Abstract
Background
Several contemporary risk stratification tools are now being used since the development of the Charlson Comorbidity Index (CCI) in 1987. The purpose of this systematic review and meta-analysis was to compare the utility of commonly used co-morbidity indices in predicting surgical outcomes.
Methods
A comprehensive review was performed to identify studies reporting an association between a pre-operative co-morbidity measurement and an outcome (30-day/in-hospital morbidity/mortality, 90-day morbidity/mortality, and severe complications). Meta-analysis was performed on the pooled data.
Results
A total of 111 included studies were included with a total cohort size 25,011,834 patients. The studies reporting the 5-item Modified Frailty Index (mFI-5) demonstrated a statistical association with an increase in the odds of in-hospital/30-day mortality (OR:1.97,95%CI: 1.55–2.49, p < 0.01). The pooled CCI results demonstrated an increase in the odds for in-hospital/30-day mortality (OR:1.44,95%CI: 1.27–1.64, p < 0.01). Pooled results for co-morbidity indices utilizing a scale-based continuous predictor were significantly associated with an increase in the odds of in-hospital/30-day morbidity (OR:1.32, 95% CI: 1.20–1.46, p < 0.01). On pooled analysis, the categorical results showed a higher odd for in-hospital/30-day morbidity (OR:1.74,95% CI: 1.50–2.02, p < 0.01). The mFI-5 was significantly associated with severe complications (Clavien-Dindo ≥ III) (OR:3.31,95% CI:1.13–9.67, p < 0.04). Pooled results for CCI showed a positive trend toward severe complications but were not significant.
Conclusion
The contemporary frailty-based index, mFI-5, outperformed the CCI in predicting short-term mortality and severe complications post-surgically. Risk stratification instruments that include a measure of frailty may be more predictive of surgical outcomes compared to traditional indices like the CCI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The current population is aging rapidly which contributes to the growing number of elderly patients presenting to undergo surgical procedures. It is estimated that approximately 53% of all surgeries are performed on patients greater than the age of 65. 1 The growing number of elderly surgical patients cannot necessarily be treated in the same way as the younger patient population. Patients below the age of 65 tend to be healthier, while older patients tend to have chronic medical problems. Yet chronological age does not necessarily predict outcome; instead, physiological age should be considered. Older patients often have one or more comorbidities, ultimately changing how physicians should view and treat them. 2
Developing a generalizable yet accurate method to risk stratify patients that takes into account their physiological age for treatment has been an ongoing task for many years, beginning with the Charlson Comorbidity Index (CCI). CCI was developed in 1987 as a way to risk stratify patients based on their comorbidities to predict mortality. 3 The work developed the index with patients admitted to a hospital’s medical service, then validated the index in a population of women with breast cancer. 3 The index is weighted, meaning it accounts for not only the number of diseases but their severity as well. For example, having a mild liver disease gives a score of 1, whereas having a moderate or severe liver disease gives a score of 3. The score for each comorbidity is summed and can give a total score up to 37. CCI has been used in numerous situations including inpatient services, 4,5 elective surgery, 6,7 and surgical oncology. 8,9,10 Despite its continued use, some physicians believe that it is outdated, especially for specific populations for which the original index was not intended. 11,12 There are several reasons that the a newer risk stratification tool should be utilized over the CCI. First, patients now survive longer than they did in 1987 when the original weights for the CCI were developed due to advancements in treatment options. 13 Second, we have found that the CCI score for surgical oncology patients is often homogenous and does not allow for sensitive risk stratification with regard to the commonality of co-morbid conditions in those diagnosed with the same type of cancer. Current research highlights that the CCI is not accurate for specific surgical patient populations and thus researchers have developed their own scoring systems to better risk stratify particular subsets of patients. 7,14
Many variations of the CCI have been developed including the Age-Adjusted CCI (ACCI) which takes into account chronological age, the Charlson-Deyo score (CCI-D) which is a 1992 CCI revision that allowed for use with ICD-9 codes, and the Elixhauser Co-morbidity Index (ECI). The ECI is a more recent model compared to the CCU that includes 31 unique co-morbidities. 15 Contemporary indices have been developed focusing on the variable measure of frailty versus categorical co-morbidities alone. Frailty is a measure is a state of limited physiological reserve that can have tremendous impact on surgical outcomes. 16 One such index is the 5-item modified Frailty Index (mFI-5) which has slowly been gaining popularity since its development in 2017. 17 One of the promising features of the mFI-5 over traditional options such as CCI is the inclusion of a measure of the patient’s specific functional dependent status (FDS). 17 Frailty and FDS has been shown in recent studies to be a strong predictor of surgical outcomes including complications, mortality, and adverse peri-operative events. 16,18,19 Indices that capture a patients FDS may prove to be more effective compared to co-morbidity-based indices alone. 20 The aim of this systematic review and meta-analysis was to identify the optimal comorbidity index that can be reliably measured from the electronic medical record for short term outcome prediction following surgical intervention.
