Abstract
BACKGROUND
In 2005 the American Heart Association (AHA) released updated recommendations for blood pressure (BP) monitoring in order to ensure accurate BP measurements.
OBJECTIVE
To determine if current methods of BP assessment in an ambulatory clinic result in significantly different BP measurements than those obtained by following the AHA recommendations and if these BP differences impact treatment decisions.
RESEARCH DESIGN
Randomized prospective analysis.
SETTING
University of New Mexico Hospital Adult Internal Medicine clinic.
PATIENTS
Forty adults with hypertension
METHODS
Patient BPs were measured using both the traditional triage method and the AHA-recommended method in cross-over fashion in random order. Two complete medical profile summaries were then constructed for each patient: one for each BP measurement obtained by each technique. These profiles were then reviewed by a panel of providers who provided hypothetical hypertension treatment recommendations.
RESULTS
Individual BP results varied greatly between the two methods. SBP readings differed by ≥5 mmHg in either direction for 68% of patients while 78% of patient’s DBP readings differed by ≥2 mmHg in either direction. Overall, 93% of patients had a BP difference of either ≥5 mmHg systolic or ≥2 mmHg diastolic. Five patients were determined to be at goal with the triage method, but were higher than their goal BP with the AHA method Significant differences were also seen in treatment recommendations for a given patient based on the differences seen between the two obtained BP readings. The number of patients with treatment variations between their two profiles ranged from 13% to 23% depending on the reviewing provider (p < 0.01 for all providers).
CONCLUSION
Inaccurate BP assessment is common and may impact hypertension treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) defines hypertension as a systolic blood pressure (SBP) ≥140, or diastolic blood pressure (DBP) ≥90 mmHg, and/or current use of antihypertensive medication1 Approximately 65 million Americans, or 32% of the population in the United States have hypertension2. People with elevated blood pressure are at four times higher relative risk of stroke and two to three times higher risk for developing congestive heart failure2.
In 2005, the American Heart Association (AHA) released updated recommendations for blood pressure monitoring in order to ensure accurate blood pressure measurements5. Inaccurate measurement of blood pressure can potentially result in misclassification of patients as hypertensive or normotensive as well as lead to inappropriate medical management. Differences in blood pressure monitoring technique can result in significantly different readings. Numerous factors such as body position, arm position, inter-arm differences, cuff size, and cuff placement can affect the reading3–10. A study conducted recently on hypertensive patients compared usual blood pressure monitoring, ambulatory monitoring, and monitoring following the Canadian Hypertension Education Program protocol11. The average blood pressures taken by the nurses following the protocol had significantly lower readings than the usual clinic readings (SBP: 138.7 ± 15.8 vs. 149.5 ± 16.4 mmHg, p < 0.001. DBP: 85.5 ± 7.9 vs. 90.4 ± 11.3 mmHg, p < 0.001).
Kim et al. also demonstrated the inaccuracy of clinic-based blood pressure readings by comparing them to standard mercury sphygmomanometry. In this study, the clinic-based readings were higher than the mercury standard leading the authors to suggest that this could result in inappropriate treatment decisions12. The primary objective of our study was to determine if following the AHA recommendations for blood pressure measurement results in significantly different blood pressure measurements than would be obtained by current methods of blood pressure assessment used in an ambulatory clinic and if this difference impacts hypertension treatment decisions.
METHODS
Design and Setting
This single-center investigator-initiated prospective analysis was designed in two phases. The first phase was a cross-over design to determine if following the AHA recommendations for blood pressure assessment would result in significantly different measurements than would be obtained by the current method of blood pressure measurement used in an ambulatory clinic and if these differences would lead to differences in achievement of goal blood pressure. The second phase was a continuation phase, which used the blood pressure values obtained by both methods to determine if the different measurements would result in hypertension treatment variability. Participants were enrolled into the first phase at the University of New Mexico Hospital Adult Internal Medicine Clinic in March 2007. The study was approved by the Health Sciences Center Human Research Review Committee at the University of New Mexico.
Participants
Patients were recruited as they presented for their regularly scheduled appointments at the Adult Internal Medicine Clinic. Patients were eligible if they carried a current diagnosis of hypertension, were greater or equal to 18 years of age, and were capable of reading and comprehending the English language. Patients were excluded if they were unable to have bilateral blood pressure assessment. All patients gave informed consent. The first 40 patients to consent were included in the study.
