ABSTRACT
BACKGROUND
Despite new treatment therapies and the emphasis on patient activation, nearly 50 % of diabetes patients have hemoglobin A1c levels above target. Understanding the impact of unmet treatment goals on the physician-patient relationship is important for maintaining quality care in clinical practice.
OBJECTIVE
To explore physicians’ and type 2 diabetes patients’ views of patients’ difficulty achieving diabetes treatment goals.
DESIGN
Qualitative study using in-depth interviews with a semi-structured interview guide.
PARTICIPANTS
Nineteen endocrinologists and primary care physicians and 34 patients diagnosed with type 2 diabetes at least two years prior.
MAIN MEASURES
In-depth interviews with physicians and patients. A multidisciplinary research team performed content and thematic analyses.
KEY RESULTS
Qualitative analysis revealed two main findings, organized by physician and patient perspectives. Physician Perspective: Physicians’ Perceived Responsibility for Patients’ Difficulty Achieving Treatment Goals: Physicians assumed responsibility for their patients not achieving goals and expressed concern that they may not be doing enough to help their patients achieve treatment goals. Physicians’ Perceptions of Patients’ Reactions: Most speculated that their patients may feel guilt, frustration, or disappointment when not reaching goals. Physicians also felt that many patients did not fully understand the consequences of diabetes. Patient Perspective: Patients’ Self-Blame for Difficulty Achieving Treatment Goals: Patients attributed unmet treatment goals to their inability to carry out self-care recommendations. Most patients blamed themselves for their lack of progress and directed their frustration and disappointment inwardly through self-deprecating comments. Patients’ Perceptions of Physicians’ Reactions: Several patients did not know how their physician felt, while others speculated that their physicians might feel disappointed or frustrated.
CONCLUSIONS
Physicians’ perceived responsibility and patients’ self-blame for difficulty achieving treatment goals may serve as barriers to an effective relationship. Physicians and patients may benefit from a greater understanding of each other’s frustrations and challenges in diabetes management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this age of expensive health care costs and severe cost-cutting efforts,1–3 an efficient and effective physician-patient relationship is paramount in the treatment of type 2 diabetes.4–10 Effective physician-patient collaboration entails a sustained working relationship8,11/secure attachment,12,13 shared goals,8 a mutual understanding of respective tasks and roles,6,9,10,14 and a bond characterized by liking, trust, and confidence.8,11,14 Patient-centered medicine promotes this paradigm of collaborative management,8,15–17 demonstrating its significance via optimal medical outcomes in diabetes and other chronic diseases.7,18–20
In diabetes, a collaborative physician-patient relationship is associated with increased self-efficacy, improved attitudes towards the impact of diabetes on quality of life, decreased negative attitudes towards living with diabetes, and improved glycemic control.21–23 Yet little is known about the impact of the physician-patient relationship on diabetes management. Diabetes patients face complex self-care prescriptions, including weight reduction, increased physical activity, diabetes nutrition guidelines, oral and/or insulin medication regimens, and frequent blood glucose monitoring. These behaviors are critically linked to improved glycemic control24–26; however, patients often struggle to integrate these behaviors into their daily lives.27–30 In fact, nearly one half of diabetes patients have hemoglobin A1c levels above target.31 Frustration to meet recommended glycemic and behavioral goals may be reflected in new or existing emotional difficulties that further hamper patients’ efforts to manage diabetes.27,32–38 Similarly, physicians are often frustrated by patients’ difficulties integrating self-care into their lifestyles.39–41 Thus, understanding patients’ struggle to achieve treatment goals and physicians’ responses to patients who are struggling to integrate self-care into their lifestyles is important for understanding the physician-patient relationship in type 2 diabetes.
The overall purpose of this qualitative study was to explore physicians’ and type 2 diabetes patients’ perceptions, attitudes and behaviors that support or impede the physician-patient relationship in type 2 diabetes treatment. In this paper we focused on patients’ struggles to achieve treatment goals and how physicians’ respond to patients who are not reaching goals.
