Abstract
Background
Patient education materials can assist patient decision making on prostate cancer screening.
Objective
To explore the effectiveness of presenting health information on prostate cancer screening using video, internet, and written interventions on patient decision making, attitudes, knowledge, and screening interest.
Design
Randomized controlled trial.
Participants
A total of 161 men aged over 45, who had never been screened for prostate cancer, were randomized to receive information on prostate cancer screening.
Measurements
Participants were assessed at baseline and 1-week postintervention for decisional conflict, screening interest, knowledge, anxiety, and decision-making preference.
Results
A total of 156 men were followed-up at 1-week postintervention. There was no statistical, or clinical, difference in mean change in decisional conflict scores between the 3 intervention groups (video vs internet −0.06 [95% CI −0.24 to 0.12]; video vs pamphlet 0.04 [95%CI −0.15 to 0.22]; internet vs pamphlet 0.10 [95%CI −0.09 to 0.28]). There was also no statistically significant difference in mean knowledge, anxiety, decision-making preference, and screening interest between the 3 intervention groups.
Conclusion
Results from this study indicate that there are no clinically significant differences in decisional conflict when men are presented health information on prostate cancer screening via video, written materials, or the internet. Given the equivalence of the 3 methods, other factors need to be considered in deciding which method to use. Health professionals should provide patient health education materials via a method that is most convenient to the patient and their preferred learning style.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Prostate cancer is one of the most prevalent cancers in men worldwide.1 The introduction and widespread use of the prostate-specific antigen (PSA) test as a diagnostic screening instrument has led to a significant increase in the detection of prostate cancer.1,2 Despite the high incidence of prostate cancer, many medical organizations offer conflicting recommendations as to the merits of screening for prostate cancer.3 Much of this debate is caused by the inadequacies of diagnostic screening tests, including the PSA test, and lack of high-quality evidence from randomized controlled trials (RCTs) of a salutary effect of prostate cancer screening on patient outcomes.3 This uncertainty will persist until long-term follow-up data from ongoing RCTs indicates whether screening offers clinically significant improvements in patient outcomes by reducing prostate-specific and all-cause mortality.3
In the absence of any definitive evidence on the merits of prostate cancer screening, greater emphasis is placed on the patient/doctor relationship, their interaction, and the ability of the patient to understand the potential benefits and risks of screening. Traditionally, the patient/doctor relationship has been paternalistic in nature, with the doctor acting as the gatekeeper of health information and guiding the decision-making process.4 Education materials have traditionally been used by health professionals to better inform patients and supplement discussions on specific health issues. Such materials, along with decision aids, can increase the effectiveness of decision making by reducing patients’ decisional conflict.5 Decisional conflict is defined as a state of uncertainty about a particular course of action.6 Patients will often experience decisional conflict when confronted with making a decision about a medical issue that has high trade-offs between benefits and harms, as is the case with screening for prostate cancer.
Patient education has traditionally been facilitated through written and audio-visual formats. More recently, increased public access to the internet has seen it develop as another potential patient education resource. The internet is a resource that allows patients to access health information anonymously, which can be beneficial when searching for information on patient-perceived sensitive issues such as prostate cancer.7 In addition, the internet allows users to access health information easier and in a format that is most suited to their learning style, accounting for different levels of education, language, and media.7,8 Despite such benefits, users must also overcome potential barriers including accessibility to the internet and expertise in searching for online health information.
The majority of patient education materials on prostate cancer to date have been facilitated through video and written formats. Both formats have been associated with an increase in patient health knowledge, a shift toward an active or shared decision-making process, a decrease in patient decisional conflict, and a preference to not undergo screening for prostate cancer.9–20 To date, only one study has investigated the effectiveness of the internet as a patient education tool for prostate cancer screening. It compared information delivered via the internet and video and identified increases in patient knowledge and a decrease in patient preference for prostate cancer screening across both interventions.11 There was no significant difference in knowledge scores between the interventions, however, statistically significantly fewer participants who were assigned to the video intervention requested a PSA test than those assigned to the internet intervention. Other RCTs, which have evaluated the effectiveness of the internet as a patient education source across a variety of health topics, have also concluded the potential for the internet as a viable method of delivering health information to patients.21–23
The aim of this study was to determine which format for delivering information about prostate cancer screening (video, internet, or written materials) has the greatest effects on patient decision making, attitudes, knowledge, and screening interest.
