Abstract
BACKGROUND
Cost-related underuse of medications is common among older adults, who seldom discuss medication costs with their physicians. Some older adults may use free drug samples or industry-sponsored patient assistance programs (PAP) in hopes of lowering out-of-pocket costs, although the long-term effect of these programs on drug spending is unclear.
OBJECTIVE
To examine older adults’ use of industry-sponsored strategies to reduce out-of-pocket drug costs and the association between doctor–patient communication and use of these programs.
DESIGN
Cross-sectional analysis of a 2006 nationally representative survey of Medicare beneficiaries.
PARTICIPANTS
14,322 community-dwelling Medicare beneficiaries age ≥65.
MAIN MEASURES
We conducted bivariate and multivariate analyses of the association between receipt of free samples and participation in PAPs with sociodemographic characteristics, health status, access to care, drug coverage, medication cost burden, and doctor–patient communication.
KEY RESULTS
51.4% of seniors reported receiving at least one free sample over the last 12 months and 29.2% reported receiving free samples more than once. In contrast, only 1.3% of seniors reported participating in an industry-sponsored PAP. Higher income respondents were more likely to report free sample receipt than low-income respondents (50.8% vs. 43.8%, p < 0.001) and less likely to report participating in a PAP (0.42% vs. 2.2%, p < 0.001). In multivariate analyses, those who reported talking to their doctor about the cost of their medications had more than twice the odds of receiving samples as those who did not (OR 2.17, 95% CI 1.95–2.42).
CONCLUSIONS
In 2006, over half of seniors in Medicare received free samples, but only 1.3% reported receiving any medications from a patient assistance program. Doctor–patient communication is strongly associated with use of these programs, which has important implications for clinical care regardless of whether these programs are viewed as drivers of prescription costs or a remedy for them.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Many seniors have difficulty paying for their medications and may respond by skipping doses of their medications or failing to fill prescriptions.1–5 Such cost-related non-adherence persists even after the expansion in drug coverage brought about by Medicare Part D, because of coverage gaps in the Part D benefit.6–9 Seniors’ strategies to lower out-of-pocket costs may include use of free samples from the pharmaceutical industry and enrollment in pharmaceutical industry-sponsored patient assistance programs (PAP), which provide certain medications at low or no cost. The extent to which Medicare beneficiaries have used these two strategies after Part D’s implementation is unknown.
While free samples may help to alleviate some of the financial burden associated with drug costs for low-income patients, evidence suggests that samples are not always targeted to those who could most benefit from them10–13, and their use may be associated with an increase in out-of-pocket drug costs.14 Much less is known about seniors’ participation in PAPs and very little data exist on the use of these programs.15–20 In a telephone survey of PAPs, only 4% of programs would state how many people they had helped, which ranged from single digits to over 10,000.19,20
Physicians report provision of free samples as one of their most frequently used strategies for reducing patients’ out-of-pocket costs.21 Medicare beneficiaries, however, seldom discuss these costs with their physicians.22 We know little about how doctor–patient communication about drug costs may be associated with the use of free samples or participation in PAPs. Understanding this association may shed light on whether physicians are targeting the programs to patients they think are most likely to benefit. Our goal for this study is to provide nationally representative data on seniors’ use of free samples and patient assistance programs, to describe the characteristics of users of these programs, and to examine the association between doctor–patient communication and participation in these programs.
METHODS
Study Design and Sample
We used data from a 2006 survey of 16,072 community-dwelling Medicare beneficiaries age 65 and older, administered in English and Spanish between October and December 2006. Respondents included individuals who responded to a 2003 national survey of Medicare beneficiaries4, plus an additional random sample of beneficiaries newly enrolled in Medicare since 2003. The survey used a mail- and telephone-based system and administered validated questions on sociodemographics, health characteristics, drug coverage, medication use, out-of-pocket spending and cost-related nonadherence. A more detailed description of the survey instrument and sampling frame is available elsewhere.1,23
After accounting for beneficiaries excluded because of death, institutionalization, non-English/Spanish language, and severe cognitive impairment, the response rate was 56 percent. Nonrespondents were slightly older with less education and poorer health, and disproportionately of minority race/ethnicity.1 For this analysis, we included individuals who reported taking at least one prescription medicine over the past year (n = 14,322).