RESEARCH DESIGN AND METHODOLOGY
Research Design
We conducted in-depth face-to-face interviews with type 2 diabetes patients and physicians (endocrinologists and primary care physicians) who treat patients with type 2 diabetes. In-depth interviewing is a qualitative technique involving intensive one-on-one interviews with a small number of participants.42
Sample
We employed criterion sampling,43 a form of purposive sampling, to recruit participants: 1) English-speaking endocrinologists and primary care physicians with at least 5 % of their practice consisting of patients with type 2 diabetes in order to ensure experience treating patients with diabetes; and 2) English-speaking patients, aged 30–70 years, diagnosed with type 2 diabetes for at least two years with a hemoglobin A1c (A1C) <14.0 %, and no diagnosis of cognitive impairment, severe visual impairment, or severe psychopathology. We recruited patients 1) between the ages of 30–70 to ensure a diagnosis occurred during adulthood, and 2) who received treatment in an adult diabetes clinic, not pediatric or geriatric clinics. Physicians were recruited via telephone, emails, and letters to Boston area hospitals, clinics, and practices, and patients via direct mailings, advertisements, and flyers in Boston area hospitals and clinics. Specifically, we recruited ten endocrinologists practicing in diabetes clinics, four endocrinologists in private practice, and five primary care physicians practicing in the general community. We recruited ten patients with A1C < 7.0 %, eight patients with A1C levels between 7.0 % and 8.0 %, and 16 patients with A1C > 8.0 % to provide perspectives of patients throughout the range of glycemic control. The Joslin Diabetes Center Committee on Human Subjects approved the study. All physicians and patients provided informed written consent prior to participation.
Data Collection
A multidisciplinary research team devised and field-tested a semi-structured interview guide. A clinical psychologist and a health psychologist, two experienced interviewers, asked physicians and patients broad, open-ended questions about factors impeding the achievement of treatment goals (Appendix). Both were asked about reasons for not achieving treatment goals (e.g., glycemia, blood pressure, cholesterol, and weight targets) and how they felt when goals were not met. Interviewers used directive probes to elicit additional information and clarify questions; interviewers also wrote field notes to capture key points and observations from the interviews. Interviews were conducted at Boston area hospitals, clinics, and practices, and lasted 30–60 minutes. All interviews were digitally audio-recorded and transcribed. We performed quality checks of the transcribed files while listening to the interview recordings to validate the transcriptions. Names and identifiers were removed to protect physician and patient confidentiality. Data were collected until saturation was reached; that is until no new information was generated from the interviews.44 In our study, no new information was generated after interviewing 14 endocrinologists and 5 primary care physicians and 20 endocrinologist patients and 14 primary care patients.
Data Analysis
The multidisciplinary research team, consisting of two health psychologists, a clinical psychologist, an endocrinologist, and two research assistants, used standard qualitative methods to perform content analysis by independently marking and categorizing key words, phrases, and texts to identify themes.45–47 The research team met weekly over the course of a year to code the data; discrepancies were reviewed, discussed, and resolved through consensus. After the transcripts were coded and reviewed, one member of the research team entered the coded transcripts in NVivo 8 software.48
To support credibility (validity), we triangulated data sources and investigators.49,50 Using a multidisciplinary data analyst strategy we converged multiple data sources, including in-depth interviews, participant observation (e.g., participant affect, behaviors) and field notes (i.e., written accounts of what happened during interviews) to verify the consistency of our findings. To support dependability (reliability) of the data, we tracked the decision-making process using an audit trail.49,50 The audit trail is a detailed description of the research steps conducted from the development of the project to the presentation of findings.
RESULTS
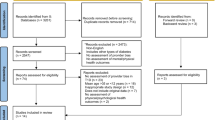
Nineteen physicians and thirty-four type 2 diabetes patients participated (Table 1). Qualitative analysis of physicians’ and patients’ responses, from separate interviews, revealed two main findings, organized by physician and patient perspectives.
Physician Perspective
Physicians’ Perceived Responsibility for Patients’ Difficulty Achieving Treatment Goals
Physicians described a self-reflective approach to interacting with patients who were struggling to achieve treatment goals. When patients were not meeting medical treatment goals, many physicians directed questions inwardly and asked themselves what more they could be doing to assist their patients:
“Have you gotten to know the patient? Have you really addressed the issues at hand? Have you had enough time, given the patient enough time to work on this? Have you provided the resources? Have you clearly identified what the challenges and issues are so that the patient can work on it? Have you communicated specific enough goals that patients can reach, can work towards?”
