Abstract
Background
Bedside rounds have decreased in frequency on teaching services. Perceived barriers toward bedside rounds are inefficiency and patient and house staff lack of preference for this mode of rounding.
Objectives
To evaluate the impact of a bedside rounding intervention on the frequency of bedside rounding, duration of patient encounters and rounding sessions, and patient and resident attitudes toward bedside rounds.
Design
A pre- and postintervention design, with a bedside rounding workshop midway through two consecutive internal medicine rotations, with daily resident interviews, patient surveys, and an end-of-the-year survey given to all Medicine house staff.
Participants
Medicine house staff and medicine patients.
Measures
Frequency of bedside rounds, duration of new patient encounters and rounding sessions, and patient and house staff attitudes regarding bedside rounds.
Results
Forty-four residents completed the bedside rounding workshop. Comparing the preintervention and postintervention phases, bedside rounds increased from <1% to 41% (p < 0.001). The average duration of walk rounding encounters was 16 min, and average duration of bedside rounding encounters was 15 min (p = 0.42). Duration of rounds was 95 and 98 min, respectively (p = 0.52). Patients receiving bedside rounds preferred bedside rounds (99% vs. 83%, p = 0.03) and perceived more time spent at the bedside by their team (p < 0.001). One hundred twelve house staff (71%) responded, with 73% reporting that bedside rounds are better for patient care. House staff performing bedside rounds were less likely to believe that bedside rounds were more educational (53% vs. 78%, p = 0.01).
Conclusions
Bedside rounding increased after an educational intervention, and the time to complete bedside rounding encounters was similar to alternative forms of rounding. Patients preferred bedside rounds and perceived more time spent at the bedside when receiving bedside rounds. Medicine residents performing bedside rounds were less likely to believe bedside rounds were more educational, but all house staff valued the importance of bedside rounding for the delivery of patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Bedside rounds, the time-honored tradition of performing the activities of clinical care at the patient’s bedside, was the crux of medical education from the mid-17th century to the early 21st century1. By the 1960s, however, attending rounds occurred at the bedside 75% of the time, with a further decline to 16–20% by the late 1970s2–4. A more recent study has confirmed that bedside rounds occur an estimated 25% of the time5. In an era of resident work hour regulations, increased reliance on technology (e.g., electronic medical records), and the changing roles of inpatient attendings, medicine rounds have moved away from the bedside, occurring more often in hallways and conference rooms6. This downward trend in bedside teaching has raised concerns by medical education councils and medical educators about the teaching of clinical skills to trainees, prompting recommendations that residency training programs further incorporate bedside teaching into clinical curricula6–8.
A primary barrier to bedside rounding cited by physicians is time constraints9–11. One observational study showed that rounds including bedside encounters were significantly longer than rounds that did not include time spent at the bedside12. However, rounds at the bedside have distinct advantages, such as opportunities to teach physical diagnosis and model skills in communication and professionalism. Additionally, several studies have demonstrated that patients prefer case presentations at the bedside13–15; when these occur, patients perceive that their medical providers spend more time caring for them13–16. Generally, medicine residents and medical students have reported neutral preference for bedside rounds, but those who have had experience with bedside case presentations prefer this mode of rounding5,13,15. No study has directly investigated patient and house staff attitudes toward bedside rounds following an intervention aimed at increasing the occurrence of bedside rounds.
We implemented an educational program on bedside rounding for internal medicine house staff and encouraged the incorporation of bedside rounds into morning rounding sessions. We hypothesized the intervention would increase the frequency of bedside rounding. We also hypothesized that bedside rounding would (1) involve a similar amount of time compared to alternative forms of rounding per new patient encounter, (2) not lengthen the total duration of morning rounds, and (3) positively influence patient and resident attitudes toward bedside rounds.