Free Samples and Patient Assistance Programs
The survey included two questions specifically asking about receipt of free samples and participation in PAPs: 1) during the last 12 months, have any of your doctors given you free samples of prescription medicine? (Yes, more than once; Yes, one time; No); 2) do you currently get some of your prescription medicines through a patient assistance program run by a company that makes the medicines? Although we report the crude percentages of free sample receipt as a three-category variable, for the purposes of the bivariate and multivariate analyses we dichotomized sample receipt (yes/no).
Doctor–Patient Communication
The survey included several questions soliciting experiences with and beliefs about the doctor–patient relationship and communication. These included questions on respondent attitudes about the doctor’s role in lowering drug costs (e.g., how willing would they be to talk about costs with their doctors) and on behaviors and communication with doctors about drug costs (e.g. did they talk to their providers about drug costs and their medications; did they let their doctor know that they did not fill a prescription because of cost (cost-related nonadherence)). These validated items have been used in prior analyses of doctor–patient communication.22
Covariates
Covariates included age (65–74, 75–84, 85+), gender, race/ethnicity (white, black, Hispanic, other), residence in a rural state, the number of self-reported chronic conditions (including hypertension, myocardial infarction, congestive heart failure, asthma or COPD, diabetes, rheumatoid arthritis or osteoarthritis, cancer, and depression), number of medications (1–2, 3–4, or more than 5), education (less than high school, high school, some college, and college graduate), and monthly income categories based on the 2006 federal poverty line (≤$800, $801–2000, $2001–2500, >$2500). For approximately 12% of respondents with missing income data, income was imputed based on Buck’s Method24, which uses ordinal logistic regression to estimate the predicted probabilities of the missing income data and replaces missing values with values having the highest probability among the income categories; this method puts respondents into the single most likely category, which has an advantage of ease of understanding over other imputation methods that may classify respondents into multiple categories based on a probability distribution. An alternative specification using a dummy variable for missing income yielded similar results; thus we report the results using imputed income.
We included an indicator for primary source of prescription drug coverage: (stand alone Part D Prescription Drug Plan (PDP), Medicare Advantage Prescription Drug Plan (MAPD), employer-sponsored plans (including Tricare), Veterans Affairs (VA), Other). Those indicating more than one source of coverage were assigned to a primary source based on this hierarchy. An alternative specification using a dummy variable for those with multiple sources of coverage yielded results that were qualitatively similar to the main analysis; thus we report the results using this hierarchy.
Finally, we included several self-reported indicators of health status and access to care: self-reported fair or poor health, having a regular doctor, any hospitalization in prior year, and number of visits to “your personal doctor” over the past year.
Analysis
We conducted bivariate analyses of the association of sociodemographic characteristics, health status, access to care, and doctor–patient communication factors with receipt of free samples and participation in PAPs using chi-square tests. We used multivariate logistic regression analyses to examine the independent association between free sample use and sociodemographic, health status, and access to care variables. Because many of the doctor–patient communication variables were highly correlated, we included one measure—whether the respondent had discussed medication costs with the doctor in the previous year—in the multivariate analysis. Participation in PAPs was too low to warrant multivariate analyses. Probability sampling weights were applied to all analyses to correct for unequal sampling probabilities across states and strata. All p values are two-tailed with a significance level of 0.05. Analyses were performed using SAS version 9.2.
RESULTS
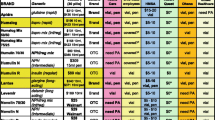
The study sample included 14,322 seniors (Table 1). The respondents were predominately white (86%) and had 2 or more chronic conditions (71%). Almost half reported using five or more medications. Nearly all reported having a regular doctor (95%) whom they visited at least once in the past 12 months (98%).
Sample Receipt
Overall, 51.4% of seniors reported receiving at least one free sample over the last 12 months and 29.2% reported receiving free samples more than once. Higher income respondents were more likely to report free sample receipt than their lowest income counterparts (50.8% with monthly income >$2500 vs. 43.8% with incomes ≤$800) (Table 2). Whites were more likely to report free sample receipt than black and Hispanic respondents (52.3%, 46.3%, and 45.1%, respectively) (all p < 0.001). Free sample receipt varied significantly by source of drug coverage; only 38% of respondents with VA insurance reported free sample receipt, compared to 50.8% of those with employer insurance, 45.5% of those in MAPD plans, and 55.6% of those in PDPs. Seniors with a regular doctor were more likely to report receiving free samples (52.1% vs. 37.4%, p < 0.001).