Through this self-reflective approach, physicians described how their own barriers in the treatment relationship, including communication difficulties (e.g., language barriers, explaining treatment recommendations, not following up with the patient), time constraints during medical visits, and treatment-related expectations, contributed to patients’ poor clinical outcomes:
“My main thing that I think I lack is reaching out to people frequently enough because we’re not well set up to do that. If someone [patient] goes, then they just go. And I think it’s an odd thing that you just send them out the door…I would like to track those people better. I could make note of them, I could call them, but I don’t do that...”
“I think that what we ask patients to do is hard and it’s continuous. I think that, that in and of itself, leads to expectations that are difficult to buy into. Somebody recognizes that they need to lose 50 pounds, that’s insurmountable. …I think that the failures largely are due to [providers] setting expectations that are insurmountable.”
Physicians openly assumed responsibility for their patients not achieving treatment goals: “Maybe…I’m not really figuring out what their problem is. Maybe I’m missing something. Maybe it’s because I’m rushed and I have patients to see—I don’t have enough time to spend with them.” Interestingly, physicians’ self-reflection often manifested itself in disparaging comments about their own performance. These physicians appeared to set very high standards for themselves and expressed concern when they felt they were not doing enough to help their patients achieve treatment goals:
“We all feel a little bit of failure I suppose if we haven’t done whatever’s necessary to get that person better.”
“I know that I probably fail more often than I think I do, because everyone thinks that they’re doing the right thing.”
Physicians were aware of patients struggling to achieve treatment goals; however, many expressed uncertainty for how to best help their patients or how to improve the care that they provided:
“I think sometimes we don’t really understand why what we’re saying is not making sense to them. I have a [patient] who for the life of me, I can’t get him into keep his appointments. He went blind before he would get his cataracts taken care of…But he’s still not taking care of his diabetes…Some would say it’s his fault, but it’s my fault too. I don’t know what else to do. I don’t know what question to ask in terms of saying, how am I not being helpful?”
Feeling as though they were not making an impact on their patients’ treatment, many physicians expressed feelings of inadequacy, frustration, and fatigue:
“You get very tired at the end of the day. I think it really exhausts your physical and mental energy because you want to try and stay positive and encouraging, that’s sort of how I try to do things. But nevertheless at the end of the day you really sort of wonder, why am I not accomplishing more? And, why am I doing this?”
Physicians’ Perceptions of Patients’ Reactions
In response to a question about patients’ responses to difficulty achieving treatment goals, physicians stressed that patients’ responses to not achieving treatment goals depended on the individual person and the goals being set. Two physicians stated that they did not know how their patients felt, while most speculated that their patients may feel guilt, frustration, or disappointment when not reaching treatment goals:
“Frustrated, disappointed. I think there are truly some who don’t care. Although there’s a whole population that won’t even come. Some just float away and don’t come to the appointments at all. So it’s a spectrum.”
“It depends on the patient. The ones who are motivated, it bothers them tremendously because those are often the folks who are putting in a fair amount of effort. So they unfortunately feel like failures as opposed to the fact that they’re just failing to control their blood sugar. The ones who are not motivated, I think that they’re bothered that they’re not hitting the goal, but I don’t think that they feel the same sort of failure…they’re not equating themselves with their diabetes control.”
Further, some physicians thought that many patients did not take their diabetes seriously because patients may not fully understand the consequences of diabetes. These physicians explained that their patients may not be concerned because they had not yet experienced the negative consequences of poor glycemic control:
“I think it depends on how they’re not meeting their goals. When blood sugars are modestly elevated people don’t necessarily feel terrible, and therefore when you’re not meeting the goals, some cannot appreciate the consequences that are not more immediate.”
Lastly, two physicians speculated that not reaching goals may result in patients assuming they were disappointing their doctors:
“If they show up [to an appointment], they feel better. If they feel bad, [it’s] probably because of the relationship that we’ve had and the patient hates to disappoint us.”