Methods
Search Strategy and Exclusion Criteria
A literature search was performed in a comprehensive manner according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines (PRISMA guidelines). 21 An electronic search of PubMed, Embase, and EBSCO databases was performed using the combinations of “comorbidity index,” “comparison,” “surgery,” “mortality,” “morbidity,” “prediction,” and “outcome” in the keyword and title fields. The search was limited to contemporary studies published between 2014 and 2022 unless hand-selected through citation searching, in order to include recent more clinically relevant studies. Examiners reviewed all abstracts for potential inclusion. Inclusion criteria included studies that focused upon measuring the predictive capability of comorbidity indices prior to surgical intervention. Articles were excluded according to the following criteria: comorbidity indices that are not able to be measured/extracted from medical record data, non-English language, outcomes assessed other than in surgery, and review or meta-analysis articles. The full text of each article was then reviewed for data related to the key clinical outcomes outlined below; studies not including adequate data regarding surgical outcomes after surgery or trauma were excluded from the final cohort of studies for the meta-analysis. The surgical outcome data for the remaining articles was extracted. The systematic review included retrospective studies if they measured a comorbidity index or indices able to be calculated retrospectively from hospital database data and assessed outcomes after surgery or trauma. Additionally, studies were included in the meta-analysis if they assessed at least one of the key outcomes. Non-English studies, reviews, and meta-analyses were excluded. The majority of frailty instruments were excluded from this study. Indices that rely on frailty depend heavily on factors not consistently available in the medical record. 22,23 The five-item modified frailty index (mFI-5) is a less complex option that has shown to be just as effective in outcome prediction when compared to the more comprehensive 11 item mFI-11 and is closer in nature to a co-morbidity index rather than a multi-dimensional frailty index. 24
Quality Assessment of Studies
One researcher independently reviewed each study for strength of data utilizing the following data points: author(s), year, number of patients in cohort, indication for surgery, type of procedure, and surgical outcomes following the procedure (Table 1). The studies were assigned a score using a modified scoring system for minors. 25 Up to two points were assigned for each of the following standards: a clearly stated aim (+ 2), inclusion of consecutive patients with no exclusion or information detailing the reason for exclusion (+ 2), prospective data collection that details a clear collection plan (+ 2), endpoints relevant to this study assessed (+ 2), an unbiased assessment of the study endpoint through proper controls (+ 2), proper follow-up after study period (+ 2 for median and range of follow-up, + 1 for inexplicit information regarding follow-up), loss to follow-up less than 5% (+ 2 if all patients with missing medical record data were excluded), and prospective calculation of study size (+ 2 if they include data regarding the power of the study).
Outcomes of Interest
The primary outcome of this study was mortality within 3 months (in-hospital, 30-day, or 90-day mortality). Secondary outcomes were the rates of any complication (in-hospital, 30-day, or 90-day morbidity) and severe complications typically defined according to Clavien-Dindo (CD) guidelines or predefined by the author. 26 The outcome of overall survival (OS) was not reviewed as this measure has confounding variables that may not accurately capture morbidity and mortality due to the physical insult of surgery. For interpretation, mortality was divided into two groups (in-hospital/30-day and 90-day) as was morbidity (in-hospital/30-day and 90-day). Damhuis et al. has shown that the rate of morbidity and mortality vastly differs between the 30-day and 90-day time intervals and thus should be considered as separate groups. 27 For severe complications, outcomes defined as CD ≥ III or IV were grouped together and CD complications < III considered minor.
Data Extraction
The following data was extracted from all eligible studies: number of patients that underwent procedure, comorbidity indices measured, index cutoff, disease type, disease site, type of surgery, and surgical specialty. Data for each comorbidity indexes’ ability in predicting the following primary surgical outcomes were extracted when applicable: post-operative 30-day morbidity and/or mortality, 90-day morbidity and/or mortality, in-hospital morbidity and/or mortality, major complications (Clavien-Dindo grade III and above or Clavien-Dindo grade II and above) and overall complications.
Statistical Analysis
Meta-analysis was performed for the results of included studies when applicable. For the chosen outcomes of interest, odds ratios and 95% confidence intervals were extracted if available. Only the standard indices with sufficient combined results from all the studies were included in the meta-analysis (ECI, CCI, ACCI, CCI-D, mFI-5). Additionally, whether the index was assessed on a continuous predictor, or a cut-off was recorded. The co-morbidity indices utilizing continuous predictors were pooled in a group labeled scale. The co-morbidity indices using a cut-off value were pooled together in group labeled categorical. The statistical programming language R was then used to generate forest plots for the extracted odds ratios.
Results
Study Selection
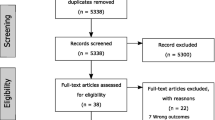
The initial search revealed 748 records with an additional three records attained through citation searching (PRISMA Fig. 1). From the combined 751 articles, 581 articles were excluded after being screened via title and abstract yielding 170 articles after duplicates were also removed. The group of 170 studies were then sought for retrieval and the full text reviewed for each, 7 reports were unable to be retrieved leaving 163 studies for the assessment. After reviewing the full text for 163 articles, 111 studies were included in this review (Tables 1, 2, 3, 4, 5, 6).
Study Characteristics
All 111 included studies were published between 2014 and 2022. The total cohort size of all studies assessed was 25,011,834 (cohort sizes ranged from 55 to 14,007,813). The operation of highest frequency was oncologic resection (n = 50/111, 45%). The other procedure types were amputation (n = 1/111, 0.9%), arthroplasty (n = 10/111, 9%), augmentation (n = 1/111, 0.9%), bypass (n = 2/111, 1.8%), fusion/decompression (n = 7/111, 6.3%), graft (n = 1/111, 0.9%), interventional (n = 1/111, 0.9%), reconstruction (n = 7/111, 6.3%), repair (n = 6/111, 5.4%), revascularization (n = 1/111, 0.9%), trauma (n = 8/111, 7.2%), and various others (n = 12/111, 10.8%). There were 25/111 studies included in this review that compared multiple comorbidity indices in the same cohort.
