Abstract
OBJECTIVE
The study explored the perceptions of Australian immigrants about their interactions with doctors regarding the diagnosis, treatment, and management of type 2 diabetes mellitus.
RESEARCH DESIGN AND METHODS
In-depth interviews were conducted with 30 men and women from Greek, Indian, Chinese, and Pacific Island backgrounds living in Melbourne, Australia, to elicit their perceptions of the management of diabetes and its impact. Participants were recruited through a convenience sample of general practitioners and community organizations providing support to people living with diabetes. Topics discussed included initial reaction to diagnosis, patient—health care provider communication, and the influence of message framing on the perception of the quality of the doctor–patient relationship. Transcripts were coded and analyzed by both authors.
RESULTS
Numerous issues facilitate or inhibit constructive and positive relationships between doctors and patients with type 2 diabetes. Patients reported difficulty in absorbing all the information provided to them at early consultations, and experienced difficulty comprehending the practical aspects of management. Styles of communication and discourses of normalization and catastrophe influenced participants’ responses.
CONCLUSION
Doctors face a complex task in encouraging behavioral change and adherence and establishing and maintaining a supportive relationship with patients. The timing and technical complexity of communication about diabetes, its management, and the prevention of complications require further attention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
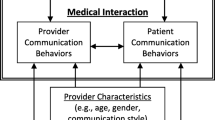
Ethnicity and minority status impact perceptions of illness and may require special consideration in developing appropri ate services and effective clinician responses.1–4 While personal, social, and cultural factors are particularly important where multifaceted lifestyle adjustments are required, as in managing type 2 diabetes mellitus, doctor–patient communication is central to supporting self-management.5–7 In Australia, prevalence estimates of diabetes draw attention to marked variations by ethnicity, but little is known about minority patients with diabetes.8,9 Migration and resettlement patterns differ between countries and communities, making generalizations problematic and pointing to the need for further inquiry into ethnicity and other background factors. Clinicians must convince patients of the value of controlling blood glucose and adhering to other aspects of self-care, medications, diet, and cardiovascular health maintenance. For most people, this is a complex instruction set that may require major changes in ideas and practices related to body image, diet, and exercise.10 The challenges to sustain behavioral change are often related to patient education, but while insufficient knowledge about diabetes and its complications can contribute to poor adherence,11 patients may reject or ignore advice because of differing beliefs about disease control, competing life priorities, and circumstances.12,16 In emphasizing the importance of control, doctors may understate the seriousness of the disease to avoid alarm, potentially creating confusion and lowering patient motivation for self-management.17,18 Physicians alternatively may use strategies inducing fear to gain adherence to advice.19,20 Patient care may be enhanced where patients and physicians share decision-making.6,7 This is often compromised by physician’s lack of time18,19,21 and patients’ views about appropriate interactions.22 For some, direct negotiation with or challenges to the physicians’ view may be considered inappropriate.23,24
We describe how patients in an Australian setting are told of diabetes and offered advice about its management in primary care settings. We describe their reactions to this information, their ideas of the quality of their relationship with their doctor, and their comprehension of the management plan. We considered how reports of doctors’ comments about the condition inform patients’ interpretations of advice and illustrate the range of views about the nature of the disease and their communication with doctors.
RESEARCH DESIGN AND METHODS
Study Participants
A qualitative study was conducted in Melbourne, Australia, with 30 participants from backgrounds with a higher-than-average incidence of type 2 diabetes. Recruitment took place over six consecutive months through collaboration with general practitioners (GPs) in suburbs with substantial numbers of patients of Chinese, Indian, and South and Pacific Island (Tongan, Samoan, and NZ Maori) background, and through collaboration with an ethnic community organization for participants born in Greece. In total, 16 women and 16 men were recruited (Table 1). Participants were included if they were older than 18 years (mean 66.43), diagnosed with type 2 diabetes at least 5 years earlier, taking oral medication or used insulin, and had no complications. All participants were first-generation immigrants and only two had lived in Australia for less than 10 years (mean 25.57). The majority had come to Australia for economic reasons (46.7%) or to be reunited with their family (33%).
