Abstract
BACKGROUND
Hospital-based clinicians and educators face a difficult challenge trying to simultaneously improve measurable quality, educate residents in line with ACGME core competencies, while also attending to fiscal concerns such as hospital length of stay (LOS).
OBJECTIVE
The purpose of this study was to determine the effect of multidisciplinary rounds (MDR) on quality core measure performance, resident education, and hospital length of stay.
DESIGN
Pre and post observational study assessing the impact of MDR during its first year of implementation.
SETTING
The Norwalk Hospital is a 328-bed, university-affiliated community teaching hospital in an urban setting with a total of 44 Internal Medicine residents.
METHODS
Joint Commission on Accreditation of Healthcare Organizations (JCAHO) core measure performance was obtained on a monthly basis for selected heart failure (CHF), pneumonia, and acute myocardial infarction (AMI) measures addressed on the general medical service. Resident knowledge and attitudes about MDR were determined by an anonymous questionnaire. LOS and monthly core measure performance rates were adjusted for patient characteristics and secular trends using linear spline logistic regression modeling.
RESULTS
Institution of MDR was associated with a significant improvement in quality core measure performance in targeted areas of CHF from 65% to 76% (p < .001), AMI from 89% to 96% (p = .004), pneumonia from 27% to 70% (p < .001), and all combined from 59% to 78% (p < .001). Adjusted overall monthly performance rates also improved during MDR (odds ratio [OR] 1.09, CI 1.06–1.12, p < .001). Residents reported substantial improvements in core measure knowledge, systems-based care, and communication after institution of MDR (p < .001). Residents also agreed that MDR improved efficiency, delivery of evidence-based care, and relationships with involved disciplines. Adjusted average LOS decreased 0.5 (95% CI 0.1–0.8) days for patients with a target core measure diagnosis of either CHF, pneumonia, or AMI (p < .01 ) and by 0.6 (95% CI 0.5–0.7) days for all medicine DRGs (p < .001).
CONCLUSIONS
Resident-centered MDR is an effective process using no additional resources that simultaneously improves quality of care while enhancing resident education and is associated with shortened length of stay.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Hospital-based educators and clinicians have recently found themselves in the center of multiple seemingly discordant pressures. How does an institution allocate resources to improve measurable quality and tackle requirements for residency education while simultaneously addressing the reality of increasing fiscal constraints? A realistic approach should include the design of efficient, sustainable processes that address these issues yet require minimal additional resources.
The challenge to improve quality of care set forth by the Institute of Medicine1 has been met with less than satisfactory results in the area of core measure performance. A report in 2004 of the core measures assessed by the Centers for Medicare and Medicaid Services (CMS) and Joint Commission on Accreditation of Healthcare Organizations (JCAHO), for example, revealed that only 46% of patients eligible for pneumococcal vaccine with community-acquired pneumonia received it, whereas 1 out of every 11 patients with a myocardial infarction eligible for aspirin on arrival did not receive that potentially life-saving treatment.2 Furthermore, public reporting of quality core measures by JCAHO and CMS and the potential advent of pay for performance have placed quality improvement in the forefront of hospitals’ priorities.
Physicians based at teaching hospitals also face the challenge of ensuring that their trainees deliver high-quality medicine. The Accreditation Council for Graduate Medical Education (ACGME) has defined core competencies as patient care, medical knowledge, practice-based learning improvement, interpersonal and communication skills, professionalism, and system-based improvement. These core competencies recognize the importance of the delivery of evidence-based care and training in systems of care. Demonstration that residents are progressing in these core competencies requires steps beyond traditional teaching and documentation.3,4 Hospital-based clinicians and educators must attend to these quality and educational priorities while also focusing on the fiscally driven requirement to improve patient flow and reduce length of stay.