Comorbidity Instruments
Limiting included comorbidity indices per study to only those that meet the criteria for ease of use and reproducibility yielded 12 unique co-morbidity indices. In total, there were 136 co-morbidity indices assessed. The most common index assessed was the Charlson Comorbidity Index (CCI) (n = 42/136). Other indices assessed included the age-adjusted Charlson Comorbidity Index (ACCI) (n = 17/136), five-item modified frailty index (mFI-5) (n = 40/136), Elixhauser Comorbidity Index/Measure (ECI/ECM) (n = 17/136), modified ACCI (mACCI) (n = 1/136), Charlson-Deyo Comorbidity Index (CCI-D) (n = 9/136), comorbidity-polypharmacy score (CPS) (n = 7/136), modified Charlson Comorbidity Index (mCCI) (n = 1/136), enhanced ECI (n = 1/136), and age-adjusted mFI-5 (aamFI-5) (n = 1/136).
90-Day Morbidity and Mortality
Three studies reported data for 90-day mortality. There was not enough combined data to perform meta-analysis on these results. Franko 2018 28 reported a statistically significant association between CCI-D and 90-day mortality for patients undergoing esophagectomy (OR: 1.58, 95% CI: 1.01–2.49, p = 0.046). McFerrin 2019 29 reported a statistically significant association between CCI and oncologic cystectomy (HR: 1.42, 95% CI: 1.27–1.57, p < 0.001). Chiu 2015 30 reported a statistically significant association between CCI-D and 90-day mortality in patients undergoing oncologic hepatic resection (HR: 1.05, 95% CI: 1.023–1.068, p < 0.001). One study reported data for 90-day morbidity. DH Park 2022 31 reported a statistically insignificant association between CCI and 90-day morbidity in patients undergoing genitourinary oncologic resection (OR: 1.24, 95% CI: 0.8–1.04, p = 0.341). One study also reported data for 90-day major morbidity. Pujara 2015 32 found a statistical association between a polypharmacy score of greater than or equal to five and 90-day major morbidity among patients undergoing oncologic gastrectomy (OR: 2.36, 95% CI: 1.08–5.17, p = 0.3). The same study did not find a statistical association between CCI and 90-day major morbidity.
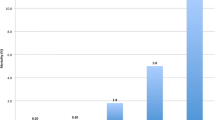
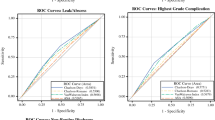
In-Hospital/30-Day Mortality
Fifty-four studies reported outcomes on in-hospital/30-day mortality, twenty-one of those studies reported odds ratios that could be pooled for meta-analysis. Of the twenty-one studies, there were four studies 24,33,34,35 that reported unadjusted data while the remaining seventeen studies reported adjusted data. Eleven studies 24,35,36,37,38,39,40,41,42,43,44,45 (20%) reported odds ratios for the mFI-5 and were pooled for meta-analysis. Of the studies reporting mFI-5, there was a statistical association with an increase in the odds of in-hospital/30-day mortality (OR: 1.97, 95% CI: 1.55–2.49, p < 0.01) (Fig. 2). There were five studies 39,46,47,48,49 (9.4%) that reported odds ratios for CCI and were pooled for meta-analysis. Of the pooled CCI results, there was an increase in the odds for in-hospital/30-day mortality (OR: 1.44, 95% CI: 1.27–1.64, p < 0.01) (Fig. 2). Pooled results for ACCI (n = 2, p = 0.38),33,34 CCI-D (n = 1), 28 and ECI (n = 1) 50 showed a positive trend but were not significant (Fig. 2).
Comparative performance of indices for in-hospital/30-day mortality. Shown: age-adjusted Charlson (ACCI), Charlson Co-morbidity Index (CCI), Charlson-Deyo score (CCI-D), Elixhauser Co-morbidity Index (ECI), and 5-item Modified Frailty Index (mFI-5). The overall effect of mFI-5 and CCI showed a statistical association with in-hospital/30-day mortality
In-Hospital/30-Day Complications
Fifty-two studies reported outcomes for in-hospital/30-day morbidity. There were 26 (50%) studies that reported ORs for in-hospital/30-day morbidity that could be pooled for meta-analysis. Of the pooled studies, eleven studies 24,34,35,51,52,53,54,55,56,57 (21.2%) reported unadjusted odds ratios. Of the pooled unadjusted results, there was a statistical association between co-morbidities and an increase in the odds of in-hospital/30-day morbidity (OR: 1.62, 95% CI: 1.30–2.02, p < 0.01) (Fig. 3). Sixteen studies 36,38,40,41,42,43,44,45,58,59,60,61,62,63,64 (30.8%) reported adjusted odds ratios that were able to be pooled for meta-analysis. It should be noted that all studies (n = 16) from which adjusted data was obtained utilized the mFI-5. Of the pooled adjusted results combining data for all of the co-morbidity indices, there was a statistical association between the co-morbidity instruments and an increase in the odds of in-hospital/30-day morbidity (OR: 1.47, 95% CI: 1.31–1.64, p < 0.01) (Fig. 3). Ten studies 24,34,35,36,42,43,44,51,54,56 (19.2%) reported odds ratios assessing co-morbidity instruments utilizing a continuous predictor (scale) and were pooled for meta-analysis. Pooled results for co-morbidity indices utilizing a scale-based predictor were significantly associated with an increase in the odds of in-hospital/30-day morbidity (OR: 1.32, 95% CI: 1.20–1.46, p < 0.01) (Fig. 4). Sixteen studies 38,40,41,45,52,53,55,57,58,59,60,61,62,63,64,65 (30.8%) reported odds ratios assessing co-morbidities on a categorical basis. On pooled analysis, the categorical results showed a higher odd for in-hospital/30-day morbidity (OR: 1.74, 95% CI: 1.50–2.02, p < 0.01) (Fig. 4). One study (Marya et al. 2016) reported an increased odds of 30-day morbidity utilizing the ACCI (OR: 4.16, 95% CI: 1.87–9.26) and CCI (OR: 3.35, 95% CI: 1.08–10.40) that showed increased statistical power compared to the other studies (Fig. 4).
