Abstract
Background
Disparities can be caused by minorities receiving care in low-quality settings. The patient-centered medical home (PCMH) has been identified as a model of high-quality primary care that can eliminate disparities. However, Latinos are less likely to have PCMHs.
Objective
To identify Latino subgroup variations in having a PCMH, its impact on disparities, and to identify factors associated with Latinos having a PCMH.
Design
Analysis of the 2005 MEPS Household Component, a nationally representative survey with an oversample of Latino adults. The total sample was 24,000 adults, including 6,200 Latinos.
Measurements
The PCMH was defined as having a regular provider, who provides total care, fosters patient engagement in care, and offers easy access to care. Self reports of preventive care (cholesterol screening, blood pressure check, mammography, and prostate-specific antigen screening) and patient experiences were examined.
Results
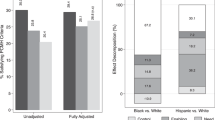
White (57.1%) and Puerto Rican (59.3%) adults were most likely to have a PCMH, while Mexican/Mexican Americans (35.4%) and Central and South Americans (34.2%) were least likely. Much of the disparity was caused by lack of access to a regular provider. Respondents with a PCMH had higher rates of preventive care and positive patient experiences. Disparities in care were eliminated or reduced for Latinos with PCMHs. The regression models showed private insurance, which is less common among all Latinos, was an important predictor of having a PCMH.
Conclusions
Eliminating health-care disparities will require assuring access to the PCMH. Addressing differences in health-care coverage that contribute to lower rates of Latino access to the PCMH will also reduce disparities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
BACKGROUND
Research on causes of disparities shows that providers, such as hospitals and physicians, who care for minorities tend to be lower performing, and deliver lower quality care, than those caring for the general population.1–4 Other work to identify racial disparities in care within hospitals has found very few if any differences in quality delivered to minority patients versus white patients.3,5 Thus, disparities are often caused across settings by minorities receiving care in low-quality settings, as opposed to being treated differently by health-care providers within settings. This indicates health-care disparities can be eliminated by improving quality in settings caring for large numbers of minority patients. In fact, a recent national survey showed when minorities have access to high quality primary care, as is offered in the patient-centered medical home, they experience no disparities in access, preventive care, or chronic disease care.6
The central tenet of the patient-centered medical home (PCMH) is care is focused on the patients’ needs rather than the providers’.7 The Joint Principles of the Patient-Centered Medical Home state the PCMH includes having a personal physician who provides first contact care that is continuous, comprehensive, and accessible, while being coordinated with the care offered by other providers.8 From the patients’ perspective this means having a regular provider who knows them well, timely access to well-coordinated care, patient engagement, and shared decision making. Successful PCMH providers have information systems for decision support, care coordination, and continuous quality improvement for patients and their families.8,9 Preliminary evidence indicates primary care delivered via the PCMH model leads to better clinical outcomes and patient experiences at a reduced cost.10–14 Unfortunately, the PCMH is not equally available to all. Latinos report the lowest rates of access to a PCMH among all racial/ethnic groups (15% of Latinos vs 28% of whites).6 It is not known whether there are Latino subgroup differences in access to the PCMH. The purpose of this project was to determine whether there are Latino subgroup variations in having a PCMH, assess whether disparities in preventive care and patient experiences are reduced in the PCMH, and determine what factors are associated with Latinos having a PCMH as their source of primary care.
METHODS
Data
The Medical Expenditure Panel Survey (MEPS) is a large nationally representative survey designed to provide estimates of health-care utilization of the US civilian, non-institutionalized population. Conducted by the Agency for Healthcare Research and Quality (AHRQ), the MEPS survey includes an oversample of Black and Latino households and has the statistical power to accurately examine health-care questions in those populations. Data for these analyses come from the 2005 Household Component that contains detailed information on self-reported patient demographics, health conditions, health status, access to care, health insurance coverage, utilization, and patient satisfaction.15 The total sample for our study consisted of 25,000 adults aged >18, including 6,200 Latinos. All estimates were weighted to reflect the complex survey design of MEPS and to provide unbiased national estimates.