METHODS
At a single medical center, we performed a 3-arm, randomized controlled trial with blinded outcome assessment; delivering information about prostate cancer screening via paper pamphlet, video, or the internet was performed. Institutional Review Board approval for this study was received from the Monash University Standing Committee on Ethics in Research Involving Humans.
Participants and Recruitment
Men aged over 45 years of age who had not previously been tested for prostate cancer were recruited through radio and newspaper advertisement over 12 months across 5 states in Australia. Men in this age bracket were eligible for selection as it was it was believed that they best represented the population most likely to be seeking information about screening. Respondents were screened by telephone by the lead investigator (DI) to ensure they met the selection criteria and were provided with verbal and written information about the project and their required contribution. Along with this information participants were also sent a consent form, which they were required to complete and send back to the lead investigator before being involved in the study. Men who were unable to understand English, who did not provide informed consent, or who were not contactable by telephone were not eligible for inclusion.
Protocol, Assignment, and Blinding
Participants were randomized to receive information on prostate cancer screening delivered through 1 of the 3 formats: video, internet, pamphlet. The allocation sequence was generated using a random number generator by the trial statistician (JM). A file containing this sequence was then loaded into a database that was accessed through an internet application. To randomize a participant, the lead investigator would enter the participant’s ID, initials, age, and last 3 digits of their land and/or mobile number. The application would then return the group to which the participant had been allocated. Demographic details and responses to selected measures were participant reported. Details were collected by telephone at baseline and at 1-week post intervention by a single outcome assessor (KE) who was blinded to group allocation. At 1-week postintervention participants were also asked whether they had viewed the sent material in its entirety to quantify compliance. Any participants who had only partially viewed the material were classified as not completely viewing the material. All telephone interviews were audio recorded and monitored for quality assurance purposes.
Intervention
The content information presented in each intervention was standard, with only the format varying. Content included Australian epidemiology on prostate cancer, the diagnostic process, treatment options, and the benefits/risks associated with the “prostate journey.”
The media format for the 3 groups were;
-
Video: Participants randomized to this group were sent a video that was 20 min in duration.
-
Internet: Participants randomized to this group were sent a letter directing them to a specific website. The letter also contained contact details of libraries, near their place of residence, where there was public internet access in the event that they did not have internet access in their home or workplace.
-
Pamphlet: Participants randomized to this group were sent a 28-page paper pamphlet that was identical to the internet format in terms of content and design.
Outcome Measures
Primary Outcome Measure—Decisional Conflict
Decisional conflict was chosen as the primary outcome as in the absence of evidence, as is the case for prostate cancer screening, the purpose of patient education is to increase the patient’s confidence in making decisions that are inline with their personal values. Decisional conflict was measured using the Decisional Conflict Scale, which consists of 16 items divided into 3 subscales measuring: decision uncertainty, factors contributing to uncertainty, and perceived effective decision making.5,24 Decisional conflict is reported on a continuous scale ranging from 0 to 5, with larger values reflecting greater decisional conflict.
Secondary Outcome Measures
Secondary outcomes measured included:
-
Knowledge: Participants answered a 5-item multiple-choice question assessing their knowledge about prostate cancer and PSA testing. For each participant, the percentage of items correctly answered was calculated.10
-
Anxiety: Participants’ anxiety relating to their decision about whether or not to be screened for prostate cancer was assessed using the Spielberger State Trait Anxiety Inventory (STAI) short form instrument.25 Responses to 5 items are recorded on a 4-point scale, resulting in a scale ranging from 20 to 80, with higher scores reflecting greater anxiety.
-
Consumer Decision-Making Role: Participants’ preferred role in decision making (active, passive, or collaborative role) was assessed using the Control Preferences Scale).18,26
-
Screening Interest: Participants reported propensity toward prostate cancer screening at the time of interview on a 5-point response scale (1—‘Be unlikely to want a screening test for prostate cancer’ to 5—‘Definitely want a screening test for prostate cancer’).13
Statistical Power and Analysis
The primary outcome for this study was decisional conflict measured at 1-week postrandomization. A previous RCT of men with benign prostatic hypertrophy compared a multimedia design aid with normal care received from practitioners.27 At 3 and 9 months, patients in the intervention group were found to have on average 0.3 lower decisional conflict compared to the control group. Clinically important differences between those who make and delay decisions can be discriminated by effect sizes ranging from 0.4 to 0.8 on the decisional conflict scale.6 This study was powered to detect a minimum difference in decisional conflict of 0.3 between any 2 groups with 85% power, and α = 0.05.
