Abstract
Background
Long-term complications following pancreatoduodenectomy (PD) can significantly impact quality of life and healthcare utilization. Most reports focus on short-term (within 90 days) PD outcomes; however, the incidence and risk factors for long-term complications (> 90 days) remain to be evaluated. We sought to identify the incidence, outcomes, and risk factors for long-term complications post-PD.
Methods
All PD survivors between 2010 and 2017 were identified from a single-institutional database. Long-term complications (> 90 days post-PD and not resulting from cancer recurrence), including biliary stricture, cholangitis, pancreatitis, peptic ulcer, small bowel obstruction, and incisional hernia, were identified. Logistic regression was used to identify perioperative predictors of long-term complications.
Results
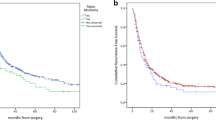
Of 906 PDs, 628 long-term survivors met criteria for analysis (mean age of 65.3 years, 47% female). Median follow-up and overall survival were 51.1 months (95% CI 47.6, 55.7) and 68.5 months (95% CI 57.9, 81.4), respectively. A total of 198 (31.5%) experienced at least one long-term complication. Complications included incisional hernia (17.7%), biliary stricture or cholangitis (8.0%), pancreatitis (5.7%), small bowel obstruction (4.3%), and peptic ulcer (3.2%). In total, 108 (17.2%) of the complications required an intervention, nearly half of which were surgical. On multivariable analysis, several predictors of long-term complications were identified: obesity (BMI ≥ 30 kg/m2), postoperative wound infection, prolonged index length of stay, readmission (< 90 days), operative approach (open vs. robotic), and pylorus-preservation.
Conclusion
Long-term complications occur in nearly a third of PDs and nearly one-fifth of all PDs require re-intervention. Several modifiable predictors of long-term complications were identified.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatoduodenectomy (PD) is a complex procedure used to treat benign and malignant periampullary lesions. Mortality after PD has fallen to 2.7%1 in recent decades; however, postoperative morbidity remains as high as 40%, even at high-volume centers.2 Critical short-term (30- and 90-day) complications, such as pancreatic fistula, delayed gastric emptying, and post-pancreatectomy hemorrhage, have been extensively studied.3,4,5 However, the incidence and risk factors associated with late complications (including biliary stricture and cholangitis, pancreatitis, peptic ulcer disease, small bowel obstruction, and incisional hernia) remain to be fully evaluated. Late-onset complications can significantly impact quality of life and pose a significant burden on healthcare resources due to the need for hospital readmission, radiographic imaging, and interventional procedures.
Data on long-term surgical complications has also become increasingly important as the utilization of PD increases for both benign and premalignant diseases, including neuroendocrine tumors, mucinous cystic lesions, and chronic pancreatitis—conditions in which long-term survival is anticipated.6,7,8,9 Furthermore, evidence suggests that 5-year survival for resected pancreatic adenocarcinoma (PDA) has incrementally improved over time as a result of more effective adjuvant treatment, use of neoadjuvant therapy, and an increase in margin-negative resections over the last two decades.10,11,12,13,14,15,16,17,18 Thus, the population of long-term survivors post-PD is growing.
Considering these trends in survival, as well as the impact of PD on quality of life and healthcare cost, recent studies have sought to determine the long-term consequences of PD. 19,20,21,22 Whereas some reports have focused on a specific surgical complication (e.g., biliary stricture) or the impact of a surgical modification of PD (e.g., pylorus-preservation), none has systematically evaluated the incidence and risk factors for several late-onset complications followed over an extended time-period. Thus, the aim of this study was to comprehensively document and analyze the incidence and risk factors for late adverse surgical sequelae among long-term survivors of PD at a single academic center. We hypothesized that several perioperative variables would be associated with the occurrence of late complications following PD.
Methods
Study Design, Data Collection, and Definitions
This was an observational study utilizing a prospectively maintained institutional database of all consecutive PDs performed between January 2010 and May 2017, for benign or malignant indications, at the University of Pittsburgh Medical Center (UPMC). This study was approved by the Institutional Review Board of the University of Pittsburgh (PRO15040497).
