Abstract
Background
Simple ileocecectomy and right hemicolectomy are two potential operative approaches to treat patients with neuroendocrine neoplasm in the terminal ileum and/or cecum (IC-NENs). We sought to define the long-term outcome of patients undergoing ileocecectomy versus right hemicolectomy for IC-NENs, as well as characterize number of nodes evaluated and lymph node metastasis (LNM) associated with each procedure.
Methods
Patients who underwent curative-intent resections for IC-NENs between 2000 and 2016 were identified from a multi-institutional database. The clinicopathologic characteristics, surgical procedures, and the overall (OS) and recurrence-free survival (RFS) were compared among patients who underwent formal right hemicolectomy versus ileocecectomy only.
Results
Among 127 patients with IC-NENs, median size of the largest tumor size was 2.0 (IQR 1.2–2.9) cm; 35 (27.6%) patients had multiple lesions. At the time of surgery, 93 (73.2%) patients underwent a right hemicolectomy, whereas 34 (26.8%) had ileocecectomy only. Every patient had a lymph node dissection (LND) with a median number of 16 (IQR 12–22) nodes evaluated. A majority (n = 110, 86.6%) of patients had LNM with a median number of 3 (IQR 2–5) LNM. Patients who underwent hemicolectomy had more lymph nodes evaluated versus patients who had an ileocecectomy only (median, 18 vs. 14, p = 0.004). Patients who underwent formal right hemicolectomy versus ileocecectomy had a similar OS (median OS, 101.9 vs. 144.5 months, p = 0.44) and RFS (median RFS, 70.3 vs. not attained, p = 0.80), respectively.
Conclusions
Ileocecectomy had similar long-term outcomes versus right hemicolectomy in treatment of IC-NENs despite a difference in the lymph node harvest.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With improvement in imaging modalities, the detection of incidental gastrointestinal neuroendocrine neoplasms (NENs) is increasing worldwide.1 While small bowel NENs remain rare, these tumors constitute approximately 15% of all neoplasm of the jejunum and 60% of the ileum.1,2 For most patients with NENs arising in the duodenum, small intestine, and colon, surgical resection of the involved segment of bowel with regional lymphadenectomy is recommended as the standard of care.3,4 The National Comprehensive Cancer Network (NCCN) recommends right hemicolectomy for patients with distal ileal carcinoma with ligation of the ileocolic artery and subsequent regional lymphadenectomy.3 In contrast, the North American Neuroendocrine Tumors Society (NANETS), European Neuroendocrine Tumor Society (ENETS), and NCCN guidelines do not provide specific recommendations on the optimal surgical procedure for terminal ileum and/or cecal NENs (IC-NENs). Traditionally, simple ileocecectomy or right hemicolectomy are both considered potentially appropriate as long as a negative margin is achieved and a regional lymphadenectomy is performed.4,5,6,7
Because of the relatively indolent biological nature of most IC-NENs,8 the survival benefit of simple ileocecectomy versus formal right hemicolectomy has been debated. For example, several guidelines have recommended right hemicolectomy for IC-NENs larger than 2 cm or NENs with aggressive features (i.e., lymphovascular invasion, atypical or mixed with adenocarcinoma).4,5,9,10 These recommendations have been questioned, however, as several studies have suggested similar long-term survival among patients with IC-NENs following formal right hemicolectomy versus simple ileocecectomy.11,12 These studies noted that right hemicolectomy may also be associated with increased operation time and postoperative morbidity.11,12 Previous studies have, however, been limited by small sample size, as well as were single institution in nature.
Therefore, the objective of the current study was to define the long-term outcome of patients undergoing ileocecectomy versus formal right hemicolectomy for IC-NENs. In addition, using a large multi-center database, we sought to characterize the utilization of lymphadenectomy, as well as the total number of nodes evaluated and the impact of lymph node metastasis (LNM) on long-term outcome of patients with IC-NENs.