Comparative performance of indices using a continuous predictor (scale) and studies that use a cut-off (categorical) for in-hospital/30-day morbidity. Shown: age-adjusted Charlson (ACCI), Charlson Co-morbidity Index (CCI), and 5-item Modified Frailty Index (mFI-5). The overall effect of scaled and categorical indices showed a statistical association with in-hospital/30-day morbidity
Comparative performance of adjusted and unadjusted study results for in-hospital/30-day morbidity. Shown: age-adjusted Charlson (ACCI), Charlson Co-morbidity Index (CCI), and 5-item Modified Frailty Index (mFI-5). The overall effect for adjusted and unadjusted data predicted in-hospital/30-day morbidity
Severe Complications
Eighteen studies 34,41,44,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79 reported outcomes on severe complications. Severe complications were typically defined as CD grade III/IV and higher. 26 Eleven studies 34,41,44,65,68,71,72,73,74,77,78 (61%) reported odds ratios that were able to be pooled for meta-analysis (Fig. 5). Six studies 41,43,65,68,77,78 (33%) reported odds ratios for mFI-5 that were able to be pooled for meta-analysis. Of the pooled results, mFI-5 was significantly associated with severe complications (OR: 3.31, 95% CI: 1.13–9.67, p < 0.04) (Fig. 5). Pooled results for ACCI (n = 3, p = 0.19) and CCI (n = 2, p = 0.38) showed a positive trend toward severe complications but were not significant (Fig. 5).
Discussion
In this systematic review and meta-analysis of 111 studies, we found that, the mFI-5 outperformed the other traditional comorbidity indices (CCI, ACCI, ECI, CCI-D) in predicting in-hospital/30-day mortality and severe complications post-operatively. There was a great degree of statistical reporting heterogeneity among studies included which prevented two of the key outcomes (90-day mortality and morbidity) from being included in meta-analysis. Additionally, studies utilizing CPS were unable to be included in the meta-analysis due to how few studies reported data and based on their level of heterogeneity.
Additionally, it was found that Marya et al. 2016 reported extremely high ORs for 30-day morbidity utilizing the CCI and ACCI (Fig. 3). The reason for the high statistical power in this study are probably related to the fact that it represents one of the largest single-center, single-surgeon bilateral simultaneous total knee arthroplasty (BSLKA) studies done in the Asian population. Thus, the variation in management was kept for the most part homogenous among all participants which could have allowed for a more controlled study environment to measure CCI and ACCI. It was found that the ACCI out-performed CCI probably due to the inclusion of age since this is a major risk factor in BSLKA. 52 Unfortunately, there was limited reporting of studies utilizing the ACCI that were able to be included in the meta-analysis making the comparison to mF-5 somewhat limited. However, our meta-analysis still found the mFI-5 to be superior to the ACCI in predicting severe complications and in-hospital/30-day mortality.
To date, this is the first systematic review and meta-analysis to compare the effectiveness of co-morbidity indices versus the newer mFI-5 index. Functional dependent status (FDS) captured by mFI-5 could be the reason it out-performed the other indices on meta-analysis. FDS could better capture health status and risk for complications than traditional co-morbidity lists. The role of frailty in surgical outcomes has been highlighted in a recent well conducted systematic review and meta-analysis that found frailty indices significantly associated with 30-day mortality, adverse discharge disposition, post-operative complications, long-term mortality, and hospital length of stay. 16
The strengths of this study include the comprehensive nature of the literature search and the sound statistical comparisons made when available. Limitations of this review include the fact that the meta-analysis was limited to studies reporting ORs and thus many important data points may have not been included. The heterogeneity among reporting styles included in this study signal a need for more uniformity among the studies investigating frailty and co-morbidity indices in surgical patients. This would allow a more comprehensive meta-analysis to be performed to compare each index. Additionally, there may have been cohort overlap between studies which could have potentiated a bias in the results and our conclusions. In the severe complications category, some studies used their own definition and severe and this could have differed from the CD grading system of complications. Determining the best index per specialty would provide more value to this work. However, while attempting to make a statistical comparison of the different indices within a specialty, we realized that we do not have the data to make such a quantitative analysis. Within each specialty group, we only have multiple papers for mFI-5 but not any of the other indices. This is something that we would like to address in a future literature review as more publications become available. Finally, quality assessment of the studies found that generally the studies included were sound in methodology.
