Abstract
BACKGROUND
Patients’ race and ethnicity play an important role in quality of and access to healthcare in the United States.
OBJECTIVES
To examine the influence of ethnicity – Hispanic whites vs. non-Hispanic whites – on respondents’ self-reported interactions with healthcare providers. To understand, among Hispanic whites, how demographic and socioeconomic characteristics impact their interactions with healthcare providers.
DESIGN
Cross-sectional analysis of the 2002 Medical Expenditure Panel Survey, a nationally representative survey on medical care conducted by the Agency for Healthcare Research and Quality.
PARTICIPANTS
Civilian, noninstitutionalized U.S. population aged ≥18 years who reported visiting a healthcare provider within the past 12 months prior to data collection.
RESULTS
After controlling for several demographic and socioeconomic covariates, compared to non-Hispanic whites (reference group), Hispanic whites who had visited a doctor’s office or clinic in the past 12 months were more likely to report that their healthcare provider “always” listened to them [odds ratio (OR) = 1.36, 95% confidence interval (CI) 1.21–1.53], explained things so that they understood (OR = 1.25, 95% CI 1.10–1.41), showed respect for what they had to say (OR = 1.52, 95% CI 1.35–1.72), and spent enough time with them (OR = 1.22, 95% CI 1.08–1.38). However, Hispanics were less likely to indicate that their health care provider “always” gave them control over treatment options (OR = 0.83, 95% CI 0.72–0.95) as compared to non-Hispanics. Within the Hispanic population exclusively, age, place of residence, census region, health insurance status, and presence of a usual source of care influenced self-reported interactions with healthcare providers.
CONCLUSION
Hispanic white respondents were more likely to report that some aspects of provider–patient interactions were indicative of high quality, whereas those related to decision-making autonomy were not. These somewhat paradoxical results should be examined more fully in future research.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
As highlighted in the Institute of Medicine’s Unequal Treatment report,1 access to preventive health care services and life-saving technologies varies according to patients’ racial and ethnic characteristics. To date, comparisons have typically focused on health-related disparities between blacks and whites.2,3 Notably, fewer Hispanics receive medical care on a monthly basis in physician offices, outpatient clinics, and emergency departments as compared to whites.4 Not only are Hispanics more likely to have unmet medical needs5 and less access to healthcare,6 but they also tend to be less engaged in medical consultations.7 Furthermore, Hispanics differ from whites in attitudes and beliefs regarding medical procedures8,9 and perceived presence of racial discrimination in healthcare settings.10
For many adults, navigating their way through the healthcare system is an overwhelming task. Theoretical models of health services utilization described by Aday, Andersen, and others have outlined societal factors, patient characteristics, and health services system factors that contribute to the difficulties encountered by certain populations.11–14 Furthermore, the process of obtaining medical care and the complexity of health-related decision making are especially daunting for the one-third of American adults with limited health literacy skills.15 Among Hispanic Americans, the number with limited health literacy skills jumps to two-thirds, thereby defining this ethnic minority group as at risk for having greater difficulty understanding interactions with healthcare providers and experiencing poorer health-related outcomes.15
In light of the importance of patient–healthcare provider interactions in facilitating quality care16 and encouraging patients to be active participants in the process of seeking and obtaining medical care,17 understanding disparities in healthcare communication is crucial to improving outcomes for ethnic minority populations. Because recent studies have reported that Hispanics have lower quality patient–physician interactions18,19 and poorer self-reported health20 as compared to non-Hispanics, we sought to investigate these differences further using data from a survey designed to gather health utilization information from a nationally representative sample of civilian, noninstitutionalized adults. The primary purpose of our study was to examine the influence of ethnicity – Hispanic whites vs. non-Hispanic whites – on respondents’ self-reported interactions and decision-making autonomy with healthcare providers. Although links between health-related outcomes and quality-of-care indicators have been explored across patients with different ethnic backgrounds,18,19,21 little is known regarding these issues within the Hispanic population exclusively. To address this gap, the secondary purpose of our study was to describe the extent to which previously reported demographic and socioeconomic characteristics affect the likelihood that Hispanic respondents report positively about their interactions with healthcare providers.