Data Collection
An interview guide for in-depth interviews was developed by the authors to gather information on reaction to diagnosis and potential complications, doctor–patient communication, and other factors believed to influence diabetes management. Interviews commenced with an invitation to the participant to describe his or her experience, with the guide used where necessary to ensure that all topics were covered. Greek participants were interviewed at a Greek community center; most others elected to be interviewed at their homes. Interviews were conducted by the first author in English or with interpreting assistance (all Greek, three Chinese, three Samoan, and two Tongan participants); many who used an interpreter also communicated in English. Having the researcher conduct the interviews is conventional and preferable in qualitative research because of the skills required to encourage open discussion. Interviews lasted for 1 to 2 h and were audio-taped, transcribed, and translated where necessary. Ethics approval for the study was granted by the Human Ethics and Research Committee, The University of Melbourne.
Data Analysis
Data were analyzed using Mays and Pope’s framework of qualitative research and analysis in health care25,26, which emphasizes common themes. Both authors read the transcripts and coded them independently to identify preliminary themes and categories from individual narratives. We then discussed the themes and together made decisions about dominant and emergent categories. This process was repeated, with new categories added as appropriate. Coding was subsequently reviewed, and while there were no discrepancies, we noted and discussed differences in priority and emphasis to reach consensus. Because this was a small sample with primarily qualitative data, statistical analysis was not appropriate; thus, we report our findings by summarizing and discussing the predominant themes. Quotations are attributed by sex and ethnicity.
RESULTS
Communication of Diagnosis
Participants recalled their distress when first advised of their diagnosis, reflecting their perceived vulnerability as they embarked on life as a “diabetic patient.” Individual reactions to diagnosis, regardless of gender or cultural group, tended to be one of two extremes. One was shock and disbelief, often leading to a search for an alternative opinion and delay in advice:
I didn’t even believe it. So I went to see the other doctor and got the same [result] there. And then she [GP] was questioning me why I wanted it [a second opinion]. And I told her I didn’t believe what I was being told, but I ended up with same thing [diagnosis of diabetes]. I went home and didn’t do a thing... Then I went back and asked for treatment (M, Samoan).
Other participants, familiar with diabetes because of family history, were better able to accept diagnosis; for some, diagnosis validated feelings of poor health. Others simply elected to “get on with life.”
Doctors’ communication of the diagnosis, management, and prognosis of diabetes varied considerably. Some participants reported that they received only general information; they were admonished to “be careful,” “take care,” “watch what they ate,” and “lose weight,” without explicit advice or monitoring. These participants stated that they were referred to publications, a diabetes educator, or a support group for further information if desired. Others received complex explanations that they found difficult to comprehend: the role of the pancreas in the production of insulin and genetic and other factors implicated in the disease: “He (the doctor) told me a lot of things. I don’t think anybody understands at the beginning what the doctor is saying. Slowly you learn and other things come to you” (F, Greek).
In general, doctors used one of two strategies to impart information about self-management, which we termed “normalizing” and “catastrophizing.” In normalizing discourse, doctors often emphasized the commonness of the disease—“You have diabetes. What’s the difference? It’s not only you, it’s thousands” (M, Greek)—and downplayed the risks of complications by emphasizing its manageability through adherence to medication and changes in diet and level of activity. In this context, participants tended to perceive the condition as minor, requiring few behavioral adjustments: “I haven’t got really major diabetes, I just have to be careful about eating cakes and sweet things” (F, Greek). While advised to take medication, avoid sugar and fats, be “careful” of their diet, and lose weight, these participant were advised not to worry: “The doctor said, ‘It’s up to you now. If you control your diet, you won’t need the medicine. You like to eat but you will have to go on to insulin.’ He told me that it is not really a disease. It is something that comes from when you eat. You need to control it. It’s up to you” (M, Greek). Some interpreted this approach to imply that they had only a “little bit of diabetes” or were “on the level in between good and bad.” Diabetes was seen as of little significance, its complications reframed as normal for any older person: “After you get to 45 (years of age), it’s very, very rare if people haven’t got blood pressure or cholesterol or other disease, you know” (F, Greek). Normalizing discourse also assisted acceptance: “It’s quite common hearing about people having diabetes. It’s like people having a cold and that now. I think that quite a lot of Australians are having diabetes” (M, Chinese).
“Catastrophizing” in contrast emphasized the risk of severe complications and the imperative of strict adherence to behavioral rules. Participants were advised of the risks of cardiovascular problems, problems with vision, peripheral neuropathy, ongoing infections, and renal disease impacting on quality of life and resulting in early death. Some participants were critical of this approach, which they referred to as “scare tactics,” to motivate them to comply with prescriptions, and argued that this contributed to stress, anxiety, and confusion: “My anxiety is [because of] the constant scaring by my doctors (laughs) of the diabetes...that, uh, you’re going to lose a leg, you’re going to lose your eyesight” (M, Chinese).