METHODS
Study Design
We conducted this study on the inpatient internal medicine teaching service at the Beth Israel Deaconess Medical Center in Boston, a 556-bed, tertiary care teaching hospital. We implemented a bedside rounding intervention midway through two consecutive internal medicine rotations and compared the occurrence of bedside rounding before and after the intervention. We collected data on mode of rounding and time spent rounding through daily house staff interviews. We determined attitudes toward bedside rounds through patient interviews and a house staff survey. The study was approved by the institutional review board.
Medicine Service Structure and Intervention
During the two consecutive inpatient medicine blocks studied (December 2008 and January 2009), there were a total of 16 residents and 32 interns on service. Medicine teams consist of one junior or senior resident, two interns, and one or two third-year medical students. The blocks studied did not overlap with the winter holidays; thus, all teams were fully staffed during the study periods. Each team takes long call every 4th day with a maximum of 16-h shifts. The patients on a house staff team may have several different assigned attending physicians. The morning rounding sessions for each team are led by the resident with optional participation by the attending(s). The duration of rounds are not limited by scheduled teaching sessions or a fixed hour.
In lieu of a teaching attending session in the middle of each of the two blocks, an hour-long workshop was delivered to the house staff by the lead investigator (JG) on bedside rounding that covered the definition, history, advantages, and barriers to bedside rounds identified in the literature. The participants then viewed a video demonstrating a resident-led bedside rounding session developed for the purpose of the study and discussed the barriers to bedside rounds and methods to overcome them. Each resident was given a “Tips for Bedside Rounding” handout for future reference (Appendix I). After the intervention, the lead investigator sent a reminder e-mail to each team’s resident, encouraging them to perform bedside rounds during the last week of the rotation. An associate program director (CS) and a chief resident also sent one e-mail to the house staff encouraging their participation in the study. Aside from these two e-mails for each block, program leadership did not otherwise monitor resident participation.
Outcome Measures
Mode of Rounding, Duration of New Patient Rounding Encounters, and Duration of Morning Rounds
The outcome measures were mode of rounding on all patients, length of time spent on each rounding encounter with new patients, and total time spent on rounds. After the completion of rounds each day during the two rotation months, the lead investigator (JG) contacted the resident on each of the eight house staff teams to query the mode of rounding used for every patient encounter, the estimated time spent for each new patient rounding encounter, and total rounding time as a team. A patient was considered “new” for the first 2 days in which a team could potentially conduct morning rounds on that patient; this could be on hospital day 0, 1, or 2, Monday through Friday. For example, a patient admitted on Monday evening (day 0) would be considered a new patient during Tuesday (day 1) and Wednesday (day 2) morning rounds; a patient admitted in the early morning of Tuesday (day 0) would be considered a new patient during Tuesday (day 0) and Wednesday (day 1) morning rounds. We studied “new” patients because the majority of clinical decision making occurs early in the hospital course, and these inclusion criteria were similar to those in a prior study16. The mode of rounding was categorized as bedside rounds, walk rounds, or card flips. We defined bedside rounds as a minimum of two physicians (attending or house staff) performing all three of the following at the bedside in the presence of the patient: (1) case presentation/history, (2) performance of at least one physical exam skill, and (3) discussion of the patient’s daily plan of care. We defined walk rounds as any form of interaction with the patient by a minimum of two physicians that did not meet all three of the parameters above. For example, if only the history and exam were performed at the bedside, but the patient’s plan of care was discussed in an alternative location, this would classify as a walk round. Any form of rounding that did not include a patient interaction was defined as a card flip.
Patient Attitudes
Following the first study block (December 2008), the investigators decided to conduct patient interviews to assess attitudes toward bedside rounds. Therefore, during the second study block (January 2009), the lead investigator (JG) conducted structured face-to-face interviews with a convenience sample of new patients in both the pre- and postintervention periods to assess the patient’s perceived degree of respect offered to them from the medicine team, preference for bedside rounds, and perceived amount of time their physicians spent with them at the bedside. The question pertaining to respect was adapted from a previous study17; the other items were designed for the purposes of this study (see Appendix II). We pilot tested the interview contents with a sample of non-participating patients. Patients who agreed to participate consented to medical record review to ascertain age and length of hospital stay.