Seniors who talked about the cost of their medications with their doctor were significantly more likely to receive samples than those who did not (67.6% vs. 44.4%, p < 0.001) (Table 3). Patients who expressed a willingness to talk to their doctor if they had a problem affording their medication were significantly more likely to receive free samples, with 54.8% of those saying they definitely would talk vs. 43.4% of those saying probably not or 39.5% saying definitely not, receiving free samples (p < 0.001). Likewise, seniors saying it is definitely part of a doctor’s job to ask patients about problems paying for prescriptions were more likely to receive samples than those saying ‘no probably not’, or ‘no definitely not’ (53.7% vs. 49.3% and 37.7% respectively, p < 0.001). Seniors who let their doctor know about their cost-related non-adherence were more likely to receive samples than those who did not (70.5% vs. 54.4%, p < 0.001).
After controlling for other factors, those who talked to their doctor about medication costs had 2.17 times the odds of receiving samples as those who did not (OR 2.17, 95% CI 1.95, 2.42) (Table 4). Blacks and Hispanics had lower odds of reporting sample receipt (OR 0.79, 95% CI 0.67, 0.95 and OR 0.79, 95% CI 0.63, 1.00), as did those in the lowest income group. Respondents from rural regions had lower odds of sample receipt as well (OR 0.68, 95% CI 0.52, 0.88).
Patient Assistance Programs
Only 1.3% of seniors reported participating in a PAP run by a pharmaceutical company. Lower income seniors were more likely to report participation than those in the highest income groups (2.2% vs. 0.42%, p < 0.001) and those lacking insurance coverage were more likely to participate (2.7% of those without prescription insurance vs. 0.44% of those with employer insurance, 1.1% of those in MAPD plans, and 1.7% in PDPs (p < 0.001) (Table 2). Respondents with less than a high school education were significantly more likely to participate (2.0%) than those with additional years of education (p < 0.001). Of those individuals who did use PAPs, 67% reported free sample use during the year (data not shown).
Seniors who talked with their doctor about the costs of medications were more likely to use PAPs than those who did not (1.9% vs. 0.9%, p < 0.001) (Table 3). Seniors reporting they would definitely not talk to their doctor if they had problems affording medications were less likely to use these programs than those who definitely would talk to their doctor (0.3% vs. 1.5%, p < 0.001)
DISCUSSION
This nationally representative survey of Medicare beneficiaries indicates that use of free samples is widespread among older adults, while participation in industry-sponsored patient assistance programs appears extremely limited. Those with less education, lower income and lacking a primary care physician were less likely to receive free samples. Seniors who expressed a willingness to and experience with discussing medication costs with their doctors were much more likely to receive free samples than those who did not have these discussions. In contrast, while few seniors participated in industry-sponsored PAPs, participation was higher among those with low income and those lacking prescription coverage.
Two prior studies of free sample receipt in the Medicare population reported similar rates of use, but these studies used pre-Part D data.25,26 In the most recent of these studies, low-income seniors and racial/ethnic minorities in the 2004 Medicare Current Beneficiary Survey (MCBS) were less likely to ask for or receive samples, similar to our findings post Part D.25 We additionally found that one-third of those who had used PAPs, who presumably have the greatest need for financial assistance, did not report any free sample use.
The important question of whether prescription samples and PAPs are truly helping those in need versus driving the use of higher cost drugs warrants further study.10,13,27 Ideally, patients with lower income and those most in need would receive the majority of free samples if they had a clear indication for a brand-name drug over a generic equivalent. The high prevalence of cost-related non-adherence among lower income seniors23 could be partially mitigated by use of free samples. On the other hand, samples have the potential to increase costs and the use of brand name drugs.10,28–30 It is possible, in fact, that lower income seniors are receiving fewer samples precisely because they have higher rates of generic drug use, and that increasing the use of samples among this group might increase their use of more expensive medications.
