Abstract
BACKGROUND
Food insecurity refers to limited or uncertain access to food resulting from inadequate financial resources. There is a clear association between food insecurity and obesity among women, but little is known about the relationship between food insecurity and type 2 diabetes.
OBJECTIVE
To evaluate whether there is an independent association between food insecurity and diabetes.
DESIGN
Cross-sectional analysis of the nationally representative, population-based National Health and Nutrition Examination Survey (1999–2002 waves).
PARTICIPANTS
Four thousand four hundred twenty-three adults >20 years of age with household incomes ≤300% of the federal poverty level.
MEASUREMENTS
We categorized respondents as food secure, mildly food insecure, or severely food insecure using a well-validated food insecurity scale. Diabetes was determined by self-report or a fasting serum glucose ≥126 mg/dl.
RESULTS
Diabetes prevalence in the food secure, mildly food insecure, and severely food insecure categories was 11.7%, 10.0%, and 16.1%. After adjusting for sociodemographic factors and physical activity level, participants with severe food insecurity were more likely to have diabetes than those without food insecurity (adjusted odds ratio [AOR] 2.1, 95% CI 1.1–4.0, p = .02). This association persisted after further adjusting for body mass index (AOR 2.2, 95% CI 1.2–3.9, p = .01).
CONCLUSIONS
Food insecurity may act as a risk factor for diabetes. Among adults with food insecurity, increased consumption of inexpensive food alternatives, which are often calorically dense and nutritionally poor, may play a role in this relationship. Future work should address how primary care clinicians can most effectively assist patients with food insecurity to make healthy dietary changes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Households are food insecure when access to nutritionally adequate and safe foods is limited, uncertain, or dependent on emergency food supplies, scavenging, or stealing.1,2 In the United States, food insecurity is primarily caused by a lack of financial resources. Rates of food insecurity in the United States have been rising since 1999.3,4 In 2004, almost 40 million people (12% of the population) lived in households experiencing food insecurity.3 Eleven million people lived in households experiencing the most severe form of food insecurity, food insecurity with hunger.3
Common household responses to inadequacies in food supplies and food budgets include anxiety about food insufficiency, food budget adjustments, alterations in the types of food served, and reduced food intake.1 With severe food insecurity, individuals miss meals or report hunger because of the inability to afford food.2
Among women in the United States, mild—but not severe—food insecurity is associated with weight gain and obesity. This “obesity–hunger paradox” may be driven by changes in dietary intake in response to food insecurity.5 Cheaper food alternatives, such as refined grains, added sugars, and added fats tend to be nutritionally poor but calorically dense.6 With mild food insecurity, daily caloric needs are maintained, and often exceeded, by these substitutions.5 With severe food insecurity, similar food substitutions may occur, but caloric requirements are less likely to be met.
Obesity and weight gain are strong risk factors for type 2 diabetes; for every kilogram increase in weight, the risk of diabetes increases 4.5%.7 Although there are clear associations among food insecurity, dietary consumption, weight gain, and obesity,8,9 little is known about the relationship between food insecurity and diabetes.
Using a nationally representative sample, this paper explores whether a relationship exists between food insecurity and diabetes and whether such a relationship is independent of obesity. We evaluate risk of diabetes according to level of food insecurity (mild vs. severe) because the food insecurity–obesity relationship differs by level of food insecurity.
METHODS
Sample
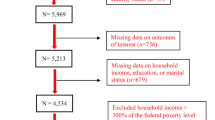
We combined data from the 1999–2000 and 2001–2002 waves of the National Health Examination and Nutrition Examination Survey (NHANES). NHANES is a cross-sectional, nationally representative survey of the non-institutionalized U.S. civilian population administered by the National Center for Health Statistics (NCHS).10 Details of recruitment and study procedures have been previously published.11 We excluded participants under 20 years of age because our outcome of interest was type 2 diabetes and pregnant women to increase the accuracy of the body mass index (BMI) measurement. Because food insecurity in the United States affects predominantly the poor, we restricted the analysis to individuals reporting a household income ≤300% of the federal poverty level (FPL).
Independent Variable
The core food-security module used in NHANES is a well-validated questionnaire developed by the United States Department of Agriculture (USDA) to measure the presence of food insecurity at the household level.1 This standard survey has been used in a number of large, population-based surveys.12–14 It includes 18 items, 10 of which refer to adults in the household and 8 of which refer to children.