House Staff Attitudes
At the end of the academic year (June 2009), we asked all 158 house staff of the Beth Israel Deaconess Medicine Residency to participate in an anonymous online survey, regardless of whether they participated in the bedside rounding intervention conducted 6 months prior. Survey items assessed demographic data, participation in the bedside rounding intervention, and preference and perceptions about bedside rounds. We pilot tested the survey with a sample of staff physicians and chief residents.
Statistical Analysis
We analyzed data using Stata version 8 (StataCorp LP, College Station, TX). The descriptive characteristics and survey responses are presented. We used paired t-tests for comparison of means, chi-square analysis for frequencies (with Fisher’s exact test for samples less than 5), and the Kruskal-Wallis test for ratings on Likert-type scales.
RESULTS
House Staff Participants in Intervention
A total of 44 house staff participated during the two consecutive medicine blocks studied. Sixteen junior and senior residents and 28 interns were included, with 4 interns rotating on the inpatient service for the two consecutive blocks and thus receiving the workshop twice. Four house staff could not attend the workshop due to ambulatory clinic duties; they received a one-on-one session by the investigator (JG) at an alternative time prior to the bedside rounding week.
Mode of Rounding
We successfully contacted the senior resident on each medicine team after rounds every day during the study period to determine the mode of rounding for each patient. The average team census during the study was 9.4 patients (preintervention 9.3, postintervention 9.6). In the preintervention phase (15 work days), there were 1,104 total patient rounding encounters, with 273 new patient rounding encounters. In the postintervention phase (9 work days), there were 694 total patient rounding encounters, with 210 new patient rounding encounters. Comparing the preintervention and postintervention phases, the proportion of bedside rounds increased from <1% to 41% (p < 0.001) and walk rounds decreased from 47% to 16% (p < 0.001), while card flips decreased from 52% to 42% (p < 0.001). Reasons cited by residents for excluding patients (n = 53) from bedside rounds in the postintervention period included: breakdown of rounds because of clinic or unstable patients (n = 18), mental status changes (n = 9), “patient off of floor” (n = 2), language barrier (n = 1), and unexplored reasons (n = 23).
Duration of New Patient Rounding Encounters and Duration of Morning Rounds
The average duration of new patient encounters that involved walk rounds in the preintervention phase was 16 min (SD 0.73), and new patient encounters that involved bedside rounds in the postintervention phase was 15 min (SD 0.82, p = 0.42). The average time spent rounding as a team per day was 95 min (SD 16) during the preintervention period and 98 min (SD 17) during the postintervention period (p = 0.52).
Patient Attitudes
A total of 89 patients were interviewed, 71 in the preintervention period and 18 in the postintervention period (Table 1). Fewer patients were interviewed during the postintervention period due to a 4-day work week and availability of the interviewer to conduct interviews. The majority of patients strongly agreed with the statement that they would prefer their physicians to round at the bedside as a team during rounds. The preference for bedside rounds, as indicated by “somewhat agree” or “strongly agree,” was significantly greater in patients whose medical team performed bedside rounds compared to patients receiving walk rounds (99% vs. 83%, p = 0.03). When asked if the medicine team included them in the medical decision-making process, the proportion of patients who either “somewhat agreed” or “strongly agreed” did not differ in the pre- and postintervention phases (55% vs. 61%, p = 0.43). Both the pre- and postintervention groups of patients felt highly respected by their doctors, with 92% (65 of 71) and 94% (17 of 18) reporting a “moderate” or “significant” degree of respect offered to them by their medicine physicians (p = 0.67, Appendix II).
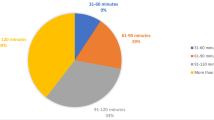
As shown in Figure 1, patients in the preintervention period perceived their medicine team was spending significantly less time with them compared with patients in the postintervention period (p < 0.001). Among the preintervention patients, 1% reported a minimum of 16 min spent at the bedside by their medicine team, compared with 44% of postintervention patients. Of note, 62% of preintervention patients and 0% of postintervention patients reported that less than 5 min was spent with them at the bedside.