Long-term complications were defined as those occurring greater than 90 days post-PD, in the absence of cancer recurrence based on follow-up imaging (CT, MRI, PET), and requiring admission or percutaneous, endoscopic, or surgical intervention. Long-term complications included biliary stricture, cholangitis, pancreatitis, peptic ulcer disease, small bowel obstruction (SBO), and incisional hernia. Biliary stricture was identified by radiographic evidence of anastomotic narrowing at the hepaticojejunostomy in the context of elevated LFTs or symptoms of cholangitis, while cholangitis was defined by the classic triad of abdominal pain, fever, and jaundice, or by elevated LFTs and radiographic evidence of biliary dilation when only two of three symptoms were present. Pancreatitis was diagnosed in a patient with acute epigastric pain, serum lipase elevated greater than three times the normal upper limit, and radiographic evidence of pancreatitis. Peptic ulcers were diagnosed by endoscopic imaging in the context of abdominal pain or upper gastrointestinal (GI) bleeding. SBO was confirmed by radiographic imaging, while incisional hernia was identified on physical examination. Interventions (endoscopic, percutaneous, or surgical) were recorded if they occurred in the context of any of these complications.
Demographic and clinical information were collected from the institutional database and analyzed for factors associated with long-term complications. Preoperative variables included age, sex, body mass index (BMI), Charlson comorbidity index (CCI), prior abdominal surgery, cardiovascular comorbidity, preoperative albumin and bilirubin, pathologic diagnosis, and neoadjuvant therapy. Operative variables included total operation time (OT), estimated blood loss (EBL), pancreatic duct size and texture, pylorus-preservation (PPPD) versus pylorus resection (PRPD), vascular resection, and utilization of open (OPD) or robotic (RPD) approach. Postoperative 90-day outcome variables included clinically relevant postoperative pancreatic fistula (CR-POPF: grade B or C) according to the International Study Group of Pancreatic Fistula (ISGPF) criteria, delayed gastric emptying (DGE), wound infection, Clavien-Dindo complication rate, length of hospital stay (LOS), readmission, reoperation, recurrence, and death. Survival time was calculated from the date of surgery until the date of death from any cause.
Operative Details
During the study time-period, seven surgeons performed the majority of PDs at this institution. RPD was the preferred approach for three surgeons, with the remaining surgeons performing OPD exclusively. Those surgeons who preferred RPD opted for OPD in the following circumstances: (1) need for vascular reconstruction, or (2) prior gastrointestinal surgery involving gastric or small bowel resection and reconstruction and/or resulted in extensive intraabdominal adhesions. For OPD, surgeons utilized either transverse or midline laparotomy. For RPD, 6 ports were used (4 upper robotic and 2 lower laparoscopic), of which one laparoscopic port (12 mm left lower quadrant) was enlarged to 4–5 cm transversely for specimen extraction. All gastrojejunostomies were Billroth II reconstructions, and all pancreatic anastomoses were pancreatojejunostomies.
Statistical Analysis
The distributional characteristics for variables were checked for normalcy. Continuous variable data were presented as mean ± standard deviation, or median and interquartile range (IQR). Categorical data were summarized using frequency and percentage. Student’s t test was used to compare normally distributed continuous variables between groups, and the Wilcoxon rank-sum test was used for non-normally distributed continuous variables. The chi-squared or Fisher exact test was used to compare categorical variables between groups.
To account for cancer-related death as a confounding and competing event for long-term surgical complications, only patients with survival or follow-up greater than 17.3 months with absence of recurrence on radiographic imaging were analyzed for predictors of complications. Thus, patients with periampullary cancer were excluded from analysis if they died prior to 17.3 months after their operative date. Moreover, we excluded any patient from analysis (whether benign or malignant) who were lost to follow-up prior to 17.3 months after their operative date in order to avoid any selection bias. The cutoff of 17.3 months was selected based on the lower limit of the 95% confidence interval for survival in the ESPAC (95% CI 17.3, 22.0 months) and CONKO (95% CI 18.5, 27.2) trials—the two largest and contemporaneous randomized controlled trials of adjuvant chemotherapy in resected pancreatic cancer.13,23
Three predictive models were constructed for the following outcomes: (1) any complications; (2) composite outcome of biliary stricture, cholangitis, and pancreatitis; and (3) composite outcome of incisional hernia and SBO. Biliary stricture, cholangitis, and pancreatitis were combined into a composite outcome due to similarities in their genesis (anastomotic failure or stasis within the pancreaticobiliary limb) and treatment (percutaneous/endoscopic or surgical revision of the anastomosis). Similarly, incisional hernia and SBO were combined into a composite outcome due to their similar management (conservative or surgical exploration/repair).
