer technology: a comparison of two theoretical models. Manag Sci. 1989;35(8):982–1003.
Venkatesh V, Davis F. A model of the antecedents of perceived ease of use: development and test. Decis Sci. 1996;27(3):451–481.
Venkatesh V, Davis F. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag Sci. 2000;46(2):186–204.
Venkatesh V, Morris M. Why do not men ever stop to ask for directions? General, social influence and their role in technology acceptance and usage behavior. MIS Q. 2000;24(1):115–139.
Venkash V, Morris M, Davis G, Davis F, Venkatesh VMM, Davis G, Davis F. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–478.
Holden R, Karsh B. The technology acceptance model: its past and its future in health care. 2010. 2010;43(1):159-172.
Pommerenke F, Dietrich A. Improving and maintaining preventive services. Part I: applying the patient path model. J Fam Pract. 1992;34(1):86–91.
Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. Newbury Park: Sage; 1990.
Borkan J. Immersion/Crystallization. In: Crabtree, B and Miller, W, eds. Doing Qualitative Research 2nd ed; 1999.
Amatayakul M. Why workflow redesign alone is not enough for EHR success Healthcare Financial Management 2011(March):130–132.
Beasley J, Wetterneck T, Temte J, et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Pract. 2011;24:745–751.
Chesluk BJ, Holmboe ES. How teams work—or don’t–in primary care: a field study on internal medicine practices. Health Aff (Millwood). 2010;29(5):874–879.
Nelson BA, Massey R. Implementing an electronic change-of-shift report using transforming care at the bedside processes and methods. J Nurs Adm. 2010;40(4):162–168.
Sinsky CA, Sinsky TA, Althaus D, Tranel J, Thiltgen M. Practice profile. ‘Core teams’: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Aff (Millwood). 2010;29(5):966–968.
Nutting P, Crabtree B, Miller W, Stewart E, Stange K, Jaen C. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the national demonstration project. Ann Fam Med. 2010;8(supp 1):S45–S56.
Crosson J, Etz R, Wu S, Straus S, Eisenman D, Bell D. Meaningful use of electronic prescribing in 5 exemplar primary care practices. Ann Fam Med. 2011;9(5):392–397.
Karsh B-T. Clinical practice improvement and redesign: how change in workflow can be supported by clinical decision support. AHRQ Publication 2009;No. 09-0054-EF.
Campbell E, Guappone K, Sittig D, Dykstra R, Ash J. Computerized provider order entry adoption: implications for clinical workflow. J Gen Intern Med. 2008;24(1):21–26.
Aarts J, Ash J, Berg M. Extending the understanding of computerized physician order entry: implications for professional collaboration, workflow and quality of care. Int J Med Informat. 2007;76S:S4–S13.
Bodenheimer T, Laing BY. The teamlet model of primary care. Ann Fam Med. 2007;5(5):457–461.
Ferrer RL, Mody-Bailey P, Jaen CR, Gott S, Araujo S. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7(6):504–512.
Yarnall KS, Pollak KI, Ostbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Public Health. 2003;93(4):635–641.
Morrison I, Smith R. Hamster health care: time to stop running faster and redesign health care. BMJ. 2000;321:1541–1542.
Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? J Am Med Informat Assoc. 2004;291(10):1246–1251.
Carayon P, Hundt A, Karsh B, Gurses A, Alvarado C, Smith M. Work system design for patient safety: the SEIPS model. Qual Saf Health Care. 2006;15(Supp I):i50–i58.
Lapin J, Beasley J, Smith P, al. e. Proactive risk assessment of primary care of the elderly. ARHQ Conference. Bethesda, MD2008.
Funding
This work was supported by a grant from the National Heart, Lung and Blood Institute (R21HL092046).
Conflict of Interest
Elizabeth C. Clark: Demissie K, PI; Clark EC, co-investigator. “Long term medication adherence in renal transplant patients.” Novartis Pharmaceuticals. 2011–2012; annual direct costs: $72,000. Benjamin F. Crabtree: royalties from Sage Publications, Inc. for edited book, Doing Qualitative Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Howard, J., Clark, E.C., Friedman, A. et al. Electronic Health Record Impact on Work Burden in Small, Unaffiliated, Community-Based Primary Care Practices. J GEN INTERN MED 28, 107–113 (2013). https://doi.org/10.1007/s11606-012-2192-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2192-4