Due to the controversy surrounding the provision of free samples, there are efforts underway to limit and regulate their distribution.31 In a 2009 report on conflicts of interest in medicine, the Institute of Medicine recommended that physicians and training programs limit (and in some cases prohibit) the use of free drug samples, except in situations for patients with financial difficulty.32 The Medicare Payment Advisory Commission (MedPAC) recently recommended tracking the distribution of free samples to physician practices by pharmaceutical companies.33 It will be important to understand how these policy changes affect the use of free samples.
Our survey is the first that directly asks a national sample of seniors whether they receive drugs through patient assistance programs. PAPs cover a majority of the top-selling medications in the US18,20, and most of the programs base eligibility partially on income, although income cutoffs vary, with some as high as 750% of the federal poverty limit.20 Slightly more than a quarter of these programs did not require documentation of income in 2007 and about half allowed patients to have existing prescription coverage.20
The industry emphasizes the important role these programs play in helping people pay for prescription drugs27,34, yet our survey finds that only 1.3% of Medicare beneficiaries report program participation. It may be that the PAPs are geared towards those under the age of 65, and in fact a survey of these patient assistance programs found that only 29% provided assistance for patients enrolled in Part D, with an additional 17% assisting Part D beneficiaries only if they are in the coverage gap.20 While there is some concern that these programs may lead patients towards a brand-name product when other less costly alternatives are available20,35, the low rate of PAP use among Medicare beneficiaries may mean this is less of a problem. Alternatively, given the high-rate of cost-related nonadherence observed among low-income seniors and those lacking prescription coverage, many seniors could potentially benefit from these programs.
Doctor–Patient Communication
Reporting discussing medication costs with one’s physician had a strong positive association with free sample receipt as well as participation in PAPs. Seniors who talked about the cost of their medications with their doctor were significantly more likely than those who did not to receive samples (67.6% vs. 44.4%, p < 0.001) and to use patient assistance programs (1.9% vs. 0.9%, p < 0.001). While we are unable in a cross-sectional survey to infer a causal relationship between these behaviors, communication about drug costs was a more important predictor of free sample receipt in multivariable analyses than either income or drug coverage. Evidence suggests that communication with patients about costs can improve adherence to medication36, but that these conversations are still rare.21,22,37–39 Our results reinforce this important association between doctor–patient communication and management of prescription costs.
There are potential differences in how doctor–patient communication could affect receipt of samples and participation in PAPs. Physician offices are the key source of prescription samples for patients. While over 90% of PAPs required patients in 2007 to submit prescriptions to receive assistance and almost half delivered the medication to the doctor’s office rather than directly to the patient20, patients likely have more flexibility to enroll in PAPs outside of the doctor’s visit. Nonetheless, the physician plays a central role in both of these processes because they are ultimately responsible for the prescription. Improved doctor–patient communication does not necessarily have to lead to greater participation in these programs; it would, however, open the door to participation for many patients who could benefit and would encourage honest discussions about the risks and benefits of participation in the programs.
Limitations
The results of this study must be interpreted in the context of the study design. First, the survey achieved a modest response rate (56%) and did not include institutionalized Medicare beneficiaries or those younger than age 65. Because the most vulnerable seniors are not represented, we may underestimate the socioeconomic disparity in free sample use. Second, we assigned the 20% of beneficiaries reporting multiple sources of drug coverage to one primary source using a pre-defined hierarchy; we may have thus overlooked the effect of secondary sources of coverage in helping patients afford prescriptions (such as VA or employer plans). However, the distribution of coverage sources in our sample using the hierarchical approach is similar to national data from the Department of Health and Human Services.40 Third, our question about prescription assistance programs asks respondents whether they receive any of their medications through programs sponsored by manufacturers that make their drugs, and thus asks about current use. As a result, our analysis may underestimate the number of people who have ever used these programs. Finally, the study is cross-sectional, and as such, we cannot infer a causal relationship between doctor–patient communication and receipt of assistance with prescription medications.
CONCLUSIONS
In this analysis, we examine the use of two pharmaceutical industry activities that have very different rates of take-up among seniors. More than half of seniors use free samples, with the highest rates among higher income seniors; patient assistance programs, on the other hand, have very low use but are predominately used by those most in need. Our results reinforce the importance for physicians and other providers of communicating with their patients about these programs and about their patients’ difficulties paying for medications, and increasing their efforts to connect those in need with patient assistance programs, if possible. Physicians and researchers must also be vigilant in monitoring the drugs available through these programs, regardless of whether they are viewed as drivers of prescription costs or a remedy for them, to assure that the most cost-effective and safe medications are used.