SUBJECTS AND METHODS
Data Source and Study Population
Data for this study were drawn from the 2002 Medical Expenditures Panel Survey (MEPS) Household Component.22 MEPS Household Component data are collected from a subsample of the National Household Interview Survey via telephone interviews using computer-assisted personal interviewing technology. Bilingual interviewers were available to administer surveys in either English or Spanish, based on the preference of each participant. The MEPS, a nationally representative sample of civilian, noninstitutionalized U.S. adults, utilizes a stratified multistage area probability design in which certain groups (e.g., low income, racial minorities) are oversampled. MEPS respondents are queried on such topics as demographic characteristics; self-reported health status; health insurance coverage; and use of, access to, and satisfaction with healthcare services. In line with the purposes of our study, respondents’ self-reported interactions with healthcare providers regarding communication dynamics and decision-making autonomy were explored.
Study Variables
Dependent Variables
Six MEPS items were used as outcome variables to gauge respondents’ perceptions of communication dynamics and decision-making autonomy with healthcare providers. Four items were asked of MEPS respondents (≥18 years of age) who had visited a healthcare provider within the 12 months preceding data collection. Those reporting a doctor’s office or clinic visit responded to the following questions: (1) “How often did providers listen carefully to you?”; (2) “How often did providers explain things so you understood?”; (3) “How often did providers show respect for what you had to say?”; and (4) “How often did providers spend enough time with you?” Additionally, all respondents who reported having an identified usual source of care (USC) responded to the following 2 items: (5) “If there were a choice between treatments, how often would your provider at your USC ask you to help make the decision?” and (6) “How often does your provider at your USC give you some control over your treatment?” Responses to these 6 items were reported on a 4-point scale (always, usually, sometimes, never).
Independent Variables and Covariates
To address the primary purpose of the study, the dichotomous predictor (independent) variable was respondents’ self-reported ethnicity (Hispanic or non-Hispanic). For consistency and to allow comparison to previous studies, we included only those reporting their race as white. Demographic and socioeconomic covariates were selected according to the health services utilization conceptual models described by Aday, Andersen, and others, including gender, age (at time of interview), place of residence [metropolitan statistical area (MSA)], family income (adjusted for family size), completion of high school (head of household), census region, health insurance status, and USC.11–14 To focus on the secondary purpose of the study, individual effects of demographic and socioeconomic characteristics on communication patterns with healthcare providers were explored within the Hispanic cohort exclusively. In other words, each of the above covariates were treated as independent variables for this stratified multivariate analysis.
Statistical Analysis
All statistical analyses were conducted with SUDAAN (Research Triangle Institute, Research Triangle Park, NC, USA) statistical software (release 9.0.1) to account for the complex survey design of the MEPS. Descriptive comparisons were conducted to explore the relationship of respondent ethnicity across demographic and socioeconomic characteristics. Bivariate chi-square (χ 2) analyses were used to examine differences in demographic and socioeconomic characteristics as a function of respondent ethnicity. Similar descriptive analyses revealed that all characteristics were significantly associated with at least one of the outcome variables; therefore, all were included in the multivariable analyses (P < 0.05). In all tables provided, the reported percentages were weighted to produce estimates for white respondents of both Hispanic and non-Hispanic ethnicities within the civilian, noninstitutionalized U.S. population.
Pertaining to our first aim, multiple logistic regression analyses were performed to assess the impact of ethnicity on respondents’ perceptions of healthcare providers’ communication skills, while controlling simultaneously for the effect of potentially confounding demographic and socioeconomic factors. Second, among the white Hispanic cohort exclusively, a series of multiple logistic regression analyses were performed to explore the independent influence of all demographic and socioeconomic covariates – while simultaneously controlling for all of the other covariates – on respondents’ interactions with healthcare providers. For the purposes of multiple logistic regression analyses, responses to the 6 MEPS items were dichotomized as “always” and “not always” (usually–sometimes–never). Results of the multiple logistic regression models are reported in adjusted odds ratios (ORs) with corresponding 95% confidence intervals (CIs).
