Abstract
BACKGROUND
There is a gap between the need for patient-centered, evidence-based primary care for the large burden of chronic illness in the US, and the training of resident physicians to provide that care.
OBJECTIVE
To improve training for residents who provide chronic illness care in teaching practice settings.
DESIGN
US teaching hospitals were invited to participate in one of two 18-month Breakthrough Series Collaboratives—either a national Collaborative, or a subsequent California Collaborative—to implement the Chronic Care Model (CCM) and related curriculum changes in resident practices. Most practices focused on patients with diabetes mellitus. Educational redesign strategies with related performance measures were developed for curricular innovations anchored in the CCM. In addition, three clinical measures—HbA1c <7%, LDL <100 mg/dL, and blood pressure ≤130/80—and three process measures—retinal and foot examinations, and patient self-management goals—were tracked.
PARTICIPANTS
Fifty-seven teams from 37 self-selected teaching hospitals committed to implement the CCM in resident continuity practices; 41 teams focusing on diabetes improvement participated over the entire duration of one of the Collaboratives.
INTERVENTIONS
Teaching-practice teams—faculty, residents and staff—participated in Collaboratives by attending monthly calls and regular 2-day face-to-face meetings with the other teams. The national Collaborative faculty led calls and meetings. Each team used rapid cycle quality improvement (PDSA cycles) to implement the CCM and curricular changes. Teams reported education and clinical performance measures monthly.
RESULTS
Practices underwent extensive redesign to establish CCM elements. Education measures tracked substantial development of CCM-related learning. The clinical and process measures improved, however inconsistently, during the Collaboratives.
CONCLUSIONS
These initiatives suggest that systematic practice redesign for implementing the CCM along with linked educational approaches are achievable in resident continuity practices. Improvement of clinical outcomes in such practices is daunting but achievable.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
The high prevalence of chronic illness, which consumes the majority of health care expenditures in the US1, calls for residency training that is conducted in clinical settings designed and organized to provide high quality chronic illness care2–4. The current approach to physician training reflects a heavy focus on acute disease and inpatient medicine. A gap exists between evidence-based care for the growing burden of chronic illness in the US and the training of physicians who will provide that care.
The Chronic Care Model (CCM), an evidence-based strategy for the care of patients with chronic illness5–8, has been implemented in hundreds of community clinical settings, generally with associated improvement of chronic illness care8. However, the participation of teaching practice settings in quality improvement activities based on the CCM has been limited.
We describe two initiatives—the national Academic Chronic Care Collaborative (ACCC) and a subsequent California Academic Chronic Care Collaborative (CACCC)—that supported resident practices in their efforts to transform their practices and training in accord with the CCM. The overarching goal was twofold: to improve the training for the residents who provide chronic illness care in resident practices and to improve the care delivered to chronically ill patients in those practices. The following were the specific aims: first, redesign resident practices based on the CCM; second, implement and test educational strategies based on the CCM in these settings; and third, evaluate changes in the clinical processes and outcomes of care in such practices.
METHODS
Organization and Support of the Collaboratives
The Collaboratives were conducted by a partnership between the Institute for Improving Clinical Care of the Association of American Medical Colleges (AAMC), and Improving Chronic Illness Care, a national program based at Group Health Cooperative. The national staff and faculty for both initiatives were supported in large measure by generous grants from the Robert Wood Johnson Foundation and the California HealthCare Foundation.
Residency Practices and Their Patients
Participating resident practices in internal medicine, family medicine or pediatric training programs were affiliated with either traditional research-focused institutions (90% of teams) or community-based residency programs.
The majority of patients were uninsured or supported by Medicaid or Medicare. Patients’ social circumstances frequently added impediments to continuity of their care, e.g., limited personal financial means, difficulty finding timely transportation to clinic appointments, cost of medications and disability.
“Learners” were defined as all local team participants who intended to change their approach to the care of patients with chronic conditions in the resident practices. A faculty member generally led teams that included residents, other attending physicians, students, nurses, medical assistants, pharmacists, and/or social workers.
While the clinical conditions selected by one or more teams included chronic obstructive pulmonary disease, asthma, or hepatitis C, we report here only the results from the 41 practices that focused on diabetes care.