Randomization, Intervention, and Measurements
Phase 1
The blood pressure for each patient was measured by clinic personnel during triage for their appointment and also by the same study investigator following the AHA recommendations for blood pressure measurement (hereafter referred to as the AHA method)5. Patients were randomized by block randomization to the sequence of blood pressure assessment to minimize treatment order bias.
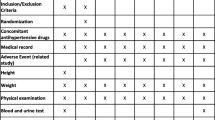
During both assessments, a trained observer utilizing a checklist passively monitored the blood pressure measurement taken by the nurse or assistant as well as by the study investigator. Body position, arm position, cuff position, cuff size, resting time, talking or no talking during measurement, and total time for measurement was documented for comparison purposes. The patient was informed of the observer during the consent process. The clinic staff was also informed of the observer; however, they did not know that technique was being observed. Both the study investigator and the clinic staff were blinded to the other blood pressure reading.
A study investigator also collected a current medication history as well as a past medical history. The patient’s other vital signs from this appointment were documented as well as demographic information such as age and sex. Goal blood pressures were determined by assessing the patient’s past medical history. Goal blood pressures as per JNC-7 were <130/80 mmHg for patients with diabetes or chronic kidney disease and <140/90 mmHg for all others1.
Phase 2
After all blood pressure data had been collected for all patients, two complete de-identified profiles were constructed for each patient. One included the triage blood pressure measurement, and the other included the measurement using the AHA method. The method used was not documented on the patient profile. The patient profiles also included the past medical history, medication list, drug allergies, vital signs, the presence or absence of ongoing pain (quantified on a 0–10 scale), pertinent physical exam findings, pertinent laboratory values, and the last two blood pressures taken at clinic visits including the measurement taken during the study visit. A panel of providers consisting of two internal medicine physicians and a cardiologist then independently reviewed these profiles. The providers were given 40 profiles with the AHA measurements followed one to two weeks later by 40 profiles with the triage measurements, so as to minimize recollection bias. The providers were unaware if the profiles contained the AHA or triage measurement. The providers were given an assessment form and the following question: based on this patient’s past medical history, current medications, and last two blood pressure measurements, should antihypertensive medications be initiated or changed at this visit (yes or no)? If yes, they were then asked to choose from the following options: increase dose of current medication(s); add new drug(s) to existing regimen; decrease dose of current medication(s); discontinue medication(s).
STATISTICAL ANALYSIS
Differences in mean blood pressures were assessed with paired Student’s t-tests and were considered significant at p < 0.05. We defined clinically significant differences in SBP and DBP as 5 mmHg and 2 mmHg respectively based off of previous clinical trials13–15. Differences in treatment decisions by the expert panel and differences in achieved goal blood pressures were analyzed with chi-square tests. Inter-rater reliability between the expert panel members was measured using the Kappa statistic. All statistical analyses were performed with SPSS for Windows version 11.0.1.
RESULTS
Forty subjects were enrolled and all 40 were included in the final analysis. Figure 1 shows the flow of study subjects. The mean age was 56.6 ± 10.2 years and 24(60%) were male. With regards to goal blood pressure, 27 (68%) patients had a goal of <140/90 mmHg, with the remainder having a goal of <130/80 mmHg.
Blood Pressure Results
Overall, individual blood pressure measurements varied greatly between the two methods. Figures 2a and b demonstrate the absolute differences between readings obtained using the triage and AHA methods for both SBP and DBP. Because the differences in absolute blood pressures between the two methods varied in both directions, no significant difference was seen in the mean SBP between the AHA and triage methods (133.6 ± 16.8 mmHg vs. 132.6 ± 17.3 mmHg; p = 0.605). However, mean DBP was significantly higher with the AHA method compared to the triage method (80.4 ± 10.5 mmHg vs. 77.6 ± 11.9 mmHg; p = 0.02). Readings differed by ≥5 mmHg in either direction for 68% of patients with respect to SBP while 78% of patients had DBP readings differing by ≥2 mmHg in either direction. Combined, 93% of patients had a BP difference of either ≥5 mmHg systolic or ≥2 mmHg diastolic. There was no observable difference in the magnitude of blood pressure variation depending on the actual blood pressure value. In other words, a high (or low) blood pressure did not necessarily mean that a patient was more likely to have a difference in their two blood pressure measurements between triage and AHA methods (Figs. 3a and b). Also when comparing measurement methods, 21/40 (53%) of patients had both a systolic and diastolic pressure that differed by at least 5 and 2 mmHg respectively. In 14 of these 21 patients, both components of blood pressure (i.e. systolic and diastolic) differed in the same direction. In other words, if the systolic measurement was higher with the AHA method versus triage, then the diastolic measurement was also higher with the AHA method versus triage. Overall, 65% of patients were not at their goal blood pressure when measured with the AHA method compared to 52% with the triage method (p < 0.001), which is a result of five patients who were determined to be at goal with the triage method, but were higher than their goal BP with the AHA method (Table 1 ).
