Abstract
Background
Guidelines recommend colectomy for appendiceal carcinoid tumors larger than 2 cm, but physicians debate whether colectomy would be beneficial in treating smaller tumors. We sought to determine when colectomy confers a survival advantage over appendectomy.
Methods
Appendiceal carcinoid patients in the US Surveillance, Epidemiology, and End Results (SEER) database (1988–2011) were stratified by age group, gender, TNM stage, tumor grade, and race. Kaplan-Meier and logistic regression analyses relating grade, stage, and receipt of colectomy to overall and cancer-specific survival were performed.
Results
Of 817 patients who underwent surgical extirpation of an appendiceal carcinoid, 338 (41%) had appendectomy alone and 479 (59%) had additional colectomy. Surprisingly, patients who underwent colectomy had worse cancer-specific survival (HR 1.98, 95% CI 1.32–2.98, p = 0.001) than those who underwent appendectomy, and colectomy did not confer a survival advantage over appendectomy in any subset analysis including low-grade or high-grade tumors, smaller or larger than 2 cm, or node-positive, non-metastatic tumors. Even when accounting for stage and grade, colectomy was not associated with significantly better survival rates. Furthermore, as colectomy frequency has increased over the last decade, the 5-year survival rate has trended down. The main predictors of cancer-specific mortality in carcinoid patients were high-grade (grades 3–4) and high-stage (node positive or metastatic) tumors.
Conclusions
Survival in patients with carcinoid tumor of the appendix is primarily determined by tumor grade and stage. Our study found no survival advantage to colectomy over appendectomy in a large cohort of patients with the disease. Further investigation is necessary prior to recommending change of practice for patients with appendiceal carcinoid tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carcinoid tumors are the most common tumor of the appendix, accounting for more than half of all appendiceal malignancies and discovered in seven of every 1000 appendectomy specimens.1 The majority of patients with appendiceal carcinoid are asymptomatic, and most tumors are located in the distal third of the appendix where they are unlikely to cause obstruction.2 Appendiceal carcinoid is typically discovered incidentally in an appendectomy specimen. The decision must then be made whether or not to return to the operating room for colectomy for adequate tumor and lymph node resection. The optimal surgical management for appendiceal carcinoid, however, is subject to debate.
Carcinoid tumors are classified histologically based on tumor differentiation and tumor grade.3 Most neuroendocrine tumors fall into four broad histologic categories: well-differentiated, low-grade (G1); well-differentiated, intermediate grade (G2); poorly differentiated, high grade (G3); and anaplastic, high grade (G4). Tumor differentiation and grade often correlate with the mitotic index and Ki-67 proliferation index. Studies have confirmed that increased mitotic rate and high Ki-67 index, and therefore high grade, are associated with a more aggressive clinical course and worse prognosis.4
Currently, treatment modalities are largely directed by TNM staging of the tumor. Current National Comprehensive Cancer Network (NCCN) guidelines recommend simple appendectomy for tumors < 2 cm (T1a and T1b), but that colectomy should be offered to those patients with primary appendiceal carcinoid tumors greater than 2 cm (T2–4). This was initially borne out of literature suggesting a 30% plus risk of lymph node metastases at this size cutoff. This was also supported by recent reviews suggesting that 86% of patients with tumors > 2 cm have lymph node metastases.5,6
The majority of appendiceal carcinoid tumors, however, are < 2 cm in size, and there has been debate as to whether patients with these smaller tumors should have formal colectomy as well. A long-term series from the Mayo Clinic suggests that appendectomy is adequate to treat patients with localized tumors < 2 cm as none of 122 patients with appendiceal carcinoid tumors < 2 cm had local recurrence or metastatic disease; however 80% of the patients in this cohort had tumors < 1 cm in size (T1a).7 Other studies show that lymph node metastases are present in up to 50% of patients with 1 to 2 cm appendiceal carcinoid tumors (T1b), suggesting a more aggressive approach is needed. As such, some studies recommend colectomy even in patients with tumors measuring < 2 cm that are higher grade and have more aggressive histologic features.8,9
The purpose of our study is to compare outcomes of appendiceal carcinoid tumor patients to see if colectomy confers survival advantage over appendectomy, especially in T1 tumors (smaller than 2 cm). In addition, we determined the influence of tumor grade, stage, and surgical treatment (appendectomy versus colectomy) on survival in patients with carcinoid.
