Abstract
Background
The placebo and the placebo effect are often investigated in the context of clinical trials. Little data exist on the use of placebos in the course of routine health care.
Objective
The aim of this study is to describe a group of academic physicians’ use of placebos and their knowledge, attitudes, and beliefs about placebos and the placebo effect.
Design
A 16-question anonymous web-based survey of physicians from Internal Medicine departments of 3 Chicago-area medical schools was used.
Results
There were 231/466 (50%) physicians who responded; of these, 45% reported they had used a placebo in clinical practice. The most common reasons for placebo use were to calm the patient and as supplemental treatment. Physicians did not widely agree on the definition of a placebo and had a variety of explanations for its mechanism of action. Ninety-six percent of the respondents believed that placebos can have therapeutic effects, and up to 40% of the physicians reported that placebos could benefit patients physiologically for certain health problems. Only 12% of the respondents said that placebo use in routine medical care should be categorically prohibited. Regarding “placebo-like” treatment, 48% of respondents reported giving at least 1 type of treatment in a situation where there was no evidence of clinical efficacy.
Conclusion
Nearly half of the respondents use placebos in clinical practice and most believe in the mind–body connection. The results of this study, based on retrospective self-reported behavior, are subject to recall bias and may not be representative of American physicians.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Recently, there has been an increased interest in exploring placebos and the placebo effect. In 2000, the National Institutes of Health sponsored a conference called “Science of the Placebo,” which brought together 500 medical scholars, researchers, and clinicians9. Between the years 1992 to 2002, the National Library of Medicine reported an annual average of 3,972 scholarly articles that include the keywords “placebo,” “placebos,” or “placebo effect.”15 Whereas a review of results from over a hundred clinical trials that included placebo and no treatment groups “found little evidence that placebos in general have powerful effects,”12 other investigators provide evidence that placebos have effects including specific physiologic consequences. Benedetti and Amanzio1 showed that a placebo intervention could lead to the production of endogenous opiates when used as a form of patient analgesia. The opiate antagonist naloxone reversed the analgesic effects of the placebo.
Despite this heightened interest in placebos, there have been few studies published on placebo use outside of clinical research trials. Two American studies on placebo use in clinical practice were published in 1979.6,7 In one study, the majority (78%) of physicians from 2 university teaching hospitals had administered at least 1 placebo for pain relief and 60% believed placebos could be used as a diagnostic tool to determine whether patient symptoms were “real.”7 Since 1979, only 1 additional American study examined placebo use. The majority of medicine interns in a single residency program reported they were aware of placebo use in clinical practice, but only 16% had ordered a placebo.3 Because there has been no significant research on placebo use by US physicians in over a quarter of a century, we developed a study to explore physicians’ current use, knowledge, attitudes, and beliefs about placebos and the placebo effect.
METHODS
Questionnaire
Questionnaire items measure how physicians define a placebo, use of placebos outside of clinical trials, information given to patients who receive a placebo treatment, perceived therapeutic value and benefits of placebos, circumstances accompanying placebo use, perceived mechanism of action of placebos, and ethical stances about the use of placebos in routine care. Several of the survey questions were adapted from previous studies.13,16 For a copy of the complete questionnaire, please contact the corresponding author.
Analysis
We produced frequency distributions of responses, and we tested associations among physician demographic variables, the frequency of placebo use, and beliefs regarding the therapeutic value of placebos (Pearson Correlation). The percentage totals add up to more than 100% for several questions to which physicians could give more than 1 response.
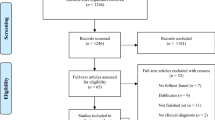
Sample
The questionnaire was distributed electronically using Perseus web-survey software17 to 466 faculty physicians at 3 Chicago-area medical schools: The University of Chicago Pritzker School of Medicine, Northwestern University Feinberg School of Medicine, and the University of Illinois at Chicago School of Medicine. The sampling frame included all Chicago-area department of medicine physician faculty who publicly listed their email contact information (representing over 90% of the total faculty).
Subjects received an email invitation explaining the purpose of the study, the guarantee of anonymity and an individualized online link to the research questionnaire. A maximum of 2 reminder email letters were sent to physicians who did not respond initially unless they were “away from email” in which case they received another round of reminders.
RESULTS
After excluding 23 physicians who reportedly do not actively see patients, 231 (50%) of physicians invited to participate returned the questionnaire. Of the respondents, 20% practice general Internal Medicine, 71% are subspecialty Internists, and 9% are other medical specialists. Seventy-one percent of the respondents are male. The average age of the respondents is 46 years old.
How Physicians Define Placebos
Fifty-one percent of respondents endorsed the definition that a placebo is “an intervention that is not expected to have an effect through a known physiologic mechanism,” 37% of the respondents chose “an intervention not considered to have a ‘specific’ effect on the condition treated, but with a possible ‘unspecific’ effect,” 28% of the respondents chose “an intervention that is inert or innocuous,” while 6% expressed other definitions, such as “an intentionally ineffective medical treatment” and “a sham intervention used as a control to test the safety and effectiveness of the active intervention.”