The results of this review highlight the value of newer frailty indices like mFI-5 in predicting surgical outcomes. There is a need for an increased degree of statistical homogeneity among studies attempting to validate co-morbidity indices. Specifically, the co-morbidity polypharmacy score (CPS) needs for studies to be conducted to allow a better comparison of the predictive capability of an index focused on capturing polypharmacy. As society ages, both frailty and polypharmacy are becoming significant factors in surgical performance and are in need of simple, yet accurate tools for their measure.
Conclusion
In conclusion, the cumulative data of this study suggest that frailty indices like mFI-5 are more predictive over traditional co-morbidity indices that do not include a capture of functional dependent status regarding surgical outcomes. Further studies are warranted to obtain a wider picture of how mFI-5 compares to other indices in predicting surgical outcomes including a comparison of both frailty and polypharmacy-based indices.
References
Veering BT. Management of anaesthesia in elderly patients. Curr Opin Anaesthesiol. 1999;12(3):333-6.
Wolfe JD, Wolfe NK, Rich MW. Perioperative care of the geriatric patient for noncardiac surgery. Clin Cardiol. 2020;43(2):127-36.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-83.
Menendez ME, Ring D. A Comparison of the Charlson and Elixhauser Comorbidity Measures to Predict Inpatient Mortality After Proximal Humerus Fracture. J Orthop Trauma. 2015;29(11):488-93.
Ofori-Asenso R, Zomer E, Chin KL, Si S, Markey P, Tacey M, et al. Effect of Comorbidity Assessed By the Charlson Comorbidity Index On the Length of Stay, Costs and Mortality Among Older Adults Hospitalised for Acute Stroke. Int J Environ Res Public Health. 2018;2532. https://doi.org/10.3390/ijerph15112532.
Bulow E, Rolfson O, Cnudde P, Rogmark C, Garellick G, Nemes S. Comorbidity does not predict long-term mortality after total hip arthroplasty. Acta Orthopaedica. 2017;88(5):472-7.
Wasilewicz M, Raszeja-Wyszomirska J, Wunsch E, Wojcicki M, Milkiewicz P. Modified Charlson Comorbidity Index in predicting early mortality after liver transplantation. Transplant Proc. 2009;41(8):3117-8.
Strombom P, Widmar M, Keskin M, Gennarelli RL, Lynn P, Smith JJ, et al. Assessment of the Value of Comorbidity Indices for Risk Adjustment in Colorectal Surgery Patients. Annals of Surgical Oncology. 2019;26(9):2797-804.
Sun V, Burhenn PS, Lai L, Hurria A. The Impact of Comorbidity on Surgical Outcomes in Older Adults with Cancer. Semin Oncol Nurs. 2017;33(1):80-6.
Bosch DJ, Pultrum BB, de Bock GH, Oosterhuis JK, Rodgers MG, Plukker JT. Comparison of different risk-adjustment models in assessing short-term surgical outcome after transthoracic esophagectomy in patients with esophageal cancer. Am J Surg. 2011;202(3):303-9.
Dell'Oglio P, Tian Z, Leyh-Bannurah SR, Trudeau V, Larcher A, Moschini M, et al. Short-Form Charlson Comorbidity Index for Assessment of Perioperative Mortality After Radical Cystectomy. J Natl Compr Canc Netw. 2017;15(3):327-33.
Lambert E, D'Hondt F, Mazzone E, Vollemaere J, Larcher A, Van Der Jeugt J, et al. Time to Move On: The Impending Need for a New Disease-specific Comorbidity Index for Bladder Cancer Patients Undergoing Robotassisted Radical Cystectomy. Eur Urol Focus. 2019;139-141.
Ternavasio-De La Vega HG, Castaño-Romero F, Ragozzino S, Sánchez González R, Vaquero-Herrero MP, Siller-Ruiz M, et al. The updated Charlson comorbidity index is a useful predictor of mortality in patients with <i>Staphylococcus aureus</i> bacteraemia. Epidemiology and Infection. 2018;146(16):2122–30.
Mehta HB, Yong S, Sura SD, Hughes BD, Kuo YF, Williams SB, et al. Development of comorbidity score for patients undergoing major surgery. Health Services Research. 2019;54(6):1223-32.
Baron RB, Neifert SN, Ranson WA, Schupper AJ, Gal JS, Cho SK, et al. A Comparison of the Elixhauser and Charlson Comorbidity Indices: Predicting In-Hospital Complications Following Anterior Lumbar Interbody Fusions. World Neurosurg. 2020;144:e353-e60.
Shaw JF, Budiansky D, Sharif F, McIsaac DI. The Association of Frailty with Outcomes after Cancer Surgery: A Systematic Review and Metaanalysis. Ann Surg Oncol. 2022;29(8):4690-704.
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. New 5-Factor Modified Frailty Index Using American College of Surgeons NSQIP Data. J Am Coll Surg. 2018;226(2):173–81 e8.
Clifton JC, Engoren M, Shotwell MS, Martin BJ, Clemens EM, Guillamondegui OD, et al. The Impact of Functional Dependence and Related Surgical Complications on Postoperative Mortality. Journal of Medical Systems. 2022;46(1).
Robinson TN, Eiseman B, Wallace JI, Church SD, McFann KK, Pfister SM, et al. Redefining geriatric preoperative assessment using frailty, disability and co-morbidity. Ann Surg. 2009;250(3):449-55.
McIntyre MK, Gandhi C, Dragonette J, Schmidt M, Cole C, Santarelli J, et al. A comparison of frailty indices in predicting length of inpatient stay and discharge destination following angiogram-negative subarachnoid hemorrhage. Br J Neurosurg. 2021;35(4):402-7.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1-34.
