Abstract
Background
Small bowel lesions (SBL) are rare, representing diagnostic and management challenges. The purpose of this cross-sectional study was to evaluate diagnostic modalities used and management practices of patients with SBL at an advanced endoscopic referral center.
Methods
We analyzed patients undergoing surgical management for SBL from 2005 to 2015 at a single tertiary care center. Patients were stratified into gastrointestinal bleed/anemia (GIBA) or obstruction/pain (OP).
Results
One hundred and twelve patients underwent surgery after presenting with either GIBA (n = 67) or OP (n = 45). The mean age of our study population was 61.8 years and 45% were women. Patients with GIBA were more likely to have chronic or acute-on-chronic symptoms (100% vs 67%) and more often referred from outside hospitals (82 vs. 44%) (p < 0.01). The most common preoperative imaging modalities were video capsule endoscopy (VCE) (96%) for GIBA and computer tomography CT (78%) for OP. Findings on VCE and CT were most frequently concordant with operative findings in GIBA (67%) and OP (54%) patients, respectively. Intraoperatively, visual inspection or palpation of the bowel successfully identified lesions in 71% of patients. When performed in GIBA (n = 26), intraoperative enteroscopy (IE) confirmed or identified lesions in 69% of patients. Almost all (90%) GIBA patients underwent small bowel resections; most were laparoscopic-assisted (93%). Among patients with OP, 58% had a small bowel resection and the majority (81%) were laparoscopic-assisted. Surgical exploration failed to identify lesions in 10% of GIBA patients and 24% of OP patients. Among patients who underwent resections, 20% of GIBA patients had recurrent symptoms compared with 13% of OP patients.
Conclusion
Management and identification of SBL is governed by presenting symptomatology. Optimal management includes VCE and IE for GIBA and CT scans for OP patients. Comprehensive evaluation may require referral to specialized centers.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The mid/distal small bowel has been referred to as the “dark continent” or “black box” of the gastrointestinal tract due to its length, complex anatomy, and inaccessibility to endoscopists.1,2 Clinical symptoms of lesions located in the jejunum and ileum are often vague and non-specific, including intermittent abdominal pain, obstruction, iron deficiency anemia, and occult gastrointestinal bleeding, resulting in delayed diagnosis.3,4,5,6 The small intestine is the most common source of obscure gastrointestinal bleeds, a majority of which are from angiodysplasias and less commonly tumors.1,7 Malignant small bowel tumors are more common and more often symptomatic in comparison to benign tumors.3 In one study, upwards of two thirds of malignant neoplasms of the small bowel presented with abdominal pain.8
Recent advances in technology have begun to shed light on diagnosing lesions in the jejunum and ileum. Capsule endoscopy has been shown to be more sensitive in diagnosing small bowel lesions compared to standard imaging approaches.9,10,11,12 Single, double-balloon, and spiral enteroscopy offer both diagnostic and therapeutic potential. These modalities are diagnostically comparable to VCE, but are more invasive 1. Intra-operative enteroscopy (IE) is usually a last resort for obscure lesions that are not amenable to less-invasive interventions.1,13
Mid/distal small bowel lesions can be managed in a variety of ways. Initially, bleeding lesions can be managed through endoscopic interventions including electrocoagulation, sclerotherapy, and hemoclip placement.14,15 When these modalities fail, surgical intervention remains the treatment of choice for definitive therapy.8,14,15 There is limited literature on surgical intervention for small bowel lesions of the jejunum and ileum, due in part to their relative rarity. Presentations are starkly different between patients with gastrointestinal bleeds/anemia (GIBA) and those with obstruction and pain (OP), prompting this study to explore whether diagnostic workup and therapy reflect these differences as well. The objectives of this observational study were to examine the presentation, diagnostic workup, and outcomes of patients undergoing surgical intervention for jejunal/ileal lesions further stratified on the basis of their presenting symptomatology. We hypothesize that investigation and management of small bowel lesions among these groups of patients will differ.