Multiple linear regression and proportional odds ordinal regression were used to estimate the intervention effect for continuous and ordinal data, respectively. For the linear regression models, adjustment was made for the baseline measure of the outcome by including this as a covariate in the model.28 For the proportional odds model, the assumption of proportionality was investigated visually.29 The likelihood ratio χ 2 test was used to test if the percentage of those reporting complete revision of materials or seeking additional information differed between groups. Because of baseline imbalance in internet use between groups, an additional secondary analysis was carried out for the primary outcome, decisional conflict, which adjusted for both baseline decisional conflict and internet use. Participants were analyzed as randomized. No imputation was performed for the 5 participants who withdrew from the study. No adjustment was made for multiple testing. All analyses were carried out in Stata/SE version 9.0 (StataCorp. 2005. Stata Statistical Software: Release 9. College Station, TX, StataCorp LP.)
RESULTS
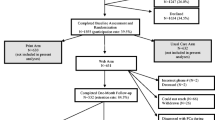
A total of 236 men volunteered to participate in the study, 161 (68%) of which were eligible and enrolled in the study (Fig. 1). Five participants did not want to conduct a follow-up interview, leaving a total of 156 men (97% of those enrolled) who were followed-up at 1-week postintervention. The demographic details of all participants by intervention group are presented in (Table 1). The age, marital status, education, and employment status of participants were similar across the 3 groups. Slightly fewer men randomized to the video group reported a family history of prostate cancer. A higher proportion of men assigned in the video group accessed the internet daily, but fewer accessed it 2–3 times a week compared to the internet and pamphlet groups.
There was no evidence that the level of participation was statistically significantly different between the 3 groups (p = 0.258), with 49 (92%) participants in the video group, 52 (96%) participants in the internet group, and 43 (88%) participants in the pamphlet group reporting complete revision of the materials. In addition, there was no evidence that the percentage of participants seeking additional information during the period of the trial was statistically significantly different between groups (p = .422), with a total of 6 (11%) participants in the video group, 11 (20%) in the internet group, and 7 (14%) in the pamphlet group seeking additional information.
Primary Outcome
Decisional Conflict
Decisional conflict was similar across intervention groups at baseline (Table 2). At 1-week follow-up, there were no statistically or clinically significant differences in mean decisional conflict between the 3 intervention groups (Tables 3 and 4). Given there was some baseline imbalance in internet use, an additional analysis was carried out adjusting for both baseline decisional conflict and internet use. Compared to the primary analysis, additional adjustment for baseline internet use resulted in essentially the same estimates of intervention effect (Table 4).
Secondary Outcomes
There were no inter-group differences in knowledge and anxiety before the intervention. Postintervention, knowledge increased equally in all groups, and there was no difference in anxiety scores across the 3 groups (Tables 3 and 4). The majority of participants at baseline indicated a preference for taking an active role in decision making. This preference remained at follow-up, however; there were no statistically significant differences in decision-making preference between the 3 intervention groups at follow-up (Tables 3 and 4). The majority of participants indicated a greater propensity of wanting to be screened for prostate cancer, rather than not, at baseline. This was consistent postintervention; however, the propensity for screening at 1-week follow-up did not vary statistically between groups (Tables 3 and 4).
DISCUSSION
Findings from this study suggest video, internet, and pamphlet formats are equally effective media for presenting information on prostate cancer screening, as they had similar impact on patient decisional conflict, knowledge of prostate cancer, anxiety about prostate cancer, participating in decision-making about prostate cancer screening, and actual screening preferences. Several other factors need to be considered when deciding which format to use when educating men about prostate cancer screening. Patient knowledge, interest in being screened, and anxiety associated with considering the benefits and limitations with prostate cancer screening may all influence the manner in which patients interact with their doctor and what role is adopted during the decision-making process. The outcomes of this study also add to findings from previous studies that have identified the beneficial impact of prostate cancer education materials on patient decisional conflict, knowledge, anxiety, and role in the decision-making process.9–20 However, this study is the first to directly compare patient information on prostate cancer screening delivered through video, internet, and written formats to men previously not screened for prostate cancer, and suggest that media format may not significantly alter these clinical outcomes.
