Abstract
Background
Endoscopic submucosal dissection (ESD) of superficial esophageal cancer has been used increasingly as an alternative to surgery because it is minimally invasive and has a high rate of en bloc resection. We previously reported that the double endoscopic intraluminal operation (DEILO) is a useful technique for ESD of early esophageal cancers. In the current study, we showed comparable short-term data between DEILO and conventional ESD groups to demonstrate the further advanced use of DEILO.
Methods
We studied 111 esophageal cancer patients with 111 lesions treated using endoscopic surgery between January 2010 and June 2016 at Gunma University Hospital. Of the patients, 51 underwent DEILO (DEILO group) and 60 underwent conventional ESD (ESD group). We compared the operable performance, complications, and pathological outcome between the ESD and DEILO groups.
Results
There was no significant difference in operable performance. However, the DEILO group showed a significantly lower rate of mediastinal emphysema compared to the ESD group (p = 0.025). Overall, the DEILO group showed a lower complication rate compared to the ESD group, although there was no apparent significance.
Conclusion
To our knowledge, this is the first report comparing DEILO and conventional ESD for esophageal cancer. The results showed that DEILO is not inferior to conventional ESD. DEILO is an excellent endoscopic surgical method, although it has some limitations compared to conventional ESD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoscopic resection of early esophageal cancer without risk of lymph node metastases has been accepted widely as an effective therapeutic strategy because it offers similar success rates compared to esophagectomy, but carries lesser morbidity and mortality. Endoscopic submucosal dissection (ESD) was developed as a novel endoscopic treatment. ESD of superficial esophageal cancer has been performed increasingly as an alternative to surgery because it is minimally invasive and has a high rate of en bloc resection.1 However, ESD is a more difficult technique for esophageal cancer than for gastric cancer because the working space for esophageal ESD is small. In addition, the difficulty level increases gradually depending on the size of the carcinoma. Also, during conventional ESD, the entire procedure is done through a single endoscope and there is no second hand to help as in conventional surgery. Adequate tissue tension and clear visibility of the tissue to be dissected by traction are important for effective and safe ESD. Many traction methods have been reported to date.
Some reports showed the use of magnetic anchor-guided-ESD (MAG-ESD) to help provide traction during ESD.2,3,4,5,6 Gotoda et al.3 reported MAG-ESD to be a feasible and safe method that allowed for excellent visualization with suitable tissue tension, and that MAG-ESD facilitated gastric ESD in patients with esophagogastric cancer. For gastric cancer, several traction techniques have been reported,7,8 but few reports discussed esophageal cancer.
Oyama et al.9 reported on the clip-with-line method, which is a simple, easy, and useful method of traction not only for gastric ESD, but also for esophageal, colonic, and duodenal ESD. Chen PJ et al.10 reported on percutaneous transgastric traction (PTT)-assisted ESD for esophageal lesions using pigs.
In 2004, we reported on the double endoscopic intraluminal operation (DEILO), which enables resection of mucosal lesions using two fine endoscopes and monopolar shears.11 The use of two fine endoscopes allows for easy dissection of lesions in the esophageal and gastric lumens.11 Subsequently, short-term and long-term outcomes of DEILO for gastric cancer have been reported at our institution.12,13 The DEILO procedure for early gastric cancer was reported to shorten ESD operative time, and efficacy and complication rates were comparable with those of the standard procedure.12 We also previously reported the use of DEILO for esophageal cancer.13 For all patients, the DEILO procedure was performed successfully, en bloc resection was achieved, and there were no apparent complications except postoperative hemorrhage in one case. As a result, we concluded that DEILO was a useful technique for ESD of early esophageal cancers.14
However, to our knowledge, no comparable data have been reported between DEILO and conventional ESD. In the current report, we compared DEILO and conventional ESD performed in a short-term period to discover the further advanced use of DEILO.
