Abstract
BACKGROUND
Alcohol screening and brief intervention (BI) is an effective primary care preventive service, but implementation rates are low. Automating BI using interactive voice response (IVR) may be an efficient way to expand patient access to needed information and advice.
OBJECTIVE
To develop IVR-based BI and pilot test it for feasibility and acceptability.
DESIGN
Single-group pre-post feasibility study.
PARTICIPANTS
Primary care patients presenting for an office visit.
INTERVENTIONS
IVR-BI structured to correspond to the provider BI method recommended by NIAAA: (1) Ask about use; (2) Assess problems; (3) Advise and Assist for change, and (4) Follow up for continued support. Advice was tailored to patient readiness and preferences.
MEASUREMENTS
Utilization rate, call duration, and patients’ subjective reports of usefulness, comfort and honesty with the IVR-BI. Pre-post evaluation of motivation to change and change in alcohol consumption as measured by Timeline Follow Back.
RESULTS
Call duration ranged from 3–7 minutes. Subjective reactions were generally positive or neutral. About 40% of subjects indicated IVR-BI had motivated them to change. About half of the patients had discussed drinking with their provider at the visit. These tended to be heavier drinkers with greater concerns about drinking. Patients who reported a provider-delivered BI and called the IVR-BI endorsed greater comfort and honesty with the IVR-BI. On average, a 25% reduction in alcohol use was reported two weeks after the clinic visit.
CONCLUSIONS
Using IVR technology to deliver BI in a primary care setting is feasible and data suggest potential for efficacy in a larger trial.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
BACKGROUND
Alcohol screening and brief intervention (BI) is ranked among the highest priority preventive services by the National Commission on Prevention Priorities, based on their index of cost effectiveness and clinically preventable burden1 and is recommended by the US Preventive Services Task Force2. There is considerable evidence of its efficacy to reduce alcohol consumption up to four years following the intervention3–7; however, only about one-third of primary care patients are screened for substance misuse by their providers (PCPs)8,9. Furthermore, biases in the delivery of BI mean that the intervention is more likely to occur with a narrow spectrum of patients, i.e. those who are male, unemployed, less educated, and/or earn lower income10–12.
Barriers to routine screening and BI include lack of established organizational support systems, lack of reimbursement for preventive interventions, heavy workloads, PCP reluctance to address non-acute behavioral problems, and PCP lack of confidence or skill discussing alcohol problems9,13,14. While many of these barriers have proven intractable to targeted training13, there is early evidence that they may be circumvented through the use of systematic and automated approaches to screening. For example, web-based alcohol interventions have been created for a variety of audiences and have demonstrated user acceptability and efficacy15,16. An alternative modality for automating BI that has not been tested to date is telephone interactive voice response (IVR) technology. IVR has been used successfully for alcohol use assessment17,18, alcohol self-monitoring19–21, symptom reporting22–24, post-BI alcohol monitoring and feedback25; smoking cessation26, and supplemental case management in substance abuse treatment27.
IVR systems offer cost and other significant advantages for primary care settings. Importantly, IVR is an auditory interactive process that is not hampered by low literacy. Privacy and anonymity are greater with an IVR than on a computer screen or written questionnaire because others cannot see or hear the questions or responses, even if others are present at the time of the call. Touch tone phones are familiar, easy to use, and more widely available than computers. Furthermore, the hardware and software of a centrally-housed IVR system can support multiple clinic sites and thus there are no on-site installation costs beyond telephone access.
OBJECTIVE
The goal of this study was to develop an IVR-based BI (IVR-BI) and pilot test it for feasibility and patient acceptability.
METHODS
Participants and Procedures
Recruitment took place in a suburban, university-affiliated primary care internal medicine office with eight providers. This busy office was short staffed at the time of recruitment, so it was not possible to invite every clinic patient to participate. In designing a process to identify the subset of patients who would be candidates for the study, the following were the primary considerations: (1) to avoid bias in selection of participants and (2) to minimize the effect of the study on the flow of patients through the office. The procedures were as follows: the evening before each clinic day, the practice supervisor selected a priori the subset of patients who would be invited to participate the following day. Certain visit types/ patients were excluded from the recruitment pool: new patient visits, acute illness visits, severe mental health disorder follow-ups, patients (very limited in number) who were known to be belligerent who would refuse and might cause a disturbance in the waiting area, and very elderly patients or those with impaired vision. Additionally, four patients per half-day were selected, each of whom was scheduled to see a different provider. Otherwise, the selection of patients was random. The clinic supervisor marked on the schedule which patients were to be invited, and the receptionist followed a protocol for inviting them. All selected patients were invited to make a brief call using a dedicated waiting room phone to answer five screening questions (the IVR-screen) in preparation for the office visit. Patients were told that they and their PCP would receive a printout of their answers before the examination, and that participation was voluntary.