Definition of the Medical Home
Most measures of the PCMH rely on organizational self assessments by providers and are based on structural and process measures such as having IT systems to monitor and track patients.16,17,19 However, patient reports of practice characteristics and their experiences with care have been used to develop robust indicators of medical home practices.18
Using MEPS data, we determined whether respondents had a PCMH based on the following indicators: (1) having a regular provider; (2) their provider’s role in total care for the patient (i.e., new health problems, preventive health care, ongoing health problems, and referrals to other health professionals); (3) patient engagement in care (provider asks about medications and treatments prescribed by other doctors or asks respondent to help decide treatment); (4) care accessibility (able to contact their provider during regular business hours, at night or on weekends).
We developed four different methods for aggregating these items to create a medical home variable and conducted sensitivity testing to determine how the different methods functioned for being able to detect differences in respondents’ ratings of their health care. We also included measures for the medical home variable based on face validity, specifically requiring that a medical home provides total care for the patient (i.e., new health problems, preventive health care, ongoing health problems, and referrals to other health professionals) and includes a specific person who cares for the patient. Using the items listed above, respondents were categorized into three groups: (1) having a medical home (those who said yes to all assessed indicators); (2) having a regular source of care that is not a medical home (those with a regular source of care who said no to any of the other indicators); (3) having no regular source of care (those who reported no regular source of care).
Identification of Latino Respondents and Latino Subgroups
Respondents were categorized into their ethnic groups based on three questions: whether they were Latino, their ethnicity, and their race. All respondents who identified as Latino were then classified into Latino subgroups based on their ethnicity. The remaining non-Latino respondents were then classified into their self-reported racial groups. All analyses were conducted comparing whites and the Latino subgroups with at least 300 respondents. These were Mexican/Mexican Americans, Puerto Ricans and Central/South Americans.
Preventive Care Measures
We used four measures to assess rates of preventive care among the respondents. These were self reports of: (1) cholesterol screening in the past 2 years, (2) blood pressure check in the past 2 years, (3) mammography screening in the past 2 years for women age 30 and older, and (4) prostate-specific antigen (PSA) screening in the past 2 years for men age 40 and older.
Patient Experiences With Care
Our assessments of patient experiences with care were based on responses of “always or usually” relative to “sometimes or never” when asked how often have your providers: (1) explained things so you understood, (2) listened carefully to you, (3) spent enough time with you, and (4) showed respect for what you had to say.
Demographic Measures
The demographic measures were all based on self report and included age, sex, and income level. Categories for insurance status were no coverage at the time of the interview, having any private insurance (including those with both private and public coverage such as Medicare), or having only public insurance (including those with just Medicare but no supplemental insurance). Comorbidities were included using a modified Charlson Comorbidity Index, which includes conditions commonly found in ambulatory care settings.19 Language preference was determined using questions of primary language spoken at home, if all members of the family were comfortable speaking English, and if the respondent was comfortable speaking English. Respondents were categorized as English speaking if English was spoken at home, or all family members were comfortable speaking English, or if the respondent was comfortable speaking English.
Statistical Analyses
All results show weighted estimates and indicate where differences were statistically significant at the 5 percent level. We used two regression models to estimate the likelihood of having a medical home versus a regular source of care that is not a medical home, and having a medical home versus not having a regular source of care. Each model included Latino subgroup, age, sex, income level, insurance status, comorbidities, and language. We used SAS version 9.2 (SAS Institute, Inc, Cary, NC) for all analyses to estimate standard errors that adjust for the complex multistage survey design.
RESULTS
Respondent Demographics
Whites differed from Latinos in many of the demographic measures (Table 1). Whites were older, more likely to have higher incomes, less likely to be uninsured, and more likely to be privately insured. There were also Latino subgroup differences in some measures. Puerto Ricans were least likely among Latinos to be uninsured (16% vs 37% of Mexicans/Mexican Americans and Central/South Americans) and were most likely to be publicly insured (28% vs 19% of Mexicans/Mexican Americans and 15% of Central/South Americans). The number of comorbidities reported by Puerto Ricans was similar to whites, and they were less likely than other Latino groups to report having no chronic conditions. Regarding language preference, 7.5% of Puerto Ricans were not comfortable speaking English, as compared to 29% of Mexicans/Mexican Americans and 31% of Central/South Americans.