We used responses to only those 10 items referring to adults. These questions address anxiety that the household food budget or food supply may be insufficient to meet basic needs, the experience of running out of food without money to obtain more, perceptions that food is inadequate in quality or quantity, adjustments to normal food use (such as substituting fewer and cheaper foods than usual), reduced food intake, the physical sensation of hunger, and weight loss.1
The standard scale for adults is used to create a 4-level categorical variable: 0–2, 3–5, 6–8, or 9–10 affirmative responses.1 Because few NHANES participants reported having the most severe level of food insecurity, NCHS made 2 changes to the standard scale; they collapsed the 2 most severe levels of food insecurity into a single category and created a new category of marginal food insecurity (1–2 affirmative responses). Thus, data are released from NCHS with the following categories: 0, 1–2, 3–5, or 6–10 affirmative responses. Given these constraints, we maintained an adequate sample size for the analysis and simplified presentation of our results by reporting “food security” (0 affirmative responses), “mild food insecurity” (1–5 affirmative responses), and “severe food insecurity” (6–10 affirmative responses).
Dependent Variables
We examined body mass index (BMI), waist circumference, and diabetes as dependent variables. We calculated BMI as measured weight (in kilograms) divided by the square of measured height (in meters). We analyzed BMI as both a continuous and dichotomous variable (BMI < 30 vs BMI ≥ 30 kg/m2, corresponding to the standard definition of obesity15).
Whereas BMI is a good measure of overall adiposity, waist circumference may more accurately reflect visceral adiposity.16 We also evaluated waist circumference as a dependent variable because visceral adiposity may be a stronger predictor of diabetes than overall adiposity.17,18
Our primary outcome of interest was diabetes. Diabetes was defined for most participants by a self-reported diagnosis of diabetes. The specificity of a self-reported diabetes diagnosis is as high as 97%.19–21 There is significant variability in the sensitivity of a self-reported diagnosis of diabetes.20,21 To investigate the sensitivity in our sample, we determined that of the 2,214 patients who had a fasting serum glucose measured, 92 had a value ≥126 mg/dL but did not report having diabetes. For the statistical analysis, we also considered these patients to have diabetes to reduce the misclassification rate.
We did not consider patients to have diabetes if they were likely to have a diagnosis of type 1 diabetes. Using the method of Koopman et al, we excluded from the diabetes group participants who reported a diabetes diagnosis before the age of 30 years and treatment with insulin.22 Ninety-two percent of NHANES participants identified as having type 2 diabetes by this method have a C-peptide level ≥0.50 nmol/L (consistent with a diagnosis of type 2, rather than type 1, diabetes).22
Statistical Analysis
All results, except where indicated, are weighted to represent the US population. We used the complex survey commands in Stata 9.2 (College Station, TX) to obtain weighted estimates, standard errors, and p values which correctly reflect the stratification and clustering of observations induced by the complex survey design. We used either the mobile examination center or interview weights provided by the NCHS, as appropriate; both reflect differential sampling probabilities and non-response.11 We compared differences in baseline characteristics using the design-based F statistic (equivalent to a chi-squared or t test adjusted for the complex survey design). We used linear or logistic regression, as appropriate, to assess the association of food insecurity with BMI, waist circumference, obesity, and diabetes. We present results stratified by gender for the BMI, waist circumference, and obesity outcomes because of gender-related differences in observed associations.
Our covariates included sociodemographic factors known to be associated with diabetes: age, race/ethnicity (self-reported non-Hispanic White, non-Hispanic Black, Hispanic, or other/multiple), parity (women only; 0, 1–2, 3–5, or 6+ live births), household income, family history of diabetes in a sibling or parent, educational attainment (less than high school, high school degree, or more than high school degree), and level of physical activity. We defined household income using a 6-level income/poverty ratio (0–50% of the federal poverty level, 50.1–100%, 100.1–130%, 130.1–200%, or 200.1–300%). We used as covariates 3 questions assessing occupational, vigorous leisure-time, and moderate leisure-time physical activity. The occupational leisure-time question asked people to describe their “usual daily activities” as sitting and not walking around very much, standing a lot but not having to carry or lift things very often, having to lift light loads or climb stairs or hills often, or having to do heavy work or carry heavy loads. The leisure-time physical activity questions asked participants whether they had done vigorous (causing heavy sweating or large increases in breathing or heart rate) or moderate (causing light sweating or a slight to moderate increase in breathing or heart rate) physical activity during leisure-time exercise, sports, or physically active hobbies during the last 30 days.