Resident Survey
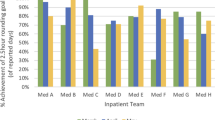
One hundred fifty-eight residents were invited to complete the online survey with 112 participating (71% response rate, Table 2). Thirty-two of the 44 house staff (73%) who participated in the intervention and 80 of the 114 house staff (70%) who did not participate in the intervention completed the survey. There was no statistical difference between educational intervention participants and non-participants regarding attitudes of bedside rounds offering patients “more dignity” or “preference for bedside rounds.” Seventy-three percent of house staff surveyed believed bedside rounds are better for patient care than alternative forms of rounding. In response to “Bedside rounds are more efficient,” 20 of 32 (63%) of intervention residents and 38 of 80 (48%) of residents who did not participate in the intervention reported they “somewhat agreed” or “strongly agreed” (p = 0.32). House staff experiencing the intervention were less likely to believe that bedside rounds were more educational (53% vs. 78%, p = 0.01).
DISCUSSION
Our study demonstrates that bedside rounding increases after an educational bedside rounding intervention. We found the time required to complete bedside rounds was similar to walk rounds, patients prefer bedside rounds and perceive more time spent at the bedside when their medicine teams round at the bedside, and medicine residents highly value the importance of bedside rounding for the delivery of patient care. An unexpected finding was that medicine residents who performed bedside rounds were less likely to believe bedside rounds were more educational than other forms of rounding.
The downward trend of bedside rounds was reaffirmed in our study, as the percentage of bedside rounds during the preintervention period was <1%. Through the educational intervention, with encouragement from program leadership, however, our resident physicians were given the opportunity to experience bedside rounds, allowing for this mode of rounding to be incorporated into their morning rounding sessions.
Our study shows that bedside rounding encounters involve a similar amount of time compared to walk rounds and the total daily rounding time does not change if bedside rounds are included. These findings refute the perceived barrier of “inefficiency” as cited by clinicians in prior studies9–11. No studies have identified time requirements for bedside rounding encounters, as in our study. At their institution, Crumlish et al. found that total daily rounding time was significantly longer when rounds also included time spent inside patient rooms12. In our study, we evaluated whether the time needed for bedside rounding (defined as case presentation, review of at least one physical exam skill, and discussion of patient’s daily plan of care in the presence of the patient) would be increased over time needed for walk rounds (when the team went into the patient’s room, but not all three of the above criteria were met)—it did not. Furthermore, the house staff performing bedside rounds in our study reported similar perceptions regarding “efficiency” as those not performing bedside rounds. These data suggest that the “inefficiency” of rounds may be more of a perceived barrier than a realistic one.
Our patients reaffirmed the sentiments of patients assessed in previous studies regarding their desire to have the medicine team at the bedside on internal medicine services13–16. But importantly, the patients in our study who experienced bedside rounds were significantly more likely to prefer bedside rounds and perceived more time spent at the bedside by their medicine team. Thus, our study provides further evidence that patients perceive benefits toward having medicine doctors at the bedside during rounds.
Less than half of all house staff preferred bedside rounds. Based upon experience in a prior study, we expected that more experience with bedside rounding would be associated with greater preference and positive attitudes toward bedside rounds, but this was not demonstrated5,13. In addition, it is unclear why house staff who participated in bedside rounding encounters do not believe bedside rounds are more educational for learners. For the house staff in our study, accomplishing the two goals of the bedside rounding encounter, i.e., the delivery of patient care and education for participants, may have been difficult during the initial phase of overcoming the inexperience and unknown barriers inherent in bedside rounding encounters. Despite their lack of personal preference, however, most house staff believed that bedside rounds were better for patient care, revealing that our primary caregivers on internal medicine floors believe that although not an easy task, bedside rounds may be better for patient care. Further exposure and practice to sharpen bedside rounding skills for house staff and faculty may have a positive impact on physician preferences for bedside rounds.