Materials and Methods
Patient Population
A retrospective chart analysis was performed on adult patients (≥ 18 years of age) who underwent open or laparoscopic abdominal surgery for suspected small bowel lesions in the jejunum or ileum at a single tertiary care center in Central Massachusetts from July, 2005, to September, 2015. Inclusion criteria consisted of pre-operative diagnosis of either a gastrointestinal bleed, small bowel obstructive symptomatology not related to adhesions, small bowel mass/tumor, intussusception, small bowel diverticulum, small bowel ulcer, or small bowel perforation. Cases of duodenal ulcers/perforations, duodenal diverticulum, inflammatory bowel disease, and obstructive symptomatology due to adhesions from prior surgery were excluded.
Data Collection
Medical charts were reviewed for patient demographic characteristics, co-morbidities, pre-operative imaging/workup, endoscopic interventions, surgical interventions, hospital course, and disposition. Study data were collected and managed using REDCap (Research Electronic Data Capture) electronic data capture tools hosted at the University of Massachusetts Medical School. REDCap is a secure, web-based application designed to support data capture for research studies, providing (1) an intuitive interface for validated data entry, (2) audit trails for tracking data manipulation and export procedures, (3) automated export procedures for seamless data downloads to common statistical packages, and (4) procedures for importing data from external sources.16
Endoscopic Approach
Deep enteroscopy (DE) is a generic term for techniques including spiral enteroscopy double balloon enteroscopy (DBE) and single balloon enteroscopy. The spirus technique is used anterograde and the balloon methods may be used anterograde or retrograde. They all allow visualization and therapeutic intervention much deeper into the small bowel than was previously possible. Video capsule endoscopy (VCE) was performed using a Given Imaging PillCam [SB2™ or SB3™: Yokneam, Israel] that was usually swallowed and allowed to transit through the gastrointestinal tract. Images were reviewed by gastroenterologists with expertise in VCE. VCE and DE are complimentary techniques; VCE is used first as it is non-invasive. Intraoperative enteroscopy (IE) is the utilization of either a gastroscope or enteroscope endoscope to evaluate the entire length of the small bowel. IE can be performed by inserting an enteroscope in a transoral or transanal approach and surgically running the bowel over the scope to evaluate the entire small bowel. An alternative approach is making a surgical enterotomy in the small bowel, and then passing a sterile endoscope into the lumen and examining the small bowel retrograde and anterograde.
Surgical Approach
Laparoscopic explorations are defined as diagnostic laparoscopy, where the entire small bowel was “run” laparoscopically. Laparoscopic-assisted procedures are defined as either explorations or resections performed laparoscopically and then a mini laparotomy was made for further investigation, intraoperative enteroscopy, and/or resection. Laparoscopic converted to open procedures were those that initially started as a laparoscopic approach and then a full exploratory laparotomy incision was made for further exploration with manual palpation.
Data Analysis
Based on the patient’s presenting symptomatology, patients were classified into two distinct subgroups: those with gastrointestinal bleed/anemia (GIBA), and those with obstruction/pain (OP), because of the marked differences in presentation and work up. Statistical analysis was performed using Stata Statistical Software: Release 13 (College Station, TX). Comparisons between patients with GIBA vs. OP were performed using Chi-Square analysis and Fisher’s Exact test or Student’s t test for discrete and continuous variables, respectively. Institutional Review Board approval was obtained for this study.
Results
Patient Characteristics
The mean age of the study population was approximately 62 years, 55% were men, and more than three-quarters were Caucasian and over half had public insurance. Among all patients, 60% (n = 67) presented with GIBA. The average body mass index (BMI) was significantly greater in the GIBA group. Patient presentations between groups differed significantly. All GIBA presented with either chronic or acute-on-chronic symptoms compared with two-thirds of patients with OP. Significantly more GIBA patients were referred from an outside institution (Table 1).