Univariable and multivariable analyses were performed using logistic regression to indicate clinical and technical factors associated with long-term complications. Backward stepwise selection and Akaike information criterion were applied in building different multivariable models. All statistical tests were two-tailed, and p values < 0.05 were considered statistically significant. Statistical analyses were performed using STATA, version 13 (Stata Corporation, College Station, TX).
Results
Descriptive Statistics of the Overall Cohort
Of 906 PDs performed within the study period, 628 (69.3%) patients had survival or follow-up time greater than 17.3 months and were analyzed for long-term surgical complications (Fig. 1). Table 1 lists the demographic and clinical variables for the analyzed cohort. The mean age was 65.3 and 47.3% were female. In total, 443 (70.5%) had periampullary adenocarcinoma (48.9% PDA, 10.8% ampullary cancer, 5.7% cholangiocarcinoma, 5.1% duodenal cancer) and 185 (29.5%) had indolent malignancies or benign lesions (10.7% mucinous lesion, 8.1% neuroendocrine tumor, 3.5% chronic pancreatitis, 7.2% other). A total of 306 patients (48.7%) underwent robotic PD, 115 (18.3%) had PPPD, and 105 (16.7%) required vascular resection. Of the 322 OPD patients, 41 (12.7%) underwent a transverse laparotomy.
Short-term (< 90-day) complications included a 12.9% CR-POPF (grade B or C) rate, a 19.3% wound infection rate, and a 30.6% readmission rate. Median follow-up for the entire cohort was 51.1 months (95% CI 47.6, 55.7), while median overall survival was 68.5 months (95% CI 57.9, 81.4). Notably, pylorus-preservation was more common in patients with indolent/benign pathology (27.6% vs. 14.5% in periampullary cancers, p < 0.001). Furthermore, pylorus-preservation was associated with incidence of CR-POPF (23.5% in PPPD vs. 10.5% in pylorus-resecting PD, p < 0.001).
Incidence of Long-Term Surgical Complications and Re-Intervention
A total of 198 patients (31.5%) experienced at least one long-term complication. The incidence and median time-to-event for specific complications were as follows: biliary stricture or cholangitis = 50 patients (8.0%) at 401 days (IQR 213-952), pancreatitis = 36 patients (5.7%) at 456 days (IQR 239-771), peptic ulcer = 20 patients (3.2%) at 610 days (IQR 219-1274), SBO = 27 patients (4.3%) at 512 days (IQR 171-1052), and incisional hernia = 111 patients (17.7%) at 334 days (IQR 232-608). The majority of complications (97.5%) occurred less than 5 years post-PD, with only five (2.5%) complications occurring after 5 years.
There were 133 total interventions for long-term complications. At least one re-intervention was required in 108 (17.2%) patients, of which 14 (2.2%) required more than one intervention. Of the total interventions, 21 were percutaneous, 46 were endoscopic, and 66 were surgical. All 21 percutaneous interventions were percutaneous transhepatic cholangiographies (PTC) for biliary stricture. Among the endoscopic interventions, 21 were endoscopic retrograde cholangiopancreatography (ERCP) for biliary complications, 20 underwent esophagogastroduodenoscopy (EGD) for peptic ulcers, and 5 had upper GI endoscopies for SBO. Among the surgical interventions, 54 were incisional hernia repairs, 8 were exploratory laparotomies for SBO, and 4 were hepaticojejunostomy revisions.