Planning the Interventions
The CCM5,8 guided the teaching and improvement activities of the Collaboratives. Implementation of the CCM in these practices required substantial practice redesign, which included the following7:
-
Redesign the practice microsystem to assure that care was provided by an effective care team, which usually consisted of a physician, nurse, and medical assistant and less frequently included a clinical pharmacist and/or social worker;
-
Develop evidence-based clinical decision-making, guided by review and adherence to the published literature for chronic diabetes management;
-
Establish a clinical information system with particular attention to a patient registry for tracking clinical measures at both the individual and population level;
-
Conduct planned visits that assured that patients received guideline-influenced care;
-
Develop effective self-management support to patients; and
-
Help patients access and use valuable community resources such as peer support programs for behavioral change, and patient education offerings.
The initiatives employed the Institute for Healthcare Improvement Breakthrough Series Collaborative strategy9–11 to learn and implement the CCM. Over the course of the Collaboratives, participating residency program teams met together for three, two-day learning sessions, and one all-day virtual web-mediated meeting. Teams learned about the CCM and exchanged program redesign strategies that they conducted between sessions. Every month teams reported their aggregated patient data taken from their electronic registries. Monthly telephone conferences led by national program faculty focused on these reports.
Based on earlier experiences with Chronic Care Collaboratives in non-academic settings6,7, the national program leadership crafted a recruitment strategy that was designed to identify highly motivated institutions2,3,12. The national initiative offered no financial support, but it offered the opportunity to participate with the national faculty in the national inter-institutional program that facilitated change and learning. Institutions provided support for the cost of redesign of local practices.
A similar invitation was issued subsequently for the California Collaborative. Here successful applicant teams were awarded stipends of $12,000 per team to help defray costs of redesign of practices and education, e.g., travel and release time for strategic design meetings. These funds were supplemented by contributions from participating institutions in both Collaboratives.
Study of the Intervention and Methods of Evaluation
Implementation Measures
Implementation of the CCM was measured by the Assessment of Chronic Illness Care (ACIC) Instrument. The ACIC is a previously validated instrument10, which evaluates success in implementing 7 key components of the CCM—delivery system design, decision support, clinical information systems, patient self-management, integration, healthcare system organization, and community linkages. At the beginning, in the middle and at the end of the initiatives, the residencies used the ACIC to self-evaluate implementation and application of each of the components of the CCM. National faculty reviewed in depth each of the reported measures with teams in open meetings at Collaborative sessions. Teams frequently modified these self-reported measures based on such feedback and discussion, and the process often led to less optimistic self-evaluation.
Education Measures
Because the CCM had not previously been systematically implemented in academic settings, it was necessary to develop measures to assess progress of educational redesign during the national Collaborative. An instrument was developed specifically for this purpose—the Assessment of Chronic Illness Care for Education (ACIC-E), which tracked the extent of educational engagement and redesign that addressed the same 7 components of the CCM described above for the ACIC. This instrument, a direct modification of the ACIC with a focus on specific changes in the education program, is described in detail elsewhere13. It was employed in the Collaboratives in the same way as described for the ACIC above.
The national Collaborative faculty and teams developed an additional set of representative, defined educational measures to compare teams. The measures were developed through a consensus process among teams, which prioritized significance and feasibility of proposed measures14. The two explicit educational measures that were adopted by this process were: first, “percent of learners who have used a registry to change care,” and second, “percent of learners who have developed self-management plans with a patient.” Teams also developed their own optional education measures to help track local progress. Examples of these additional measures included, “percent of learners identifying, learning and teaching others about a clinical question,” and “percent of learners appraising literature for clinical guidelines and sharing findings with team members.”
Clinical Measures
Six clinical measures were tracked in patient registries for each practice and were reported monthly to the Collaborative director: three patient health indicators—percent of patients with HbA1c <7%, LDL <100 mg/dL, and blood pressure ≤130/80; and three process measures—percent of patients with up to date retinal and foot examinations, and who had established patient self-management goals. Improvement scores were calculated as the difference between baseline and final reports. The national faculty aggregated and plotted the three patient health indicators using statistical process control with upper and lower limits set at 3 sigma in a Shewhart p chart15. Statistical process control has been used to track defined processes since its introduction by Shewhart and Deming in the 1920s15. It was employed in this instance to determine whether special cause variation—the term that describes variation that is unlikely to occur by chance—occurred during participation in the collaboratives.