Doctor–Patient Relationships
The ability to establish and sustain preventive practices depends, in part, on the consulting style of the health provider. Participants appreciated extended consultation times and the readiness of the GP to understand their personal circumstances and to empathize with and support them. What anyone needed was “a sympathetic medical practitioner. Like mine, he gives you all the time you want” (M, Chinese). Partcipants regarded a continuing relationship with a doctor as important for continuity of care and support “because it’s really important that all my records and things are kept with the one doctor that I know” (F, Tongan). Doctors’ familiarity with patients’ life circumstances, reflecting prior contact, influenced their ability to manage (or not) their diabetes. Where participants were confident in their doctor, the relationship was sustained even if they were critical of “scare tactics” or questioned the appropriateness of medical advice. This was often represented as a partnership: “I think the biggest problem we had at that time was my blood pressure, so we were working on that. But it was just medication mainly and diet that we were working on” (M, NZ Maori) (our emphasis).
In general, the relationship between doctors and participants was hierarchical. Patients sought approval from their doctors when they were compliant and feared reproach when they deviated from advice. Some intermittently ceased to present to a specialist or GP if they thought that their advice would be discouraging or if they had not adhered to advice consistently, and attempted to manage their condition alone. Participants also experienced difficulties in establishing a relationship with their GPs because of limited consultation time. Consultations were often restricted to clinical assessment and brief discussions about their physical health, without opportunities to discuss other questions related to the social and personal impact of diabetes: “He will explain it to you, but he hasn’t got enough time to explain everything. No doctor has time” (F, Greek). Some GPs and specialists were criticized as being particularly distant and alienating, giving little time and attention to the relationship.
Participants who had numerous medical procedures were also critical about doctors’ recommendations to increase medication or to have more regular check-ups, which they saw as unnecessary. Several participants argued the need to take control of their own bodies and to manage their illness, not in conformity with their doctor’s view about self-management but because they questioned medical competence and authority. Although they reiterated what doctors told them, they also challenged medical expertise and expert knowledge, emphasizing their personal experience of living with diabetes and self-management:
Yes, you know, for myself, I am the only person that knows my body. The issue is that I don’t want to take them [medication]. I might take them Monday, Tuesday, Wednesday or Thursday, Friday. OK? Yes. Maybe then I will give myself Saturday, Sunday and Monday off. You’ve got to give your body, my body anyway, a rest from, you know, taking [medication]—and so far, so good. It’s work; it works, you know. So I just keep on doing that, you know. My sugar level doesn’t go up too high. (M, NZ Maori).
DISCUSSION
Doctor–patient relationships and the communication processes that influence patient attitudes and behavior are important factors in diabetes management and require further research. Strict control of blood glucose and related risk factors can reduce the incidence and progression of complications,27,28 but the effectiveness of interventions in regular clinical settings is hampered by many factors, including the complexity of lifestyle changes. The physician–patient relationship is central in translating efficacy into effectiveness.15,16 Prior exposure appears to influence readiness to accept the diagnosis and its implications. However, dialogues between doctors and their patients often focused on the control of illness (e.g., discussions of blood glucose levels) and long-term complications, excluding other relevant topics.
Physicians were reported to have adopted two key strategies to discuss diabetes. One is normalization, which tends to minimize the severity of the illness to reduce patients’ distress, but which may be counterproductive in establishing and sustaining self-management. The minimization of diabetes is not uncommon among patients,19,29 and Hiss17 has also raised the concern that physicians themselves may foster such views in their patients.
Other doctors were reported to have used a catastrophizing approach, emphasizing diabetes as a significant chronic illness with the potential for multiple and widespread health problems and reduced quality of life. Participants tended to recognize catastrophizing as a means to motivate them to adhere to advice. Although some dismissed these as “scare tactics,” the approach resulted in considerable patient anxiety and contributed to negativity towards the physician.
The level and detail of information reported to have been provided by doctors in our sample varied considerably, raising questions of the need to standardize diabetes care in (Australian) primary care settings. Efforts by doctors to provide extensive information were often met with incomprehension because of the timing of the information or its complexity, particularly for low-health-literacy patients from different language backgrounds.30 Participants also reported that they lacked information about self-management because physicians provided only limited advice and were not involved in supporting required behavior change. Several factors may be related to this, including lack of physician knowledge and skill in areas such as nutritional management and counselling,31,32 lack of knowledge of diabetes or endocrinology,33 or lack of time available for consultations.21,31 Participants considered a lack of consultation time as reducing their opportunity to learn about their condition and precluded the discussion of other important issues. In Australia, small practices often struggle to remain viable by turning to numerous brief consultations, which are more lucrative than fewer, longer consultations, and this may act as a disincentive for complex disease management (see also31).