Unfortunately, traditional strategies for changing hospital practices and especially physician behavior have limited value. The dissemination of information alone, without direct human intervention, does not significantly affect management.5 Despite wide promulgation, clinical practice guidelines alone have only a limited effect in changing physician behavior.6 Moreover, analyses of hospital characteristics associated with high-quality care reveal only an inconsistent advantage of having residency programs, but a positive association with strong leadership and multidisciplinary approaches.7
Given that most teaching hospitals rely on residents to provide a large proportion of inpatient care, we concluded that residents could serve as a strategic resource for improving quality and efficiency—especially when integrated into a multidisciplinary effort. Labresh and colleagues demonstrated, for example, that such an approach can improve performance of measures for secondary prevention of cardiovascular disease.8 Hence, to address quality improvement goals, meet the complimentary needs to train residents in competencies that promote best practice, and achieve operational efficiency, we implemented medical resident-centered thrice-weekly multidisciplinary rounds. In this study, we sought to determine whether resident-centered multidisciplinary rounds lead to achievement of best demonstrated practice in measurable quality as defined by the core measures embraced by JCAHO and CMS while simultaneously enhancing resident education in line with ACGME core competencies and improving length of stay.
METHODS
Setting
Norwalk Hospital is a 328-bed, university-affiliated community teaching hospital in an urban setting. The Department of Internal Medicine supports a residency program of 44, with 14 residents and 1 physician assistant comprising the 5 teams on the inpatient general medical service. Residents rotate in 4-week blocks on the medical teaching service for 4 months as postgraduate year (PGY) 1, 3 months as PGY2, and 2 months as PGY3. Residents care for about 80% of all medical admissions. The remaining 20% of cases are cared for by private medical attendings on the non-teaching service. During the study period, the 4 full-time Hospitalist clinician-educators on faculty were attendings for one-third of the patients on the resident teaching service, with the remaining two-thirds of those patients covered by private medical attending staff. Each of the 5 medical units is directed by a nurse coordinator and served by 1 or 2 case managers. Three pharmacists round on the general medical units and are in charge of drug utilization.
Intervention
With the consent of senior hospital administrators, representatives were drawn from all departments directly involved in patient care to form a multidisciplinary team. Members of the team observed the conduct of multidisciplinary rounds at another hospital (Berkshire Medical Center, Pittsfield, MA) to gain familiarity with it and enhance acceptance. In addition to members of the internal medical service, the multidisciplinary team is comprised of case managers and nurse coordinators from each of the non-intensive care medical units, a dietician, pharmacists, and representatives from the physical medicine and psychiatric services. MDR is led by the chief of medicine and a clinician-educator and conducted on Monday, Wednesday, and Friday from 10 to 11 a.m. in a conference room located in the center of the 2 main general medicine units. The core measure descriptions are posted on a bulletin board in the conference room and loaded on residents’ personal data assistant (PDA) devices. Monthly core measure performance is highlighted in figures displayed in the MDR conference room. Senior administrators, including the hospital chief executive and operating officers, provided visible support for MDR by occasionally sitting through rounds.
One to 2 hours before MDR, nurses and/or case managers gather data on the patients related to diagnoses, care issues, and core measure compliance. Starting at 10 a.m., the first of the 5 resident teams is paged by the physician leaders. Case manager or nurses from each unit present thumbnail descriptions of the cases, residents respond and integrate suggestions from all members of the MDR team into the patient’s care plan, whereas the physician leaders facilitate and advise. Tasks are assigned to the appropriate members of the care team. Resident teams leave upon completion of their patient list. Summoned by a physician leader’s page just before the completion of the preceding team’s discussions, the next team takes it turn. Given that 50 to 80 patients are discussed, the MDR team focuses exclusively on quality and core measure compliance, advancement of care, system barrier recognition and removal, clarification of diagnoses, coding accuracy and optimization, drug dosing and safety, and exchange of other essential clinical information. Formal didactics and issues requiring prolonged discussions are handled outside of MDR. Rounds on the entire resident teaching service usually are completed in 1 hour and never extend beyond 5 minutes past the hour.