RESULTS
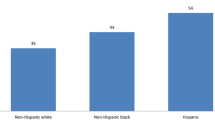
The sample included 12.2% Hispanics (weighted sample size = 25,921,210) and 87.8% non-Hispanics (weighted sample size = 187,029,977). Demographic and socioeconomic characteristics among the white population by ethnicity – Hispanic vs. non-Hispanic – are summarized in Table 1. Males composed 51.1% of Hispanics and 48.2% of non-Hispanics. A larger proportion of Hispanics were younger (18–24 years) than non-Hispanics (18.3 vs. 11.1%). As compared to non-Hispanics, a greater number of Hispanics lived in MSAs (91.9 vs. 78.0%), were poor (18.6 vs. 7.7%), had not completed high school (45.9 vs. 13.6%), were without health insurance (32.7 vs. 9.3%), and did not have a USC (40.1 vs. 17.4%).
After controlling for the effects of demographic and socioeconomic characteristics presented in Table 1, Hispanics who had visited a healthcare provider in the previous 12 months reported more positively about aspects of general communication with healthcare providers than non-Hispanics (Table 2). When compared to non-Hispanics (reference group), Hispanics were more likely to report that their healthcare provider “always” listened to them carefully (adjusted OR = 1.36, 95% CI, 1.21–1.53), explained things so that they understood (adjusted OR = 1.25, 95% CI, 1.10–1.41), showed respect for what they had to say (adjusted OR = 1.52, 95% CI, 1.35–1.72), and spent enough time with them (adjusted OR = 1.22, 95% CI, 1.08–1.38). However, when examining responses pertaining to health care decision-making autonomy among all respondents with a USC, Hispanics were less likely to report that their healthcare provider “always” gave them control over treatment options (adjusted OR = 0.83, 95% CI, 0.72–0.95), as compared to non-Hispanics (reference group). Hispanics were no less likely than non-Hispanics to report that their healthcare provider “always” involved them in healthcare decisions (adjusted OR = 0.87, 95% CI, 0.76–1.00).
Among white Hispanic respondents exclusively, self-reported positive healthcare provider interactions varied as a function of several demographic and socioeconomic factors (Table 3). Among those who had visited a healthcare provider in the past year, those living in MSAs (vs. non-MSAs) and without a USC (vs. with a USC) were less likely to report that their healthcare provider “always” listened to them, explained things so that they understood, respected them, and spent enough time with them (P < 0.01). The youngest age groups (18–24 and 25–44 years) and those without health insurance reported poorer interactions with healthcare providers as compared to older (≥65 years) and publicly insured respondents (P < 0.01). Those living in the Northeast and Midwest were more likely to indicate that healthcare providers “always” showed respect for what they had to say and spent enough time with them as compared to those living in the West (P < 0.01). Differences in self-reported interactions with healthcare providers did not emerge based on family income or educational attainment.
Among Hispanic respondents with a USC exclusively, decision-making autonomy was associated with some of the same demographic and socioeconomic characteristics as healthcare provider interactions reported in Table 3. However, there were some notable differences (Table 4). Poor respondents (vs. high income) were less likely to report that their healthcare provider involved them in decision-making (P < 0.01). As compared to females, males were less likely to report that their healthcare provider “always” gave them control over treatment options (P < 0.01). Those living in the South and Northeast were more likely to indicate that they were involved in autonomy-making decisions than those living in the West (P < 0.01).