Materials and Methods
Subjects and Databases
The data for this analysis was abstracted from the Surveillance, Epidemiology, and End Results (SEER) database (1973-2011). This database is a publicly available cancer registry maintained by the National Cancer Institute that includes approximately 26% of the US population representing Connecticut, Iowa, rural Georgia, Alaska, New Mexico, Greater California, Utah, Hawaii, Kentucky, New Jersey, and Louisiana as well as the metropolitan areas of Detroit, San Francisco-Oakland, Seattle (Puget Sound), Metropolitan Atlanta, Los Angeles, and San Jose-Monterey. Records before 1988 were excluded as the SEER registry did not collect detailed lymph node data from 1973 to 1987.
Inclusion and Exclusion Criteria
We included patients of any age who underwent partial colectomy or appendectomy for histologically confirmed appendiceal carcinoid tumor diagnosed between 1988 and 2011. We incorporated patients with a primary tumor site within the appendix. Patients were included in the analysis if surgery type was coded as appendectomy alone or partial colectomy (with or without prior appendectomy). Patients who received more extensive surgery, namely subtotal/colectomy, total colectomy, total proctocolectomy, or colectomy or coloproctectomy with resection of contiguous organs, were excluded. From henceforth, we will refer to partial colectomy simply as colectomy.
Patients were excluded if the number of nodes examined was blank. Patients were also excluded if they had a cancer diagnosis before 1988, as there is inadequate lymph node data prior to this year. Patients were staged based on American Joint Committee on Cancer TNM staging guidelines (7th edition) into T1a, T1b, T2, T3, T4, and advanced node-positive (N+M0) or metastatic (M+) disease. Node-positive and metastatic diseases were considered to overrule the T stage, and these were classified as either N+M0 or M+. In a subset analysis, patients with available T stage were subdivided by T stage and lymph node status, positive (N+) or negative (N0), and presence (M+) or absence (M0) of metastases. Patients who were not able to be staged were excluded from this subset analysis. Not all patients who had metastatic disease had an accompanying T stage (27 out of the 94 patients). Similarly, not all patients who had node-positive disease had an accompanying T stage (76 out of the 249 patients).
For further subset analyses, patients were grouped by grade as low grade (grade 1–2), high grade (grade 3–4), or unknown. Demographic groupings included age (< 50, 50–59, 60–69, 70–79, and 80 years or older), gender, and race (white, black, other, and unknown).
Statistical Analysis
Logistic regression analysis was used to determine the likelihood of having a colectomy (versus appendectomy) based upon age group, gender, TNM stage, tumor grade, and race. Chi-squared analysis was used to ascertain differences in the T stage as related to nodal positivity and metastases. Overall and cancer-specific survivals were the primary outcome measures. Univariable Kaplan-Meier analyses and Cox proportional hazard modeling were used to evaluate overall and cancer-specific survival in the entire cohort with respect to tumor grade, stage, and surgical type. Variables that were statistically significant in the univariate proportional hazards models were included in a multivariate proportional hazards model. The final proportional hazards model included tumor grade, stage, and surgical type. Stratified univariate Kaplan-Meier curves were also plotted to evaluate the association between surgery type (appendectomy versus colectomy) and cancer-specific and overall survival. This association was evaluated across grade strata (low grade and high grade), stage strata (T1, T2-T4), lymph node–positive disease, and metastatic disease. All statistical analysis was performed using STATA® statistical software version 10.0 (College Station, Texas) and all testing was 2 sided.