Outcomes
The JCAHO core measures are evidence-based, peer reviewed quality markers of common inpatient diagnoses.9 Given the focus on inpatient medicine quality, we selected as outcomes the performance of all core measures that could be affected by MDR. For congestive heart failure, the core measures chosen were discharge instructions, left ventricular function (LVF) assessment, angiotensin-converting enzyme inhibitor (ACEI) for left ventricular systolic dysfunction (LVSD), and smoking-cessation counseling. For acute myocardial infarction, the core measures chosen were aspirin prescribed at discharge, ACEI for LVSD, smoking-cessation counseling, and beta-blocker prescribed at discharge. For community-acquired pneumonia, the core measures chosen were pneumococcal vaccination and smoking-cessation counseling. Whereas important, the remaining core measures were controlled by either the intensive care unit or emergency department, and not by the general medical units.
The impact of MDR on length of stay and resident education and attitudes were also assessed. Lengths of stay were determined for all medical patients 1 year before MDR, and for the first year of MDR. To gauge their knowledge and attitudes about MDR, residents completed an anonymous questionnaire.
Data Collection
Core Measures
In 2002, our quality improvement team joined the National Voluntary Hospital Reporting Initiative through the American Hospital Association. Data on core measures performance were abstracted and reported to the Connecticut Hospital Association (CHA) by a nurse abstractor in accordance with JCAHO policy as outlined in the Specifications Manual for National Hospital Quality Measures Version 1.0.10 All patient data were included for submission to the CHA for patients age 18 and older with a principal diagnosis ICD9-CM code for AMI, CHF, or pneumonia according to Tables 1.1, 2.1, and 3.1 provided in Appendix A of the JCAHO Specifications Manual.10 Patients were excluded from the study according to the algorithm for each specific core measure. These data were reported on a monthly basis to the CHA for distribution to CMS and JCAHO. A CMS Clinical Data Abstraction Center audit of 66 data elements from July 2004 through September 2004 yielded an overall abstraction reliability score of 95%. Core measure data and patient comorbidities used in this study were obtained from the official verified reports sent from the CHA.
Length of Stay
Data regarding LOS were drawn from an administrative data base and sorted according to medical attending and medical diagnosis between July 2002 and June 2004, inclusively.
Resident Survey
Residents received an anonymous 2-section questionnaire that they answered privately after completing at least 2 blocks (8–12 weeks) of the new MDR on the general medical service. Residents placed the completed questionnaires in a basket and checked off their names from a posted list. Questionnaires were retrieved as a group only after all residents had checked off their names. The first section utilized a 5-point Likert scale for residents to recall their level of knowledge and attitudes before MDR, and then after completing at least 2 blocks of MDR. The second section assessed agreement or disagreement with statements about the value of MDR on a 5-point Likert scale. The questions were chosen thorough consensus agreement by the authors regarding which ACGME Core Competencies the MDR could affect and the potential impact on resident working conditions.
Data Analysis
Core Measures
Core measure performance and LOS was compared as “pre-MDR” from July 2002 to June 2003 and “MDR” from July 2003 to June 2004, inclusively. Core measure performance was assessed by tabulating either the success at or failure to satisfy each individual core measure requirement. These data were further grouped into their appropriate “targeted” category by pooling total successes versus eligible patients for CHF, AMI, and pneumonia, respectively. Bivariate analyses were performed to assess differences in patient’s characteristics and core measure performance before and after institution of MDR across the 3 targeted groups. Pre-post comparisons of aggregate categorical data were conducted with chi square tests, and continuous variables with t tests. Monthly rates of core measure performance were adjusted for patient characteristics and secular trends using linear spline logistic regression modeling.11 All statistical analyses were conducted using STATA version 8.0 (STATA Corporation, College Station, TX).
Length of Stay
LOS was calculated by averaging the hospital days, excluding outliers (LOS>30 days), used by each patient in the corresponding group studied. The average LOS was computed for “targeted diagnoses” and all medicine diagnoses. Targeted diagnoses consisted of DRG 127 Heart Failure and Shock, DRG 121 Circulatory Disorders with Acute Myocardial Infarction, and DRG 089/090 Simple Pneumonia and Pleurisy. LOS was adjusted for patient characteristics and secular trends using linear spline logistic regression modeling.
