Abstract
Background
Low health literacy and low cognitive abilities both predict mortality, but no study has jointly examined these relationships.
Methods
We conducted a prospective cohort study of 3,260 community-dwelling adults age 65 and older. Participants were interviewed in 1997 and administered the Short Test of Functional Health Literacy in Adults and the Mini Mental Status Examination. Mortality was determined using the National Death Index through 2003.
Measurements and Main Results
In multivariate models with only literacy (not cognition), the adjusted hazard ratio was 1.50 (95% confidence of interval [CI] 1.24–1.81) for inadequate versus adequate literacy. In multivariate models without literacy, delayed recall of 3 items and the ability to serial subtract numbers were associated with higher mortality (e.g., adjusted hazard ratios [AHR] 1.74 [95% CI 1.30–2.34] for recall of zero versus 3 items, and 1.32 [95% CI 1.09–1.60] for 0–2 vs 5 correct subtractions). In multivariate analysis with both literacy and cognition, the AHRs for the cognition items were similar, but the AHR for inadequate literacy decreased to 1.27 (95% CI 1.03 – 1.57).
Conclusions
Both health literacy and cognitive abilities independently predict mortality. Interventions to improve patient knowledge and self-management skills should consider both the reading level and cognitive demands of the materials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In a prospective cohort study of 3,260 new Medicare-managed care enrollees, we found that after adjusting for demographics, socioeconomic status, and baseline health, the hazard ratio for all-cause mortality was 1.52 for participants with inadequate versus inadequate health literacy.1 However, some investigators have questioned whether tests of reading fluency such as the Test of Functional Health Literacy in Adults (TOFHLA)2, 3 may actually be measuring cognitive function and whether cognitive abilities may be the actual causal factor that affects health behaviors and outcomes for individuals with limited reading ability.4–6 Reading skills are strongly associated with several cognitive domains,4 and poorer cognitive ability has also been linked to medical understanding,7 self-management skills,8–9 and higher mortality.10–12 We analyzed whether measures of cognitive function independently predict mortality after adjusting for health literacy and whether the association between literacy and mortality changes after adjusting for cognitive abilities.
METHODS
The study design, health literacy levels, and characteristics of the study population have been described previously.1,13 New Medicare-managed care enrollees age 65 and older in 4 US cities were contacted in 1997. Participants completed an interview in their home in 1997. The survey assessed race/ethnicity, education, income, health behaviors, chronic medical conditions, self-rated physical and mental health (measured by the SF-12),14 and impairments in instrumental activities of daily living (IADLs) and ADLs. Health literacy was evaluated with a shortened version of the TOFHLA2,3 that included 2 reading passages and 4 numeracy items.
Cognitive abilities were measured by the Mini Mental Status Examination (MMSE).15 Performance on some MMSE items may depend on educational experience and literacy.16 We chose to use MMSE measures that we thought a priori should be minimally influenced by educational experience or reading fluency: (1) delayed recall of 3 spoken items (“apple”, “penny”, and “table”); (2) the ability to follow 3-step oral instructions (“Take the paper in your right hand. Fold the paper in half. Put the paper on the floor”); and (3) the ability to copy overlapping pentagons (score 0 or 1). We also included the ability to perform 5 serial subtractions in increments of 7 starting from 100; each subtraction step was scored independently regardless of any prior errors. This measure may depend somewhat on education, but it is widely viewed as a measure of working memory, which is defined as the structures and processes used for temporarily storing and manipulating information.17 We tracked deaths through 2003 using the National Death Index.
All analyses were conducted using Stata version 9 (College Station, TX). Of 3,260 participants, 69 had missing data on cognitive functioning. The relationship between health literacy and time to death was examined using Kaplan–Meier curves and age-adjusted Cox proportional hazards models. This was repeated using cognitive abilities as the only independent variables. We then analyzed 3 multivariate models to examine the independent associations of literacy and cognitive abilities with mortality: Model 1 included literacy but not cognitive measures, Model 2 included cognitive measures but not literacy, and Model 3 included both. All models adjusted for age, sex, race, language, income, education, physical functioning, mental health, number of chronic diseases, ADL and IADL impairments, and study site.