“Part of it [not reaching goals] is they want to please the doctor more than they’re necessarily worried about the specific goals to them.”
Patient Perspective
Patients’ Self-Blame for Difficulty Achieving Treatment Goals
During the interviews, patients were asked about their struggles reaching treatment goals. Thirty-three of the 34 patients described difficulty not achieving treatment targets regardless of their A1C levels. Most of these patients assumed responsibility for unmet treatment goals and expressed a sense of personal failure for their perceived lack of progress:
“When I come to see my doctor and she tells me that, ‘You’re doing good on this aspect, but you’re not doing good on that aspect,’ I feel kind of bad because when I come in I want a clean record…I’m failing myself, I’m not failing them, I’m failing myself.”
“When I see the high numbers I feel lousy. I feel frustrated with myself, I feel that it’s my fault because I keep looking at the pieces I can do, like the exercise and the food, and saying well you’re not doing those things that you know.”
Patients attributed their difficulty achieving treatment goals to an inability to carry out medical self-care recommendations: “I’m a relatively smart person…it does not make sense for me to eat incorrectly. It does not make sense for me not to exercise properly…I’m making these bad choices.” Further, patients frequently expressed frustration and disappointment in their struggles to follow recommended self-care regimens. Most blamed themselves for “not doing what they should be doing” in their self-care. These patients directed their frustration and disappointment inwardly through self-deprecating comments:
“How do I feel? Discouraged. And I ask myself, ‘Why can’t I do it?’ And, often the time comes when you’ll say I’m lazy. I don’t want to give up what I like. And that’s selfishness also. And that’s the reason I think that I can’t reach it. It’s because I’m lazy and I’m selfish.”
“Because I think I’m such a bad patient. I think they do a great job. I think…the people in this building every time I talk to them they try to help…It’s me that’s the problem, not them.”
Difficulty managing diabetes appeared to take an emotional toll on the patients. Patients described feeling defeated and depressed in response to unmet treatment goals:
“I think you just give up. That’s what it is. It’s such a baffling disease. You think you’re doing fine and you take your sugar and it’s, ‘What’s going on here?’ And so you just give up.”
“I feel depressed, I feel that I can’t accomplish [anything]. When I strive for something and I can’t do it, I become bitter, not only with myself but my surroundings. I don’t blame it on others, but I blame it on myself ‘What did I do wrong that I did not reach my goal?’”
Several patients felt that they could never do enough to manage their diabetes successfully. This sense of hopelessness was characterized by an increased vulnerability to the progressive course of their disease and constant struggles with food and weight:
“I don’t see too much success because I think it gets progressively worse. It’s depressing in the fact that you have to eat next to nothing and then when you eat next to nothing it’s [blood glucose] high. I wish I could get a little more success out of it. I feel like I’m always going backwards.”
“For instance with the weight, that is something that has always made me lose my hope…Right now, instead of losing weight, and I have been eating less, I am gaining…I don’t know if it is the medicine, but that sort of has me a little depressed…I just feel sad. Sometimes I don’t even want to take the medicine because I feel like it’s not doing anything.”
Patients’ Perceptions of Physicians’ Reactions to Unmet Goals
When asked how their physicians might feel when treatment goals were not being met, several patients seemed surprised by the question. These patients said that they did not know how their physicians felt or did not feel comfortable answering for their physicians: “Well I can’t really answer for my doctors. I would imagine they would probably think that I could work harder at it. But you would probably need to ask them how they would feel about it.” Further, these patients explained that their physicians did not express any reactions during the medical visit: “I have absolutely no idea how he feels…not that I’ve never thought about it, I’ve just never seen any expression of how he feels.”
Many patients speculated that their physicians might feel disappointed or frustrated when patients are not achieving treatment goals:
“I think she feels like she’s losing part of the battle. It’s not her, it’s me. It’s nothing against her, because I think she’s the greatest doctor…It must be discouraging for her to look at somebody like myself that can do it and does it, then doesn’t do it.”
“It’s got to be discouraging for him because he’s telling me to do something and he’s asking me to give a hundred percent where he’s giving a hundred percent, and when I don’t do that I think it’s got to be discouraging…He won’t ever show me.”