Reports of Medical Home Indicators
There were significant ethnic variations in reports of having a medical home in the weighted, unadjusted analyses (Table 2). White and Puerto Rican adults were most likely to report receiving care from practices that had indicators of being a medical home (57.1% and 59.3%, respectively). In contrast, only 35.4% of Mexican and Mexican Americans and 34.2% of Central and South Americans report having a medical home. These disparities were largely due to differences in having a regular provider with 41.3% of Mexican/Mexican Americans and 48.6% of Central/South Americans reporting not having a regular source of care.
Preventive Care
Among those with a regular source of care, rates of receiving preventive care were higher for adults with a medical home compared to those with a regular source of care that is not a medical home, with two exceptions: rates of blood pressure screening among Central/South Americans and mammography screening among Mexican/ Mexican Americans. Adults in all ethnic groups without a regular source of care had the lowest rates of receiving preventive care. White and Puerto Rican adults had the highest rates of receiving preventive care, while Mexican/Mexican Americans tended to have the lowest rates. However, when stratified by medical home, disparities were reduced or eliminated. For example, in the unstratified, unadjusted estimates of having a cholesterol check, there were significant differences: 70.4% of Whites and 74.3% of Puerto Ricans report being tested, compared to 56.0% of Mexican/Mexican Americans and 64.9% of Central/South Americans. For those who had a medical home, the rates of cholesterol screening were higher than those with only a regular source of care, and racial/ethnic differences were no longer statistically significant: 79.4% of Whites, 75.7% of Mexican/Mexican Americans, 83.3% of Puerto Ricans, and 82.0% of Central and South Americans (Table 3). We found a similar pattern for the other preventive measures of blood pressure check, mammography and PSA screening; the rates of preventive care were higher for those with a medical home, and disparities were reduced or eliminated.
Patient Experience
The overall rates of positive patient experiences were generally high, although adults with a medical home had the highest rates. When asked whether their doctor usually or always explains things, listens, spends enough times, and shows respect, most groups had high rates of positive response with at least 80%–93% reporting a positive experience. When stratified by having a medical home, the rates were consistently, but only slightly higher and ranged from 85%–96%. On measures of the doctor explains things, listens carefully, and spends enough time, both Mexican/Mexican Americans and Central/South Americans reported the lowest rates in the unstratified estimates. When stratified into the medical home, the disparities were no longer statistically significant except for doctor explains things for 95.2% of Whites, 93.2% of Mexican/Mexican Americans, 90.1% of Puerto Ricans, and 87.5% of Central and South Americans who gave a positive response (Table 4).
Correlates of Access to a Medical Home
Given the observation that having a medical home was a significant correlate of preventive care and patient experiences, and the significant ethnic differences in rates of having a medical home, we sought to determine what factors were associated with having a medical home. We ran two models. The first was among adults with a regular source of care and modeled what factors were associated with having a medical home versus having a regular source of care that is not a medical home. The second modeled what factors were associated with having a medical home versus not having a regular source of care. Both models included ethnicity, age, sex, income level, insurance status, comorbidities, and comfort with speaking English.
In the first model, insurance coverage and comorbidities were significantly associated with having a medical home (Table 5). Compared with people who had private insurance, adults with public insurance were 80% as likely to have a medical home, while the uninsured were 62% as likely to have a medical home. Adults with chronic conditions were 27% more likely to have a medical home with each comorbid condition. No other factors, including ethnicity, were significantly associated with having a medical home versus a regular source of care that is not a medical home.
The second model produced very different results. Ethnicity was a significant independent factor with Mexican/Mexican Americans and Central and South Americans being half as likely as Whites to have a medical home versus no usual source of care. Language was also a significant independent factor, with respondents who were comfortable speaking English being twice as likely to have a medical home. As would be expected, higher income respondents and those with chronic conditions were also more likely to have a medical home. Regarding insurance coverage, the uninsured were 27% less likely than the privately insured to have a medical home. Unlike the first model, public insurance was not a significant factor for having a medical home versus no source of care. The primary difference was between those with any type of coverage versus the uninsured.
DISCUSSION
Our results show significant Latino subgroup differences in having a medical home and that much of the difference is driven by the basic requirement for “medical homeness,” that is, having a regular provider. The differential access to a medical home among Latino subgroup populations was associated with disparities in health care. In this case, we showed that there were significant disparities in common preventive care procedures—cholesterol screening, blood pressure check, mammography and PSA screening—but those disparities were reduced or eliminated for those who had a medical home. Although disparities in patient experiences were less pronounced, they did occur and were reduced or eliminated among those with a medical home. Of note, these findings were all based on unadjusted analyses. While there are several factors, such as insurance coverage, income status, and primary language, that contribute to health-care disparities experienced by Latinos, having a medical home can improve care and eliminate disparities regardless of coverage, income, or other factors known to impact care.