The IVR-screen (See online Appendix) was developed by the authors, pilot-tested on a sample of 119 patients, and revised for use in this study. Alcohol use was assessed with two items, either one of which qualified the respondent for the IVR-BI. The question, “In general, do you feel you drink more than you should?” was asked first because the PCPs at the clinic site were accustomed to this as a general question regarding readiness to engage on the topic of alcohol use. Responses of “yes” or “not sure” were scored positive. The second question, “How often do you have five (four for women) or more drinks on one occasion?” is taken directly from the World Health Organization’s Alcohol Use Disorders Identification Test28, as revised by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) to reflect standard drink sizes in the United States29. Any response other than “never” was scored positive, in accordance with NIAAA guidelines.
At the end of the IVR-screen, those who screened positive heard the following: “The amount of alcohol you are drinking can affect your health and interfere with some medical treatments.” The IVR then alerted them that in the privacy of the examination room the Medical Assistant (MA) would invite them to test a “Health Information Line” (the IVR-BI) that provides information and advice about drinking and health. In the exam room, the MA obtained written informed consent, provided a card with the toll free IVR-BI number, and asked the subjects to call within 48 hours. The MA explained this was voluntary and, whether or not they called the IVR-BI, a member of the research team would be contacting them to ask follow-up questions. The patient then remained in the exam room for the PCP. The PCPs received a printout of screening items, but they otherwise were neither encouraged to nor discouraged from conducting an in-office BI with study participants. All study procedures were approved by the University of Vermont Institutional Review Board.
Intervention
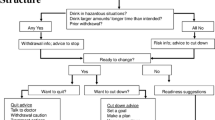
The IVR-BI begins with an introductory description of the program and its purpose, a reminder that it is part of a research project, assurance of privacy and confidentiality, and a request for callers to enter the personal ID number given by the MA. The IVR-BI content is based on NIAAA29 recommendations for an alcohol brief intervention by a PCP (see Fig. 1). The “Ask” element was accomplished with the two alcohol items in the IVR-screen that the patient completed in the waiting room; the remaining 3 elements are covered in the IVR-BI. The “Assess” phase is accomplished using the three AUDIT-C questions about quantity, frequency and heavy episodic consumption of alcohol30. The “Advise/Assist” section first gives the NIAAA safe-drinking guidelines of no more than 14 drinks per week and fewer than 5 drinks on one occasion for men, and the corresponding 7 per week, fewer than 4 per occasion for women. This section then assesses the caller’s readiness to change their drinking and offers three “Readiness Suggestions” to those who are not currently ready to change. Callers who endorse readiness to change can then choose to hear guidance and suggestions for either cutting down or for stopping alcohol consumption. Advice for cutting down includes goal-setting, planning for urges and high-risk situations, proactive avoidance of triggers, self-monitoring, and other strategies. The advice is voiced by different characters speaking in the first person so as to maintain the listener’s interest. Advice to abstain describes treatment and mutual-help models commonly used to achieve abstinence, and includes information on local support and treatment resources. For all callers, the IVR-BI ends with a section on “Follow-up Support”: callers are encouraged to talk with their PCP about their alcohol use and to call the IVR-BI again at any time. The full text of the IVR-BI can be obtained from the authors.
Measurements
Two follow-up telephone assessments were conducted at approximately one and two weeks following the clinic visit by a research assistant (RA) who was not involved with patient care. The RA employed a structured interview that was developed by the research team and tested in a pilot study. It included a mixture of question formats. The interviewer recorded participant responses verbatim, and each response was coded according to a scheme developed after the pilot test that reflected possible respondent options.
The first call elicited feedback about the patient’s visit with the PCP as well as their subsequent call to the IVR-BI. The RA ascertained patients’ recollections of whether or not they had discussed their drinking with their PCPs during the office visit. If so, the patient was asked whether the conversation was initiated by the provider or by the patient, and whether it made them more aware of how much they drink. On this basis, we classified patients as either having or not having a brief intervention by the provider (i.e., PCP-BI). Patients were also asked to compare the PCP-BI with the IVR-BI in terms of personal usefulness, comfort with the process, and their honesty in answering questions. Patients who did not discuss drinking with their PCP were asked to hypothetically evaluate the expected usefulness, comfort, and honesty with a PCP-BI compared with the IVR-BI. The interviewer also assessed patients’ general reactions to the IVR-BI, the personal relevance of the information it contained, the impact of the information on their drinking-related attitudes or behavior, and suggestions for improvements in the IVR-BI.