For most participants, relationships were hierarchical and involved seeking approval and avoiding reproach from their doctors for their successes and failures in diabetes management. Why hierarchy was a dominant pattern in our sample is not clear, and is worthy of further inquiry. Ethnic or racial matching between doctor and patient appeared to foster participatory patterns of communication (also22,24,34), but a participatory style is not necessarily preferred,23 and age, gender, and cultural backgrounds of participants may all have influenced their perceptions of the doctor–patient relationship. The most evident impact of hierarchy in our sample was participant avoidance of medical consultations when the adequacy of the patient’s diabetes management was contestable. In addition, some participants, while conforming to their doctors’ message to take responsibility for their own care, resisted medical authority and modified their treatment in accordance with their own views of what was best. Forms of nonadherence included reducing medication dosages or frequency of medication.
CONCLUSION
The present study was a small qualitative study that, because of the diversity of participants’ backgrounds, precluded close analysis of the role of culture in the experience of diabetes. Our concern was to identify common emergent themes among Australian immigrant participants across different cultural groups. Given the small sample, we have not attempted to explore how cultural context moderates the processes of the therapeutic relationship and communication issues. The comprehensiveness and generalization of findings are further limited because of the cross-sectional nature of the study: we were unable to track the evolution of relationships over time. There is a clear need for further research in this domain.
Despite limitations, we are impressed by the uniformity of emergent issues, patient reactions, and patterns of communication between our sample and other studies. The most obvious common factors are the nature of medical culture and models of care, which do not necessarily best meet the task of managing chronic diseases and preventive care.18,35 In diabetes management, multiple factors need to be addressed clinically to prevent complications, including how the disease impacts on the patient’s personal, emotional, and social lives; the personal meanings and consequent actions developed around the disease; the perceived level of threat to life and lifestyle; and coincidental adversities and limitations faced by patients. While high value is placed on the ability to achieve lifestyle changes to maintain optimal levels of blood glucose, this is not easy even for well-informed patients because of the complexity of self-management, recurrent demotivation from blood glucose variations regardless of adherence,36,37 and the onset or progression of complications. The model of prevention in diabetes management requires substantial expertise, a wide variety of skills, and long-term commitment in health care providers.18,21,31 Doctor–patient communication and therapeutic relationships are central in supporting patients faced with the threat of complications. It is of critical importance to continue to research this relationship to reduce the gap between efficacy and effectiveness in diabetes outcomes.
References
Alcozer F. Secondary analysis of perceptions and meanings of type 2 diabetes among Mexican American women. Diabetes Educ. 2000;26:785–95.
Arcury TA, Skelly AH, Gesler WM, Dougherty MC. Diabetes meanings among those without diabetes: explanatory models of immigrant Latinos in rural North Carolina. Soc Sci Med. 2004;59:2183–93.
Chun KM, Chesla CA. Cultural issues in disease management for Chinese Americans with type 2 diabetes. Psychol Health. 2004;19:767–85.
Hjelm KG, Bard K, Nyberg P, Apelqvist J. Beliefs about health and diabetes in men of different ethnic origin. J Adv Nurs. 2005;50:47–59.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97.
Delamater AM. Improving patient adherence. Clin Diabetes. 2006;24: 71–7.
Hampson SE, McKay GH, Glasgow RE. Patient–physician interactions in diabetes management:2 consistencies and variation in the structure and content of two consultations. Patient Educ Couns. 1996; 29:49–58.
Australian Institute of Health and Welfare. Diabetes: Australian Facts. Canberra: National Centre for Monitoring Diabetes, Australian Institute of Health and Welfare; 2002.
Holdenson Z, Ctanzariti L, Phillips G, Waters A. A Picture of diabetes in overseas-born Australians. Bulletin No 9. AIHW Cat. No. AUS 38. Canberra: Australian Institute of Health and Welfare; 2003.
Maldonato A, Bloke D, Ceci M, Fraticelli E, Fallucca F. Diabetes mellitus: lessons from patient education. Patient Educ Couns. 1995;26: 57–66.
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 2001;24:1069–78.
Parsons J, Wilson D, Scardigno A. The Impact of Diabetes in South Australia 2000. Adelaide: South Australian Department of Human Services Epidemiology Branch; 2000.