Subgroup Variations
Among the Latino subgroups, Mexicans/Mexican Americans tended to have the lowest rates of having a medical home, lowest rates of receiving preventive care, and smallest gains from having a medical home. Puerto Ricans had rates similar to whites in having a medical home and receiving preventive care services. Some of these differences could be due to differences in citizenship status between the two groups. However, that difference would also affect Central/South Americans, whose health-care measures were also consistently poorer than others, although they tend to do better than Mexicans and Mexican Americans. Clearly other factors that were not included in our analyses contribute to differential outcomes. These variations among Latino subgroups in health-care outcomes demonstrate the need for more in-depth assessment of Latino health to inform the development of effective interventions or policies to address disparities.
Regular Source of Care
The prevalence of access to a medical home was the primary question for this study. However, the model of medical home versus no regular source of care was an assessment of basic access to a regular provider. Other researchers have shown that patients without a basic regular source of care experience significant barriers to receiving appropriate services.20–23 The regression analyses showed significant ethnic variations in having no regular source of care with Mexicans/Mexican Americans, and Central/South Americans being twice as likely to have no regular source of care. While the medical home model is a better source for primary care, many populations are challenged to access any type of care. No one can obtain care in the medical home if they cannot even get a regular provider. The goal of access to the medical home will remain elusive without basic access to care.
Insurance Matters
In both regression models the uninsured were significantly less likely to have a medical home. However, among the insured, the type of insurance one has led to different results in our models. The first model was among people who already had a regular source of care and showed that respondents with public insurance were less likely than those with private insurance to have a medical home. The second model looked at having absolutely no regular source of care versus having a medical home and found that respondents with public insurance were just as likely as those with private insurance to have a medical home. These different results indicate that when people have insurance—whether private or public—they are able to identify some sort of regular source of care. However, among those who do have a regular source of care, there is a difference in having a medical home based on type of coverage, and it is the privately insured who are more likely to have a medical home.
Study Limitations
The MEPS is a large national database that allowed us to conduct analyses of major Latino subgroups. However, we could not include Cuban, Dominican, and other Latino subgroups because of small sample sizes and loss of predictive power as we stratified into the three medical home categories. Thus, we limited our analyses to the major Latino subgroups represented in the MEPS. One of the questions we could not address was whether country of birth, length of time in the US, or citizenship status of the respondents would affect our outcomes. Unfortunately, in MEPS linking to questions of birth country or length of time in the US would cause us to lose significant sample size, further limiting our subgroup analyses. The MEPS does not ask about citizenship status, as this is an understandably sensitive topic for those responding to a government survey. Further work needs to elucidate how citizenship status affects health-care access and outcomes to determine what factors mediate its effect.
We had to liberalize age cutoffs for some of the preventive care measures because of challenges with sample size. For example, we analyzed PSA screening rates for men age 40 and above rather than 50 and above as is commonly recommended. While we could easily detect disparities in screening rates by race/ethnicity, we could not use the same age cutoffs for the subsequent analyses when we further stratified by who had a medical home or not. Our numbers within each cell for some of the Latino subgroups became too small for meaningful analysis. The age cutoffs may have caused us to overestimate disparities because the Latino respondents were younger than the white respondents. However, our hypothesis is that those with a medical home will experience no disparities. Thus, although we may have introduced an overestimation of the degree of disparities because of our age cutoffs, we were still able to demonstrate that disparities were eliminated or reduced for respondents with a medical home.
Conclusions
While care for those with a medical home was better, and disparities were reduced, they were not always eliminated—particularly for Mexican/Mexican Americans. The medical home model is extremely promising for improving care and reducing disparities; however, it will not solve all health-care problems. When addressing the needs of diverse or vulnerable patient populations, the generic medical home model will be important, but may not be enough for all populations. Instead, it may serve as a foundation for developing truly patient-centered care that can address the various needs of diverse populations. As the medical home model gains greater recognition for improving care and reducing health-care disparities, we recommend ongoing assessment by race/ethnicity to ensure it fulfills that promise for all patients.