Importantly, several patients described supportive reactions from their physicians. Patients noted that their physicians’ approached unmet goals with a positive attitude to help steer patients back on track:
“He just sort of says, ‘Well, how’d you do on this?’ He can tell by the numbers how I did, but he’s asking how I felt I did and he usually is very good in the way he says, ‘So do you think you can increase the incline on the treadmill? Do you think you can handle that?’ Then he’ll write up the prescribed thing for the next six months so we come to an agreement.”
DISCUSSION
In our qualitative study of physicians’ and type 2 diabetes patients’ views of patients’ difficulty achieving treatment goals, both physicians and patients assumed responsibility for poor clinical outcomes. Physicians acknowledged how their own communication difficulties, time constraints during medical visits, and unrealistic expectations contributed to patients’ unmet goals. Further, several physicians described feeling inadequate, frustrated, and fatigued when they were not making an impact on their patients’ treatment. Patients attributed their difficulty achieving treatment goals to an inability to follow self-care recommendations. Most patients blamed themselves for their lack of progress and directed their frustration and disappointment inwardly through self-deprecating comments. Like the physicians, patients described an emotional toll from managing the day-to-day tasks of diabetes. Many patients described feeling depressed and defeated when not achieving recommended goals. Importantly, both physicians and patients were asked how the other might feel when treatment goals were not being met. Some physicians and patients said they did not know how the other person felt. Others speculated they may be frustrated or disappointed, but neither the physicians nor the patients seemed to recognize that the other person felt responsible for unmet treatment goals.
While physiologic factors can contribute to patients’ inability to achieve treatment goals, difficulties maintaining the rigors of recommended self-care and psychosocial factors may also be important. Thus, an important challenge is not only to identify barriers to successful diabetes care but also to understand why they occur in order to develop successful clinical approaches that will help patients follow their treatment prescription and improve glycemia. Self-blame is not a new concept in chronic disease management.51–57 Self-blame may be an unintended consequence of the emphasis on patients’ increased involvement in chronic disease management and their accepting greater responsibility for self-care. For patients with chronic conditions other than diabetes, self-blame is associated with poor psychological adjustment, depressive symptoms, and ineffectual coping.53,56–58 In diabetes, self-blame may result from challenges managing the complex self-care regimen along with the potential for poor treatment outcomes, which can amplify a sense of failure and lead to self-blame.54,59 In our study, patients described feeling a sense of personal failure when not achieving treatment goals. Difficulty managing the complex tasks of diabetes left patients feeling defeated and depressed. This finding is particularly important because patients with diabetes are at a higher risk for depression compared to the general population60–62 and depression further complicates diabetes self-care.61,63 We hypothesize that patient self-blame for difficulty achieving treatment goals may lead to or exacerbate distress and/or depressive symptoms. This hypothesis needs to be tested with more refined quantitative measures in patients with different ethnic, cultural or socioeconomic backgrounds.
For many physicians, helping patients achieve optimal blood glucose control remains a challenging and often unattainable goal despite an abundance of new medications and treatment options. Thus physicians may assume responsibility for patients’ difficulty achieving treatment goals. In our study, physicians felt they may not be doing enough to help their patients and/or did not know how to best help their patients. Whether physicians set too high expectations for themselves and for their patients is not clear. Further, when physicians felt they were not making an impact on their patients’ treatment, they described feeling inadequate, frustrated, and fatigued. These feelings may be indicative of physician burnout, which is a serious problem in medicine.64–66 Quantitative research should examine the hypothesized association between physicians’ perceived inadequacy, frustration, fatigue and burnout.
Interestingly, our findings indicate that neither physicians nor patients seemed to recognize that the other person felt responsible for unmet treatment goals, which may indicate communication problems and/or non-collaboration in the physician-patient relationship. Alternatively, physicians’ perceived responsibility and patients’ self-blame also suggest both physicians and patients care about achieving treatment goals and often feel responsible or at fault when these goals are not met. Clinicians are well positioned to encourage and support patients who are not achieving treatment goals, which may help patients feel more motivated and empowered to integrate self-care recommendations into their lifestyle and feel less self-blame. The use of a team approach in diabetes care provides additional support and resources for physicians,67 thus helping physicians feel less overwhelmed and less responsible for unmet treatment goals.