In the era of evidence-based medicine, it is widely recognized that patient education materials are necessary. More so, such materials must be easily accessible for patients to truly participate in informed medical decision-making processes. This provision of information is particularly important when patients are faced with making a choice in the absence of definitive evidence to guide the assessment of their options. Although men’s perceived awareness of prostate cancer screening may be high, many do not have a complete understanding of the issue.7 The presence of psychosocial barriers, including perceived emasculation/embarrassment during physical examination of the reproductive organs, stoicism, and anxiety associated with diagnostic tests, may prevent men from accessing traditional sources of patient education.7 This inability to access high-quality information from traditional patient education sources may negatively influence men to make an uninformed medical decision.
Findings from this study lend further support to the notion that the internet is a viable method of delivering patient education materials and one that may circumvent psychosocial barriers including embarrassment, anxiety, and stoicism.7,8 Accessing health information online in this patient-perceived nonthreatening environment increases men’s knowledge and understanding on prostate cancer screening.11 However, information delivered online also has the potential to increase a patient’s confidence to initiate a discussion with their doctor about their health situation, feeling that they can equally contribute to the discussion and decision-making process.8 In the next few years, data from large RCTs will provide further evidence on the benefits and limitations of prostate cancer screening3—evidence that may be substantially different to current recommendations. It is essential that patients have access to such information that may influence their decision-making behavior quickly and in a manner most conducive to their learning style.
A major strength of this study was the low attrition rate. However, study recruitment relied on men to volunteer as participants, thereby potentially introducing volunteer bias to the study. Compliance with viewing the materials and previous history of prostate cancer screening were participant reported. Access to patient medical records could have also confirmed participants’ previous history for prostate cancer screening; however, this was beyond the scope of this trial. A further limitation of this study was that participant satisfaction with the educational materials and the format of delivery was not measured. It was also noted that more than half of the participants recruited in this study were regular users of the internet. Therefore, it is possible that these participants may have accessed further information online before their follow-up. During the recruitment period for this study, a variety of prostate cancer awareness campaigns were advertised. This may have impacted on baseline decisional conflict scores, but because participants were randomized to the intervention groups, it is unlikely to have affected our estimates of intervention effects.
CONCLUSION
Patient education materials increase knowledge and decrease decisional conflict and anxiety associated with making medical decisions.30 With more patients wanting more than just “basic” levels of information, future research could center on the most effective method of providing different levels (i.e., basic, intermediate, and advanced) of patient information. If such materials are presented via the internet, then further research must be undertaken to investigate the impact of the public’s health literacy to comprehend such information. Until the results of randomized controlled trials about effectiveness of prostate cancer screening are available in the next few years, patient education materials should explain the benefits and risks associated with prostate cancer screening. Men should have free access to high-quality evidence-based information in a format most suited to their learning style.
References
Parkin D, Bray F, Devesa S. Cancer burden in the year 2000. The global picture. Eur J Cancer. 2001;37:S4–S66.
Frankel S, Smith G, Donovan J, Neal D. Screening for prostate cancer. Lancet. 2003;361:1122–8.
Ilic D, O’Connor D, Green S, Wilt T. Screening for prostate cancer. Cochrane Database Syst Rev. Issue 3, 2006.
Eysenbach G, Jadad A. Evidence-based patient choice and consumer health informatics in the internet age. J Med Internet Res. 2001;3:e19.
O’Connor A, Rostom A, Fiset V, et al. Decision aids for patients facing health treatment or screening decisions: systematic review. Br Med J. 1999;319:731–4.
O’Connor A. Decisional conflict scale. 4th Edition, 1999. Available at; http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_DecConflict2006.pdf. Accessed July 4, 2007.
Ilic D, Risbridger G, Green S. The informed man: attitudes and information needs on prostate cancer screening. Journal of Men’s Health and Gender. 2005;2:414–20.