References
Neuman P, Strollo MK, Guterman S, et al. Medicare Prescription Drug Benefit Progress Report: Findings From A 2006 National Survey Of Seniors. Health Aff. 2007;26(5):w630-43.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94(10):1782–87.
Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164(16):1749–55.
Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood). 2005;Suppl Web Exclusives:W5-152-W155-166.
Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled Medicare beneficiaries: a national survey 1 year before the Medicare drug benefit. Arch Intern Med. 2006;166(17):1829–35.
Madden JM, Graves AJ, Ross-Degnan D, Briesacher BA, Soumerai SB. Cost-related medication nonadherence after implementation of Medicare Part D, 2006–2007. JAMA. 2009;302(16):1755–56.
Zhang Y, Donohue JM, Newhouse JP, Lave JR. The effects of the coverage gap on drug spending: a closer look at Medicare Part D. Health Aff (Millwood). 2009;28(2):w317-25.
Zhang Y, Lave JR, Newhouse JP, Donohue JM. How the Medicare part D drug benefit changed the distribution of out-of-pocket pharmacy spending among older beneficiaries. J Gerontol B Psychol Sci Soc Sci. 2009.
Zivin K, Madden JM, Graves AJ, Zhang F, Soumerai SB. Cost-related medication nonadherence among beneficiaries with depression following Medicare Part D. Am J Geriatr Psychiatry. 2009;17(12):1068–76.
Chimonas S, Kassirer JP. No more free drug samples? PLoS Med. 2009;6(5):e1000074.
Cutrona SL, Woolhandler S, Lasser KE, et al. Free drug samples in the United States: characteristics of pediatric recipients and safety concerns. Pediatrics. 2008;122(4):736–42.
Cutrona SL, Woolhandler S, Lasser KE, Bor DH, McCormick D, Himmelstein DU. Characteristics of recipients of free prescription drug samples: a nationally representative analysis. Am J Public Health. 2008;98(2):284–89.
Whittle J, Good CB. Prescription drug samples: making decisions with imperfect data. J Gen Intern Med. 2008;23(6):890–92.
Alexander GC, Zhang J, Basu A. Characteristics of patients receiving pharmaceutical samples and association between sample receipt and out-of-pocket prescription costs. Med Care. 2008;46(4):394–402.
Chen JT, Summers KH. Pharmaceutical manufacturer prescription assistance programs: are they worth it? J Manag Care Pharm. 2007;13(7):611–13.
Chisholm MA, DiPiro JT. Pharmaceutical manufacturer assistance programs. Arch Intern Med. 2002;162(7):780–84.
Van Diepen LR. Pharmaceutical manufacturer assistance programs for indigent patients: solution or symptom? Am J Health Syst Pharm. 2001;58(2):162–63.
Chauncey D, Mullins CD, Tran BV, McNally D, McEwan RN. Medication access through patient assistance programs. Am J Health Syst Pharm. 2006;63(13):1254–59.
Choudhry NK, Lee JL, Agnew-Blais J, Corcoran C, Shrank WH. Patient Assistance Programs: Information Is Not Our Enemy. Health Aff. 2009;28(3):843–44.
Choudhry NK, Lee JL, Agnew-Blais J, Corcoran C, Shrank WH. Drug Company-Sponsored Patient Assistance Programs: A Viable Safety Net? Health Aff. 2009;28(3):827–34.
Alexander GC, Casalino LP, Meltzer DO. Physician strategies to reduce patients' out-of-pocket prescription costs. Arch Intern Med. 2005;165(6):633–36.
Wilson IB, Schoen C, Neuman P, et al. Physician–patient communication about prescription medication nonadherence: a 50-state study of America's seniors. J Gen Intern Med. 2007;22(1):6–12.
Safran DG, Strollo MK, Guterman S, Li A, Rogers WH, Neuman P. Prescription coverage, use and spending before and after Part D implementation: a national longitudinal panel study. J Gen Intern Med. 2010;25(1):10–17.
Buck S. A method of estimation of missing values in multivariate data suitable for use with an electronic computer. J R Stat Soc. 1960;22(2):302–306.