Results
We identified 817 patients who underwent surgery for appendiceal carcinoid tumor from 1988 to 2011. Of these, 338 (41%) had an appendectomy alone and 479 (59%) underwent additional partial colectomy. Median survival in the appendectomy group was 64 months (0–287) while median survival in the partial colectomy group was 48 months (0–285). Table 1 summarizes the demographics of the cohort. Patients with higher stage disease were all significantly more likely to undergo colectomy than patients with T1aN0M0 disease. Patients with T1bN0M0 through T4N0M0 and metastatic disease were 3.42 to 4.39 times more likely to get colectomy than patients with T1aN0M0 disease (p ≤ 0.001). Patients with node-positive disease (N+M0) had the highest likelihood of colectomy and were 10.70 times more likely to have a colectomy than those with T1aN0M0 tumors (95% CI 5.81–19.60, p < 0.001). There was no statistically significant difference in patients who underwent colectomy by tumor grade or race. Females were significantly less likely to get colectomy than males (0.75, 95% CI 0.57–0.99, p = 0.044) and patients aged 50–59 were significantly more likely to get colectomy than patients less than 50 years old (1.66, 95% CI 1.15–2.40, p = 0.007).
There were 669 patients in whom data on T size, nodal, and metastatic status were all known (Table 2). As expected, increasing T stage was significantly correlated with nodal positivity (p < 0.001) and marginally correlated with metastasis (0.061). Out of patients with T1a tumors, 4% had positive lymph nodes and 3% had distant metastases, which increased to 38% positive lymph nodes and 13% metastatic disease in patients with T4 tumors.
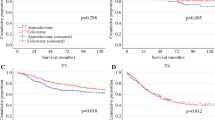
Although there was no significant difference in overall survival of patients by surgical type (Fig. 1a), patients who underwent colectomy were 1.98 times more likely to die of carcinoid than those who had an appendectomy alone (95% CI 1.32–2.98, p = 0.001) (Fig. 1b). While surprising, this result could be due to a selection bias of patients with more severe disease being more likely to receive colectomy. Therefore, we went on to analyze survival by surgical type in subsets grouped by grade or stage.
In univariable analysis, tumor grade was highly predictive of survival in appendiceal carcinoid (Table 3, Fig. 2a, b). Patients with high grade (grades 3–4) disease were 4.75 times (95% CI 2.82–8.01, p < 0.001) more likely to die overall and 12.00 times (95% CI 5.01–28.60, p < 0.001) more likely to die of carcinoid than patients with low-grade (grade 1–2) disease. However, there was no significant cancer-specific survival advantage to colectomy in subset analyses of patients with low-grade tumors or high-grade tumors (Fig. 2c, d).
Stage was similarly an important driver of survival in univariable analysis in appendiceal carcinoid (Table 3, Fig. 3a, b). Patients with T2-T4N0M0 stage disease tended to have worse survival than T1N0M0, but did not always reach significance. Patients with advanced disease that was node positive or metastatic had significantly worse survival than patients with T1N0M0 disease, and were 4.83 times (95% CI 3.18–7.32, p < 0.001) more likely to die overall and 12.5 times (95% CI 5.44–28.74, p < 0.001) more likely to die of carcinoid than patients with T1N0M0 disease. Again, subset analysis, this time by stage (T1N0M0, T2-T4N0M0, N+M0, and M+), did not show a significant cancer-specific survival advantage to colectomy (Fig. 3c–f). In fact, even though it did not reach statistical significance, patients with node-positive, non-metastatic disease who underwent colectomy were 2.28 times more likely to die of carcinoid than those who underwent appendectomy alone (95% CI 0.90–5.77, p = 0.081) (Fig. 3e). Thus, in the group of patients with appendiceal carcinoid most thought to benefit from colectomy, those with node-positive, non-metastatic disease, no survival benefit was seen in patients who underwent colectomy.
On multivariable analysis, only tumor stage was significantly associated with survival, with a 1.52 times higher likelihood of death overall (95% CI 1.36–1.69, p < 0.001) and 2.07 times higher cancer-specific death rate (95% CI 1.67–2.57, p < 0.001) for each increase in stage (Table 4). Surgical type was not associated with significantly better or worse survival rates when accounting for tumor stage and grade.