Ziebland S, Chapple A, Dumelow C, Evans J, Prinjha S, Rozmovits L. How the internet affects patients’ experience of cancer: a qualitative study. Br Med J. 2004;328:564–70.
Flood A, Wennberg J, Nease R, Fowler F, Ding J, Hynes L. The importance of patient preference in the decision to screen for prostate cancer. J Gen Intern Med. 1996;11:342–9.
Frosch D, Kaplan R, Felitti V. Evaluation of two methods to facilitate shared decision making for men considering the prostate-specific antigen test. J Gen Intern Med. 2001;16:391–8.
Frosch D, Kaplan R, Felitti V. A randomised controlled trial comparing internet and video to facilitate patient education for men considering the prostate specific antigen test. J Gen Intern Med. 2003;18:781–7.
Gattellari M, Ward J. Does evidence-based information about screening for prostate cancer enhance consumer decision-making? A randomized controlled trial. J Med Screen. 2003;10:27–39.
Gattellari M, Ward J. A community-based randomized controlled trial of three different educational resources for men about prostate cancer screening. Patient Educ Couns. 2005;57:168–82.
Partin M, Nelson D, Radosevich D, et al. Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences and behaviors. J Gen Intern Med. 2004;19:835–42.
Ruthman J, Ferrans C. Efficacy of a video for teaching patients about prostate cancer screening and treatment. Am J Health Promot. 2004;18:292–5.
Volk R, Cass A, Spann S. A randomized controlled trial of shared decision making for prostate cancer screening. Arch Fam Med. 1999;8:333–40.
Schapira M, Van Ruswyk J. The effect of an illustrated pamphlet decision—aid on the use of prostate cancer screening tests. J Fam Pract. 2000;49:418–24.
Davison J, Kirk P, Degner L, Hassard T. Information and patient participation in screening for prostate cancer. Patient Educ Couns. 1999;37:255–63.
Wilt T, Paul J, Murdoch M, Nelson D, Nugent S, Rubins H. Educating men about prostate cancer screening. A randomized trial of a mailed pamphlet. Eff Clin Pract. 2001;4:278–86.
Schapira M, Meade C, Nattinger A. Enhanced decision-making: the use of a videotape decision—aid for patients with prostate cancer. Patient Educ Couns. 1997;30:119–27.
Tate D, Wing R, Winett R. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–7.
Christensen H, Griffiths K, Jorm A. Delivering interventions for depression by using the internet: randomised controlled trial. Br Med J. 2004;328:265–70.
Scherrer-Bannerman A, Fofonoff D, Minshall D, et al. Web-based education and support for patients on the cardiac surgery waiting list. J Telemed Telecare. 2000;6:s72–74.
O’Connor A. Validation of a decisional conflict scale. Med Decis Mak. 1995;15:25–30.
Marteau T, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State-Trait Anxiety Inventor. Br J Clin Psychol. 1992;31:301–6.
Degner L, Sloan J. Decision making during serious illness: what role do patients really want to play? J Clin Epidemiol. 1992;45:941–50.
Murray E, Davis H, Tai S, Coulter A, Gray A, Haines A. Randomized controlled trial of an interactive multimedia decision aid on benign prostatic hypertrophy in primary care. Br Med J. 2001;323:1–6.
Wei L, Zhang J. Analysis of data with imbalance in the baseline outcome variable for randomized clinical trials. Drug Inf J. 2001;35:1201–14.
Scott S, Goldberg M, Mayo N. Statistical assessment of ordinal outcomes in comparative studies. J Clin Epidemiol. 1997;50:45–55.
Murray E, Burns J, See Tai S, Lai R, Nazareth I. Interactive health communication applications for people with chronic disease. Cochrane Database Syst Rev. Issue 4, 2005.
Acknowledgments
A portion of the results from this manuscript was presented at the 2nd Asia-Pacific Forum on Andrology, October 27, 2006, Shanghai, China. This work was funded by internal funding from the Monash Institute of Health Services Research.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ilic, D., Egberts, K., McKenzie, J.E. et al. Informing Men about Prostate Cancer Screening: A Randomized Controlled Trial of Patient Education Materials. J GEN INTERN MED 23, 466–471 (2008). https://doi.org/10.1007/s11606-007-0466-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0466-z