NHANES includes a detailed 24-hour dietary recall. Information from the recall is used to estimate total nutrient intake using the University of Texas Food Intake Analysis System and the USDA Food and Nutrition Database for Dietary Studies.23 We compared differences in estimated total daily caloric and carbohydrate intake using a design-based F statistic. In a sensitivity analysis, we included daily caloric and carbohydrate intake in the full model evaluating the association between food insecurity and diabetes to determine whether dietary intake mediated observed relationships.
To maintain a consistent sample throughout the analysis, we included only individuals for whom we had complete information about household food insecurity, BMI, waist circumference, and diagnosis of diabetes. We also performed a sensitivity analysis evaluating the association between food insecurity and diabetes among all participants for whom we had information about these 2 variables (n = 2,649 females and 2,497 males), without excluding individuals lacking a BMI or waist circumference measurement. Results were similar to our primary analysis.
RESULTS
NHANES 1999–2000 and 2001–2002 included 2,690 nonpregnant women and 2,532 men aged 20 years or older with a household income ≤300% of the FPL. We excluded those participants for whom we were unable to determine their level of food insecurity (n =72), BMI (n = 640), waist circumference (n = 641), or diabetes diagnosis (n = 4). These exclusions left a total sample size of 4,423 participants, of whom 413 in the food secure category had diabetes, 134 in the mild food insecurity category had diabetes, and 47 in the severe food insecurity category had diabetes. Overall, food insecure individuals were younger, more likely to be from a racial or ethnic minority group, were poorer, and had achieved less educational attainment than food secure individuals (Table 1).
After adjusting for age, race/ethnicity, parity, income, educational attainment, and physical activity, women with mild food insecurity had higher obesity rates, mean BMI, and mean waist circumference than either food secure or severely food insecure women, whose values were similar to one another (Table 2). For an average-height woman in the United States (162 cm),24 the greater BMI among mildly food insecure women compared with food secure women (Δ = 2.0 kg/m2) is equivalent to a weight difference of 5.2 kg. We did not observe a relationship between food insecurity and obesity among men. Unadjusted results were similar to adjusted results for both women and men.
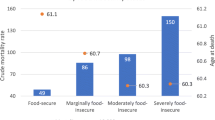
The estimated prevalence of diabetes in the food secure, mildly food insecure, and severely food insecure categories was 11.7%, 10.0%, and 16.1%. Compared to adults who were food secure, the odds of diabetes was 1.2 (95% CI 0.8–1.8) for those with mild food insecurity and 2.1 (95% CI 1.1–4.0) for those with severe food security after adjusting for gender, age, race/ethnicity, parity, income, family history of diabetes, education, and physical activity (Table 3). This relationship persisted after further adjusting for BMI.
Adjusting for waist circumference instead of BMI did not alter the observed relationship between food insecurity and diabetes. Compared to the food secure category, the odds of diabetes after adjusting for all other potential confounders including waist circumference was 1.0 (95% CI 0.7–1.5, p = .8) in the mildly food insecure category and 2.0 (95% CI 1.1–3.6, p = .03) in the severely food insecure category.
We calculated mean daily caloric and carbohydrate intake to determine whether differences in diet might mediate the observed relationship between food insecurity and diabetes. Among women, the estimated mean daily caloric intake was 1,780 kcal/day in the food secure category, 1,822 kcal/day in the mild food insecurity category (p = .3 compared to food secure women), and 1,876 kcal/day in the severe food insecurity category (p = .2 compared to food secure women). Among men, the estimated mean daily caloric intake was 2,549 kcal/day in the food secure category, 2,759 in the mild food insecure category (p = .09 compared to food secure men), and 2,543 in the severe food insecure category (p = .9 compared to food secure men). Among women, estimated mean carbohydrate intake was 233 g/day in the food secure category, 237 g/day in the mild food insecurity category (p = .4 compared with food secure women), and 242 g/day in the severe food insecurity category (p = .4 compared with food secure women). Among men, mean carbohydrate intake was 314 g/day in the food secure category, 339 g/day in the mild food insecure category (p = .09 compared with food secure men), and 311 g/day in the severe food insecure category (p = .8 compared with food insecure men).