Diagnostic Workup
Patients who presented with GIBA underwent esophagogastroduodenoscopy (EGD), colonoscopy (COL), and deep enteroscopy (DE) at least twice as often compared to those who presented with OP (p < 0.01) (Table 2). Almost all GIBA patients had VCE (96%) compared with 40% of patients with OP (p < 0.01). Of those who had capsule endoscopy, two-thirds of the GIBA patients had a positive finding that was associated with intraoperative findings. Patients who presented with OP had a CT of the abdomen and pelvis almost three times as often as patients in the GIBA group (p < 0.01). OP patients were more likely to have a positive CT finding that correlated with operative findings compared to GIBA patients.
Surgical Approach, Intraoperative Findings, and Pathology
Small bowel resection (SBR) was the most common surgical procedure, performed as laparoscopic assisted (LASBR) in over three-quarters of patients (Table 3). SBR was performed 1.5 times as often in the GIBA group compared with the OP group (p < 0.01). Of all study patients, eighteen (16%) had an exploration without a resection because no lesion could be found. Intraoperatively, visual inspection combined with palpation of the bowel most often identified lesions (71%) with no between group differences (Table 4). Lesions were most frequently identified isolated to the ileum (45%), followed by the jejunum (34%). Six patients in the GIBA group had multifocal lesions in both the ileum and jejunum. Intraoperative enteroscopy (IE) was performed four times as frequently in the GIBA group (p < 0.01) (Table 3). Of all patients who underwent IE (n = 30), IE was performed by either exteriorizing the small bowel (77%), through an oral or anal approach (20%), or a combination of both approaches (3%). Over two-thirds of IE successfully confirmed or identified a suspected lesion intraoperatively in the GIBA group (69%) compared with none in the OP group (p < 0.01) (Table 3). In six GIBA patients who underwent IE during exploration, no lesion was identified and no resection was carried out.
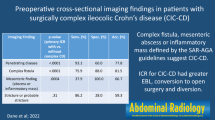
Overall, there was a wide variety of pathology found after surgical exploration (Fig. 1). Almost one-third of all lesions identified were malignant (30%), with 41% of these being carcinoid tumors. The most common pathology identified was angioectasia (24%) in the GIBA group compared to Meckel’s diverticulum (20%) in the OP group. Ten of the GIBA patients had no pathology (15%) due to either no SBR having been carried out (n = 7) or no abnormal pathology having been found in the SBR specimen (n = 3) (Fig. 1). Whereas, pathology was found in all OP patients except those who underwent exploration without resection (24%) (Fig. 1).
Hospital Course and Post-Discharge Follow-Up
Overall, the median length of stay was 5.5 days (range 4–9.5). There were no significant differences in terms of 30-day readmissions, return to the operating room, ICU readmission, wound infections, and 30-day mortality between the GIBA and OP groups (Table 5). Among all patients, six required a return to the operating room. The majority (n = 4) were for planned abdominal washout and closure in patients who presented acutely with a contaminated abdomen (n = 4). One required re-exploration with a second small bowel resection due to ischemia, and one had a re-exploration but was found to have an ileus.
Median follow-up for the GIBA group was 9 (1–47) months compared with 20 (3–66) months in the OP group. Of all study patients, 8% were lost to follow-up with no between-group differences noted. Over half of the remaining patients (57%) were asymptomatic. Recurrent symptoms similar to initial presentation were reported, in 21%, with the remaining patients reporting new symptoms not associated with their initial presentation (Table 5).
Among all patients in the GIBA group not lost to follow-up who underwent surgical resection (n = 54) or exploration without resection (n = 7), 13 had recurrent symptoms due to angioectasias (n = 10) or extra-small bowel bleed (n = 3). Of those 10 patients who had experienced recurrent symptoms of GIBA from an angioectasia, seven initially had a SBR with angioectasia confirmed, one patient had a SBR with lipoma found, one had no pathology found on their resection specimen, and one had a negative exploration, likely due to a pedunculated polyp that had undergone spontaneous avulsion. Of GIBA who had small bowel resections and were not lost to follow-up, 20% (11/54) had recurrent symptoms that were similar to their initial complaint.