The first follow-up interview also included a timeline follow back (TLFB)31 assessment of daily alcohol consumption covering the period of time from 2 weeks prior to the clinic visit up through the day before the telephone interview. The second follow-up interview, conducted an average of 16 days following the clinic visit, consisted of a second TLFB assessment covering the period of time from the clinic visit through the day before the second telephone interview.
ANALYSIS
Analyses were primarily descriptive to assess subject experience with the IVR-BI. Inferential analyses were based on chi square tests for categorical variables and paired t-tests to evaluate changes in self-reported drinking.
RESULTS
Feasibility of Screening
A total of 188 patients completed the IVR-screen, and 83 (44%) of them screened positive for at-risk drinking. Of the 83 subjects who endorsed either of the screening questions, 82 were positive on the frequency of five (four) or more drinks question and just 19 were positive on the “feel you drink more than you should” item. All but one of the 19 were also identified by the frequency question, but those who endorsed that they “feel they drink more than they should” were more likely than those who did not to later call the IVR-BI [12/19 (63%) vs 21/63 (33%), χ2 = 5.4, p = .02].
Utilization of IVR-BI
Of the 83 who screened positive, 61 (73%) consented to the IVR-BI study. Of those consenting, 34 (56%) completed the IVR-BI. Participants called The IVR-BI at varying times throughout the day, except between 2 AM and 7 AM. One-third of all calls were made outside of regular clinic hours. Call duration ranged from 3 to 7 minutes depending on the number of features the subject chose. Eight of the 34 subjects endorsed interest in changing their drinking habits. These patients proceeded to the “Advice” section where they could choose to hear information about cutting down and/or quitting. Five elected to hear the cut down information and two elected to hear the quit information. One caller listened to both sections.
IVR-BI and PCP-BI
Thirty patients (17 male/13 female) with mean age 43 years completed the IVR-BI and both follow-up interviews. The following analyses are based on data from these subjects. About 45% (n = 13) of the 30 respondents stated they had discussed drinking with their PCP during the office visit, with 9 of the 13 noting that the PCP had initiated the discussion. We compared those who had received PCP-BI with those who had not, although PCP-BI occurred in a non-random fashion. Regardless of PCP-BI, all 30 subjects completed the IVR-BI and both follow-up interviews. Heavier drinkers were more likely to report they had a PCP-BI [Mantel-Haenszel χ2 = 19.2, p < 0.001]; all ten patients who indicated they drank more than 5(4) drinks per occasion on either a daily or weekly basis reported having a BI from the PCP, whereas just one of 15 (7%) who endorsed this quantity “less than monthly” received a PCP-BI. All patients who endorsed drinking more than they should (n = 8) received a PCP-BI.
About half of those who had a PCP-BI (7/13) said the discussion made them more aware of how much they drink, whereas 82% of those who did not have PCP-BI said the IVR-BI made them more aware of how much they drink. Five subjects said the discussion with the PCP was more useful than the IVR-BI, 5 said the reverse was true, and 3 were not sure. We asked respondents about their comfort level for receiving the information by phone versus their PCP. Of those who had a PCP-BI, 50% were more comfortable with the IVR-BI, 25% were more comfortable with the PCP-BI, and 25% were equally comfortable. Regarding honesty of responses, 83% reported they were equally honest with IVR or PCP and 17% said they were more honest with the IVR. None said they were more honest with their PCP. For those who did not report receiving a PCP-BI (n = 17), 53% hypothetically said they would be more honest with the IVR, while 12% said they would be more honest with their PCP. The remaining 35% said equal or not sure.
Change in Alcohol Consumption
In the assessment section of the IVR-BI, 24% of participants indicated they were interested in changing their drinking habits. However, at the first follow-up interview, 40% said the IVR-BI had motivated them to make a change in their drinking. Overall, the TLFB data show mean drinks per week decreased 25%, from 8.7 (SD = 12.1) before to 6.5 (SD = 10.6) two weeks after the office visit (paired-t = 1.63, p = 0.11). TLFB data for the 17 individuals who did not receive a PCP-BI (i.e., IVR-BI only) showed a decrease from 4.3 (SD = 8.2) drinks per week before the visit to 2.5 (SD = 2.6) drinks per week after (42% reduction, paired-t = 0.9, p = 0.40) Those who received a PCP-BI and an IVR-BI (n = 13) decreased from 14.4 (SD = 14.3) drinks per week before the visit to 11.7 (SD = 14.5) drinks per week after (19% reduction, paired t = 1.75, p = 0.10).