Ethical Issues
Review of the ACCC was obtained through the Institutional Review Board of the AAMC at the American Institute for Research, which granted a waiver because it was determined that the project was a quality improvement initiative. IRB approval stipulated that clinical data could not be identifiable at the patient level, but could be aggregated to reflect team performance. In addition, public identification of institutions was not permitted, to maintain the opacity of patient identifiers.
RESULTS
Collaborative Participation and CCM Implementation
An invitation was extended in 2004 to the approximately 400 teaching hospitals that were members of the AAMC Council of Teaching Hospitals. Of the 400, 36 teams from 22 institutions initially agreed to participate. Of these, 26 teams focused on diabetes improvement and successfully completed the Collaborative as reflected by consistent reporting of process, educational, and clinical outcomes. Subsequently a similar invitation was extended in 2006 to a cohort of 21 teaching hospitals in California; 21 teams from 15 institutions demonstrated readiness to participate. Fifteen of these teams focused on diabetes and completed the Collaborative.
The ACIC measurements, obtained at the beginning, mid-point and end of the initiatives, provide evidence of the progressive implementation of the components of the CCM. These results are described using a spider diagram (Fig. 1).
The teams and their sponsoring institutions were self-selected from the 400 teaching hospitals. Most sites had strong commitment by senior leadership, as reflected by financial and moral support, and the teams were led by local champions16 who were often program directors and/or division chiefs. Implementation of the electronic patient registry was an early administrative challenge for many of the practices, but ultimately served as a vital tool for tracking change.
The Collaborative strategy was effective for team learning. For example, high-performing teams developed benchmarks and implementation strategies that have been reported elsewhere as the AHRQ web-based “Tool kit for developing the Chronic Care Model in an academic environment12.”
Education Measures
Participating programs designed and implemented extensive modifications in their teaching processes. Examples included didactic sessions on strategies for practice implementation of the Model and use of quality improvement techniques such as the Plan-Do-Study-Act rapid cycle improvement model. Other components included sessions that addressed evidence to support diabetes treatment decisions, and attention to team building. Experience was gained with electronic patient registries for population-based outcome analysis12. Health care team meetings generally included residents’ input in planning for care delivery. Structured mentored experiences were developed for selected components of the CCM that are not usually employed for care in resident practices such the planned visit and group visit.
The educational techniques that were developed by the national Collaborative faculty and teams laid the groundwork for their use by the California Collaborative. The national Collaborative developed the curriculum and assessment instruments13,14, and they were implemented in the latter half of the assessment period of the national Collaborative, while the California Collaborative employed the ACIC-E and the two educational measures to track their progress from the outset of the assessment period. The results for the California initiative are presented as change scores from baseline in the ACIC-E (Fig. 2), and changes in percent of residents who participated in specific CCM learning experiences (Table 1). By the end of both Collaboratives, the majority of residents had worked with registries, practiced self-management support, and conducted planned visits.
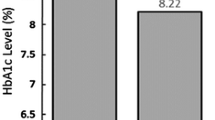
Clinical Measures
The aggregated clinical outcomes are presented in Tables 2 and 3. Teams in both Collaboratives showed improvement in process measures. Changes in measures of disease control were more modest, especially for the percentage of the population with HbA1c <7%. Nevertheless, tracking aggregate data by means of Shewhart p charts15 showed special cause variation reflecting improvement in blood pressure and LDL control in the late stages of the California Collaborative. Significant changes were not seen in HbA1c levels.
DISCUSSION
The participating practices adopted most elements of the CCM, including development of inter-professional teams, delegation of provision of care by appropriate team members, implementation of patient self-management strategies, group visits, proactive patient management—anticipating the needs of patients as opposed to providing reactive management—and use of an information system to track individual patient measures. In addition, resident training programs successfully incorporated educational strategies for learning the elements of evidence-based chronic illness care.
Resident practices, by their nature, facilitated practice redesign to implement the CCM. For example, residents, as frontline caregivers, were effective and active participants in redesign and CCM implementation. In addition, evidence-based practice was highly valued and readily adopted in these training settings8. Similarly, residents are by nature competitive in their commitment to providing good patient care17; hence, teams both competed and readily learned from each other as change strategies were adopted across the diverse Collaborative settings19. The need to address ACGME competencies for accreditation purposes17,18—particularly practice-based learning and systems-based practice—provided an opportunity to address multiple demands on learners and academic institutions.