Shahrokni A, Tin A, Alexander K, Sarraf S, Afonso A, Filippova O, et al. Development and Evaluation of a New Frailty Index for Older Surgical Patients With Cancer. JAMA Network Open. 2019;2(5):e193545.
Gani F, Canner JK, Pawlik TM. Use of the Modified Frailty Index in the American College of Surgeons National Surgical Improvement Program Database. JAMA Surgery. 2017;152(2):205.
Pierce KE, Naessig S, Kummer N, Larsen K, Ahmad W, Passfall L, et al. The Five-item Modified Frailty Index is Predictive of 30-day Postoperative Complications in Patients Undergoing Spine Surgery. Spine (Phila Pa 1976). 2021;46(14):939–43.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712-6.
Hebert M, Cartier R, Dagenais F, Langlois Y, Coutu M, Noiseux N, et al. Standardizing Postoperative Complications-Validating the Clavien-Dindo Complications Classification in Cardiac Surgery. Semin Thorac Cardiovasc Surg. 2021;33(2):443-51.
Damhuis RA, Wijnhoven BP, Plaisier PW, Kirkels WJ, Kranse R, van Lanschot JJ. Comparison of 30-day, 90-day and in-hospital postoperative mortality for eight different cancer types. Br J Surg. 2012;99(8):1149-54.
Franko J, McAvoy S. Timing of esophagectomy after neoadjuvant chemoradiation treatment in squamous cell carcinoma. Surgery. 2018;164(3):455-9.
McFerrin C, Raza SJ, May A, Davaro F, Siddiqui S, Hamilton Z. Charlson comorbidity score is associated with readmission to the index operative hospital after radical cystectomy and correlates with 90-day mortality risk. Int Urol Nephrol. 2019;51(10):1755-62.
Chiu CC, Wang JJ, Chen YS, Chen JJ, Tsai TC, Lai CC, et al. Trends and predictors of outcomes after surgery for hepatocellular carcinoma: A nationwide population-based study in Taiwan. Eur J Surg Oncol. 2015;41(9):1170-8.
Park DH, Yoo S, Do MT, Yoon HS, Jung G, Suh J, et al. Geriatric assessment using the G8 to predict postoperative complications in patients undergoing major uro-oncologic surgery: Comparison with the Charlson Comorbidity Index. J Geriatr Oncol. 2022;13(4):426-31.
Pujara D, Mansfield P, Ajani J, Blum M, Elimova E, Chiang YJ, et al. Comprehensive geriatric assessment in patients with gastric and gastroesophageal adenocarcinoma undergoing gastrectomy. J Surg Oncol. 2015;112(8):883-7.
Bateni SB, Bold RJ, Meyers FJ, Canter DJ, Canter RJ. Comparison of common risk stratification indices to predict outcomes among stage IV cancer patients with bowel obstruction undergoing surgery. J Surg Oncol. 2018;117(3):479-87.
Lakomkin N, Zuckerman SL, Stannard B, Montejo J, Sussman ES, Virojanapa J, et al. Preoperative Risk Stratification in Spine Tumor Surgery: A Comparison of the Modified Charlson Index, Frailty Index, and ASA Score. Spine (Phila Pa 1976). 2019;44(13):E782-E7.
Subramaniam S, Aalberg JJ, Soriano RP, Divino CM. The 5-Factor Modified Frailty Index in the Geriatric Surgical Population. Am Surg. 2021;87(9):1420-5.
Andersen JC, Gabel JA, Mannoia KA, Kiang SC, Patel ST, Teruya TH, et al. 5-Item Modified Frailty Index Predicts Outcomes After Below-Knee Amputation in the Vascular Quality Initiative Amputation Registry. Am Surg. 2020;86(10):1225-9.
Braet DJ, Taaffe JP, Dombrovskiy VY, Bath J, Kruse RL, Vogel TR. Modified frailty index as an indicator for outcomes, discharge status, and readmission after lower extremity bypass surgery for critical limb ischemia. J Vasc Nurs. 2020;38(4):171-5.
Goshtasbi K, Birkenbeuel JL, Lehrich BM, Abiri A, Haidar YM, Tjoa T, et al. Association Between 5-Item Modified Frailty Index and Short-term Outcomes in Complex Head and Neck Surgery. Otolaryngol Head Neck Surg. 2022;166(3):482-9.
Khalafallah AM, Huq S, Jimenez AE, Brem H, Mukherjee D. The 5-factor modified frailty index: an effective predictor of mortality in brain tumor patients. Journal of Neurosurgery. 2020;135(1):78–86.
Segal DN, Wilson JM, Staley C, Michael KW. The 5-Item Modified Frailty Index Is Predictive of 30-Day Postoperative Complications in Patients Undergoing Kyphoplasty Vertebral Augmentation. World Neurosurg. 2018;116:e225-e31.
Seilern Und Aspang J, Zamanzadeh RS, Schwartz AM, Premkumar A, Martin JR, Wilson JM. The Age-Adjusted Modified Frailty Index: An Improved Risk Stratification Tool for Patients Undergoing Primary Total Hip Arthroplasty. J Arthroplasty. 2022;37(6):1098–104.
Tracy BM, Wilson JM, Smith RN, Schenker ML, Gelbard RB. The 5-Item Modified Frailty Index Predicts Adverse Outcomes in Trauma. J Surg Res. 2020;253:167-72.