Predictive Models for Long-Term Surgical Outcomes
Tables 2, 3, and 4 depict the association of demographic, clinical, and perioperative variables with the incidence of long-term (> 90-day) complications. On multivariable analysis for any complication (Table 2), BMI > 30 kg/m2 (OR 1.48; 95% CI 1.02, 2.15; p = 0.039), a postoperative wound infection during the index admission (OR 2.34; 95% CI 1.54, 3.59; p < 0.001), readmission < 90-day post-PD (OR 1.52; 95% CI 1.04, 2.22; p = 0.028), and pylorus-preservation (OR 2.27; 95% CI 1.48, 3.48; p < 0.001) were all significant predictors of any complication.
On multivariable analysis for the composite outcome of biliary stricture, cholangitis, and pancreatitis (Table 3), readmission < 90-day post-PD (OR 2.28; 95% CI 1.38, 3.76; p = 0.001) and pylorus-preservation (OR 2.32; 95% CI 1.33, 4.02; p = 0.003) were both significant predictors, while utilization of neoadjuvant radiotherapy (OR 2.13; 95% CI 0.87, 5.18; p = 0.097) and CR-POPF (OR 1.76; 95% CI 0.95, 3.27; p = 0.074) trended toward significance.
The robotic approach was associated with reduced incidence of incisional hernia (13.1% vs 22.1%, p = 0.003) and SBO (2.6% vs 4.3%, p = 0.042) compared with the open approach. On multivariable analysis for predictors of incisional hernia or SBO (Table 4), BMI ≥ 30 kg/m2 (OR 1.67; 95% CI 1.09, 2.55; p = 0.018), pylorus-preservation (OR 1.83; 95% CI 1.12, 2.97; p = 0.015), open surgical approach (OR 1.62; 95% CI 1.07, 2.47; p = 0.024), prolonged length of hospital stay for the index admission (OR 1.04; 95% CI 1.01, 1.07; p = 0.008), and postoperative wound infection during index admission (OR 2.91; 95% CI 1.84, 4.60; p < 0.001) were all significant predictors of the composite outcome of incisional hernia and SBO.
Discussion
While perioperative mortality for PD has declined to historic lows, the incidence of postoperative morbidity remains high. Most studies have focused on short-term complications occurring within 90 days. This study sought to document the incidence, timing, and risk factors associated with long-term complications following PD. Of 628 long-term survivors after PD, nearly a third experienced at least one complication and one-fifth required an intervention. The majority (97.5%) of complications occurred within 5 years after PD, suggesting that the risk of developing complications decreases after this important milestone. On multivariable analysis (MVA), several factors were associated with long-term complications. Those included patient-related variables such as BMI ≥ 30 kg/m2, surgical factors such as pylorus-preservation and operative approach (open vs. robotic), and immediate postoperative outcomes such as wound infection, prolonged LOS, and readmission.
In this analysis, short-term (90-day) morbidity was associated with the occurrence of long-term complications. Specifically, wound infection, prolonged LOS, and readmission within 90 days post-PD were predictive of the occurrence of a late complication. Although this association may be predictable, it emphasizes the need for continued follow-up for the emergence of late complications in patients with 90-day complications and readmissions. Clinically relevant POPF occurred in 13% of patients and deserves special consideration in the pathogenesis of late complications. While CR-POPF was not significantly associated with long-term outcomes in any of the MVA models, it was associated with all long-term surgical complications on univariable analysis. On MVA, CR-POPF trended (p = 0.074) towards increasing the risk of developing biliary stricture, cholangitis, and pancreatitis. These findings are consistent with the well-documented association of POPF with local and systemic complications, delayed postoperative feeding, increased LOS, superficial and intraabdominal surgical site infections, and pseudoaneurysm and hemorrhage.24,25 Given the strong univariable associations and multivariable trends for increased CR-POPF among long-term complications in the present study, it is likely that CR-POPF adversely affects long-term recovery, especially for those “anastomotic” complications of the pancreaticobiliary limb (biliary stricture, cholangitis, and pancreatitis) which develop long after PD. Thus, reducing CR-POPF remains an important goal.