Walsh ME, Katz MA, Sechrest L. Unpacking cultural factors in adaptation to type 2 diabetes mellitus. Med Care. 2002;40:129–39 (Suppl).
Broom D, Whittaker A. Controlling diabetes, controlling diabetics: moral language in the management of diabetes type 2. Soc Sci Med. 2004;58:2371–82.
Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18:893–902.
Huang ES, Gorawara-Bhat R, Chin MH. Self-reported goals of older patients with type 2 diabetes mellitus. J Am Geriatr Soc. 2005;53: 306–11.
Hiss R. Barriers to care in Non-Insulin-dependent diabetes mellitus: the Michigan experience. Ann Intern Med. 1996;124(1S-II):146–8 (Suppl).
Larme AC, Pugh JA. Attitudes of primary care providers towards diabetes: barriers to guideline implementation. Diabetes Care. 1998;21:1391–6.
Wens J, Vermeire E, Van Royen P, Sabbe B, Denekens J. GPs perspectives of type 2 diabetes patients’ adherence to treatment: a qualitative analysis of barriers and solutions. BMC Fam Pract 2005; 6 (http://www.biomedcentral.com).
Helme DW, Harrington NG. Patient accounts for noncompliance with diabetes self-care regimens and physician compliance-gaining response. Patient Educ Couns. 2004;55:281–92.
Grant RW, Pirraglia PA, Meigs JB, Singer DE. Trends in complexity of diabetes care in the United States from 1991 to 2000. Arch Intern Med. 2004;164:1134–9.
Ashton CM, Haidet P, Paternitti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences or poor communication? J Gen Intern Med. 2003;18:146–52.
McKinstry B. Do patients wish to be involved in decision making in the consultation? A cross sectional survey with video vignettes. Br Med J. 2006;321:867–71.
Perloff RM, Bonder B, Ray GB, Ray EB, Siminoff L. Doctor–patient communication, cultural competence, and minority health: theoretical and empirical perspectives. Am Behav Sci 2006;49:835–52.
Mays N, Pope C. Qualitative research in health care: assessing quality in qualitative data. Br Med J. 2000;320:50–2.
Pope C, Ziebland S, Mays N. Qualitative research in health care: analysing qualitative data. Br Med J. 2000;320:114–6.
Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Diabetes Control and Complications Trial/Epidemiology of Diabetes and Complications Research Group. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342:381–9.
Nair KM, Dolovich LR, Ciliska DK, Lee HN. The perception of continuity of care from the perspective of patients with diabetes. Fam Med. 2005;37:118–24.
Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. J Am Med Assoc. 2002;288:475–82.
Brown JB, Harris S, Webster-Bogaert S, Wetmore S, Faulds C, Stewart M. The role of patient, physician and systemic factors in the management of type 2 diabetes mellitus. Fam Pract. 2002;19:344–9.
Puder FF, Keller U. Quality of diabetes care: problem of patient or doctor adherence? Swiss Med Wkly. 2003;133:530–4.
Rubin RR, Peyrot M, Siminerio LM. Health care and patient-reported outcomes: results of the cross-national diabetes attitudes, wishes and needs (DAWN) study. Diabetes Care. 2006;29:1249–55.
Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. J Am Med Assoc. 1999;282:583–9.
Freedman J, Loewe R. Barriers to communication about diabetes mellitus. J Fam Pract. 2000;49:507–12.
Peel E, Parry O, Douglas M, Lawton J. Blood glucose self-monitoring in non-insulin-treated type 2 diabetes: a qualitative study of patients’ perspectives. Br J Gen Pract. 2004;54:183–8.
Parry O, Peel E, Douglas M, Lawton J. Issues of cause and control in patient accounts of type 2 diabetes. Health Educ Res. 2006;21:97–107.
Acknowledgements
This work was supported in part by beyondblue: the national depression initiative and the Victorian Centre for Excellence in Depression and Related Disorders, the Australian Research Council, and by the Victorian Government Science, Technology, and Innovation Grant. We are grateful for the support of The University of Melbourne and Monash University, to the doctors who collaborated in the recruitment of participants, and to the men and women participated in the study.
Conflict of Interest
None disclosed
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kokanovic, R., Manderson, L. Exploring Doctor–Patient Communication in Immigrant Australians with Type 2 Diabetes: A Qualitative Study. J GEN INTERN MED 22, 459–463 (2007). https://doi.org/10.1007/s11606-007-0143-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-007-0143-2