Multiple technical errors were seen during the triage method that likely accounted for differences between blood pressure measurements. Table 2 reports the frequency at which the AHA recommendations were followed during either measurement. The AHA recommendations were not consistently followed during the triage measurement; compliance ranged from 0 to 90% depending on the criterion evaluated. Out of 10 possible errors, the mean number of errors per patient during the triage assessment was 4.1 ± 1.3. The most common error during triage was the lack of bilateral blood pressure measurements, which was not conducted in any patients during the triage assessment. In addition, we found six patients during the AHA measurement to have an interarm difference of ≥5 mmHg requiring repeat measurements which were not performed during triage. Of the 40 patients, 21 (52.5%) had a higher blood pressure in the right arm (Table 2). Of these 21 patients, 20 patients had blood pressure correctly measured in the right arm during triage. However, of the 19 patients with higher blood pressure in the left arm, only 5 patients had blood pressure correctly measured in the left arm during triage. Overcuffing was the most common cuffing error. This resulted in lower mean systolic and DBPs during the triage measurement: AHA SBP 135.9 ± 16.3 mmHg vs. 128.5 ± 17.9 during triage (p = 0.041) and AHA DBP 81.9 ± 9.8 mmHg vs. 77.0 ± 13.2 mmHg (p = 0.02). Due to the 5 minute resting period and bilateral measurements recommended by the AHA, the total time to measure the blood pressure using the AHA methods was 8.8 minutes vs. 2 minutes with the triage methods (p < 0.001). Patients randomized to the AHA method first had lower systolic (134.6 ± 18.8 AHA vs. 129.3 ± 16.4 Triage; p = 0.081) and diastolic blood pressures (90.2 ± 9.7 AHA vs. 75.2 ± 12.4 Triage; p = 0.004) when their blood pressure was measured with the triage method. The difference in mean SBP (132.5 ± 15 AHA vs. 135.8 ± 18 Triage; p = 0.164) or DBP (80.6 ± 11.4 AHA vs. 80.1 ± 11.1 Triage; p = 0.719) was not as great when patients were randomized to triage first.
Blood Pressure Treatment Recommendations
All three physician reviewers provided hypertension medication treatment recommendations based on the de-identified patient profiles they received. Significant intra-provider differences in treatment decisions were seen for many patients based on the blood pressures reported using the AHA and triage methods (Table 3). Compared to the cardiologist, internist 1 would have treated nine (23%) patients differently and internist 2 would have treated eight (20%) patients differently based on the different blood pressure measurements (P < 0.01 for all). Eighteen unique patients (45%) would have received different treatments by at least one provider based on the differences in blood pressure measurements between their profiles although there was not complete agreement between providers regarding individual treatment decisions.
Kappa coefficients were used to measure provider agreement between: 1) both internists, 2) internist 1 vs. the cardiologist, and 3) internist 2 vs. the cardiologist. Kappa scores indicated moderate agreement between both internists and between internist 1 and the cardiologist (kappa 0.550 for both) with substantial agreement (kappa 0.698) between internist 2 and the cardiologist.
DISCUSSION
In this randomized prospective analysis comparing triage and AHA recommended BP measurement techniques, we defined clinically significant differences in SBP and DBP as 5 mmHg and 2 mmHg respectively based off of previous clinical trials13–15 and individualized (rather than grouped) the data for purposes of our analyses. This is likely a more accurate way of depicting the results as the grouped results give the false impression that meaningful differences in SBP did not exist.