Materials and Methods
We studied 111 esophageal cancer patients (91 men and 20 women) with 111 lesions treated using endoscopic surgery between January 2010 and June 2016 at Gunma University Hospital. Of the patients, 51 underwent DEILO (DEILO group), and 60 underwent conventional ESD (ESD group). This study was approved by the institutional review board (IRB) in our institute, and patients were enrolled in the study after providing written informed consent. Patients with multiple cancers and posttreatment radiation therapy were excluded from this study. We compared the operable performance, complications, and pathological outcome between the two groups. There was no difference in qualifications of endoscopists and experienced cases in two groups. The characteristics of the 111 patients are presented in Table 1. The mean age (± standard division) was 67.7 ± 8.5 and 66.6 ± 10.5 years in the ESD and DEILO groups, respectively (p = 0.549). In the ESD group, 4 cancers were located in the cervical (Ce), 7 in the upper thoracic (Ut), 29 in the middle thoracic (Mt), 18 in the middle lower thoracic (Lt), and 2 in the abdominal (Ae) esophagus, compared to 0, 3, 28, 15, and 5, respectively, in the DEILO group (p = 0.089). According to the macroscopic diagnosis, 3 tumors were type 0-I, 9 type 0-IIa, 29 type 0-IIb, and 19 type 0-IIc in the ESD group, compared to 2, 8, 27, and 14, respectively, in the DEILO group (p = 0.948). In addition, 52 tumors (86.7%) had been diagnosed preoperatively as cT1a (invaded to the muscularis mucosae) and 8 (13.3%) as cT1b (invaded to the superficial submucosal layer) in the ESD group, compared to 76.5% and 23.5%, respectively, in the DEILO group (p = 0.164).
ESD and DEILO Technique
All treatments were performed with the patient under general anesthesia. Airway management by insertion of an endotracheal tube assisted secure ventilation and might have prevented intraoperative aspiration or postoperative pneumonia. The patients were positioned laterally on the left side throughout the operation.
ESD Technique
After spraying Lugol’s solution onto the mucosa, the mucosal surface surrounding the lesion margin was marked carefully using the Flush knife (DK2618JN15; Fuji Film Co., Ltd.) with electrocauterization (soft coagulation mode). A submucosal injection using MucoUp® (Johnson & Johnson Co., Ltd.) mixed with epinephrine and indigo carmine was administered to lift the lesion. A circumferential mucosal incision was made around the lesion using a Flush knife. Continuous submucosal dissection was performed from the oral to the anal sides in sequence, and the specimen was resected. Finally, ESD was finished after checking for hemostasis.
DEILO Technique
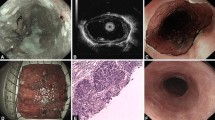
The DEILO technique for esophageal cancer has been described previously in detail.1114 (Fig. 1). The procedure for the DEILO group was the same until the circumferential mucosal incision. Submucosal dissection was performed for approximately half of the entire dissection. Immediately following completion of this procedure, DEILO was commenced using a dedicated overtube and separator. Two gastrointestinal endoscopes were used for DEILO, which made the procedure more precise than diagnostic endoscopy.14 The advantage of DEILO was to provide adequate tension and a clear view of the cutting plane and dissected tissue. However, DEILO has a crucial limitation to be described. The Ce and parts of the Ut esophageal cancers were excluded from the indication for DEILO because of the use of an overtube covering those areas. Moreover, the cases of stricture at a part of the overtube were excluded because a forceful insertion could lead to esophageal injury.14
Procedure of DEILO. After spraying Lugol’s solution onto the mucosa, the mucosal surface surrounding the lesion margin was carefully marked using the Flush knife with electrocauterization. After a submucosal injection using MucoUp®, a circumferential mucosal incision was made around the lesion using a Flush knife. Subsequently, the second endoscope was inserted into the esophagus, and the edge of the lesion was elevated using a grasping forceps after submucosal dissection was performed for approximately half of entire dissection. This traction provided a clear view of the cutting plane and dissected tissue
Histological Assessment of the Resected Specimen
The resectability of the DEILO specimens was evaluated carefully histopathologically in 2-mm thick slices, according to the Guidelines for Clinical and Pathological Studies on Carcinoma of the Esophagus, 10th ed.15 Each slice was assessed microscopically for histological type, depth of invasion, presence or absence of lymphatic or venous invasion, and completeness of the resection.
Evaluation of Complications After Endoscopic Resection and Follow-Up
Chest and abdominal x-rays were performed to identify any complications in all patients, such as mediastinal emphysema, pneumothorax, or pulmonary atelectasis. The following day, all patients underwent a follow-up endoscopic examination to check for bleeding of the resected ulcer. After the follow-up endoscopy, water and food intake were permitted in sequence. After discharge from the hospital, an endoscopic examination was performed at fixed intervals according to the results of pathological examination or resected circumference.
Statistical Analysis
The patient characteristics, operable performance complications, and pathological outcome were analyzed by the χ2 method, Fisher’s exact test, and the analysis of variance (ANOVA) method. Probability values of p < 0.05 indicated a statistically significant difference.