DISCUSSION
This pilot study demonstrated that an IVR-based screening and brief intervention system for at-risk drinking was both feasible in a busy primary care office setting and acceptable to patients. Compared with a PCP-BI, the IVR-BI was perceived to be at least as useful, and patients reported being at least as comfortable and as honest with the IVR-BI as they were with their PCPs.
Patient willingness to complete the IVR-BI was particularly important because fewer than half of patients who screened positive for possible alcohol misuse received a brief intervention from their PCP during the clinic visit. Furthermore, one-third of the calls to IVR-BI were made outside of clinic hours. Clearly, the IVR-BI produced greater exposure to needed advice and information than would have occurred otherwise.
The strengths of the IVR-BI approach are that it can be accomplished in a way that is minimally disruptive to the office workflow, can prompt patient and PCP to act, is scalable to large populations, and once it is developed is inexpensive to deploy. In this study, the IVR was programmed by a commercial vendor for an initial set-up fee then hosted for a monthly fee thereafter. Calls to the toll-free number can be received from any location so theoretically the same IVR system can support an infinite number of practices. Interference with clinic routine could be avoided altogether if the IVR-screen and IVR-BI were completed prior to the visit, for example at the time of pre-registration or appointment reminder call. If this were to occur, relevant IVR data could be merged with an electronic medical record or other pre-visit paperwork process, and the information from the IVR-BI made available to the PCP at the time of the visit to facilitate further discussion.
This study has some limitations. Since this was designed as a feasibility study, the sample was drawn from a single clinic and there was no control group. Recruitment to the study required clinic staff to spend extra time to explain the study; thus the number of patients who could participate was limited. Certain patients were excluded from the recruitment pool because of the reason for the visit or their own physical/ cognitive limitations, which affects the generalizability of findings to the entire clinic population or to other settings or populations. The impact of volunteer bias on the results is not known.
Among this sample of patients who completed the IVR-BI and two follow-up interviews, 45% reported they had discussed their drinking with the PCP during the visit. We do not interpret this to mean that 45% of screen-positive patients received PCP-BI (a much higher rate than that reported in the literature) because our sample of 30 patients only represents 16% of patients screened for the study. However, it is possible that the provider intervention rate for this study was higher than it might have been because providers were aware that the study was going on. As part of the study, patients were screened and results of the screen were prominently displayed on the patients’ charts. Also, the providers in this clinic all had received training in BI within the past 6 years.
The study was not designed or powered to evaluate the impact of the IVR-BI on alcohol consumption. However, we do have some evidence of a possible therapeutic effect. First, 40% of respondents indicated in the exit interview that the IVR-BI had motivated them to change their drinking. Second, we observed a substantial but non-significant decline in consumption during the two weeks after the clinic visit in subjects who did and did not receive a BI from their PCP. These results suggest a larger controlled trial is warranted.
CONCLUSIONS
Screening and brief intervention using interactive voice response technology is feasible in a primary care setting. Given that this pilot has shown acceptability and feasibility, our next goal is to examine clinical efficacy of the IVR-BI. If an IVR-BI proves efficacious, it is conceivable that it would be accepted as a reimbursable service.
References
Maciosek MV, Edwards NM, Coffield AB, Flottemesch TJ, Nelson WW, Goodman MJ. Solberg, ML. Priorities among effective clinical preventive services: methods. Am J Prev Med. 2006;31(1):90–6.
US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140(7):554–6.
Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88(3):315–36.
Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002;26(1):36–43.
Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. [Review] [93 refs]. Cochrane Database Syst Rev. 2007;(2):CD004148.
Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279–92.
Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557–68.
National Center on Addiction and Substance Abuse (CASA). Missed opportunity: CASA national survey of primary care physicians and patients on substance abuse. New York: Columbia University; 2000.
Spandorfer JM, Israel Y, Turner BJ. Primary care physicians' views on screening and management of alcohol abuse: inconsistencies with national guidelines. J Fam Pract. 1999;48(11):899–902.
Kaner EF, Heather N, Brodie J, Lock CA, McAvoy BR. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br J Gen Pract. 2001;51(471):822–7.
Lock CA, Kaner EF. Implementation of brief alcohol interventions by nurses in primary care: do non-clinical factors influence practice? Fam Pract. 2004;21(3):270–5.