After adding daily caloric and carbohydrate intake to the models including gender, age, race/ethnicity, parity, income, family history of diabetes, educational attainment, level of physical activity and BMI, mild food insecurity was associated with a 1.1 (95% CI 0.7–1.6, p = .7) higher odds of diabetes and severe food insecurity was associated with a 2.2 (95% CI 1.2–4.2, p = .01) higher odds of diabetes.
CONCLUSIONS
Of the almost 40 million people in the United States living in food insecure households, almost 25 million of them are adults over the age of 18 years.3,4 This study in a nationally representative sample of Americans finds that food insecurity is independently associated with diabetes. Although obesity among women is also associated with mild food insecurity, the increased obesity rates account for only 20% of the increased odds of diabetes among these women.
Prior evidence suggests that food insecurity may be associated with general health status and chronic disease, including major depression, diabetes, and hypertension.25,26 This is the first study, to our knowledge, to find an association between food insecurity and diabetes in a nationally representative sample and the first to suggest that the association between food insecurity and diabetes is independent of BMI.
Individuals living in food insecure households may substitute preferred foods with cheaper alternatives.1,5,6,27,28 These cheaper alternatives tend to be nutritionally poor but calorically dense, allowing individuals to maintain—and potentially exceed—their caloric requirements.6 For example, in other studies food insecurity has been associated with reduced consumption of fruits and vegetables and an increased percentage of caloric intake from fat (including saturated fats) and refined carbohydrates.29–31 These diets have been associated with the development of diabetes.8,32–34
The association between food insecurity and diabetes may also stem from the cyclic nature of food insecurity, either because of monthly paychecks, monthly Food Stamp Program assistance, or periodic, unforeseen competing needs.2,35,36 Individuals with episodic underconsumption may overcompensate during times of relative food adequacy resulting in binge-fast cycles.37,38 This pattern of dietary intake has also been linked to insulin resistance.39–41
Our evidence suggests that the relationship between food insecurity and diabetes differs from the relationship between food insecurity and obesity. From an evolutionary perspective, survival advantage may have been bestowed on those who could conserve muscle protein during times of famine, rather than destroying it to produce usable energy for the brain. Peripheral insulin resistance helps achieve this evolutionary advantage, but may ultimately result in the failure of insulin-producing beta-cells and diabetes.42 Repeated episodes of inadequate access to food could exacerbate this tendency toward insulin resistance.
Chronic stress might also mediate the relationship between food insecurity and diabetes. Individuals in food insecure households report high levels of anxiety and worry.43,44 Stress has been associated in previous studies with adiposity, particularly the visceral adiposity, which may be a stronger risk factor for diabetes than overall adiposity.45,46 However, visceral adiposity, as measured by waist circumference, did not appear in this study to be a strong mediator of the food insecurity–diabetes association.
Our data are limited by the sensitivity of a self-reported diagnosis of diabetes for some NHANES participants. Including elevated fasting plasma glucose as a criterion for diabetes diagnosis helped address this problem, but only a subset of our sample had a fasting glucose measured. Because access to medical care is more limited among those who are food insecure,47 this bias conservatively influences our results.
Several other methodologic issues also limit our results, but in the first 2 cases the expected bias is likely conservative. First, we were unable to use standard cut points for categorizing food insecurity because of the format in which data were released from the NCHS. The “mild food insecurity” category used in this paper therefore includes a population with less severe difficulties accessing food than the USDA’s standard “food insecurity without hunger” category. Second, food insecurity is a household measure, whereas diabetes is an individual-level outcome. Preliminary evidence suggests that when there is household food insecurity at a level severe enough to result in hunger for any household adults, most, if not all, of the adults in the household are usually affected.1 We are unaware of any validated individual-level measures of food insecurity. Third, differential nonparticipation in the study population may have biased the observed association.