RESULTS
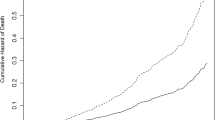
Individuals with inadequate and marginal health literacy were more likely to die during follow up than those with adequate health literacy (38.4%, 28.4%, vs 18.9%, respectively; p < .001). Performance on the delayed recall, serially counting backward, and copying overlapping pentagons were significantly associated with mortality; however, performance on the 3-step command was not (Table 1). Performance on the sequential subtraction showed a threshold effect with a higher mortality among those who completed ≤2 subtractions correctly (Table 1). Relative to participants who recalled all 3 items, the age-adjusted hazard ratios for death were 1.30 (95% CI 1.11–1.53), 1.46 (1.17–1.82), and 2.20 (95% CI 1.67–2.91) for those who correctly recalled 2, 1, or no items, respectively (Fig. 1).
After adjusting for baseline covariates (but not cognitive measures), the adjusted hazard ratio for time to death was 1.50 (95% CI 1.24–1.81) for participants with inadequate literacy compared to those with adequate literacy (Table 2, Model 1). Delayed recall and the ability to serially subtract were also independently associated with death when literacy was not included (Table 2, Model 2). Compared to participants who recalled all 3 items correctly, the adjusted hazard ratios for death for those who recalled only 2, 1, or 0 items correctly were 1.20 (95% CI 1.02–1.42), 1.29 (95% CI 1.03–1.62), and 1.74 (1.30–2.34), respectively. Those who completed 2 or less subtractions had an adjusted hazard ratio of death of 1.32 (95% CI 1.09–1.60) compared to those who completed 5 subtractions correctly.
In multivariate analysis with both health literacy and cognitive variables (Table 2, Model 3), literacy, delayed recall, and the ability to subtract were all significant. The hazard ratios for the cognition items in Model 3 were very similar to the model without literacy (Model 2). However, the adjusted hazard ratio for inadequate literacy in Model 3 was only 1.27 (95% CI 1.03–1.57) compared to 1.50 when cognitive abilities were not included (Model 1).
DISCUSSION
We found that both health literacy and cognitive abilities independently predicted mortality among elderly, community-dwelling individuals. Both reading comprehension and cognitive abilities are likely to be important for gaining health information and interacting with the health care system. For example, patients are often required to read prescriptions and other materials to successfully follow recommended treatments. However, many recommendations and instructions are spoken but never written, and patients must rely on their memory. Even when written, instructions often place high demands on working memory for comprehension and retention.18 Individuals who are unable to meet these reading and cognitive demands are likely to have worse outcomes.
When we included only Short Test of Functional Health Literacy in Adults (S-TOFHLA) performance in our multivariate models (i.e., without cognitive measures), the association was stronger than when cognitive abilities were included. This suggests that some of the association between health literacy and mortality is accounted for by individuals with lower health literacy having lower cognitive abilities. To understand this, we must examine what is required to complete the S-TOFHLA. For the reading comprehension passages, respondents must read prose in which words have been replaced by blanks and select the words that best complete the blanks. This requires decoding individual words, discerning the meaning of sentences when a word is missing, mentally placing the possible word choices into the blanks, and assessing whether the sentence makes sense. The 4 numeracy items in the S-TOFHLA similarly place demands on several cognitive abilities.
Thus, although the S-TOFHLA is thought of as a measure of “health literacy,” performance probably depends on a complex array of cognitive abilities, including word recognition, phoneme recognition and decoding of unfamiliar words, working memory, and judgment. When viewed from this perspective, it is not surprising that performance on the S-TOFHLA is correlated with measures of cognitive abilities.19 In our initial multivariate model with only health literacy and no measures of cognitive abilities (Table 1, model 1), the S-TOFHLA score likely acted as both a direct measure of reading comprehension and an indirect measure of cognitive abilities, and the adjusted hazard ratio for inadequate literacy was 1.50. When we included direct measures of cognitive abilities in the multivariate models (Table 1, model 3), the adjusted hazard ratio for inadequate literacy decreased to 1.27 because the S-TOFHLA was no longer serving as a surrogate measure for cognitive abilities.
There are important limitations to this study. The S-TOFHLA is not a comprehensive measure of health literacy. In a similar way, we had only a limited set of measures of cognitive abilities. The strength of the associations between health literacy, cognitive abilities, and mortality depend on the precision with which these domains are measured. Additional studies with more accurate and extensive measures are needed.