Interestingly, our study is the first to suggest an association between pylorus-preservation and long-term complications following PD. To date, reports on pylorus-preservation have typically focused on short-term morbidity, especially DGE.26 Data on the impact of pylorus-preservation on rates of DGE is inconsistent, with some studies supporting resection of the pylorus-resection over its preservation,27 and others indicating equivalence.28,29 As such, the debate is likely to continue. Our study however suggests that pylorus-preservation may adversely affect long-term outcomes; on MVA, PPPDs were twice as likely to develop biliary stricture, cholangitis, or pancreatitis as pylorus-resecting PD, an association that was independent of preoperative radiation, early readmission (< 90-day), and CR-POPF.
Several explanations may account for this provocative finding. Recent studies suggest that strictures arising at the biliary-enteric anastomosis range from 2.6 to 4.3%, with cumulative estimates as high as 8.0% for 5-year survivors.22,30,31,32 Cholangitis post-PD has been associated with numerous factors, including preoperative radiation, operative aspects of the hepaticojejunostomy, pancreaticobiliary limb stasis (or afferent limb syndrome), and anastomotic stenosis.30,31,32,33,34 Pancreatitis after PD, on the other hand, is not well studied and while its exact pathophysiological mechanism is undetermined, has been correlated with mechanical obstruction (ductal stricture), increased ductal “hypertension,” and/or reflux of bile or pancreatic juices.35,36,37 Recent studies suggest that pancreaticojejunostomy stenosis is a significant late complication after PD, with an incidence ranging from 2.0 to 11.3%, and is highly associated with postoperative (recurrent) pancreatitis.38,39,40 Unfortunately, since magnetic resonance cholangiopancreatography (MRCP) was not routinely performed in the context of pancreatitis at our institution, data concerning pancreatic duct stricture was unreliable in this cohort of PDs. Nevertheless, the present study identified long-term onset (> 90 day) of pancreatitis after PD in 5.7% of patients, a non-negligible proportion of patients that requires further research.
While prior studies indicate that cholangitis and pancreatitis arise in the context of mechanical obstruction (e.g., anastomotic stenosis), intestinal stasis, and chronic inflammation, the present study suggests that pylorus-preservation may contribute to this adverse physiological milieu. During pylorus-preserving PD, the right gastric, gastroduodenal, and right epiploic arteries are ligated, rendering the pylorus relatively devascularized, potentially leading to ischemia and stricture in the long run.41,42 Though speculative, the duodenojejunal anastomosis may thicken and narrow over time, even if not developing into a full-blown stricture that causes gastric outlet obstruction. This may lead to stasis of bile, pancreatic enzymes, and microbiota in the pancreaticobiliary limb, which in turn leads to ductal inflammation, anastomotic strictures, and (recurrent) cholangitis or pancreatitis. On the other hand, this study does not address potential benefits of PPPD, namely, preservation of gastric volume, capacity and antral motor function, decreased bile reflux, and avoidance of dumping syndrome, and other post gastrectomy sequelae. Furthermore, we did not examine important longitudinal parameters such as nutritional state and weight loss since this data was not as thoroughly captured. Such metrics must be taken into consideration when evaluating the long-term outcomes of pylorus-preservation.
The association between pylorus-preservation and incisional hernia/SBO in this study is difficult to account for. Perhaps, since pylorus-preservation was more commonly performed in patients without PDA, and since PDA is protective against CR-POPF, it is possible that pylorus-preservation is a surrogate for CR-POPF in the case of incisional hernias. CR-POPF would therefore impact short-term wound healing and subsequently incisional hernia rates in the long term. Despite these speculations, the findings of the present study concerning long-term complications should be considered in the continuing debate about pylorus-preservation.