Resident Survey
For the resident questionnaire, statistical significance of resident knowledge and attitudes about MDR in section 1 was calculated using a paired t test on scores before and since MDR. For resident assessments of MDR in section 2, positive responses were judged by a score of either agree or strongly agree (4 or 5 on a 5-point Likert scale).
RESULTS
Core Measures
Comparison of patient characteristics before and after institution of MDR reveals a few differences in ethnicity, payer source and illness severity (Table 1). Analysis of performance of core measures reveals statistically significant improvement in all 3 targeted groups, and in 5 out of 10 individual core measures after the institution of MDR (Table 2). Adjusted montly rates of performance during MDR surpassed the pre-MDR period except for AMI (Table 3).
Length of Stay
Adjusted average LOS decreased 0.5 (95% CI 0.1–0.8) days for patients with the targeted diagnoses of CHF, pneumonia, or AMI (p ≤ .013) and by 0.6 (0.5–0.7) days for all medicine DRGs (p < .001) during this time period (Fig. 1).
Comparison of adjusted average LOS 1 year pre-MDR versus 1 year of MDR on targeted diagnoses (CHF, AMI, and pneumonia) and all medicine diagnoses. LOS was adjusted for patient characteristics and potential secular trends using linear spline logistic regression modeling. Patient characteristics include patients’ age, gender, and comorbidities including COPD, diabetes mellitus, hypertension, and dementia. Bars represent the 95% confidence interval. *p = .013, †p < .001
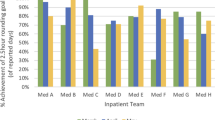
Resident Survey
The resident assessment of MDR questionnaire was completed by 100% of the medical residents (13 PGY-2 and 13 PGY-3). Residents reported substantial improvements in core measure knowledge, systems-based care, and communication with involved disciplines after institution of MDR (p < .001) (Fig. 2). Residents also agreed that MDR improved efficiency, delivery of evidence-based care, and relationships (Table 4). Although roughly 1 quarter of residents felt uneasy during any point in MDR, none felt “picked on.” Finally, residents responded that MDR is not only a valuable process, but that it yields positive returns on the time spent and improves the overall quality of patient care.
DISCUSSION
These results reveal a robust improvement in quality of care, resident attitudes, and average LOS following institution of MDR. The cost of MDR lies only in the time invested in thrice weekly, hour-long rounds. No additional full-time equivalents (FTEs), equipment, or technology was needed to run MDR, and no other identifiable interventions occurred during this time period.
The data reveal that not only did overall performance increase with MDR, but the overall monthly rates of improvement during MDR exceeded baseline rates. This finding suggests that MDR contributed to core measure success above that expected from concurrent secular influences. When viewed by targeted category, an exception was AMI, which significantly improved overall but did not experience a monthly rate of performance increase. This latter finding is attributable to the near 100% AMI performance during MDR that left little room for rate improvement.
MDR serves as an attractive method for achieving the goals of quality, education, and expediting patient care because of its relative efficiency. As noted by the residents in their survey and by the other participants informally, MDR enhances communication and saves time otherwise spent tracking down the many participants in patient care. This demonstrated success of MDR helps address the call by Zwarenstein and Reeves12 for more evidence of the positive value of such collaboration.
Performance of important processes of care may vary in association with different patient characteristics.7,13,14 However, only small differences in race and payer status were observed for the periods before and after MDR, which were unlikely to account for the significant improvements in quality seen. MDR’s concentration on diagnosis rather than on patients’ personal characteristics, moreover, may serve to negate biases.
A significant increase in study patients’ case mix index (CMI), as determined by case DRG weight, was also observed with MDR. This increase may be partially attributable to the focus of MDR on proper identification of active comorbidities and improvement in documentation to support accurate DRG assignment. Given that the overall hospital CMI went down slightly by 0.01 during the same time period, the increased DRG weight of 0.20 seen in the core measure eligible patients may further support the financial benefit of MDR along with the LOS reduction.