The finding that both reading comprehension and cognitive abilities predict mortality has important implications for provider–patient communication and designing health education programs. Efforts to overcome the learning barriers posed by limited health literacy over the last decade have focused on simplifying written materials. However, if cognitive abilities such as memory are also important, these strategies will not be enough. More recently, researchers have advised the use of “teach-back” techniques in which health care providers have patients repeat back in their own words explanations of diseases and treatment plans to confirm understanding. This procedure will identify individuals who either failed to understand the material initially and those who forgot information that was originally understood. “Teach-back” and “teach to goal” strategies, in which comprehension is formally assessed and information is repeated if necessary until understanding is achieved, are complementary strategies to plain language communication that should help minimize the impact of differences in cognitive abilities on patients’ learning. There is also an emerging literature on ways to decrease the “cognitive load” of multimedia educational tools and improve comprehension.20 Studies are greatly needed to understand how to design health communication tools so all patients can understand the essential information necessary for proper self-management and be motivated and empowered to use this information to improve their health.
References
Baker DW, Wolf MS, Feinglass JM, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–9.
Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41.
Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42.
Barnes DE, Tager IB, Satariano WA, Yaffe K. The relationship between literacy and cognition in well-educated elders. J Gerontol. 2004;59A:390–5.
Manly JJ, Schupf N, Tang MX, Stern Y. Cognitive decline and literacy among ethnically diverse elders. J Geriatr Psychiatry Neurol. 2005;18:213–7.
Deary IJ, Batty D, Gottfredson LS. Human hierarchies, health, and IQ. Science. 2005;309:703.
Beier ME, Ackerman PL. Determinants of health knowledge: an investigation of age, gender, abilities, personality, and interests. J Pers Soc Psychol. 2003;84:439–48.
Insel K, Morrow D, Brewer B, Figueredo A. Executive function, working memory, and medication adherence among older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61:102–107.
Stilley CS, Sereika S, Muldoon MF, Ryan CM, Dunbar-Jacob J. Psychological and cognitive function: predictors of adherence with cholesterol lowering treatment. Ann Behav Med. 2004;27:117–24.
Pavlik VN, de Moraes SA, Szklo M, Knopman DS, Mosley TH, Hyman DJ. Relation between cognitive function and mortality in middle-aged adults. Am J Epidemiol. 2003;157:327–34.
Hart CL, Taylor MD, Smith GD, et al.. Childhood IQ, social class, deprivation, and their relationships with mortality and morbidity risk in later life: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Psychosom Med. 2003;65:877–83.
Shipley BA, Der G, Taylor MD, Deary IJ. Cognition and all-cause mortality across the entire adult age range: Health and Lifestyle survey. Pcychosom Med. 2006;68:17–24.
Gazmararian JA, Baker DW, Williams MV, et al.. Health literacy among Medicare enrollees in a managed care organization. JAMA. 1999;281:545–51.
Ware JE. The MOS 36-item Short Form Health Survey (SF-36). In: Sederer LI, Dickey B, eds. Outcomes Assessment in Clinical Practice. Baltimore, MD: Williams and Wilkins; 1996:61–4.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state": a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98.
Jorm AF, Scott R, Henderson AS, Kay DW. Educational level differences on the Mini-Mental State: the role of test bias. Psychol Med. 1988;18:727–31.
Baddeley A. The fractionation of working memory. Proc Natl Acad Sci U S A. 1996;93:13468–72.
Chandler P, Sweller J. Cognitive load theory and the format of instruction. Cogn Instr. 1991;8:293–332.
Baker DW, Gazmararian JA, Sudano J, Patterson M, Parker RM, Williams MV. Health literacy and performance on the Mini-Mental State Examination. Aging Ment Health. 2002;6:22–9.
Mayer RE, ed.. The Cambridge Handbook of Multimedia Learning. New York: Cambridge University Press; 2006.
Acknowledgments
This work was supported by grant number R01 AB026393-01 from the National Institute on Aging. Dr. Wolf received support from a Centers for Disease Control and Prevention Career Development Award (K01 EH000067-01).
Contributions of Authors
We declare that we participated in the following:
Obtaining funding—Baker, Feinglass, Wolf; obtaining data and determining deaths from the National Death Index—Feinglass, Baker; analysis of the data and interpretation of the results—Baker, Wolf, Feinglass, Thompson; drafting of the manuscripts—Baker, Wolf, Feinglass; critical feedback and suggested revisions—Thompson.
Conflict of Interest
None disclosed.
Role of the Funding Source
The funding source (the National Institute on Aging) for this project played no role in the project.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baker, D.W., Wolf, M.S., Feinglass, J. et al. Health Literacy, Cognitive Abilities, and Mortality Among Elderly Persons. J GEN INTERN MED 23, 723–726 (2008). https://doi.org/10.1007/s11606-008-0566-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0566-4