Finally, our data are cross-sectional, so we cannot determine whether food insecurity is a risk factor for diabetes or if diabetes is a risk factor for food insecurity. Diabetes might heighten individuals’ awareness of inadequate access to healthy foods. Alternatively, individuals with diabetes may preferentially allocate limited resources toward medical expenses, resulting in increased levels of food insecurity.27
Patients with limited financial resources may struggle to obtain nutritious foods, both because of their high cost6 and because nutritious foods are less often stocked in stores located in low-income neighborhoods.48,49 Clinicians offering dietary counseling must be cognizant of the additional barriers food insecurity poses to healthy dietary intake. Future research should address the most effective strategies for counseling patients with limited financial resources to make healthy dietary changes. For example, reducing portion size may be a more practical dietary strategy than many food substitutions. Further evaluation is also necessary to determine whether policies that decrease food insecurity, such as expanding access to nutritional assistance programs (e.g., the Food Stamp Program), also decrease rates of diabetes. Diabetes prevention efforts in underserved communities should consider the impact of food insecurity on dietary choices and diabetes risk.
References
Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to Measuring Household Food Security, Revised 2000. Alexandria, VA; U.S. Department of Agriculture, Food and Nutrition Service; 2000.
Wunderlich GS, Norwood JL, eds. Food Insecurity and Hunger in the United States: An Assessment of the Measure. Washington, DC: The National Academies Press; 2006.
Nord M, Andrews M, Carlson S. Household Food Security in the United States, 2004. Economic Research Report 11. Alexandria, VA: United States Department of Agriculture; 2005.
Hall B. Hunger and food insecurity increase for 5th straight year. Center on Hunger and Poverty, October 2005.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16.
Drewnowski A, Darmon N. The economics of obesity: dietary energy density and energy cost. Am J Clin Nutr. 2005;82:265S–73S.
Ford ES, Williamson DF, Liu S. Weight change and diabetes incidence: findings from a national cohort of US adults. Am J Epidemiol. 1997;146:214–22.
Franz MJ, Bantle JP, Beebe CA, et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003;26(Suppl 1):S51–61.
Ludwig DS. Dietary glycemic index and obesity. J Nutr. 2000;130:280S–3S.
Centers for Disease Control and Prevention (CDC). National Health and Nutrition Examination Survey. Hyattsville, MD: National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services; 2005.
Centers for Disease Control and Prevention (CDC). Analytic and reporting guidelines: the National Health and Nutrition Examination Survey (NHANES). Hyattsville, MD: National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services; 2005.
Bureau of the Census for the Bureau of Labor Statistics. Current Population Survey. Washington DC.
Centers for Disease Control and Prevention (CDC). National Health Interview Survey. Hyattsville, MD: National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services; 2005.
U.S. Census Bureau. Survey of Income and Program Participation. Washington DC.
National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. NIH Publ 98(4083), September 1998.
Valsamakis G, Chetty R, Anwar A, Banerjee AK, Barnett A, Kumar S. Association of simple anthropometric measures of obesity with visceral fat and the metabolic syndrome in male Caucasian and Indo-Asian subjects. Diabet Med. 2004;21:1339–45.
Albu JB, Murphy L, Frager DH, Johnson JA, Pi-Sunyer FX. Visceral fat and race-dependent health risks in obese nondiabetic premenopausal women. Diabetes. 1997;46:456–62.
Despres JP, Lemieux S, Lamarche B, et al. The insulin resistance-dyslipidemic syndrome: contribution of visceral obesity and therapeutic implications. Int J Obes Relat Metab Disord. 1995;19(Suppl 1):S76–86.
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096.
Kehoe R, Wu SY, Leske MC, Chylack LT, Jr. Comparing self-reported and physician-reported medical history. Am J Epidemiol. 1994;139:813–8.
Midthjell K, Holmen J, Bjorndal A, Lund-Larsen G. Is questionnaire information valid in the study of a chronic disease such as diabetes? the Nord-Trondelag diabetes study. J Epidemiol Community Health. 1992;46:537–42.
Koopman RJ, Mainous AG, 3rd, Diaz VA, Geesey ME. Changes in age at diagnosis of type 2 diabetes mellitus in the United States, 1988 to 2000. Ann Fam Med. 2005;3:60–3.
Centers for Disease Control and Prevention (CDC). Documentation for the dietary interview—total nutrient intakes file. National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services; 2004.
Centers for Disease Control and Prevention (CDC). Anthropometric reference data, United States, 1988–1994. National Center for Health Statistics (NCHS), U.S. Department of Health and Human Services. Available at http://www.cdc.gov/nchs/about/major/nhanes/Anthropometric%20Measures.htm. Accessed July 6, 2005.