References
Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–84.
Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–41.
Hasnain-Wynia R, Baker DW, Nerenz D, et al. Disparities in health care are driven by where minority patients seek care. Arch Intern Med. 2007;167(12):1233–88.
Reschovsky JD, O, Malley AS. Do primary care physicians treating minority patients report problems delivering high-quality care? Health Affairs. 2008;27(3):w222–31.
Gaskin DJ, Spencer C, Richard P. Do hospitals provide lower-quality care to minorities than to whites? Health Affairs. 2008;27(2):518–27.
Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K. Closing the Divide: How Medical Homes Promote Equity in Health Care. The Commonwealth Fund. June 2007. Available at: http://www.commonwealthfund.org/usr_doc/1035_Beal_closing_divide_medical_homes.pdf?section=4039 Accessed Jul 14, 2009.
Barr MS. The Need to Test the Patient-Centered Medical Home. JAMA. 2008;300(7):834–5.
American College of Physicians. Joint principles of the patient-centered medical home. March 2007. Available at: http://www.acponline.org/advocacy/where_we_stand/medical_home/approve_jp.pdf. Accessed Jul 14, 2009.
Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–57.
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457–502.
Starfield B, Shi L. The medical home, access to care, and insurance: a review of the evidence. Pediatrics. 2004;113:1493–8.
Keckley PH, Underwood HR. The Medical Home: Disruptive innovation for New Primary Care Model. Deloitte Center. February 2008. Available at: http://www.deloitte.com/dtt/cda/doc/content/us_chs_MedicalHome_w.pdf. Accessed Jul 14, 2009.
Weiss LJ, Blustein J. Faithful patients: the effect of long-term physician-patient relationships on the costs and use of health care by older Americans. Am J Public Health. 1996;86:1742–7.
Rosenthal TC. The medical home: growing evidence to support a new approach to primary care. J Am Board Fam Med. 2008;21(5):427–40.
Ezzati-Rice TM, Rhode F, Greenblatt J. Sample Design of the Medical Expenditure Panel Survey Household Component, 1998–2007. Methodology Report No. 22. March 2008. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.meps.ahrq.gov/mepsweb/data_files/publications/mr22/mr22.pdf. Accessed Jul 14, 2009.
Cooley WC, McAllister JW, Sherrieb K, Clark RE. The Medical Home Index: development and validation of a practice-level measurement of implementation of the medical home model. Ambul Pediatr. 2003;3:173–80.
Standards and Guidelines for Physician Practice Connections®— Patient-Centered Medical Home (PPC-PCMH™) CMS Version. Available at: http://www.cms.hhs.gov/DemoProjectsEvalRpts/downloads/MedHome_PPC.pdf. Accessed Jul 14, 2009.
Schoen C, Osborn R, Doty MM, Bishop M, Peugh J, Murukutla N. Toward higher-performance health systems: adults’ health care experiences in seven countries. Health Affairs. 2007;6(6):w717–34.
Balu S, Thomas J. Incremental Expenditure of Treating Hypertension in the United States. Am J Hypertension. 2006;19(8):810–6.
Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002;37:1509–29.
LeMaster J, Kruse R, Lin WC, Lindbloom E, Fryer G. Health Care Expenses for People with Diabetes Mellitus in the United States: Does Having a Usual Care Provider Make a Difference? J Health Care Finance. 2006;32(4):76–87.
Breen N, Wagener DK, Brown ML, Davis WW, Ballard-Barbash R. Progress in cancer screening over a decade: results of cancer screening from the 1987, 1992, and 1998 National Health Interview Surveys. J Natl Cancer Inst. 2001;93:1704–13.
Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97:1528–40.
Acknowledgments
We would like to thank Anne Dubois and Melinda Abrams for their thoughtful comments on earlier drafts of this paper. We would also like to thank the staff at Child Trends for their analytical support for this project, particularly Mr. Kassim Mbwana.
Conflicts of interest
All the authors of this paper were employees of the Commonwealth Fund at the time it was written; the Commonwealth Fund is the sole funder of this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beal, A., Hernandez, S. & Doty, M. Latino Access to the Patient-Centered Medical Home. J GEN INTERN MED 24 (Suppl 3), 514–520 (2009). https://doi.org/10.1007/s11606-009-1119-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1119-1