Incisional hernia and SBO are significant long-term sequelae after abdominal surgery. In the current study, incisional hernias occurred in 17.7%, while SBO occurred in 4.3%. Incisional hernia has been associated with obesity, postoperative wound infection, smoking, technique of operative incision closure, and surgical approach (minimally invasive being protective compared with laparotomy) in prior reports.43,44,45,46,47,48,49,50 Similarly, we found BMI ≥ 30 kg/m2, wound infection, and increasing LOS to be associated with incisional hernia on MVA. Notably, on MVA, an open PD was associated with a near twofold risk of developing incisional hernia or SBO compared with RPD. Prior studies suggest that the incidence of incisional hernia and SBO is reduced in patients undergoing laparoscopic surgery as compared with that in those undergoing laparotomy, especially for bariatric and colorectal resection.47,48,49,50 However, the current study is the first to document such a benefit for PD.
Despite these results, there are important limitations to this analysis. First, this study utilized existing observational data; hence, our cohorts may be confounded by selection bias. This risk of selection bias is notably evident for surgical approach because RPD-preferring surgeons opted for OPD in complex cases that required vascular reconstruction or cases with extensive prior gastrointestinal surgery. Second, this study analyzed longitudinal data, which entails shifting practice patterns, evolving surgeon experience, and varying follow-up times. Third, this series of PDs was performed by a small group of surgeons in a single, high-volume institution, thereby limiting the generalizability of the findings. As such, these results are hypothesis-generating and require further validation. Despite these limitations, this is the first study to identify the incidence, outcomes, and risk factors for several long-term complications post-PD.
Conclusion
In the largest cohort study examining long-term sequelae post-PD, surgical complications occurred in nearly one-third of patients, with nearly half of those requiring re-intervention. Several modifiable predictors of long-term complications were identified, notably obesity, pylorus-preserving PD, surgical approach (open vs. robotic), and early postoperative morbidity. These findings may serve as a useful adjunct in shared decision-making for patients and surgeons alike, while serving to improve long-term morbidity and quality of life following PD.
References
Gleeson EM, Shaikh MF, Shewokis PA, et al. WHipple-ABACUS, a simple, validated risk score for 30-day mortality after pancreaticoduodenectomy developed using the ACS-NSQIP database. Surgery. 2016 Nov;160(5):1279-1287.
Winter JM, Cameron JL, Campbell KA, et al. 1423 pancreaticoduodenectomies for pancreatic cancer: A single-institution experience. J Gastrointest Surg. 2006;10(9):1199-1210; discussion 1210-1191.
Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13.
Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2007;142:761-768.
Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20-25.
Diener MK, Hüttner FJ, Kieser M, et al. Partial pancreatoduodenectomy versus duodenum-preserving pancreatic head resection in chronic pancreatitis: the multicentre, randomised, controlled, double-blind ChroPac trial. Lancet. 2017 Sep 9;390(10099):1027-1037.
Balcom JH, Rattner DW, Warshaw AL, et al. Ten-year experience with 733 pancreatic resections: changing indications, older patients, and decreasing length of hospitalization. Arch Surg. 2001;136:391–398.
Fernandez-del Castillo C, Morales-Oyarvide V, McGrath D, et al. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery. 2012;152:S56 – 63.
Winter JM, Cameron JL, Lillemoe KD, et al. Periampullary and pancreatic incidentaloma: a single institution’s experience with an increasingly common diagnosis. Ann Surg. 2006;243:673–680.
Kleeff J, Korc M, Apte M, et al. Pancreatic Cancer. Nat Rev Dis Primers. 2016 Apr 21;2:16022.
Cameron JL and He J. Two Thousand Consecutive Pancreaticoduodenectomies. J Am Coll Surg. 2015 Apr;220(4):530-6.
Hartwig W, Hackert T, Hinz U, et al. Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg. 2011 Aug;254(2):311-9.
Neoptolemos JP, Stocken DD, Tudur Smith C, et al. Adjuvant 5-fluorouracil and folinic acid vs observation for pancreatic cancer: composite data from the ESPAC-1 and -3(v1) trials. Br J Cancer. 2009 Jan 27;100(2):246-50.
Neoptolemos JP, Palmer DH, Ghaneh P, et al. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017 Mar 11;389(10073):1011-1024.
Bockhorn M, Uzunoglu FG, Adham M, et al. Borderline resectable pancreatic cancer: a consensus statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery. 2014 Jun;155(6):977-88.