Overall, 37 (93%) of patients had a SBP which differed by ≥5 mmHg or a DBP which differed by ≥2 mmHg in either direction. These differences may seem small, however, the recently published Cardio-Sis trial suggests otherwise. The trial was designed to determine if tight SBP control (<130 mmHg) vs. usual control (<140 mmHg) in non-diabetic adults was beneficial, and found an average blood pressure difference between the two groups of 3.8 mmHg systolic and 1.5 mmHg diastolic13. After two years of follow-up, the tight-control group demonstrated a decreased likelihood of left ventricular hypertrophy as well as a statistically significant reduction in their composite cardiovascular outcome with this small mean blood pressure difference between groups13. Additionally, a 5 mmHg reduction in SBP has been shown to reduce stroke mortality by 14%, coronary heart disease (CHD) mortality by 9%, and total mortality by 7%14. A 2 mmHg reduction in DBP would result in a 6% reduction in the risk of CHD and a 15% reduction in the risk of stroke and transient ischemic attacks15. Moreover, it has been estimated that systematic errors in blood pressure measurement resulting in a 5 mmHg overestimation of DBP can falsely elevate the number of patients with a DBP >90 mmHg by 132%16. An underestimation of 5 mmHg could result in 62% of hypertensive patients appearing normotensive16.
Our study also found a significant difference in the percentage of patients who achieved their goal blood pressure with the triage method vs. the AHA method. This paralleled the treatment recommendation differences seen during phase 2 of our study Among the three reviewing providers, nearly half of the patients (45%) had differences in treatment recommendations based on their two blood pressure measurements. Interestingly, only one patient had different treatments recommended for their two blood pressure measurements from all three providers. This patient had the largest difference in blood pressure between the AHA and triage method with their AHA measurement of 164/78 mmHg and their triage measurement of 125/71 mmHg. There were six patients in whom two of three providers’ treatment decisions differed between the two profiles. However in these six patients, as well as the remainder of the patient population, magnitude of difference in blood pressures across the methods did not consistently explain differences in treatment decisions. These treatment differences included intensifying treatment when the triage blood pressure was falsely elevated, or not making changes when they were actually necessary or even reducing therapy when the triage blood pressure was falsely low (Table 3).
The technical errors observed during the triage measurement likely contributed to differences in the measurements between the AHA and triage methods. There were no bilateral measurements taken during the triage assessment. This is significant because the higher of the two arms should be used as the final blood pressure. Using the AHA method, we found that 52.5% of patients had a higher measurement in their right arm, and this was used as the final value, but during the triage assessment, 85% of patients had their blood pressure only taken in their right arm. As a result of unilateral measurements during triage, 15 patients had the incorrect arm measured during triage. While the AHA recommends taking bilateral blood pressure measurements at the initial examination, there was no documentation in any of the patients’ medical records indicating that this had previously been done, and therefore, there was no documentation if the patients’ right or left arms should be used at subsequent visits. Our results suggest that at the initial examination of a patient, the measured arm with a higher blood pressure should be recorded in the chart to facilitate future measurements.
The AHA guidelines also emphasize the importance of appropriate cuff size5. Undercuffing has previously been shown to be the most common cuffing error resulting in an average increase of 8.5 mmHg systolic and 4.6 mmHg DBP3. However, our study found overcuffing to be the most common cuffing error resulting in significantly lower blood pressure measurements during triage compared to those obtained using the AHA method. Interestingly, when the AHA method was conducted first, the triage blood pressures tended to be lower. While the exact reasons for this are unknown, one possible explanation may be the longer rest period allowed prior to triage blood pressure measurement. Because this study was not powered to analyze each technique and correlate it with a specific change in blood pressure, we cannot determine what percent of the blood pressure difference was a result of the inappropriate cuff size versus other technical errors that occurred at the same time. With an average of four technical errors per patient, it is possible that two errors could have opposite effects on blood pressure and cancel each other out. It was not possible to account for these effects on the final blood pressures.
Certain limitations of both study phases need to be considered when interpreting the results of this study. This was a single-clinic study, so the triage method of this clinic may be different than that of other ambulatory clinics. For example, there was a high rate of proper arm positioning during the triage assessment. The triage room in this clinic was conducive to appropriate patient positioning because an exam table was available for patients to rest their arm on. Other clinics might not have this available and would then be taking the blood pressure with the arm below heart level. Depending on the clinic, certain monitoring recommendations might be followed more consistently than others affecting the blood pressure measurements in different ways. While the clinic staff did not know that their technique was being documented, they did know the observer was recording blood pressure and thus could have resulted in some observation bias. However, this would suggest that had no observer been present with the triage staff, a greater number of technical errors could have occurred leading to a greater observed difference in blood pressure. In addition, a single clinic study limits the generalizability to a broad patient population. For example, our study population was middle aged and therefore the results might be different in a geriatric population. A major barrier to following the AHA recommendations in clinical practice may be the time it takes to measure blood pressure. Our study found the average time to be 8.8 minutes vs. 2 minutes with the triage method. In a busy clinical practice, the difference of 7 minutes might be difficult to manage, however given the treatment ramifications, should be considered worthy of the time. In clinical practice, some clinicians may re-check the blood pressure; however, with institutions converting to electronic health records many times only the triage blood pressure is entered into the record by the clinic staff. It will be important that all blood pressures taken during the visit be documented electronically to aid in follow-up and also for quality assurance measures.