Several limitations should be acknowledged. This study was conducted at a single institution where rounds are largely resident-driven and during one point during the academic year, which may not be generalizable. Although we collected complete data on daily rounding behaviors within minutes of completion of rounds, this was subject to recall and social desirability bias. Our analysis did not account for differences in patient characteristics between the pre- and postintervention group, limiting the significance of these results. A small number of patients in the postintervention group were interviewed, which may have underpowered the results. Lastly, residents may have been more responsive to departmental encouragement to perform bedside rounds and subject to interviewer expectation effects, although these should not have directly impacted the reported duration of encounters or attitudes regarding bedside rounds.
As demonstrated by the fading occurrence of bedside rounding encounters, a patient care delivery system without the patient at the forefront of rounds has been perpetuated. The structure of internal medicine inpatient teaching services is in a period of transformation, with the changing nature of inpatient hospitalizations, work-hour regulations, and the increasing reliance on hospitalists, who are generally younger faculty with less experience with teaching at the bedside12. Balancing multiple tasks, which include the delivery of clinical care and education, all in the context of patient-centeredness, can be a challenge for even the most experienced clinicians, let alone for inexperienced faculty and residents. Despite the paucity of literature showing improved outcomes from bedside rounds, we should consider the possible ramifications on our future physicians and our family members receiving care within this system. A prerequisite of teaching “bedside manner” to our learners requires our physicians practice medicine where these skills can be modeled—at the bedside with the patient. A larger, multi-centered study may further clarify why the house staff who performed bedside rounds were less likely to believe this method of rounding is more educational.
References
Osler W. On the need of radical reform in our methods of teaching senior residents. Medical News. 1903;(82):49-53.
Linfors EW, Neelon FA, Sounding Boards. The case of bedside rounds. N Engl J Med. 1980;303(21):1230–1233.
Thayer W. Osler the Teacher. Bull Johns Hopkins Hospital. 1919.;30(303):198-200 (1980; 1303:1230-1983).
Collins GF, Cassie JM, Daggett CJ. The role of the attending physician in clinical training. J Med Educ. 1978;53(5):429–431.
Gonzalo JD, Masters PA, Simons RJ, Chuang CH. Attending rounds and bedside case presentations: medical student and medicine resident experiences and attitudes. Teach Learn Med. 2009;21(2):105–110.
Verghese A. Culture shock--patient as icon, icon as patient. N Engl J Med. 2008;359(26):2748–2751.
Ramani S. Twelve tips to improve bedside teaching. Med Teach. 2003;25(2):112–115.
Alpert JS. Some thoughts on bedside teaching. Am J Med. 2009;122(3):203–204.
Ramani S, Orlander JD, Strunin L, Barber TW. Whither bedside teaching? A focus-group study of clinical teachers. Acad Med. 2003;78(4):384–390.
Williams KN, Ramani S, Fraser B, Orlander JD. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257–264.
Nair BR, Coughlan JL, Hensley MJ. Impediments to bed-side teaching. Med Educ. 1998;32(2):159–162.
Crumlish CM, Yialamas MA, McMahon GT. Quantification of bedside teaching by an academic hospitalist group. J Hosp Med. 2009;4(5):304–307.
Rogers HD, Carline JD, Paauw DS. Examination room presentations in general internal medicine clinic: patients’ and students’ perceptions. Acad Med. 2003;78(9):945–949.
Romano J. Patient's attitude and behavior in ward round teaching. J Am Med Assoc. 1941;(117):664-667.
Wang-Cheng RM, Barnas GP, Sigmann P, Riendl PA, Young MJ. Bedside case presentations: why patients like them but learners don’t. J Gen Intern Med. 1989;4(4):284–287.
Lehmann LS, Brancati FL, Chen MC, Roter D, Dobs AS. The effect of bedside case presentations on patients’ perceptions of their medical care. N Engl J Med. 1997;336(16):1150–1155.
Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity in the terminally ill: a cross-sectional, cohort study. Lancet. 2002;360(9350):2026–2030.