Volk RJ, Steinbauer JR, Cantor SB. Patient factors influencing variation in the use of preventive interventions for alcohol abuse by primary care physicians. J Stud Alcohol. 1996;57(2):203–9.
Beich A, Gannik D, Malterud K. Screening and brief intervention for excessive alcohol use: qualitative interview study of the experiences of general practitioners. BMJ. 2002;325(7369):870–4.
McCormick KA, Cochran NE, Back AL, Merrill JO, Williams EC, Bradley KA. How primary care providers talk to patients about alcohol: a qualitative study. J Gen Intern Med. 2006;21(9):966–72.
Bewick BM, Trusler K, Barkham M, Hill AJ, Cahill J, Mulhern B. The effectiveness of web-based interventions designed to decrease alcohol consumption-a systematic review. Prev Med. 2008;47(1):17–26.
Kypri K, Langley JD, Saunders JB, Cashell-Smith ML, Herbison P. Randomized controlled trial of web-based alcohol screening and brief intervention in primary care. Arch Intern Med. 2008;168(5):530–6.
Perrine MW, Mundt JC, Searles JS, Lester LS. Validation of daily self-reported alcohol consumption using interactive voice response (IVR) technology. J Stud Alcohol. 1995;56:487–90.
Searles JS, Helzer JE, Walter DE. Comparison of drinking patterns measured by daily reports and timeline follow back. Psychol Addict Behav. 2000;14(3):277–86.
Helzer JE, Badger GJ, Rose GL, Mongeon JA, Searles JS. Decline in alcohol consumption during two years of daily reporting. J Stud Alcohol. 2002;63(5):551–8.
Mundt JC, Moore HK, Bean P. An interactive voice response program to reduce drinking relapse: a feasibility study. J Subst Abuse Treat. 2006;30(1):21–9.
Tucker JA, Foushee HR, Black BC. Behavioral economic analysis of natural resolution of drinking problems using IVR self-monitoring. Exp Clin Psychopharmacol. 2008;16(4):332–40.
Forster AJ, Boyle L, Shojania KG, Feasby TE, van Walraven C. Identifying patients with post-discharge care problems using an interactive voice response system. J Gen Intern Med. 2009;24(4):520–5.
Kranzler HR, Abu-Hasaballah K, Tennen H, Feinn R, Young K. Using daily interactive voice response technology to measure drinking and related behaviors in a pharmacotherapy study. Alcohol Clin Exp Res. 2004;28(7):1060–4.
Simpson TL, Kivlahan DR, Bush KR, McFall ME. Telephone self-monitoring among alcohol use disorder patients in early recovery: a randomized study of feasibility and measurement reactivity. Drug Alcohol Depend. 2005;79(2):241–50.
Helzer JE, Rose GL, Badger GJ, Searles JS, Thomas CS, Lindberg SA, et al. Using interactive voice response to enhance brief alcohol intervention in primary care settings. J Stud Alcohol Drugs. 2008;69(2):251–8.
Reid RD, Pipe AL, Quinlan B, Oda J. Interactive voice response telephony to promote smoking cessation in patients with heart disease: a pilot study. Patient Educ Couns. 2007;66(3):319–26.
Hall JA, Huber DL. Telephone management in substance abuse treatment. Telemed J E Health. 2000;6(4):401–7.
Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT-The alcohol use disorders identification test$ Guidelines for use in primary health care. 2nd ed. Geneva: World Health Organization; 2001.
National Institute of Alcohol and Alcohol Abuse. Helping Patients With Alcohol Problems: A Clinician’s Guide. Bethesda: NIH: the Institute; 2005.
Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–17.
Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, eds. Measuring alcohol consumption: Psychosocial and biochemical methods. Totowa: Humana Press; 1992:41–72.
Acknowledgements
We gratefully acknowledge the assistance of Megan Malgeri in gathering the IVR-screen pre-test data.
We also would like to thank Dee Scheidel and all the staff at Given Essex for collaborating on this study.
This research was supported by NIAAA grant 1 R21 AA015777-01A1.
An abstract of this study was presented at a poster session at the Society of General Internal Medicine annual meeting, Miami, FL, May, 2009. This research was also presented as part of a symposium at the Research Society on Alcoholism annual meeting, San Diego, CA, June, 2009.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 37 kb)
Rights and permissions
About this article
Cite this article
Rose, G.L., MacLean, C.D., Skelly, J. et al. Interactive Voice Response Technology Can Deliver Alcohol Screening and Brief Intervention in Primary Care. J GEN INTERN MED 25, 340–344 (2010). https://doi.org/10.1007/s11606-009-1233-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1233-0