DISCUSSION
In this nationally representative sample of civilian, noninstitutionalized U.S. white adults, differences in interactions with healthcare providers emerged between those of Hispanic and non-Hispanic backgrounds. Contrary to our expectations and somewhat inconsistent with previous research, Hispanics were more likely to report that their healthcare provider “always” listened carefully, explained things so that they understood, respected them, and spent enough time with them. For instance, in previous analyses of nationally representative samples (Community Tracking Survey and Commonwealth Fund’s Health Care Quality Survey) of U.S. adults – using similar survey items to those employed in the MEPS – Hispanics reported poorer quality of interactions with healthcare providers.18,19 Furthermore, as part of the 2000 Behavior Risk Factor Surveillance System (BRFSS), adults from 3 states responded to similar survey items contained in the MEPS.21 Based on an analysis of BRFSS data, after adjustment for various demographic covariates, Hispanics were more likely to report that healthcare providers did not carefully listen to them as compared to non-Hispanics; however, respondent ethnicity was not related to differences in other communication variables.21
Although we cannot fully explain the inconsistency between our findings and previous research, such factors as variation in demographic characteristics of survey participants, discrepancies in formatting and administration of survey items, and variable response rates may contribute to these differences. Furthermore, data comparing Hispanics to non-Hispanics are scarce, thereby limiting our ability to draw widespread comparisons and conclusions. Therefore, our results suggest a need to explore how individual survey items are constructed, interpreted, and best administered among Hispanics. As a next step, the use of qualitative methodologies such as focus groups and in-depth interviews might help to improve quantitative instruments for this population in the future.
Why did Hispanics in this study report better communication dynamics with healthcare providers but less decision-making autonomy? Our findings that Hispanics felt listened to and respected but not necessarily included in decision making may be related to healthcare provider characteristics, as well as the patient’s ethnicity. Furthermore, linguistic factors may also be operating in the context of our analysis. Rudimentary Spanish skills among non-Hispanic healthcare providers may provide an initial feeling of being treated well and listened to in the history-gathering phase of the medical encounter, but providers’ language skills may not be advanced enough to adequately negotiate treatment options with a Hispanic, Spanish-speaking patient. Furthermore, lower levels of health literacy skills among Hispanic patients may influence communication dynamics within the medical encounter itself.15
Our findings do concur with those of Saha et al.19 in that Hispanics were less likely to report decision-making autonomy with healthcare providers. These findings suggest that healthcare providers may be more paternalistic with Hispanic patients when it comes to decision making, perhaps related to language barriers and/or unfamiliarity with cultural differences and expectations. Levinson et al.23 reported that Hispanics were more likely to rely on physicians’ medical knowledge rather than seeking out information themselves, and this population feels more comfortable with physicians making treatment-related decisions. Therefore, there may be cultural explanations for these findings, as educational attainment did not influence differences among the Hispanic cohort exclusively. Discordance in patient–physician ethnicity might also play a role.
Within the Hispanic population exclusively, several factors influenced self-reported interactions with healthcare providers, including age, place of residence, census region, health insurance status, and presence of a USC. Furthermore, those living in poverty and from urban areas were less likely to report being asked by healthcare providers to help make medical care decisions. Interestingly, Hispanic women were more likely to report being given control of medical treatments, compared to their male counterparts.
Our results should be considered in the context of several limitations. First, although the MEPS is representative of the civilian, noninstitutionalized U.S. population, the cross-sectional format limits causal inferences. Second, we were unable to control for certain patient-related variables shown to influence healthcare interactions (e.g., respondents’ health literacy skills and preferred language,15 respondents’ degree of acculturation,24 and gender–race concordance between respondent and healthcare provider25,26) not available in the MEPS. Third, as with all observational studies that rely on self-reports, response bias remains a possibility. Fourth, the survey and our analysis did not take into account healthcare provider characteristics. The culture of medicine has all its own behavioral norms, and the cultural background of the provider influences his/her style of interaction within the medical encounter itself. Lastly, those categorized into the same ethnic group do in fact represent large and highly divergent geographic, cultural, and linguistic backgrounds.
Understanding the variables, both in providers and in patients, that influence differences and disparities in healthcare communication and decision-making autonomy is crucial to achieving equal healthcare treatment for all Americans. When studying healthcare experiences of Hispanic Americans, who will represent over 20% of the U.S. population by the year 2030, evidence is still inconclusive and warrants further study.27 Healthcare providers should be cognizant of the unique communication issues faced by Hispanic patients who are at risk for poor health-related outcomes. Within this ethnic minority population, differences were reported in how patients viewed interactions with health care providers, suggesting that further training and continuing medical education must emphasize both cultural competency and how to best meet the unique needs of each individual patient.
References
Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2002.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282:583–9.
Halbert CH, Armstrong K, Gandy OH, Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166:896–901.