Materials and Methods
Data Collection and Study Design
The US Neuroendocrine Tumor Study Group (US-NETSG) is a collaboration of eight academic medical centers: the Ohio State University, Vanderbilt University, Emory University, Stanford University, the John Hopkins University, Washington University in St. Louis, University of Michigan, and University of Wisconsin. Adult patients with gastroenteropancreatic neuroendocrine neoplasms (GEP-NEN, stages I–IV) who underwent surgical resection between 2000 and 2016 were identified at each institution. Clinicopathologic data and information on long-term outcomes were collected. Data collection was approved by the Institutional Review Boards at each participating institution. After deidentification, the data were shared among the collaborating institutions for analysis.11,13
Patients who underwent surgical resection for NENs at the terminal ileum (defined as within 10 cm from the ileocecal valve) and/or cecum were included. These patients were classified by surgical procedure type: ileocecectomy versus right hemicolectomy (right hemicolectomy with segmental small bowel resection). Compared with formal right hemicolectomy, ileocecectomy was defined as only regional resection of the ileocolic vessels with no resection of right colic vessels or middle colic vessels and no removal of the hepatic flexure. The mesenteric lymph nodes were mainly dissected along the course of ileocolic vessels. The terminal ileum was resected at some distance away from the ileocecal valve, depending upon the location of tumor and amount of blood supply for the remaining bowel.
Post-operative morbidity was classified from grade I to grade V according to the Clavien-Dindo classification.14 Overall survival (OS) was calculated from the date of the surgery until the date of last follow-up or date of death. Recurrence-free survival (RFS) was measured from time of curative intent resection to disease recurrence, death, or last documented follow-up in patients who had macroscopically negative (R0 or R1) final resection margins.
Statistical Analysis
Categorical variables were reported as totals and percentages and compared using the χ2 test or Fisher exact test as appropriate. Continuous variables were expressed as median with interquartile ranges (IQRs) and compared using the Mann–Whitney U test. OS and RFS were calculated using the Kaplan–Meier method and compared using log-rank test. Significance was set at P value < 0.05. All statistical analyses were conducted using SPSS software (SPSS Inc., Chicago, USA, version 19).
Results
Baseline Characteristics
Among 127 patients with NENs at the terminal ileum or cecum, median patient age was 57 (IQR 49–64) years, and one-half (n = 62, 51.2%) of individuals were males (Table 1). Most (n = 108, 85%) patients had a tumor located at the distal ileum, whereas 19 (8.7%) patients had tumors in the cecum, and 8 (6.3%) patients had tumors in both the ileum and cecum. A small subset of patients received neoadjuvant (n = 10, 7.9%) or adjuvant (n = 17, 13.4%) therapy. The median size of the largest tumor size was 2.0 (IQR 1.2–2.9) cm; 35 (27.6%) patients had multiple lesions. At the time of surgery, 93 (73.2%) patients underwent a right hemicolectomy, whereas 34 (26.8%) had an ileocecectomy only. Every patient had a lymph node dissection (LND) with a median number of 16 (IQR 12–22) nodes evaluated. A majority (n = 110, 86.6%) of patients had lymph node metastasis (LNM) with a median number of 3 (IQR 2–5) LNM. Of note, 24 (18.9%) patients had distant metastatic disease, which was resected at the same time as removal of the primary tumor; the liver was the most commonly involved distant organ (18/24, 75%). Following surgery, the majority of patients (n = 78, 61.4%) had no complications, while on final pathology most patients had a Grade 1 tumor (n = 65, 51.2%).
Short and Long-Term Outcomes
Baseline clinical characteristics were comparable among patients with ileocecal NENs who underwent right hemicolectomy versus ileocecectomy (Table 1). Specifically, there were no differences in patient age, gender, tumor location, size, or number of NENs at the terminal ileum or cecum. In contrast, patients who underwent hemicolectomy had more lymph nodes evaluated versus patients who had an ileocecectomy only (median, 18 vs. 14, P = 0.004), although the incidence of LNM were similar between the two (LNM, 84.9% vs. 91.2%, P = 0.76). In addition, while hemicolectomy was associated with increased operation time and intraoperative blood loss than ileocecectomy only (both P < 0.05), there was no difference in the incidence and severity of postoperative morbidity (both P > 0.05) (Table 1).