Despite the previous description of successful multidisciplinary teams,15,16 most have been narrow in focus, such as targeting treatment of a single-disease process.17,18 Multidisciplinary teams broadening their scope to the general inpatient medical wards have produced improvements in satisfaction and LOS.19,20 None, however, have demonstrated specific improvements in measurable quality for multiple diagnoses. Although approaching quality through disease management guidelines has shown promise, significant attention is still needed in the implementation of these best practices.21 In addition, tools for practical achievement of top performance in quality measures have not been well demonstrated. Given the multitude of pressures on teaching hospitals, it is not desirable or even feasible to divide resources among each and every new task. Thus, both the unique nature and success of MDR depend on its ability to broadly improve quality core measures while also enhancing both educational and financial objectives.
As reflected by educational meetings and policies set forth by the ACGME, residency programs have endeavored to develop new strategies for teaching the core competencies. However, these methodologies often rely on abstract didactic tools alone or are removed from the daily routine of the resident service.22,23,24). MDR addresses this shortfall by offering an immersion method for effectively teaching both system and evidence-based care with continual data feedback. Added attractions are the grounding received by residents and other hospital staff in core measure practices and the fostering of positive relationships and mutual understanding among them.
Successful programs have been studied for their ability to change clinical practice and promote evidence-based care. Bradley et al.25 demonstrated that hospitals with superior outcomes possess 4 unique characteristics: shared goals for improvement, substantial administrative support, strong physician leadership, and use of credible data feedback. MDR possessed all 4 characteristics, namely, explicitly shared goals of improving core measure performance and enhancing patient flow, visible senior administrative support, physician leadership provided by the chief of medicine, and quantifiable core measure performance outcomes. In particular, the continuing support of senior administrators remains key to sustaining MDR.
Although MDR has been successful with quality, LOS, and education, we did not reach our goal of 100% performance of all pertinent core measures. Some issues were idiosyncratic, such as angiotension receptor blockers not recognized as being acceptable substitutions for ACE inhibitors, which now has been corrected by CMS and JCAHO. Despite significant improvement, measures such as “discharge instructions” for CHF remained suboptimal given the lack of an integrated and automated discharge process. Other core measure failures simply stemmed from missed opportunities or incomplete follow through with orders and documentation.
Although providing a substantial improvement and backbone, MDR is not a complete stand-alone solution for core measure compliance. Current and future direction of MDR involves decision support embedded in a computerized practioner order entry system to create automatic reminders, force documentation of exceptions, and automate diagnosis-driven patient instructions. This advance will close the loop on the recommendations made in MDR and, hence, further its effectiveness.
Our study demonstrates a substantial decrease in LOS for not only the core measure targeted diagnoses but for all medicine DRGs. This gain may be attributable to the advancement of care strategies promoted during MDR, as informally attested to by participants. The utilization of the medical residents as the key effector of such change provides proof of their value not only for quality of care, but for fiscal savings as well. Proponents of postgraduate medical education may be able to use this value to defend their training programs during these times of budgetary constraints.
In conclusion, resident-centered MDR is an effective process that simultaneously improves quality of care while enhancing resident education and is associated with shortened LOS.
References
Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2000.
United States Department of Health and Human Services. Hospital Compare Website. Available at: http://www.hospitalcompare.hhs.gov/. Accessed April 20, 2005.
Weingart SN, Anjala T, Driver J, Aronson M, Sands K. Creating a quality improvement elective for medical house officers. J Gen Intern Med. 2004;19:861–7.
Ogrinc G, Headrick L, Mutha S, Coleman M, O’Donnell J, Miles P. A framework for teaching medical students and residents about practice-based learning and improvement, synthesized from a literature review. Acad Med. 2003;78:748–56.
Lee TH, Pearson SD, Goldman L, et al. Failure of information as an intervention to modify clinical management. Ann Intern Med. 1995;122:434–7.
Cabana MD, Rand CS, Powe Neil R. Why don’t physicians follow clinical practice guidelines?: A framework for improvement. JAMA. 1999;282:1458–65.
Fine JM, Fine MJ, Galusha D, et al. Patient and hospital characteristics associated with recommended processes of care for elderly patients hospitalized with pneumonia: results from the Medicare quality indicator system pneumonia module. Arch Intern Med. 2002;162:827–33.