The percentage of patients with appendiceal carcinoid receiving colectomy has been trending up, particularly in the last 10–15 years (Fig. 4a). Over the same time period, survival among patients with appendiceal carcinoid appears to be getting worse, with 5-year survival trending down (Fig. 4b).
Discussion
We sought to determine under what circumstances colectomy conferred a survival advantage to patients with appendiceal carcinoid. Since colectomy is currently recommended in patients with T2 or higher stage appendiceal carcinoid tumors, our initial goal was to determine whether colectomy also conferred a survival advantage to patients with T1 appendiceal carcinoid tumors less than 2 cm in diameter. However, as our analysis progressed, we began to question the assumption that colectomy improves survival in patients with T2 or higher stage tumors, and analyzed survival by surgical type in subsets of patients throughout all grades and stages.
We found that the majority of patients with appendiceal carcinoid (59%) did have a colectomy, and colectomy was performed more commonly in patients with tumors of higher TNM stage. We also confirmed that patients with higher T stage tumors were more likely to harbor nodal or distant metastases. Even in patients with the lowest T stage tumors (T1a), there was a possibility of simultaneous nodal (4%) and/or distant metastases (3%). In those patients with higher T stage tumors (T2-T4), there was an up to 38% chance of simultaneous nodal metastases and 13% chance of distant metastases. These results confirm the findings of previous studies which suggest that higher stage tumors carry a higher incidence of positive lymph nodes and distant metastases; although in our study the numbers are lower than previously reported.5,6,7
We found that tumor grade was a significant predictor of survival, in those with high-grade tumors (3–4) being 4.8 times more likely to die overall and 12 times more likely to die of carcinoid than those with low-grade (1–2) tumors irrespective of surgical approach (appendectomy versus colectomy). This agrees with previous findings, but our numbers for cancer-specific survival rates in all patients with high-grade carcinoid (grades 3–4) were lower than previously reported survival rates.1 Similarly, those with nodal or metastatic disease were 4.8 times more likely to die overall and 12.5 times more likely to die of carcinoid than those with low stage (T1) node-negative, non-metastatic tumors. These results confirm what previous publications have shown, that patients with nodal and/or distant metastases have a worse outcome.8,9
Most importantly, those who underwent colectomy had significantly worse cancer-specific survival than those that underwent appendectomy alone. This may be due to the fact that patients receiving colectomy tend to have higher stage tumors. However, in further analysis of survival by surgical type within patients grouped by stage or grade, we found that in all comparisons, including low-grade versus high-grade and low-stage versus high-stage patients, there was no survival advantage to patients who underwent colectomy versus appendectomy alone. In fact, for patients with node-positive disease, there was a trend toward worse cancer-specific survival in those who had a colectomy. Furthermore, as the frequency of colectomy has trended up in the last decade, the 5-year survival for patients with appendiceal carcinoid is trending down. In a subset analysis of patients with small primary tumors (T1), colectomy showed no survival advantage even in patients with positive nodes. Our findings agree with Nussbaum et al. that showed colectomy does not confer survival advantage in small (< 2 cm) T1 tumors,1 and along with other studies brings into question whether there is a survival advantage for colectomy even in patients with high-stage tumors > 2 cm.10,11
Regardless of surgical approach, patients with low-grade tumors had a higher survival while those with high-grade tumors had lower survival. Similarly, analysis by stage shows that patients with higher stage disease have worse survival than patients with lower stage disease, and survival by stage was not significantly influenced by surgical type. According to our data, the grade of the tumor and the extent of disease should be considered in the management of appendiceal carcinoid to decide the type of surgery that would benefit the patient. Our findings agree with other studies that suggest patients with T1 tumors would not benefit from colectomy, even with positive nodes, and also brings into question the benefit of colectomy for higher stage tumors.1,9,10,11
This study had several important limitations. While this is a large sample size for appendiceal carcinoma (a rare tumor), there were less than 1000 patients in the analysis—making statistical comparisons difficult, particularly among subset analysis. The SEER database does not contain information on receipt or duration of chemotherapy, which may play a role in survival in patients with advanced carcinoid tumors. Also, TNM staging was incomplete for 18% (148/817) of patients included in the study. The data were also retrospectively collected and analyzed, and there may have been significant selection bias as to who underwent colectomy and the reasons for this. Finally, as with any large dataset, there is the possibility of miscoding or errant entry; however, these entries should not be biased and should balance out over the entire cohort studied.