Traven SA, McGurk KM, Reeves RA, Walton ZJ, Woolf SK, Slone HS. Modified frailty index predicts medical complications, length of stay, readmission, and mortality following total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(10):1854-60.
Traven SA, Reeves RA, Althoff AD, Slone HS, Walton ZJ. New Five-Factor Modified Frailty Index Predicts Morbidity and Mortality in Geriatric Hip Fractures. J Orthop Trauma. 2019;33(7):319-23.
Weaver DJ, Malik AT, Jain N, Yu E, Kim J, Khan SN. The Modified 5-Item Frailty Index: A Concise and Useful Tool for Assessing the Impact of Frailty on Postoperative Morbidity Following Elective Posterior Lumbar Fusions. World Neurosurg. 2019;626-632.
Aicher BO, Betancourt-Ramirez A, Grossman MD, Heise H, Schroeppel TJ, Hernandez MC, et al. Validation of the American Association for the Surgery of Trauma Emergency General Surgery Grading System for Colorectal Resection: An EAST Multicenter Study. Am Surg. 2022;88(5):953-8.
Aicher BO, Hernandez MC, Betancourt-Ramirez A, Grossman MD, Heise H, Schroeppel TJ, et al. Colorectal resection in emergency general surgery: An EAST multicenter trial. J Trauma Acute Care Surg. 2020;89(6):1023-31.
Nossaman VE, Larsen BE, DiGiacomo JC, Manuelyan Z, Afram R, Shukry S, et al. Mortality is predicted by Comorbidity Polypharmacy score but not Charlson Comorbidity Index in geriatric trauma patients. Am J Surg. 2018;216(1):42-5.
Palumbo C, Knipper S, Dzyuba-Negrean C, Pecoraro A, Rosiello G, Tian Z, et al. Complication rates, failure to rescue and in-hospital mortality after cytoreductive nephrectomy in the older patients. J Geriatr Oncol. 2020;11(4):718-23.
Potts J, Nagaraja V, Al Suwaidi J, Brugaletta S, Martinez SC, Alraies C, et al. The influence of Elixhauser comorbidity index on percutaneous coronary intervention outcomes. Catheter Cardiovasc Interv. 2019;94(2):195-203.
Koseki Y, Hikage M, Fujiya K, Kamiya S, Tanizawa Y, Bando E, et al. Utility of a modified age-adjusted Charlson Comorbidity Index in predicting cause-specific survival among patients with gastric cancer. Eur J Surg Oncol. 2021;47(8):2010-5.
Marya SK, Amit P, Singh C. Impact of Charlson indices and comorbid conditions on complication risk in bilateral simultaneous total knee arthroplasty. Knee. 2016;23(6):955-9.
Elsamadicy AA, Freedman IG, Koo AB, David WB, Reeves BC, Havlik J, et al. Modified-frailty index does not independently predict complications, hospital length of stay or 30-day readmission rates following posterior lumbar decompression and fusion for spondylolisthesis. Spine J. 2021;21(11):1812-21.
Elsamadicy AA, Havlik JL, Reeves B, Sherman J, Koo AB, Pennington Z, et al. Assessment of Frailty Indices and Charlson Comorbidity Index for Predicting Adverse Outcomes in Patients Undergoing Surgery for Spine Metastases: A National Database Analysis. World Neurosurg. 2022;1058-1070
Goldwag J, Harris A, Bettis AD. 5-Item Modified Frailty Index as a Preoperative Predictor of Morbidity Following Minimally Invasive Partial Nephrectomy. Urology. 2021;157:138-42.
Luo J, Carter GC, Agarwal JP, Kwok AC. The 5-Factor Modified Frailty Index as a Predictor of 30-day Complications in Pressure Ulcer Repair. J Surg Res. 2021;265:21-6.
Zreik J, Alvi MA, Yolcu YU, Sebastian AS, Freedman BA, Bydon M. Utility of the 5-Item Modified Frailty Index for Predicting Adverse Outcomes Following Elective Anterior Cervical Discectomy and Fusion. World Neurosurg. 2021;146:e670-e7.
Chen SY, Stem M, Cerullo M, Gearhart SL, Safar B, Fang SH, et al. The Effect of Frailty Index on Early Outcomes after Combined Colorectal and Liver Resections. J Gastrointest Surg. 2018;22(4):640-9.
Dammeyer K, Alfonso AR, Diep GK, Kantar RS, Berman ZP, Daar DA, et al. Predicting postoperative complications following mastectomy in the elderly: Evidence for the 5-factor frailty index. Breast J. 2021;27(6):509-13.
Hermiz SJR, Lauzon S, Brown G, Herrera FA. Use of a 5-Item Modified Frailty Index for Risk Stratification in Patients Undergoing Breast Reconstruction. Ann Plast Surg. 2021;86(6S Suppl 5):S615-S21.
Holzgrefe RE, Wilson JM, Staley CA, Anderson TL, Wagner ER, Gottschalk MB. Modified frailty index is an effective risk-stratification tool for patients undergoing total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(7):1232-40.
Lee CC, Hunter WP, Hajibandeh JT, Peacock ZS. Does the Modified Frailty Index (mFI-5) Predict Adverse Outcomes in Maxillofacial Fracture Repair? J Oral Maxillofac Surg. 2022;80(3):472-80.