Study limitations include the relatively homogenous sample from one city in the northeastern United States. Participating physicians and patients volunteered to be interviewed, and thus may have been more willing or motivated to discuss difficulties achieving treatment goals in the context of the physician-patient relationship. Additionally, we acknowledge that endocrinologists’ and primary care physicians’ views of patients’ difficulty achieving treatment goals may differ and warrants further study. We did not interview matched physician-patient pairs. Future research could incorporate quantitative measures with matched physician-patient pairs to assess why patients struggle to achieve treatment goals and how physicians respond to patients struggling to integrate self-care into their lifestyles. Lastly, the findings from this study, as with all qualitative research, are exploratory and should be considered hypotheses. Quantitative research with a larger, more heterogeneous sample needs to examine these hypotheses and their impact on the physician-patient relationship in diabetes treatment.
In conclusion, exploring physicians’ and patients’ responses to patients’ difficulty achieving treatment goals represents an incremental step towards improving the understanding of the physician-patient relationship in type 2 diabetes. Our findings indicate that physician-patient corroboration may depend on individual physician and patient factors. Investigations to develop methods and training for patients to address psychosocial issues (e.g., self-blame, emotional distress) with their physicians may promote greater corroboration. Resources are also needed to assist physicians when experiencing feelings of inadequacy, frustration, and fatigue because they may be signs of burnout. Lastly, our findings shed light on the importance of physicians stressing to their patients that difficulty achieving diabetes treatment goals is not about fault or blame. Physicians should discuss with their patients the progressive course of diabetes and the multiple causes for how and why diabetes management is challenging. Further, both physicians and patients may benefit from a greater understanding of the multiple frustrations and challenges in diabetes management. Identifying self-care challenges together during a medical visit may help physicians and patients collaborate on diabetes management to avoid barriers to achieving treatment goals.
REFERENCES
American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008;31(3):596-615.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25.
Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med. 2006;12(1):62–6.
Campbell C, McGauley G. Doctor-patient relationships in chronic illness: insights from forensic psychiatry. BMJ. 2005;330(7492):667–70.
Piette JD, Schillinger D, Potter MB, Heisler M. Dimensions of patient-provider communication and diabetes self-care in an ethnically diverse population. J Gen Intern Med. 2003;18(8):624–33.
Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18(11):893–902.
Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–27.
Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127(12):1097–102.
Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17(4):243–52.
Street RL Jr, Krupat E, Bell RA, Kravitz RL, Haidet P. Beliefs about control in the physician-patient relationship: effect on communication in medical encounters. J Gen Intern Med. 2003;18(8):609–16.
Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice. 1979;26(3):252–60.
Ciechanowski PS, Katon WJ, Russo JE, Walker EA. The patient-provider relationship: attachment theory and adherence to treatment in diabetes. Am J Psychiatry. 2001;158(1):29–35.
Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med. 2004;66(5):720–8.
Jahng KH, Martin LR, Golin CE, DiMatteo MR. Preferences for medical collaboration: patient-physician congruence and patient outcomes. Patient Educ Couns. 2005;57(3):308–14.
Glasgow RE, Anderson RM. In diabetes care, moving from compliance to adherence is not enough. Something entirely different is needed. Diabetes Care. 1999;22(12):2090–2.
Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26(4):597–604.
Clark NM, Gong M. Management of chronic disease by practitioners and patients: are we teaching the wrong things? BMJ. 2000;320(7234):572–5.
Fuertes JN, Mislowack A, Bennett J, et al. The physician-patient working alliance. Patient Educ Couns. 2007;66(1):29–36.
Escudero-Carretero MJ, Prieto-Rodriguez MA, Fernandez-Fernandez I, March-Cerda JC. Physician/patient relationship in diabetes mellitus type 1 treatment. A qualitative study. Aten Primaria. 2006;38(1):8–15.
Gavin LA, Wamboldt MZ, Sorokin N, Levy SY, Wamboldt FS. Treatment alliance and its association with family functioning, adherence, and medical outcome in adolescents with severe, chronic asthma. J Pediatr Psychol. 1999;24(4):355–65.
Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21(10):1644–51.
Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995;18(7):943–9.
Greenfield S, Kaplan SH, Ware JE Jr, Yano EM, Frank HJ. Patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3(5):448–57.
Conn VS, Hafdahl AR, Mehr DR, Lemaster JW, Brown SA, Nielsen PJ. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia. 2007;50(5):913–21.
Karter AJ, Ackerson LM, Darbinian JA, et al. Self-monitoring of blood glucose levels and glycemic control: the Northern California Kaiser Permanente Diabetes registry*. Am J Med. 2001;111(1):1–9.
Pi-Sunyer FX, Maggio CA, McCarron DA, et al. Multicenter randomized trial of a comprehensive prepared meal program in type 2 diabetes. Diabetes Care. 1999;22(2):191–7.
Weinger K. Psychosocial issues and self-care. Am J Nurs. 2007;107(6 Suppl):34–8. quiz 38.
Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22(10):1379–85.
Rubin RR, M P. Psychological issues and treatment for people with diabetes. J Clin Psychol. 2001;57(4):457–78.
Wdowik MJ, Kendall PA, Harris MA. College students with diabetes: using focus groups and interviews to determine psychosocial issues and barriers to control. Diabetes Educ. 1997;23(5):558–62.
Hoerger TJ, Segel JE, Gregg EW, Saaddine JB. Is glycemic control improving in U.S. adults? Diabetes Care. 2008;31(1):81–6.
Welch GW, Jacobson AM, Polonsky WH. The Problem Areas in Diabetes Scale. An evaluation of its clinical utility. Diabetes Care. 1997;20(5):760–6.
Lloyd CE, Smith J, Weinger K. Stress and diabetes: a review of the links. Diabetes Spectrum. 2005;18(2):121–7.
Weinger K, Jacobson AM. Psychosocial and quality of life correlates of glycemic control during intensive treatment of type 1 diabetes. Patient Educ Couns. 2001;42(2):123–31.
Albright TL, Parchman M, Burge SK. Predictors of self-care behavior in adults with type 2 diabetes: an RRNeST study. Fam Med. 2001;33(5):354–60.
Gonzalez JS, Delahanty LM, Safren SA, Meigs JB, Grant RW. Differentiating symptoms of depression from diabetes-specific distress: relationships with self-care in type 2 diabetes. Diabetologia. 2008;51(10):1822–5.
Gonzalez JS, Safren SA, Cagliero E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30(9):2222–7.
Gonzalez JS, Safren SA, Delahanty LM, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25(9):1102–7.
Crosson JC, Heisler M, Subramanian U, et al. Physicians' perceptions of barriers to cardiovascular disease risk factor control among patients with diabetes: results from the translating research into action for diabetes (TRIAD) study. J Am Board Fam Med. 2010;23(2):171–8.
Wens J, Vermeire E, Royen PV, Sabbe B, Denekens J. GPs' perspectives of type 2 diabetes patients' adherence to treatment: a qualitative analysis of barriers and solutions. BMC Fam Pract. 2005;6(1):20.
Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients' and physicians' different view of the disease. J Fam Pract. 2000;49(6):507–12.
Patton MQ. How to use Qualitative Methods in Evaluation. London: Sage; 1987.
Patton M. Qualitative Evaluation and Research Methods. 2nd ed. Newbury Park: Sage; 1990.
Morse J, Field P. Qualitative Research Methods for Health Profesionals. 2nd ed. Thousand Oaks, CA: Sage Publications; 1995.
Pope C, Mays N. Qualitative Research in Health Care. 2nd ed. London: BMJ Books; 2000.
Krippendorf K. Content Analysis: An Introduction to Its Methodology. 2nd ed. Thousand Oaks, CA: Sage Publications; 2004.
Neuendorf K. The Content Analysis Guidebook. Thousands Oaks, CA: Sage Publications; 2002.
NVivo [computer program]. Version 8. Victoria, Australia: QSR International.
Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. Thousand Oaks, California: SAGE Publications, Inc.; 1994.
Russell CK, Gregory DM. Evaluation of qualitative research studies. Evid Based Nurs. 2003;6(2):36–40.