Birnbaumer D, MD, FACEP. Bedside Teaching, The Teaching Microskills, and the Teachable Moment. [Online powerpoint presentation.]; 2007. www.acep.org.
Aldeen AZ, Gisondi MA. Bedside teaching in the emergency department. Acad Emerg Med. 2006;13(8):860–866.
Weinholtz D, Edwards JC, Mumford LM. Teaching during rounds: a handbook for attending physicians and residents. Baltimore: Johns Hopkins University Press; 1992.
Acknowledgements
The authors would like to thank Dr. Shoshana Herzig for assistance with survey design and implementation. Also, the authors would like to thank the Internal Medicine residents of the Beth Israel Deaconess Medical Center for their dedication to patient care and their willingness to contribute to this study. The project was presented, in part, as an oral presentation at the SGIM Annual Meeting, Miami, FL, May 15, 2009.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix I
”Tips for Bedside Rounding” Handout18–20
Before Rounding Session:
-
Prepare for patient cases before rounds
-
Decide with team which patients are appropriate for bedside rounds
-
Orient learners—ensure everyone knows what is expected of them
-
Prepare patients prior to rounds, when possible
-
Invite patient’s nurse if feasible
During Rounding Session:
-
Have patient’s doctor (resident, student, etc.) introduce all members of the team
-
Orient patient and learners—encourage patient to correct/contribute to details
-
Position patient appropriately; position team around bedside
-
Do not avoid sensitive material
-
Allow interruptions by patient and learners
-
Examine pertinent or illustrative parts−invite students to participate
-
Discuss events, labs, assessment, plan
-
Challenge intellectually with open-ended questions
-
Use “teachable moments” when available
-
Teach to all levels of learners and encourage all to participate
-
“I don’t know” is an appropriate answer
-
Communicate and summarize plan for patient and team
After Rounding Session:
-
Debrief sessions when appropriate
-
Offer time to clarify questions or address remaining issues after session
-
Offer feedback to reinforce positive skills demonstrated at bedside
Appendix II
Patient Survey Items.
-
1.
Introductory statements:
-
For patients not receiving bedside rounds: “Your Medicine team of doctors discussed your case outside of your room, then updated you about the plan.”
-
For patients receiving bedside rounds: “Your Medicine team of doctors discussed your case at the bedside in your presence.”
-
2.
What is your ethnic background (circle one):
-
Black/African-American
-
White
-
Asian
-
Other
-
3.
Which language do you consider your primary language?
-
English
-
Spanish
-
Russian
-
Other
-
4.
“In reference to the degree of respect your medicine team showed during your stay, please choose:”
-
a.
Significant Gain of Respect—respect almost always demonstrated
-
b.
Moderate Gain of Respect—most of the time, I was treated with respect
-
c.
Mild Gain of Respect—I often experienced a sense of respect
-
d.
No sense of loss or gain of respect
-
e.
Mild Loss of Respect—I often experienced low-grade loss of respect
-
f.
Moderate Loss of Respect—almost most of the time, I had concerns about disrespectful behavior
-
g.
Significant Loss of Respect—sense of loss of respect was almost always present
-
5.
Please comment on the statement: “Your Medicine team used confusing terms.”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
6.
Please comment on the statement: “I would prefer my medicine team of doctors to round as a team at the bedside during morning rounds”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
7.
Please comment on the statement: “My medicine team involved me with medical decisions.”
-
strongly agree
-
somewhat agree
-
neutral
-
disagree
-
strongly disagree
-
8.
How many minutes per morning were at least two of your physicians together at the bedside with you?
-
zero minutes
-
1 to 5 minutes
-
6 to 10 minutes
-
11 to 15 minutes
-
16 to 20 minutes
-
21-25 minutes
-
25+ minutes
Rights and permissions
About this article
Cite this article
Gonzalo, J.D., Chuang, C.H., Huang, G. et al. The Return of Bedside Rounds: An Educational Intervention. J GEN INTERN MED 25, 792–798 (2010). https://doi.org/10.1007/s11606-010-1344-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-010-1344-7