Bliss EB, Meyers DS, Phillips RL, Fryer GE, Dovey SM, Green LA. Variation in participation in health care settings associated with race and ethnicity. J Gen Intern Med. 2004;19:931–6.
Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809–29.
Taira DA, Safran DG, Seto TB, et al. Do patient assessments of primary care differ by patient ethnicity? Health Serv Res. 2001;36:1059–71.
Street RL, Gordon HS, Ward MM, Krupat E, Kravitz RL. Patient participation in medical consultations: why some patients are more involved than others. Med Care. 2005;43:960–9.
Kroll TL, Richardson M, Sharf BF, Suarez-Almazor ME. “Keep on truckin’” or “It’s got you in this little vaccum”: race-based perceptions in decision-making for total knee arthroplasty. J Rheumatol. 2007;34:1069–75.
Chen JY, Fox SA, Cantrell CH, Stockdale SE, Kagawa-Singer M. Health disparities and prevention: racial/ethnic barriers to flu vaccinations. J Community Health. 2007;32:5–20.
Chen FM, Fryer GE, Phillips RL, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Ann Fam Med. 2005;3:138–43.
Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res. 1974;9:208–20.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10.
Phillips KA, Morrison KR, Andersen R, Aday AL. Understanding the context of healthcare utilization: assessing environmental and provider-related variables in the behavioral model of utilization. Health Serv Res. 1998;33:571–96.
Cheraghi-Sohi S, Bower P, Mead N, McDonald R, Whalley D, Roland M. What are the key attributes of primary care for patients? Building a conceptual ‘map’ of patient preferences. Health Expect. 2006;9:275–84.
National Center for Education Statistics. The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Available at: http://nces.ed.gov/pubs2006/2006483.pdf. Accessed May 7, 2007.
Roter DL, Hall JA. Doctors Talking with Patients/Patients Talking with Doctors, 2nd edition. Westport, CT: Praeger; 2006.
Institute of Medicine. Improving the 21st Century Healthcare System. Crossing the Quality Chasm: A New Healthcare System for the 21st Century. Washington, DC: National Academy Press; 2001.
Doescher MP, Saver BG, Franks P, Fiscella K. Racial and ethnic disparities in perceptions of physician style and trust. Arch Fam Med. 2000;9:1156–63.
Saha S, Arbelaez JJ, Cooper LA. Patient–physician relationships and racial disparities in the quality of health care. Am J Public Health. 2003;93:1713–9.
Kandula NR, Lauderdale DS, Baker DW. Differences in self-reported health among Asians, Lationos, and non-Hispanic whites: the role of language and nativity. Ann Epidemiol. 2007;17:191–8.
Merrill RM, Allen EW. Racial and ethnic disparities in satisfaction with doctors and health providers in the United States. Ethn Dis. 2003;13:492–8.
Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Available at: http://www.meps.ahrq.gov/mepsweb/. Accessed March 14, 2007.
Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making. J Gen Intern Med. 2005;20:531–5.
Moran A, Diez Roux AV, Jackson SA, et al. Acculturation is associated with hypertension in a multiethnic sample. Am J Hypertens. 2007;20:354–63.
Laveist TA, Nuru-Jeter A. Is doctor–patient race concordance associated with greater satisfaction with care? J Health Soc Behav. 2002;43:296–306.
Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Aff. 2000;19:76–83.
U.S. Census Bureau. US Interim Projections by Age, Sex, Race, and Hispanic Origin. Available at: http://www.census.gov/ipc/www/usinterimproj/. Accessed September 13, 2007.
Acknowledgments
Funding was provided by the Department of Family Medicine at the University of Tennessee Graduate School of Medicine, Knoxville. This paper was presented in part at the 35th Annual Meeting of the North American Primary Care Research Group, October 2007, in Vancouver, Canada.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wallace, L.S., DeVoe, J.E., Rogers, E.S. et al. The Medical Dialogue: Disentangling Differences between Hispanic and non-Hispanic Whites. J GEN INTERN MED 22, 1538–1543 (2007). https://doi.org/10.1007/s11606-007-0368-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0368-0