Frequency of Placebo Use
Forty-five percent of respondents had used a placebo for clinical care with 15% doing so 1 to 10 times, 8% more than 10 times, and 22% not at all in the last year. When asked about the practices of other physicians and nurses, 80% of respondents believed their colleagues used placebos during routine care (60% “rarely,” 18% “sometimes,” 2% “often”).
Circumstances of Placebo Use
Physicians used placebos in a variety of circumstances. Of the respondents who used placebos, the most common reason was to calm the patient (18%) and as supplemental treatment (18%). Other reasons included “after ‘unjustified’ demand for medication” (15%), “for nonspecific complaints” (13%), “after all clinically indicated treatment possibilities were exhausted” (11%), “to control pain” (6%), “to get the patient to stop complaining” (6%), and “as a diagnostic tool” (4%). In addition, 80% of respondents disagreed with the statement, “I think a placebo intervention can help distinguish symptoms that have a psychogenic versus an organic origin.”
Examples of Treatments Given in Situations Where There Has Been No Demonstrated Clinical Efficacy
Forty-eight percent of physicians reported giving at least 1 type of treatment in a situation where there was no evidence of clinical efficacy. Among treatments given were antibiotics for viral or other nonbacterial diagnoses (33%), vitamins (20%), ibuprofen (12%), subtherapeutic doses of medication (7%), herbal supplements (5%), saline infusions (3%), prepared placebo tablets (2%), and sugar or artificial sweetener pills (1%).
Perceived Mechanism of Action
Physician responses regarding placebo’s mechanism of action are shown in Figure 1. In addition, 5% had other responses such as “brain–body connection,” “incompletely elucidated psychoneuroimmunological pathways” and “regression to the mean.”
Ethical Stance Toward Use of Placebos in Routine Health Care Practice
Only 12% of respondents said that placebo use should be categorically prohibited. The rest indicated placebos could be permitted in certain circumstances, including when research supported its efficacy (46%), if the experience of colleagues supported it (9%), after notifying the patient he/she is receiving a placebo (21%), or if the physician anticipated the placebo would benefit the patient (31%). Some physicians expressed additional opinions such as, “after notifying the patient that he/she MAY receive a placebo.”
Information Given to Patients
Of the respondents who reported using placebos in the course of routine health care, 34% introduced the placebo to the patient as “a substance that may help and will not hurt,” 19% said, “it is medication,” 9% said, “it is medicine with no specific effect.” Only 4% of the physicians explicitly said, “it is a placebo.” In addition, 33% of the physicians reported they gave other information to patients including, “This may help you but I am not sure how it works.”
Potential Benefits of Placebos for Various Health Problems
Ninety-six percent of physicians believed “placebos have therapeutic effects” (21% “rarely,” 58% “sometimes,” and 16% “often”). In a similar question, 95% of physicians believed that “the placebo effect is real” (68% “agreed” and 27% “strongly agreed”). Physicians were asked what types of health problems could benefit from placebo interventions and whether the perceived benefits were psychological, physiological, or both. Results to this question are in Table 1.
Perceived Benefits of Other Treatments or Factors Sometimes Associated with Placebos
We asked physicians about the possible benefits of other treatments and factors that may influence health according to a definition of a placebo (i.e., their physiologic mechanism of action is unknown or nonspecific). Physician responses are listed in Table 2.
Relationship Between Variables
There were no statistically significant associations between physician demographics (specialty, age, and gender) and frequency of placebo use or beliefs regarding the therapeutic value of placebos. Physicians who reported using a placebo were more likely to believe in the therapeutic value of placebos (Pearson correlation = 0.189, p < .01).
DISCUSSION
This is the first study examining American physicians’ use of placebos in clinical practice in the twenty-first century. Forty-five percent of physician respondents from 3 academic medical centers in Chicago reported that they had prescribed or administered a placebo. The circumstances accompanying placebo use varied, as did the explanations given to patients at the time of a placebo intervention. Furthermore, 48% of physicians reported giving a treatment to patients in situations where there was no demonstrated clinical efficacy. This study indicates a need for greater recognition of the use of placebos and unproven therapies and discussion about its implications.