Klesges LM, Pahor M, Shorr RI, Wan JY, Williamson JD, Guralnik JM. Financial difficulty in acquiring food among elderly disabled women: results from the women’s Health and Aging Study. Am J Public Health. 2001;91:68–75.
Vozoris NT, Tarasuk VS. Household food insufficiency is associated with poorer health. J Nutr. 2003;133:120–6.
Wolfe WS, Frongillo EA, Valois P. Understanding the experience of food insecurity by elders suggests ways to improve its measurement. J Nutr. 2003;133:2762–9.
Drewnowski A, Darmon N, Briend A. Replacing fats and sweets with vegetables and fruits—a question of cost. Am J Public Health. 2004;94:1555–9.
Lee JS, Frongillo EA, Jr. Nutritional and health consequences are associated with food insecurity among U.S. elderly persons. J Nutr. 2001;131:1503–9.
Tarasuk VS. Household food insecurity with hunger is associated with women’s food intakes, health and household circumstances. J Nutr. 2001;131:2670–6.
Kendall A, Olson CM, Frongillo EA, Jr. Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc. 1996;96:1019–24.
Ford ES, Mokdad AH. Fruit and vegetable consumption and diabetes mellitus incidence among U.S. adults. Prev Med. 2001;32:33–9.
Gross LS, Li L, Ford ES, Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am J Clin Nutr. 2004;79:774–9.
Montonen J, Jarvinen R, Heliovaara M, Reunanen A, Aromaa A, Knekt P. Food consumption and the incidence of type 2 diabetes mellitus. Eur J Clin Nutr. 2005;59:441–8.
Thompson FE, Taren DL, Andersen E, et al. Within month variability in use of soup kitchens in New York state. Am J Public Health. 1988;78:1298–301.
Wilde PE, Ranney CK. The monthly food stamp cycle: shopping frequency and food stamp decisions in an endogenous switching regression framework. Am J Agric Econ. 2000;82:200–13.
Urbszat D, Herman CP, Polivy J. Eat, drink, and be merry, for tomorrow we diet: effects of anticipated deprivation on food intake in restrained and unrestrained eaters. J Abnorm Psychology. 2002;111:396–401.
Polivy J. Psychological consequences of food restriction. J Am Diet Assoc. 1996;96:589–92; Quiz 93–94.
Duska F, Andel M, Kubena A, Macdonald IA. Effects of acute starvation on insulin resistance in obese patients with and without type 2 diabetes mellitus. Clin Nutr. 2005;24:1056–64.
Mansell PI, Macdonald IA. The effect of starvation on insulin-induced glucose disposal and thermogenesis in humans. Metabolism. 1990;39:502–10.
Newman WP, Brodows RG. Insulin action during acute starvation: evidence for selective insulin resistance in normal man. Metabolism. 1983;32:590–6.
Reaven GM. Hypothesis: muscle insulin resistance is the (“not-so”) thrifty genotype. Diabetologia. 1998;41:482–4.
Hamelin AM, Habicht JP, Beaudry M. Food insecurity: consequences for the household and broader social implications. J Nutr. 1999;129:525S–8S.
Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Québec: food and feelings. Soc Sci Med. 2002;54:119–32.
Epel ES, McEwen B, Seeman T, et al. Stress and body shape: stress-induced cortisol secretion is consistently greater among women with central fat. Psychosom Med. 2000;62:623–32.
Gluck ME, Geliebter A, Lorence M. Cortisol stress response is positively correlated with central obesity in obese women with binge eating disorder (BED) before and after cognitive-behavioral treatment. Ann N Y Acad Sci. 2004;1032:202–7.
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21:71–7.
Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health. 2004;94:1549–54.
Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–9.
Acknowledgments
The authors would like to express their gratitude to Dr. Umesh Masharani for his helpful comments on the manuscript. Dr. Seligman was funded by a DHHS-HRSA Primary Care Faculty Development Grant 5 D14HP00178-03-00. Dr. Kushel’s work was supported by the Agency for Healthcare Research and Quality grant K08 HS011415-03. The funders did not participate in any part of the study. Portions of this work were presented in abstract form at the 2006 Society of General Medicine Meeting.
Conflicts of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seligman, H.K., Bindman, A.B., Vittinghoff, E. et al. Food Insecurity is Associated with Diabetes Mellitus: Results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J GEN INTERN MED 22, 1018–1023 (2007). https://doi.org/10.1007/s11606-007-0192-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0192-6