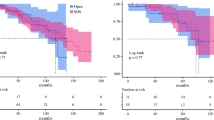
With a median follow-up of 40.6 (21.1–85.4) months, median, 3-, 5-, and 10-year survival among the entire cohort was 138.6 months, 94.3%, 87.7%, and 65.3%, respectively. Of note, patients who underwent formal right hemicolectomy versus ileocecectomy had a similar OS (median OS, 101.9 vs. 144.5 months, P = 0.44) and RFS (median RFS, 70.3 vs. not attained, P = 0.80), respectively (Fig. 1). Among the 100 patients with no distal metastasis (M0 disease) (Table 2), right hemicolectomy was associated with increased number of lymph nodes harvested (17 vs. 14, P = 0.01); however, the number of LNM was similar among patients who underwent right hemi-colectomy versus ileocecectomy, respectively (3 vs. 4, P = 0.95). Patients with M0 disease who underwent ileocecectomy (n = 30) also had similar OS (median OS 101.9 vs. not attained, P = 0.164) and RFS (median RFS, 90.76 vs. 127.9 months, P = 0.26) versus patients who underwent right hemicolectomy (n = 93) (Fig. 2).
Risk Factors Associated with OS and RFS
On multivariable analysis, tumor size larger greater than 2 cm was associated with increased risk of death among patients who underwent curative-intent resection for IC-NENs (HR 4.08, 95% CI 1.28–13.04, P = 0.02) (Table 3). In addition, multifocal disease tended to be associated with tumor recurrence after surgery (HR 2.24, 95% CI 0.98–5.13, P = 0.05) (Table 4). Of note, surgical procedure type (i.e., ileocecectomy vs. right hemicolectomy) was not associated with either OS or RFS (all P > 0.1) among these patients (Tables 3 and 4). Most patients (n = 110, 86.6%) with ileocecal NENs had LNM; in fact, only 14 and 3 patients who underwent right hemicolectomy or ileocecectomy had N0 disease, respectively. Among patients with LNM, there was no difference in OS (median OS 101.9 vs. 144.5 months, P = 0.41) or RFS (median RFS 70.26 months vs. not attained, P = 0.56) among patients who underwent ileocecectomy versus right hemicolectomy (Fig. 3). In addition, when stratified by the tumor size, there was no difference in OS or RFS after ileocecectomy versus right hemicolectomy among patients with tumor size ≥ 2 cm (median OS 86.7 vs. 135.5 months, P = 0.929; median RFS 47.7 months vs. not attained, P = 0.500) or among patients with tumor size < 2 cm (median OS 101.9 months vs. not attained, P = 0.112; median RFS: not attained vs. not attained, P = 0.866).
Discussion
According to the NCCN guidelines, resection of distal ileal carcinomas should involve a right hemicolectomy with at least 5–10 cm margins on either side of the tumor.3 In contrast, the standard surgical procedure for IC-NENs remains undefined.4 As such, the current study was important because we demonstrated that patients with NENs originating from the terminal ileum and/or cecum generally had comparable outcomes following either formal right hemicolectomy or ileocecectomy. Interestingly, while right hemicolectomy was associated with a higher number of lymph nodes harvested than ileocecectomy (median, 18 vs. 14), the incidence (84.9% vs. 91.2%) and number of LNM (median, 3 vs. 4) were no different among patients regardless of procedure type. Right hemicolectomy was, however, associated with an increased operative time and intraoperative blood loss than ileocecectomy—although the incidence and severity of postoperative complications were similar. The presence of LNM was very common among patients with IC-NENs, yet 5-year overall survival was very good at almost 90% regardless of nodal status or procedure type.
Clinical guidelines for patients with IC-NENs are somewhat ambiguous relative to the extent of surgical resection needed to achieve an “optimal” oncological outcome.3 To date, there has been more attention focused on the management of appendiceal NENs. Specifically, according to NCCN guidelines, simple appendectomy for appendiceal NENs less than 2 cm is appropriate as metastasis to the nodal basins is uncommon.3,15 In contrast, a right hemicolectomy should be considered for appendiceal NENs greater than 2 cm.3,15 Despite these traditional recommendations, there is growing evidence to suggest that an appendectomy—and not a formal right colectomy—may be sufficient even for patients with appendiceal NENs measuring over 2 cm.11,16,17,18,19 Specifically, several studies have reported no difference in long-term survival of patients after appendectomy versus right hemicolectomy for appendiceal NENs; right colectomy was, however, associated with increased operation time, blood loss, length of stay, as well as postoperative morbidity.11,16,17,18,19 In addition, in a recent study on low-grade appendiceal mucinous adenocarcinoma (LAMA), Nasseri et al. noted that formal right hemicolectomy did not improve clinical outcomes versus segmental colectomy including ileocecectomy.20 Data in the current study expanded on this previous work and similarly noted that patients with IC-NENs had no differences in short- or long-term outcomes following formal right hemicolectomy versus ileocecectomy. Specifically, the risk of post-operative complications and 5-year survival were comparable among patients with IC-NENs following formal right hemicolectomy versus ileocecectomy. Furthermore, on multivariate and stratified analyses, patients with IC-NENs < 2 cm and ≥ 2 cm had comparable outcomes after right hemicolectomy versus ileocecectomy.