Bennett KK, Compas BE, Beckjord E, Glinder JG. Self-blame and distress among women with newly diagnosed breast cancer. J Behav Med. 2005;28(4):313–23.
Eccleston C, Williams AC, Rogers WS. Patients' and professionals' understandings of the causes of chronic pain: blame, responsibility and identity protection. Soc Sci Med. 1997;45(5):699–709.
Friedman LC, Romero C, Elledge R, et al. Attribution of blame, self-forgiving attitude and psychological adjustment in women with breast cancer. J Behav Med. 2007;30(4):351–7.
Peel E, Parry O, Douglas M, Lawton J. Blood glucose self-monitoring in non-insulin-treated type 2 diabetes: a qualitative study of patients' perspectives. Br J Gen Pract. 2004;54(500):183–8.
Scambler G. Health-related stigma. Sociol Health Illn. 2009;31(3):441–55.
Tuncay T, Musabak I, Gok DE, Kutlu M. The relationship between anxiety, coping strategies and characteristics of patients with diabetes. Health Qual Life Outcomes. 2008;6:79.
Voth J, Sirois FM. The role of self-blame and responsibility in adjustment to inflammatory bowel disease. Rehabil Psychol. 2009;54(1):99–108.
Glinder JG, Compas BE. Self-blame attributions in women with newly diagnosed breast cancer: a prospective study of psychological adjustment. Health Psychol. 1999;18(5):475–81.
Rayman K. GE. Home alone: the experience of women with type 2 diabetes who are new to intensive control. Health Care for Women International. 2004;25:900–15.
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–78.
Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27(4):914–20.
Gonzalez JS, Peyrot M, McCarl LA, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31(12):2398–403.
Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25(4):246–52.
Dyrbye LN, Massie FS Jr, Eacker A, et al. Relationship between burnout and professional conduct and attitudes among US medical students. JAMA. 2010;304(11):1173–80.
Shanafelt TD, Bradley KA, Wipf JE, Back AL. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–67.
Thomas NK. Resident burnout. JAMA. 2004;292(23):2880–9.
Ritholz MD, Beverly EA, Abrahamson MJ, Brooks KM, Hultgren BA, Weinger K. Physicians' Perceptions of the Type 2 diabetes multidisciplinary treatment team: a qualitative study. Diabetes Educ. 2011;37(6):794–800.
Acknowledgement
This work was supported by the Kathleen P. Welsh Fund, NIDDK RO1-060115, the Diabetes and Endocrinology Research Core NIH P30 DK36836, and the NIH Training Grant No. T32 DK007260. We thank the physicians and patients who shared their experiences and perceptions with us. We also thank Dr. Nadine Palermo, Nicholas Hebert, and Ross Markello for their useful comments on the manuscript.
Conflict of Interest
No author received other support for this grant other than funding from the Kathleen P. Welsh Fund. However, Martin J. Abrahamson, MD has provided consulting services to Novo Nordisk, Halozyme, and Boehringer Ingelheim. No other author has anything to declare.
Author Contributions
E.A.B. conducted interviews; read, coded, and thematically analyzed the transcripts; and wrote the manuscript. M.D.R. conducted interviews; read, coded, and thematically analyzed the transcripts; and reviewed and edited the manuscript. B.A.H. and K.M.B. read, coded, and thematically analyzed the transcripts and reviewed and edited the manuscript. Y.L. analyzed the quantitative data and reviewed and edited the manuscript. M.J.A. reviewed and edited the manuscript. K.W. had the initial idea for this study and wrote the research proposal; read, coded, and thematically analyzed the transcripts; and reviewed and edited the manuscript. All contributors had access to the data and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funded by Kathleen P. Welsh Fund, NIDDK RO1-060115, NIH P30 DK36836, NIH Training Grant No. T32 DK007260
Rights and permissions
About this article
Cite this article
Beverly, E.A., Ritholz, M.D., Brooks, K.M. et al. A Qualitative Study of Perceived Responsibility and Self-Blame in Type 2 Diabetes: Reflections of Physicians and Patients. J GEN INTERN MED 27, 1180–1187 (2012). https://doi.org/10.1007/s11606-012-2070-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2070-0