Results
A comparison of operative performance is shown in Table 2. For all patients (100%) among the two groups, the procedure was performed successfully and en bloc resection was achieved (data not shown in Table 2). Median operative time was 114 (range 33–266) and 112 (33–236) min in the ESD and DEILO groups, respectively (no significant difference, p = 0.445; Fig. 2). Postoperative hospital stay and longitudinal dimension of resected specimens in the two groups also were not significant (p = 0.215, p = 0.666, respectively; Table 2). With respect to complications, a postoperative hemorrhage was recognized in only one patient in whom anticoagulants were initiated 7 days after the procedure in the DEILO group (p = 0.211). Perforation, pneumothorax, and subcutaneous emphysema occurred in one patient in the ESD group, and none in the DEILO group (p = 0.266). The rate of mediastinal emphysema was significantly lower in the DEILO compared to the ESD groups (p = 0.025; Fig. 3). There was no significant difference in the postoperative stricture rate (p = 0.838).
The comparison of pathological outcome is summarized in Table 3. There was no significant difference in the depth of invasion and histological type (p = 0.544, p = 0.159, respectively) or positive rate of cancer in the horizontal and vertical margins (p = 0.121, p = 0.266, respectively) between the two groups. The vertical margin was negative in all patients in the DEILO group. As a result, the DEILO group tended to have a lower residual tumor rate compared to the ESD group (p = 0.077); however, there was no significant difference.
Discussion
Due to the development of ESD, en bloc resection of large gastrointestinal neoplasms can be performed successfully. However, ESD still has many limitations, such as its technical difficulty, long procedure times, and risks of perforation and bleeding.14 Adequate tissue tension and good visibility of the tissue to be dissected are very important for effective and safe dissections. Ota M et al. reported the usefulness of clip traction and it shortens operating time and is safer in esophageal ESD.16 Chen PJ et al. reported percutaneous transgastric traction-assisted ESD can enhance the speed of submucosal dissection for esophageal ESD to completely remove large areas of resected mucosa in a porcine model.10 Mortagy M et al. also reported MAG-ESD reduced procedure time and enhanced exposure of dissection line compared to standard ESD.6 We think DEILO is an excellent technique as it does not require special tools and does not require any special technique as compared with these recent reports. We believe that stabilizing the submucosa with DEILO by applying tension is efficient and reduces the incidences of complications. The most important advantage of DEILO is that it allows the resected specimen to be moved freely so that the assistant can operate freely using the second scope. However, it is a little difficult to perform DEILO technique without interference of each scope (first scope and second scope). Therefore, most important tip of DEILO is to perform procedure without interference of each scope (first scope and second scope).
The knack to keep the scopes from interfering with each other is to put the two scopes alternately in and out, and interference tends to occur when trying to move at the same time. It is also important to do while checking the position so as not to interfere with each other. In our study, we reported comparable data obtained from the DEILO and conventional ESD groups. As a result, the DEILO group did not show an advantage in regard to operative times when compared to the ESD group. This is because DEILO is a more complex procedure (e.g., insertion of a separator and movement of a second scope) compared to conventional ESD. Establishment of a more stylized procedure will lead to a shortened operative time for DEILO. With regard to complications, there was a significant difference in the rates of mediastinal emphysema between the two groups. DEILO is an excellent procedure compared to conventional ESD with regard to complications of mediastinal emphysema. Our results showed that DEILO can provide adequate tissue tension and clear visibility of the tissue to be dissected by traction compared to conventional ESD. We believe this to be an important perception to establish steadier and safer endoscopic resections. However, there was no significant difference among other complications because the total complication rate was low. Regardless, we hypothesized that DEILO will reduce the incidences of complications. Moreover, one problem with DEILO is the tumor location. The Ce and some of the Ut tumors were excluded because they were covered by an overtube, which was used for the easy operation for esophageal cancer. Also, cases of strictures at a part of the overtube were excluded because a forceful insertion could lead to esophageal injury. In this study, most tumors at the Ce or Ut were resected by conventional ESD. Another problem is that a larger number of staff is required for DEILO than for conventional ESD.
Therefore, DEILO has disadvantage in terms of economy because it requires many endoscopists compared with conventional ESD, but DEILO is chosen as priority in enforcing safely. Additional improvement and advancement of the device will increase the indication for DEILO, as we mentioned previously.13 The most important finding in our report is that DEILO is not inferior to conventional ESD overall. DEILO is an excellent procedure with fewer complications, although it has some limitations compared to conventional ESD. However, great consideration is required regarding the good indications for DEILO. To our knowledge, this is the first report comparing DEILO and conventional ESD for esophageal cancer.