LaBresh KA, Gliklich R, Peto J, Ellrodt AG. Using “get with the guidelines” to improve cardiovascular secondary prevention. Joint Commission Journal on Quality and Safety. 2003;29:539–50.
Joint Commission of Accreditation of Healthcare Organizations. Comprehensive Review of Hospital Core Measures. Available at: Http://www.Jointcommission.Org/Performancemeasurement/Performancemeasurement/. Accessed October 15, 2005.
Joint Commission of Accreditation of Healthcare Organizations. Specifications manual for national implementation of hospital core measures (v 1.0). Available at: http://www.jointcommission.org/PerformanceMeasurement/PerformanceMeasurement/Historical+NHQM+manuals.htm. Accessed October 30, 2004.
Vittinghoff E. Regression models in biostatistics: linear, logistic, survival, and repeated measures models. New York: Springer;2005.
Zwarenstein M, Reeves S. What’s so great about collaboration? BMJ. 2000;320:1022–3.
Trivedi AH, Zaslavsky AM, Schneider EC, Ayanian JC. Trends in the quality of care and racial disparities in medicare managed care. N Engl J Med. 2005;353:692–700.
Rathore SS, Masoudi FA, Wang Y, et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152:371–8.
Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–44.
McVey LJ, Becker PM, Saltz CC, Feussner, JR, Cohen, HJ. Effect of a geriatric consultation tem on functional status of elderly hospitalized patients. A randomized, controlled clinical trial. Ann Intern Med. 1989;110:79–84.
Tu GS, Meehan TP, Fine JM, et al. Which strategies facilitate improvement in quality of care for elderly hospitalized pneumonia patients? Joint Commission Journal of Quality and Safety. 2004;30:25–35.
Cregin R, Segal-Maurer S, Callahan M, et al. Multidisciplinary approach to improving treatment of community-acquired pneumonia. Am J Health-Syst Pharm. 2002;59:364–8.
Curley C, McEachern JE, Speroff T. A firm trial of interdisciplinary rounds on the inpatient medical wards: an intervention designed using continuous quality improvement. Med Care. 1998;36:S4–12.
Jitapunkul S, Nuchprayoon C, Aksaranugraha S, et al. A controlled clinical trial of multidisciplinary team approach in the general medical wards of Chulalongkorn Hospital. J Med Assoc Thai. 1995;78:618–23.
Faxon DP, Lee HS, Pasternak RC, Shine K, et al. Improving quality of care through disease management: principles and recommendations from the American Heart Association’s Expert Panel on Disease Management. Circulation. 2004;109:2651–4.
Voss JD, Nadkarni MM, Schectman JM. The clinical health economics system simulation (CHESS): a teaching tool for systems and practice-based learning. Acad Med. 2005;80:129–34.
Djuricich AM, Ciccarelli M, Swigonski NL. A continuous quality improvement curriculum for residents: addressing core competency, improving systems. Acad Med. 2004;79:S65–7.
Coleman MT, Nasraty S, Ostapchuk M, et al. Introducing practice based learning and improvement ACGME core competencies into a family medicine residency curriculum. Joint Commission Journal of Quality and Safety. 2003;29:238–47.
Bradley EH, Holmboe ES, Maera JA, et al. A qualitative study of increasing beta-blocker use after myocardial infarction: why do some hospitals succeed? JAMA. 2001;285:260411.
Acknowledgements
We thank the Norwalk Hospital and its MDR attendees for their dedication to and support of this process.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented in part in workshop and oral format at the 27th Society of General Internal Medicine Annual Meeting, May 12–15, 2004, Chicago, IL
Rights and permissions
About this article
Cite this article
O’Mahony, S., Mazur, E., Charney, P. et al. Use of Multidisciplinary Rounds to Simultaneously Improve Quality Outcomes, Enhance Resident Education, and Shorten Length of Stay. J GEN INTERN MED 22, 1073–1079 (2007). https://doi.org/10.1007/s11606-007-0225-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0225-1