Eight previous survey studies of hospital-based physicians or nurses showed that between 10 and 80% of respondents had used placebos in clinical practice.3,5,8,11 Of the 2 most recent studies, the prevalence of placebo use was over 50%, and the majority of respondents agreed that use is ethical under certain circumstances.13,16 In the broader ethics literature, some commentators on informed consent and nondeceptive therapeutics caution against the use of placebos in medical practice.9 Others propose that the placebo effect can be harnessed in various therapeutic contexts that do not pose ethical dilemmas.2,4,15
History of science professor Anne Harrington10 associates placebos with a broader category of interventions and factors that affect “psychobiological functioning.” Anthropologist Daniel Moerman14 conceptualizes the placebo effect in terms of “the meaning response,” defined as “the physiological or psychological effects of meaning in the treatment of illness” (p. 77). Just 28 years ago, Goodwin et al.7 reported that the majority of academic physicians thought placebos could help determine whether a patient’s symptoms were “real” or if the patient was “faking.” Our data support that a growing number of physicians believe in a mind–body connection. For instance, our physician respondents generally believed that placebos have therapeutic effects and do not help differentiate between psychogenic versus organic symptoms.
This study has limitations. Given the convenience sample studied, the results of this study may not be representative of American physicians in general. Whereas the guarantee of anonymity aimed to eliminate reporting bias, some respondents may have misreported their use of placebos. Also, given the data are self-reported and retrospect, our results are subject to recall bias. Additional studies are necessary to assess the routine use of placebos outside of academic medicine and in other geographic regions.
References
Benedetti F, Amanzio M. The neurobiology of placebo analgesia: from endogenous opioids to cholecystokinin. Prog Neurobiol. 1997;52(2):109–25.
Benson H. Timeless healing: the power and biology of belief. New York: Simon and Schuster; 1996.
Berger JT. Placebo medication use in patient care: a survey of medical interns. West J Med. 1999;170:93–6.
Brody H. Placebos and the philosophy of medicine. Chicago: University of Chicago Press; 1980.
Ernst E, Abbot NC. Placebos in clinical practice: results of a survey of nurses. Perfusion. 1997;10:128–30.
Goldberg RJ, Leigh H, Quinlan D. The current status of placebo in hospital practice. Gen Hosp Psych. 1979;1(3):196–201.
Goodwin JS, Goodwin JM, Vogel AV. Knowledge and use of placebos by house officers and nurses. Ann Intern Med. 1979;91(1):106–10.
Gray G, Flynn P. A survey of placebo use in a general hospital. Gen Hosp Psych. 1981;3(3):199–203.
Bok S. Ethical issues in use of placebo in medical practice and clinical trials. In: Guess HA, Kleinman A, Kusek JW, Engel LW, eds. The science of the placebo: toward an interdisciplinary research agenda. London: BMG Books; 2002, pp. 53–74.
Harrington A. “Seeing” the placebo effect: historical legacies and present opportunities. In: Guess HA, Kleinman A, Kusek JW, Engel LW, eds. The science of the placebo: toward an interdisciplinary research agenda. London: BMJ Books; 2002:35–53.
Hofling CK. The place of placebos in medical practice. GP. 1955;11(6):103–7.
Hrobjartsson A, Gotzsche PC. Is the placebo powerless? An analysis of clinical trials comparing placebo with no treatment. N Engl J Med. 2001;344(21):1594–602.
Hrobjartsson A, Norup M. The use of placebo interventions in medical practice—a national questionnaire survey of Danish clinicians. Eval Health Prof. 2003;26(2):153–65.
Moerman D. Explanatory mechanisms for placebo effects: cultural influences and the meaning response. In: Guess HA, Kleinman A, Kusek JW, Engel LW, eds. The science of the placebo: toward an interdisciplinary research agenda. London: BMJ Books; 2002:77–108.
Moerman D, Jonas W. Deconstructing the placebo effect and finding the meaning response. Ann Intern Med. 2002;136(6):471–7.
Nitzan U, Lichtenberg P. Questionnaire survey on use of placebo. Br Med J. 2004;329(7472):944–6.
Perseus web-based survey solutions. Available at http://www.perseus.com.
Further READING
Brown WA. The placebo effect. Sci Am. 1998;278:68–73.
Harrington A, eds. The placebo effect: an interdisciplinary exploration. Cambridge: Harvard University Press; 1997.
Kendler KS. A psychiatric dialogue on the mind–body problem. Journal of American Psychiatry. 2001;158(7):989–1000.
Lynoe N, Mattsson B, Sandlund M. The attitudes of patients and physicians towards placebo treatment—a comparative study. Soc Sci Med. 1993;36(6):767–74.
Shapiro AK, Struening EL. The use of placebos: A study of ethics and physician attitudes. Psychiatr Med. 1973;4:17–29.
Thomson RJ, Buchanan WJ. Placebos and general practice: attitudes to, and the use of, the placebo effect. NZ Med J. 1982;95(712):492–4.
Acknowledgment
Many thanks to Sinan Kermen, Sandy Cook, Sandy Smith, and Jamie Cohen-Cole for their support.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sherman, R., Hickner, J. Academic Physicians Use Placebos in Clinical Practice and Believe in the Mind–Body Connection. J GEN INTERN MED 23, 7–10 (2008). https://doi.org/10.1007/s11606-007-0332-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0332-z