Tjia J, Briesacher BA, Soumerai SB, Ross-Degnan D, Gurwitz JH. Medicare beneficiaries and free prescription drug samples: a national survey. J Gen Intern Med. 2008;23(10):1727.
Taira DA, Iwane KA, Chung RS. Prescription drugs: elderly enrollee reports of financial access, receipt of free samples, and discussion of generic equivalents related to type of coverage. Am J Manag Care. 2003;9(4):305–12.
Johnson K. Voluntary Patient Assistance Programs: Additional Federal Oversight Unwarranted. Health Aff. 2009;28(3):835–38.
Pinckney RG, Helminski AS, Kennedy AG, Maclean CD, Hurowitz L, Cote E. The effect of medication samples on self-reported prescribing practices: a statewide, cross-sectional survey. J Gen Intern Med. 2011;26(1):40–4.
Adair RF, Holmgren LR. Do drug samples influence resident prescribing behavior? A randomized trial. Am J Med. 2005;118(8):881–84.
Chew LD, O’Young TS, Hazlet TK, Bradley KA, Maynard C, Lessler DS. A physician survey of the effect of drug sample availability on physicians' behavior. J Gen Intern Med. 2000;15(7):478–83.
Morgan W, Mihaly C, Van Tassel-Sweet AJ. Report of the Vermont Attorney General on the Advisability of Requiring Disclosure of Free Samples Distributed by Manufacturers of Prescribed Products to Vermont Health Care Providers January 15, 2010. Available at http://www.atg.state.vt.us/assets/files/Free%20Samples%20Report.pdf (Accessed June 2011).
Institute of Medicine of the National Academies. Conflict of Interest in Medical Research, Education and Practice 2009.
Medicare Payment Advisory Commission. Report to Congress, Medicare Payment Policy. 2009:332–35.
Partnership for Prescription Assistance (PPA). By the Numbers: PPA Impact, http://www.pparx.org/en/about_us/ppa_impact. Accessed February 10, 2010.
U.S. Department of Health and Human Services Office of Inspector General. Special Advisory Bulletin on Patient Assistance Programs for Medicare Part D Enrollees: Federal Register. Vol 70.; 2005:70623–628.
Shrank WH, Hoang T, Ettner SL, et al. The implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Intern Med. 2006;166(3):332–37.
Beran MS, Laouri M, Suttorp M, Brook R. Medication costs: the role physicians play with their senior patients. J Am Geriatr Soc. 2007;55(1):102–7.
Sleath B, Roter D, Chewning B, Svarstad B. Asking questions about medication: analysis of physician-patient interactions and physician perceptions. Med Care. 1999;37(11):1169–73.
Tarn DM, Paterniti DA, Heritage J, Hays RD, Kravitz RL, Wenger NS. Physician communication about the cost and acquisition of newly prescribed medications. Am J Manag Care. 2006;12(11):657–64.
Kaiser Family Foundation. Medicare Fact Sheet: The Medicare Prescription Drug Benefit. November 2006. http://www.kff.org/medicare/upload/7044-05.pdf. Accessed February 1, 2011.
Acknowledgments
This work was supported in part by a VA HSR&D Career Development Award (09–207) (Gellad), a Robert Wood Johnson Foundation Investigator Award in Health Policy Research (Huskamp), and by grants from the Agency for Healthcare Research and Quality (1RO1HS017695, R01HS018657), and the National Institute of Aging (1R01AG034056) and National Institute of Mental Health (RC1MH088510).
The original survey and data collection were funded by grants from the Commonwealth Fund and the Henry J. Kaiser Family Foundation.
Portions of an earlier version of this manuscript were presented at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) Annual European Congress in Paris, France in 2009.
The contents of this paper are the sole responsibility of the authors and do not necessarily represent the views of the US Department of Veterans Affairs or the other funding sources.
Conflict of Interest
Dr. Safran and Ms. Li are employed by Blue Cross Blue Shield of Massachusetts (BCBSMA). BCBSMA is a not-for-profit health care company whose products include a variety of plans available to Medicare beneficiaries.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gellad, W.F., Huskamp, H.A., Li, A. et al. Use of Prescription Drug Samples and Patient Assistance Programs, and the Role of Doctor–Patient Communication. J GEN INTERN MED 26, 1458–1464 (2011). https://doi.org/10.1007/s11606-011-1801-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1801-y