Lopez NE, Prendergast C, Lowy AM. Borderline resectable pancreatic cancer: Definitions and management. World J Gastroenterol. 2014 Aug 21; 20(31): 10740–10751.
Stokes JB, Nolan NJ, Stelow EB, et al. Preoperative capecitabine and concurrent radiation for borderline resectable pancreatic cancer. Ann Surg Oncol. 2011 Mar;18(3):619-27.
McClaine RJ, Lowy AM, Sussman JJ, et al. Neoadjuvant therapy may lead to successful surgical resection and improved survival in patients with borderline resectable pancreatic cancer. HPB (Oxford). 2010 Feb; 12(1): 73–79.
Fong ZV, Alvino DM, Castillo CF, et al. Health-related Quality of Life and Functional Outcomes in 5-year Survivors After Pancreaticoduodenectomy. Ann Surg. 2017 Oct;266(4):685-692.
Huang JJ, Yea CJ, Sohn TA, et al. Quality of Life and Outcomes After Pancreaticoduodenectomy. Ann Surg. 2000 Jun; 231(6): 890–898.
Klaiber U, Probst P, Hüttner FJ, et al. Randomized Trial of Pylorus-Preserving vs. Pylorus-Resecting Pancreatoduodenectomy: Long-Term Morbidity and Quality of Life. J Gastrointest Surg. 2019 Jan 22.
House MG, Cameron JL, Schulick RD, et al. Incidence and outcome of biliary strictures after pancreaticoduodenectomy. Ann Surg. 2006;243(5):571-576; discussion 576-578.
Oettle H, Neuhaus P, Hochhaus A, et al. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013 Oct 9;310(14):1473-81.
Veillette G, Dominguez I, Ferrone C, et al. Implications and management of pancreatic fistulas following pancreaticoduodenectomy: the Massachusetts General Hospital experience. Arch Surg. 2008 May;143(5):476-81.
Vin Y, Sima CS, Getrajdman GI, et al. Management and outcomes of postpancreatectomy fistula, leak, and abscess: results of 908 patients resected at a single institution between 2000 and 2005. J Am Coll Surg. 2008 Oct;207(4):490-8.
Klaiber U, Probst P, Büchler MW, et al. Pylorus preservation pancreatectomy or not. Transl Gastroenterol Hepatol. 2017; 2: 100.
Hackert T, Hinz U, Hartwig W, et al. Pylorus resection in partial pancreaticoduodenectomy: impact on delayed gastric emptying. Am J Surg. 2013 Sep;206(3):296-9.
Hackert T, Probst P, Knebel P, et al. Pylorus Resection Does Not Reduce Delayed Gastric Emptying After Partial Pancreatoduodenectomy: A Blinded Randomized Controlled Trial (PROPP Study, DRKS00004191). Ann Surg. 2018 Jun;267(6):1021-1027.
Klaiber U, Probst P, Strobel O, et al. Meta-analysis of delayed gastric emptying after pylorus-preserving versus pylorus-resecting pancreatoduodenectomy. Br J Surg. 2018 Mar;105(4):339-349.
Reid-Lombardo KM, Ramos-De la Medina A, Thomsen K, Harmsen WS, Farnell MB. Long-term anastomotic complications after pancreaticoduodenectomy for benign diseases. J Gastrointest Surg. 2007;11(12):1704-1711.
Duconseil P, Turrini O, Ewald J, Berdah SV, Moutardier V, Delpero JR. Biliary complications after pancreaticoduodenectomy: skinny bile ducts are surgeons' enemies. World J Surg. 2014;38(11):2946-2951.
Prawdzik C, Belyaev O, Chromik AM, Uhl W, Herzog T. Surgical revision of hepaticojejunostomy strictures after pancreatectomy. Langenbecks Arch Surg. 2015;400(1):67-75.
Ducrotte P, Peillon C, Guillemot F, et al. Could recurrent cholangitis after Roux-en-Y hepaticojejunostomy be explained by motor intestinal anomalies? A manometric study. Am J Gastroenterol. 1991 Sep;86(9):1255-8.