Appendiceal carcinoid is a rare tumor, thus performing prospective studies to conclusively determine the optimal surgical approach is difficult. Large database studies that lack specific information on each case must be taken in the context of smaller studies that include more demographics and data elements. Current literature has conflicting conclusions about the benefit of colectomy. Further prospective studies are required to examine whether colectomy confers benefit in patients with appendiceal carcinoid tumors.
Conclusion
Survival in patients with carcinoid tumor of the appendix is primarily determined by tumor grade and stage. Our study found no survival advantage to colectomy over appendectomy in a large cohort of patients with the disease. Further investigation is necessary prior to recommending change of practice for patients with this disease.
Abbreviations
- CI:
-
confidence interval
- HR:
-
hazard ratio
- NCCN:
-
National Comprehensive Cancer Network
- N0:
-
node negative
- N+:
-
node positive
- M0:
-
no metastasis
- M+:
-
metastasis
- SEER:
-
Surveillance, Epidemiology, and End Results
- TNM:
-
tumor, node, and metastasis
References
Yao JC, Hassan M, Phan A, Dagohoy C, Leary C, Mares JE, Abdalla EK, Fleming JB, Vauthey JN, Rashid A, Evans DB. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008;26:3063–3072.
Toumpanakis C, Standish RA, Baishnab E, Winslet MC, Caplin ME. Goblet cell carcinoid tumors (adenocarcinoid) of the appendix. Dis Colon Rectum 2007;50(3):315–322.
Nussbaum DP, Speicher PJ, Gulack BC, Keenan JE, Ganapathi AM, Englum BR, Tyler DS, Blazer DG. Management of 1- to 2- cm carcinoid tumors of the appendix: Using the National Cancer Data Base to address controversies in general surgery. J Am Coll Surg 2015;220(5):894–903.
Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: Retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 1998;41(1):75–80.
Maggard MA, O’Connell JA, Ko CY. Updated population based review of carcinoid tumors. Ann Surg 2004;240:117–122.
Stinner B, Kisker O, Zielke A, Rothmund M. Surgical management for carcinoid tumors of small bowel, appendix, colon, and rectum. World J Surg 1996;20(2):183–188.
Moertel CG, Weiland LH, Nagorney DM, Dockerty MB. Carcinoid tumor of the appendix: treatment and prognosis. N Engl J Med 1987;317:1699–1701.
Sandor A, Modlin IM. A retrospective analysis of 1570 appendiceal carcinoids. Am J Gastroenterol 1998;93:422–428.
Mullen JT, Savarese DM. Carcinoid tumors of the appendix: a population-based study. J Surg Oncol 2011;104:41–44.
Ciarrocchi A, Pietroletti R, Carlei F, Necozione S, Amicucci G. Propensity adjusted appraisal of the surgical strategy for appendiceal carcinoids. Tech Coloproctol 2015;19(1):35–41.
Bamboat ZM, Berger DL. Is Right Hemicolectomy for 2.0-cm Appendiceal Carcinoids Justified? Arch Surg 2006;141(4):349–352.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the experimental design, data analysis, and writing of the manuscript.
Corresponding author
Ethics declarations
This study was reviewed and approved by the Bassett Healthcare Network Institutional Review Board.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guzman, C., Boddhula, S., Panneerselvam, N. et al. Appendiceal Carcinoid Tumors: Is There a Survival Advantage to Colectomy over Appendectomy?. J Gastrointest Surg 24, 1149–1157 (2020). https://doi.org/10.1007/s11605-019-04306-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04306-w