Part of the traditional rationale for a formal colon resection to treat gastrointestinal cancers has been to achieve an “adequate” lymphadenectomy to stage patients. In particular, formal right hemicolectomy for adenocarcinoma should involve dissection of the nodal basin dictated by anatomic vascular/lymphatic drainage patterns so as to provide tumor staging information and mitigate the risk of recurrence.21 Of note, there were 5 patients with enlarged lymph nodes at or near the origin of the ileocecal pedicle on preoperative imaging reports; these patients all underwent formal right hemicolectomy. In the current study, perhaps not surprisingly, we noted that patients with IC-NENs who underwent right hemicolectomy had a higher median number of harvested nodes than individuals who had an ileocecectomy (median, 18 vs. 14, respectively; P = 0.004). However, the incidence of LNM was similar with a very high proportion of nodal disease among patients in both right hemicolectomy and ileocecectomy cohorts (LNM, 84.9% vs. 91.2%, P = 0.76). As such, the higher number of retrieved lymph nodes associated with right hemicolectomy did not translate into a higher detection of LNM, nor a better survival outcome. While regional LNM may be associated with a worse prognosis,22,23 the long-term survival of patients with IC-NENs was very good regardless of lymph node status. In particular, several previous studies have demonstrated that gastrointestinal NENs often have an indolent biological behavior even in the setting of LNM.22,24 While LNM may be present along central vascular structures, data from the current study suggest that LNM often were present along the distal mesentery and near the primary tumor. In turn, ileocecectomy may be adequate to stage patients relative to nodal status, as well as provide a survival benefit comparable to a more extensive right hemicolectomy.
Several limitations should be considered when interpreting results of the current study. As with all retrospective studies, there was undoubtedly some selection bias related to the choice of patients for surgery, as well as choice of right hemicolectomy versus ileocecectomy. Moreover, while the use of a multi-institution database increased sample size and generalizability of the results, this may have led to some heterogeneity in treatment choices among the centers. Despite the use of a large multi-institution dataset, the relatively small sample size may have been the reason for the lack of statistically significant differences in some outcomes among patients who underwent ileocecectomy versus right hemicolectomy (i.e., type II error). Assessing “true” differences in long-term outcome can be challenging in diseases with a relative indolent biological behavior and a long natural history such as IC-NEN. In addition, only 33 patients underwent a totally laparoscopic surgical procedure. With increasing adoption of minimally invasive approaches, the impact of laparoscopic and robot assisted surgery in the treatment of IC-NENs should be further analyzed. Finally, given that the dataset spanned 17 years, evolution in the standard of care, use of adjuvant therapy, and/or surveillance may have impacted our findings.
In summary, ileocecectomy had similar long-term outcomes versus right hemicolectomy in treatment of IC-NENs, despite a difference in the lymph node harvest. While operative time and blood loss were higher among patients who had a right hemicolectomy versus ileocecectomy, the overall incidence of postoperative complications and 5-year survival were comparable.
References
Dasari A, Shen C, Halperin D, et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017;3:1335-1342.
Kacmaz E, Klumpen HJ, Bemelman WA, Nieveen van Dijkum EJM, Engelsman AF, Tanis PJ. Evaluating Nationwide Application of Minimally Invasive Surgery for Treatment of Small Bowel Neuroendocrine Neoplasms. World J Surg. 2021;45:2463-2470.
Benson AB, Venook AP, Al-Hawary MM, et al. Small Bowel Adenocarcinoma, Version 1.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2019;17:1109-1133.
Shah MH, Goldner WS, Benson AB, et al. Neuroendocrine and Adrenal Tumors, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw. 2021;19:839-868.
Boudreaux JP, Klimstra DS, Hassan MM, et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: well-differentiated neuroendocrine tumors of the Jejunum, Ileum, Appendix, and Cecum. Pancreas. 2010;39:753-766.