Le Blanc-Louvry I, Ducrotte P, Manouvrier JL, et al. Motility of the Roux-en-Y hepaticojejunostomy in asymptomatic patients. Am J Gastroenterol. 1999 Sep;94(9):2501-8.
Steer ML, Waxman I, Freedman S. Chronic pancreatitis. N Engl J Med. 1995 Jun 1;332(22):1482-90.
Opie EL, Meakins JC. Data concerning the etiology and pathology of hemorrhagic necrosis of the pancreas (acute hemorrhagic pancreatitis). J Exp Med. 1909 Jul 17; 11(4):561-78.
Lerch MM, Saluja AK, Runzi M, et al. Pancreatic duct obstruction triggers acute necrotizing pancreatitis in the opossum. Gastroenterology. 1993 Mar;104(3):853-61.
Morgan KA, Fontenot BB, Harvey NR, et al. Revision of anastomotic stenosis after pancreatic head resection for chronic pancreatitis: is it futile? HPB (Oxford). 2010 Apr; 12(3): 211–216.
Demirjian AN, Kent TS, Callery MP, et al. The inconsistent nature of symptomatic pancreatico-jejunostomy anastomotic strictures. HPB (Oxford). 2010 Sep; 12(7): 482-487.
Cioffi JL, McDuffie LA, Roch AM, et al. Pancreaticojejunostomy Stricture After Pancreatoduodenectomy: Outcomes After Operative Revision. J Gastrointest Surg. 2016 Feb;20(2):293-9.
Gauvin JM, Sarmiento JM, Sarr MG. Pylorus-Preserving Pancreaticoduodenectomy With Complete Preservation of the Pyloroduodenal Blood Supply and Innervation. Arch Surg. 2003 Nov;138(11):1261-3.
Kim DK, Hindenburg AA, Sharma SK, et al. Is pylorospasm a cause of delayed gastric emptying after pylorus-preserving pancreaticoduodenectomy? Ann Surg Oncol. 2005 Mar;12(3):222-7.
Hesselink VJ, Luijendijk RW, de Wilt JH, et al. An evaluation of risk factors in incisional hernia recurrence. Surg Gynecol Obstet. 1993 Mar;176(3):228-34.
Sauerland S, Korenkov M, Kleinen T, et al. Obesity is a risk factor for recurrence after incisional hernia repair. Hernia. 2004 Feb;8(1):42-6.
Blatnik JA, Krpata DM, Novitsky YW, et al. Does a history of wound infection predict postoperative surgical site infection after ventral hernia repair? Am J Surg. 2012 Mar;203(3):370-4.
Velijkovic R, Protic M, Gluhovic A, et al. Prospective clinical trial of factors predicting the early development of incisional hernia after midline laparotomy. J Am Coll Surg. 2010 Feb;210(2):210-9.
Reoch J, Mottillo S, Shimony A, et al. Safety of laparoscopic vs open bariatric surgery: a systematic review and meta-analysis. Arch Surg. 2011 Nov;146(11):1314-22.
Kössler-Ebs JB, Grummich K, Jensen K, et al. Incisional Hernia Rates After Laparoscopic or Open Abdominal Surgery-A Systematic Review and Meta-Analysis. World J Surg. 2016 Oct;40(10):2319-30.
Yamada T, Okabayashi K, Hasegawa H, et al. Meta-analysis of the risk of small bowel obstruction following open or laparoscopic colorectal surgery. Br J Surg. 2016 Apr;103(5):493-503.
Klaristenfeld DD, McLemore EC, Li BH, et al. Significant reduction in the incidence of small bowel obstruction and ventral hernia after laparoscopic compared to open segmental colorectal resection. Langenbecks Arch Surg. 2015 May;400(4):505-12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by the Institutional Review Board of the University of Pittsburgh (PRO15040497).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brown, J.A., Zenati, M.S., Simmons, R.L. et al. Long-Term Surgical Complications After Pancreatoduodenectomy: Incidence, Outcomes, and Risk Factors. J Gastrointest Surg 24, 1581–1589 (2020). https://doi.org/10.1007/s11605-020-04641-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04641-3