Lee J, Alfonso AR, Kantar RS, Diep GK, Berman ZP, Ramly EP, et al. Modified Frailty Index Predicts Postoperative Complications following Panniculectomy in the Elderly. Plast Reconstr Surg Glob Open. 2020;8(7):e2987.
Magno-Pardon DA, Luo J, Carter GC, Agarwal JP, Kwok AC. An Analysis of the Modified Five-Item Frailty Index for Predicting Complications following Free Flap Breast Reconstruction. Plast Reconstr Surg. 2022;149(1):41-7.
Liu H, Akhavan A, Ibelli T, Alerte E, Etigunta S, Kuruvilla A, et al. Using the Modified Frailty Index to Predict Complications in Breast Reduction: A National Surgical Quality Improvement Program Study of 14,160 Cases. Aesthet Surg J. 2022;42(8): 890-899.
Ranson WA, Neifert SN, Cheung ZB, Mikhail CM, Caridi JM, Cho SK. Predicting In-Hospital Complications After Anterior Cervical Discectomy and Fusion: A Comparison of the Elixhauser and Charlson Comorbidity Indices. World Neurosurg. 2020;134:e487-e96.
Gordon AM, Conway CA, Sheth BK, Magruder ML, Choueka J. The 5-Item Modified Frailty Index for Risk Stratification of Patients Undergoing Total Elbow Arthroplasty. Hand (N Y) 2022. https://doi.org/10.1177/15589447221093728
Ravivarapu KT, Garden EB, Al-Alao O, Small AC, Palese MA. Adrenalectomy outcomes predicted by a 5-item frailty index (5-iFI) in the ACS-NSQIP database. Am J Surg. 2022;223(6):1120-5.
Ahola R, Siiki A, Rinta-Kiikka I, Laitinen I, Antila A, Jamsen E, et al. Preoperative measures predicting outcome after pancreatic resection in aged patients. Scand J Surg. 2022;111(1):14574969221083136.
Dodhia S, Fitzgerald CWR, McLean AT, Yuan A, Valero Mayor C, Adilbay D, et al. Predictors of surgical complications in patients with sinonasal malignancy. J Surg Oncol. 2021;124(5):731-9.
Kahl A, du Bois A, Harter P, Prader S, Schneider S, Heitz F, et al. Prognostic Value of the Age-Adjusted Charlson Comorbidity Index (ACCI) on Short- and Long-Term Outcome in Patients with Advanced Primary Epithelial Ovarian Cancer. Ann Surg Oncol. 2017;24(12):3692-9.
Shinkawa H, Tanaka S, Takemura S, Amano R, Kimura K, Nishioka T, et al. Predictive Value of the Age-Adjusted Charlson Comorbidity Index for Outcomes After Hepatic Resection of Hepatocellular Carcinoma. World J Surg. 2020;44(11):3901-14.
Fragkiadis E, Alamanis C, Constantinides CA, Mitropoulos D. Prediction of post radical nephrectomy complications based on patient comorbidity preoperatively. Arch Ital Urol Androl. 2021;93(3):251-4.
Kocher NJ, Canes D, Bensalah K, Roupret M, Lallas C, Margulis V, et al. Incidence and preoperative predictors for major complications following radical nephroureterectomy. Transl Androl Urol. 2020;9(4):1786-93.
Strombom P, Widmar M, Keskin M, Gennarelli RL, Lynn P, Smith JJ, et al. Assessment of the Value of Comorbidity Indices for Risk Adjustment in Colorectal Surgery Patients. Ann Surg Oncol. 2019;26(9):2797-804.
Woldu SL, Sanli O, Clinton TN, Lotan Y. Validating the predictors of outcomes after radical cystectomy for bladder cancer. Cancer. 2019;125(2):223-31.
Mah SJ, Anpalagan T, Marcucci M, Eiriksson L, Reade CJ, Jimenez W, et al. The five-factor modified frailty index predicts adverse postoperative and chemotherapy outcomes in gynecologic oncology. Gynecol Oncol. 2022;166(1):154-61.
Keller DS, Reif de Paula T, Kiran RP, Nemeth SK. Evaluating the association of the new National Surgical Quality Improvement Program modified 5-factor frailty index with outcomes in elective colorectal surgery. Colorectal Dis. 2020;22(10):1396–405.
Al-Khamis A, Warner C, Park J, Marecik S, Davis N, Mellgren A, et al. Modified frailty index predicts early outcomes after colorectal surgery: an ACS-NSQIP study. Colorectal Dis. 2019;21(10):1192-205.
Author information
Authors and Affiliations
Contributions
1. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: Noah A. Clements, Robert C.G. Martin II, MD, PhD.
2. Drafting the work or revising it critically for important intellectual content: Noah A. Clements, Jeremy T. Gaskins, PhD, Robert C.G. Martin II, MD, PhD.
3. Final approval of the version to be published: Noah A. Clements, Jeremy T. Gaskins, PhD, Robert C.G. Martin II, MD, PhD.
4. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy: Noah A. Clements, Jeremy T. Gaskins, PhD, Robert C.G. Martin II, MD, PhD.
Corresponding author
Ethics declarations
Not applicable since a meta-analysis.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clements, N.A., Gaskins, J.T. & Martin, R.C.G. Predictive Ability of Comorbidity Indices for Surgical Morbidity and Mortality: a Systematic Review and Meta-analysis. J Gastrointest Surg 27, 1971–1987 (2023). https://doi.org/10.1007/s11605-023-05743-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05743-4