Salazar R, Wiedenmann B, Rindi G, Ruszniewski P. ENETS 2011 Consensus Guidelines for the Management of Patients with Digestive Neuroendocrine Tumors: an update. Neuroendocrinology. 2012;95:71-73.
Pedrazzani C, Conti C, Valdegamberi A, et al. Is Laparoscopic CME Right Hemicolectomy an Optimal Indication for NET of the Right Colon and Terminal Ileum? J Gastrointest Surg. 2021;25:333-336.
Broder MS, Cai B, Chang E, Neary MP. Epidemiology of Gastrointestinal Neuroendocrine Tumors in a U.S. Commercially Insured Population. Endocr Pract. 2017;23:1210-1216.
Kulke MH, Shah MH, Benson AB, 3rd, et al. Neuroendocrine tumors, version 1.2015. J Natl Compr Canc Netw. 2015;13:78-108.
Pape UF, Perren A, Niederle B, et al. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix including goblet cell carcinomas. Neuroendocrinology. 2012;95:135-156.
Crown A, Simianu VV, Kennecke H, et al. Appendiceal Neuroendocrine Tumors: Does Colon Resection Improve Outcomes? J Gastrointest Surg. 2020;24:2121-2126.
Mehrvarz Sarshekeh A, Advani S, Halperin DM, et al. Regional lymph node involvement and outcomes in appendiceal neuroendocrine tumors: a SEER database analysis. Oncotarget. 2017;8:99541-99551.
Zhang XF, Xue F, Wu Z, et al. (2020) Development and Validation of a Modified Eighth AJCC Staging System for Primary Pancreatic Neuroendocrine Tumors. Ann Surg
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196.
Ricci C, Ingaldi C, Alberici L, et al. Histopathological diagnosis of appendiceal neuroendocrine neoplasms: when to perform a right hemicolectomy? A systematic review and meta-analysis. Endocrine. 2019;66:460-466.
Alabraba E, Pritchard DM, Griffin R, et al. The impact of lymph node metastases and right hemicolectomy on outcomes in appendiceal neuroendocrine tumours (aNETs). Eur J Surg Oncol. 2021;47:1332-1338.
Holmager P, Willemoe GL, Nielsen K, et al. Neuroendocrine neoplasms of the appendix: Characterization of 335 patients referred to the Copenhagen NET Center of Excellence. Eur J Surg Oncol. 2021;47:1357-1363.
Rault-Petit B, Do Cao C, Guyetant S, et al. Current Management and Predictive Factors of Lymph Node Metastasis of Appendix Neuroendocrine Tumors: A National Study from the French Group of Endocrine Tumors (GTE). Ann Surg. 2019;270:165-171.
Pape UF, Niederle B, Costa F, et al. ENETS Consensus Guidelines for Neuroendocrine Neoplasms of the Appendix (Excluding Goblet Cell Carcinomas). Neuroendocrinology. 2016;103:144-152.
Nasseri YY, Zhu R, Sutanto C, et al. Role of right hemicolectomy in patients with low-grade appendiceal mucinous adenocarcinoma. Am J Surg. 2019;218:1239-1243.
Xu L, Su X, He Z, et al. Short-term outcomes of complete mesocolic excision versus D2 dissection in patients undergoing laparoscopic colectomy for right colon cancer (RELARC): a randomised, controlled, phase 3, superiority trial. Lancet Oncol. 2021;22:391-401.
Kim MK, Warner RR, Ward SC, et al. Prognostic significance of lymph node metastases in small intestinal neuroendocrine tumors. Neuroendocrinology. 2015;101:58-65.
Zaidi MY, Lopez-Aguiar AG, Dillhoff M, et al. Prognostic Role of Lymph Node Positivity and Number of Lymph Nodes Needed for Accurately Staging Small-Bowel Neuroendocrine Tumors. JAMA Surg. 2019;154:134-140.
Chi W, Warner RRP, Chan DL, et al. Long-term Outcomes of Gastroenteropancreatic Neuroendocrine Tumors. Pancreas. 2018;47:321-325.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, MX., Lopez-Aguiar, A.G., Poultsides, G. et al. Surgical Treatment of Neuroendocrine Tumors of the Terminal Ileum or Cecum: Ileocecectomy Versus Right Hemicolectomy. J Gastrointest Surg 26, 1266–1274 (2022). https://doi.org/10.1007/s11605-022-05269-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-022-05269-1