The second phase was a hypothetical clinical scenario. The providers were making treatment decisions based on only two blood pressure values: the measurement from the current clinic visit and that from the last documented visit, and no home blood pressures were included. In clinical practice treatment decisions are made based on multiple factors such as previous blood pressures, blood pressure re-measurement by the provider, medication adherence, and reported pain. While we were not comparing the recommendations of the providers nor looking for appropriateness of recommendations, there could have been a Hawthorne effect because the providers did know the profiles would be examined. In this sense, it is possible that the providers may have been more aggressive in the study than they would have been in clinical practice.
CONCLUSION
We conclude that there is a clinically significant variation in blood pressure readings between the usual clinic method of blood pressure assessment and the AHA recommended method. This difference may result in differences in perceived rates of hypertension control. Importantly, incorrect blood pressure monitoring technique affected hypertension treatment decisions as demonstrated in a hypothetical clinical scenario. Clinic/office staff should be educated on the AHA recommendations for proper blood pressure measurement and encouraged to follow them in order to obtain a more accurate blood pressure. More accurate blood pressure measurement could result in improved hypertension management decisions.
References
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52.
Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics- 2006 update. A report from the American heart association statistics committee and stroke statistics subcommittee. Circulation. 2006;113:e85–151.
Manning DM, Kuchirka C, Kaminski J. Miscuffing: inappropriate blood pressure cuff application. Circulation. 1983;68:763–66.
Fonseca-Reyes S, Garcia de Alba-Garcia J, Parra-Carrillo JZ, Paczka-Zapata JA. Effect of standard cuff on blood pressure readings in patients with obese arms. How frequent are arms of a large circumference. Blood Press Monit. 2003;8:101–106.
Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals. Part 1: blood pressure measurement in humans. A statement for professionals from the subcommittee of professional and public education of the American Heart Association council on high blood pressure research. Circulation. 2005;111:697–716.
Webster J, Newnham D, Petrie JC, Lovell HG. Influence of arm position on measurement of blood pressure. Br Med J. 1984;288:1574–75.
Mourad A, Carney S, Gillies A, Jones B, Nanra R, Trevillian P. Arm position and blood pressure: a risk factor for hypertension? J Hum Hypertens. 2003;17:389–95.
Lane D, Beevers M, Barnes N, et al. Inter-arm differences in blood pressure: when are they clinically significant? J Hypertens. 2002;20:1089–95.
Pinar R, Sabuncu N, Oksay A. Effects of crossed leg on blood pressure. Blood Press. 2004;13:252–54.
Chiolero A, Gervasoni JP, Rwebogora A, Balampama M, Paccaud F, Bovet P. Difference in blood pressure readings with mercury and automated devices: impact on hypertension prevalence estimates in Dar es Salaam, Tanzania. Eur J Epidemiol. 2006;21:427–33.
Campbell NRC, Culleton BW, McKay DW. Misclassification of blood pressure by usual measurements in ambulatory physician practices. Am J Hypertens. 2005;18:1522–27.
Kim JW, Bosworth HB, Voils CI, et al. Brief report: How well do clinic-based blood pressure measurements agree with the mercury standard? J Gen Intern Med. 2005;20:647–49.
Verdecchia P, Staessen JA, Angeli F, et al. Usual versus tight control of SBP in non-diabetic patients with hypertension (Cardio-Sis): an open-label randomized trial. Lancet. 2009;374:525–33.
Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension clinical and public health advisory from the national high blood pressure education program. JAMA. 2002;288:1882–88.
Cook NR, Cohen J, Herbert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Intern Med. 1995;155:701–9.
Turner MJ, Baker AB, Kam PC. Effects of systematic errors in blood pressure measurements on the diagnosis of hypertension. Blood Press Monit. 2004;9:249–53.
Acknowledgements
This study was not supported by any internal or external funding.
The authors would like to acknowledge the physicians and staff from the UNM Internal Medicine Clinic.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ray, G.M., Nawarskas, J.J. & Anderson, J.R. Blood Pressure Monitoring Technique Impacts Hypertension Treatment. J GEN INTERN MED 27, 623–629 (2012). https://doi.org/10.1007/s11606-011-1937-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1937-9