In conclusion, DEILO a good method of endoscopic surgery for early esophageal cancer, although we should explore further less invasive and safer methods.
References
Probst A, Aust D, Märkl B, Anthuber M, Messmann H (2015) Early esophageal cancer in Europe: endoscopic treatment by endoscopic submucosal dissection. Endoscopy 47:113–121
Kobayashi T, Gotohda T, Tamakawa K, Ueda H, Kakizoe T (2004) Magnetic anchor for more effective endoscopic mucosal resection. Jpn J Clin Oncol 34:118–123
Gotoda T, Oda I, Tamakawa K, Ueda H, Kobayashi T, Kakizoe T (2008) Prospective clinical trial of magnetic-anchor-guided endoscopic submucosal dissection for large early gastric cancer (with videos). Gastrointest Endosc 69:10–15
Repici A (2009) Endoscopic submucosal dissection: established, or still needs improving?, Gastrointest Endosc 69:16–18
Fukami N (2013) What we want for ESD is a second hand! Traction method. Gastrointest Endosc 78:274–276
Mortagy M, Mehta N, Parsi MA, Abe S, Stevens T, Vargo JJ, Saito Y, Bhatt A (2017) Magnetic anchor guidance for endoscopic submucosal dissection and other endoscopic procedures. World J Gastroenterol 23:2883–2890
Nishiwaki S, Araki H, Shirakami Y, Niwa Y, Iwashita M, Hatakeyama H, Saitoh K (2009) Transgastrostomic endoscopy-assisted endoscopic submucosal dissection. Endoscopy, https://doi.org/10.1055/s-2008-1077713, Feb 5, 2009.
Imaeda H, Iwao Y, Ogata H, Ichikawa H, Mori M, Hosoe N, Masaoka T, Nakashita M, Suzuki H, Inoue N, Aiura K, Nagata H, Kumai K, Hibi T(2006) A new technique for endoscopic submucosal dissection for early gastric cancer using an external grasping forceps. Endoscopy 38:1007–1010
Oyama T(2012) Counter traction makes endoscopic submucosal dissection easier. Clin Endosc 45:375–8
Chen PJ, Huang WC, Wang HP, Chang WK, Hsieh TY, Shih SC, Wang HY, Liu CY(2012) Percutaneous transgastric traction-assisted esophageal endoscopic submucosal dissection: a randomized controlled trial in a porcine model. Scand J Gastroenterol 47:1386–1393
Kuwano H, Mochiki E, Asao T, Kato H, Shimura T, Tsutsumi S (2004) Double endoscopic intralumenal operation for upper digestive tract diseases: proposal of a novel procedure. Ann Surg 239:22–27
Mochiki E, Yanai M, Toyomasu Y, Ogata K, Andoh H, Ohno T, Aihara R, Asao T, Kuwano H (2010) Clinical outcomes of double endoscopic intralumenal surgery for early gastric cancer. Surg Endosc 24:631–636
Toyomasu Y, Suzuki M, Yanoma T, Kimura A, Kogure N, Ogata K, Ohno T, Mochiki E, Kuwano H (2016) Outcomes of patients with early gastric cancer who underwent double endoscopic intraluminal surgery. Surg Endosc 30:178–83
Sohda M, Saito H, Yoshida T, Kumakura Y, Honjyo H, Hara K, Ozawa D, Suzuki S, Tanaka N, Sakai M, Miyazaki T, Fukuchi M, Kuwano H(2017) Utility of double endoscopic intraluminal operation for esophageal cancer. Surg Endosc 31:3333–3338
Japanese Society for Esophageal Disease. Guidelines for the clinical and pathological studies on carcinoma of the esophagus (10th edition). Tokyo: Kanehara, 2008.
Ota M, Nakamura T, Hayashi K, Ohki T, Narumiya K, Sato T, Shirai Y, Kudo K, Yamamoto M (2012) Usefulness of clip traction in the early phase of esophageal endoscopic submucosal dissection. Dig Endosc 24:315–318
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sohda, M., Kuriyama, K., Yoshida, T. et al. Comparable Data Between Double Endoscopic Intraluminal Operation and Conventional Endoscopic Submucosal Dissection for Esophageal Cancer. J Gastrointest Surg 24, 307–312 (2020). https://doi.org/10.1007/s11605-019-04137-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04137-9