Nevertheless, implementation of the CCM in these settings required a substantial redesign effort even for these highly motivated practices20–22. The progression during the collaboratives of ACIC average scores to 5-8 (out of a possible 11), while reflecting change in the practices, speaks candidly to the challenge of achieving full implementation of the CCM in these resident practices.
The baseline findings in the national Collaborative—only about one-third of patients in these highly committed resident practices were initially within accepted guidelines for six clinical and process measures—reflects the challenge that good diabetes management presents in these teaching settings and emphasizes the imperative for improvement. Similar baseline findings for diabetes control have been observed in studies of chronic illness care in Community Health Centers in the US23, while observations in private practice settings generally show higher baseline levels of control24.
Previous reports suggest the importance of continuity experience both for residents and their patients in the improvement of diabetes outcomes. Warm and colleagues reported the ability to effect change in clinical outcomes using the CCM17. Of note, these observed changes occurred in a residency program that included a yearlong ambulatory block. Dearinger and colleagues also demonstrated that extensive commitment to continuity was required to have a significant impact on clinical outcomes in patients with diabetes in residency settings25. While the CCM emphasizes strategies for continuity of care, timely and continuous care is a challenge for most resident practices and may have played a role in the modest improvements in clinical outcomes in this report. Such continuity is made difficult, for example, by the obligations for residents to meet regularly changing assignments that include demands for acute care of seriously ill hospitalized patients, and the effects of regular turnover in resident clinic staffing.
Limitations
There are several limitations to interpretation of the findings that we report here. First, we cannot say with certainty that improvement observed in the care of the patients in these initiatives was due solely to adoption of the CCM. There was no control group. Moreover, the trends in healthcare delivery that increasingly give attention to good chronic illness care were unfolding during the time that these Collaboratives took place. This was particularly true in California where considerable support already existed for change of this type26. This is also suggested by the higher scores for clinical outcomes both at the outset and conclusion of the California Collaborative compared to the national Collaborative. At least some of the benefit may result from the greater attention provided patients simply because they were the focus of these redesign initiatives. Second, while we cannot determine that implementation of the CCM will result in long-term reduction in morbidity and mortality based on the changes in these 18-month Collaboratives, control of the principal clinical measures in the CCM (blood pressure, LDL and HgbA1C) has been documented to reduce over time the prevalence of microvascular disease in persons with diabetes as reflected in cardiac disease and stroke. Third, whether the changes observed in these programs can be replicated in other settings depends on the presence of many of the leadership and cultural characteristics that were found in these participating institutions3,4. Nevertheless, these early adopter institutions may possess other inherent characteristics that were not readily apparent. Insights may be found in this regard by examining further the differences between the institutions that initially joined these Collaboratives but were unable to sustain their participation. Finally, whether these changes can be sustained over time in these institutions will depend on additional resources along with continued strong leadership and a supportive culture.
CONCLUSIONS
These initiatives suggest that both the practice redesign required for implementation of the CCM and linked educational strategies are achievable in resident continuity practices. However, the modest improvement in clinical outcomes observed in these practices in comparison with initiatives from single site initiatives reported in the literature suggests that effective care of patients with chronic illness may require prolonged continuity of care that poses a challenge in many resident practices, even in those committed to implementation of the CCM. Durable implementation of the CCM in resident practices necessitates substantial commitment from local institutional, clinical and academic leadership.
References
Institute of Medicine. Crossing the quality chasm: a new health system for the twenty-first century. Washington: The National Academy Press; 2001.
Holman H. Chronic disease—The need for a new clinical education. JAMA. 2004;292:1057–9.
Stevens DP, Wagner EH. Transform residency training in chronic illness care—now. Acad Med. 2006;81:1–3.
Stevens DP, Sixta CS, Wagner EH, Bowen JL. The evidence is at hand for improving care in settings where residents train. J Gen Intern Med. 2008;23:1116–7.
Wagner EH, Austin BT, Von Korff M. Organizing care for chronic disease. Millbank Quarterly. 1996;74:511–44.
McCulloch DK, Price MJ, Hindmarsh MA, Wagner EH. Improvement in diabetes care using an integrated population-based approach in a primary care setting. Dis Manage. 2000;3:75–82.
Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20:64–78.
Coleman K, Austin BT, Brach C, Wagner WH. Evidence on the chronic care model in the new millennium. Health Aff. 2009;28:75–85.
Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. 2003.
Bonomi AE, Wagner EH, Glasgow RE, Von Korff M. Assessment of chronic illness care (ACIC): a practical tool to measure quality improvement. Health Serv Res. 2002;37:791–820.
Wagner EH, Glasgow RE, David C, Bonomi AE, Provost L, McCulloch D, Carver P, Sixta C. Quality improvement in chronic illness care: A collaborative approach. J Qual Improvement. 2001;27:63–80.
http://www.ahrq.gov//populations/chroniccaremodel. Accessed April 7, 2010
Bowen JL, Stevens DP, Provost L, Sixta CS, Johnson JK, Woods DM, Wagner EH. Assessing chronic illness care education (ACIC-E): A tool for tracking educational redesign for improving chronic care education. J Gen Intern Med 2010;XX:XX-XX
Bowen JL, Stevens DP, Sixta CS, Provost L, Johnson JK, Woods DM, Wagner EH. Developing measures of educational change for collaborative teams implementing the Chronic Care Model in teaching practices. J Gen Intern Med 2010; XX:XX-XX
Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12:458–64.
Daumschroder LJ, Banaszak-Holl J, Kowalski CP, Forman J, Saint S, Krein SL. The role of the “champion” in infection prevention: results from a multisite qualitative study. Qual Saf Health Care. 2009;18:434–40.
Warm E, Schauer DP, Diers T, Mathis BR, Neirouz Y, Boex J, Rouan GW. The ambulatory long-block: An Accreditation Council for Graduate Medical Education (ACGME) Educational Innovations Project (EIP). J Gen Intern Med. 2008;23:921–6.
Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and accreditation in graduate medical education. Health Aff. 2002;21:103–11.
Davidoff F. Heterogeneity is not always noise: Lessons from improvement. JAMA. 2009;302:2580–6.
Grant RW, Buse JB, Meigs JB, University HealthSystem Consortium (UHC) Diabetes Benchmarking Project Team. Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change. Diab Care. 2005;28(2):337–442.
Nembhard IM, Alexander JA, Hoff TJ, Ramanujam R. Why does the quality of health care continue to lag? Insights from management research. Academy of Management Perspectives. 2009;23(2):24–42.
Feifer C, Mora A, White B, Barnett BP. Challenges to improving chronic disease care and training in residencies. Acad Med. 2006;81:696–701.
Landon BE, Hicks LS, O’Malley AJ, Lieu TA, Keegan T, McNeil BJ, Guadagnoli E. Improving the management of chronic disease at community health canters. N Engl J Med. 2007;356:921–34.
Renders CM, Valk GD, Franse LV, Schellevis FG, vanEijk JT, van der Wal G. Long-term effectiveness of a quality improvement program for patients with Type 2 diabetes in general practice. Diab Care. 2001;24(8):1365–70.
Dearinger AT, Wilson JF, Griffith CH, Scutchfield FD. The effect of resident continuity on diabetes outcomes in a resident community clinic. J Gen Int Med. 2008.
Wennberg JE, Fisher ES, Baker L, Sharp S, Bronner K. Evaluating the efficiency of California providers in caring for patients with chronic illness. Health Aff. 2005;24(Suppl 3):526–4.
Davidoff F, Batalden P, Stevens D, Ogrinc G, Mooney S, SQUIRE development group. Publication guidelines for quality improvement in health care: evolution of the SQUIRE project. Qual Saf Health Care. 2008;17:i3–9.
Acknowledgements
This report employed the SQUIRE publication guidelines for reporting healthcare quality improvement research27. The national staff and faculty for both initiatives were supported in large measure by generous grants to the AAMC from the Robert Wood Johnson Foundation and the California HealthCare Foundation. In addition, the AAMC and the MacColl Institute provided in kind support for the Collaborative co-chairs (EW and DS) as well as additional administrative support. The Agency for Healthcare Research and Quality and Delmarva Foundation provided support for development of the web-based “Tool kit for developing the Chronic Care Model in an academic environment.”
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stevens, D.P., Bowen, J.L., Johnson, J.K. et al. A Multi-Institutional Quality Improvement Initiative to Transform Education for Chronic Illness Care in Resident Continuity Practices. J GEN INTERN MED 25 (Suppl 4), 574–580 (2010). https://doi.org/10.1007/s11606-010-1392-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1392-z