In the OP group, nine patients had recurrent symptoms. Of those with recurrent obstructive symptoms (n = 3), two had ischemic small bowel resected on their initial operation and one had an exploration without resection. Among those with recurrent abdominal pain (n = 6), four had an exploration without resection and two had a SBR, with a jejunal diverticulum with ulceration in one and a Meckel’s diverticulum and ulceration in the other. Of OP patients that had a small bowel resection and were not lost to follow-up, 13% (4/31) had recurrence of presenting symptoms.
Discussion
The present study represents one of the largest descriptive studies of patients who underwent surgery for a SBL. The distinct presentations of patients with SBL can provide guidance as to the diagnostic workup and operative management. Therefore, we propose an algorithm for effectively managing patients with presumed SBL based on their presenting symptoms of either GIBA or OP (Fig. 2).
Approach for the management of presumed small bowel lesions workup and treatment for patients with suspected SBL should be determined by their presenting symptoms of either gastrointestinal bleeding/anemia (GIBA) or obstruction/pain (OP) symptoms. Deep enteroscopy (DE) includes spiral enteroscopy, single-balloon enteroscopy (SBE), and double-balloon endoscopy (DBE). Computed tomography (CT), computed tomography enterography (CTE), intraoperative enteroscopy (IE)
Pre-Operative Workup of Patients with Small Bowel Lesions
Radiologic Approach
Patients referred for workup for a small bowel lesion presenting with symptoms of GIBA and OP often required repeat investigations for identification of the lesion and appropriate operative planning. The most common radiological investigations overall were CT and CTE, which is similar with previous studies.1,17,18 Among OP patients, CT scan had the highest diagnostic yield of any diagnostic modality (Table 2). Results from previous literature have demonstrated that CT scans have a higher sensitivity in detecting small bowel obstruction compared to other radiologic studies.19 Therefore, in patients with SBL presenting with symptoms of OP, CT of the abdomen and pelvis should be considered early during diagnostic workup.
Capsule and Deep Enteroscopic Approach
Capsule endoscopy was the most commonly performed study in all GIBA patients (96%) and had the highest diagnostic yield of any study performed (67%); however, it was not as useful in patients with OP symptomatology (Table 2). Capsule endoscopy has been demonstrated as being superior in diagnosing Crohn’s disease compared with other modalities.20 In addition, more recent literature shows that capsule endoscopy has a higher diagnostic yield compared to other advanced endoscopic modalities for obscure small bowel gastrointestinal bleeds and has been suggested to be implemented sooner in diagnostic algorithms.1,15
In previous literature, capsule endoscopy has been shown to have complications such as retention.21,22 In fact, retention of capsules has a rate as high as 21% in patients with obstructive symptoms.22 Although the risk of retained capsule is quite high, it can be turned into an advantage in the surgical setting. The retained capsule is highly likely to be able to show the nature of the cause of retention and may in fact be retained at a site where there is no serosal evidence of any pathology.
The overall diagnostic yield of DE was 40% among all patients in this study and it had a higher utility among GIBA patients (Table 2). Previous studies have shown varying diagnostic yields of this imaging modality ranging from 22–80%.1,23,24,25,26 A number of prior studies have commented on the utility of advanced endoscopic modalities in small bowel tumor identification, but not on its utility in patients with obstructive symptomatology,27–29 similar to our findings.
Given the discrepancy in diagnostic yield between DE and VCE, in patients presenting with GIBA, a capsule study alone may be sufficient in identifying a suspected lesion without the need for other investigations prior to operative intervention. In fact, at our institution, we have initiated a protocol where GIBA patients receive a VCE in the emergency room, which may allow for earlier diagnosis and intervention.
Operative Intervention and Intraoperative Diagnostic Approach in Patients with Small Bowel Lesions
Small bowel resection was the most common procedure performed overall and operative intervention was more varied in OP patients (Table 3). Regardless, the utility of intraoperative visual inspection and manual palpation offered similar diagnostic yield in both GIBA and OP patients, identifying lesions approximately 70% of the time (Table 4). On the other hand, further intra-operative approaches to lesion identification and management differed in patients who presented with GIBA from those who presented with OP.
Intra-Operative Enteroscopy
Due to its invasive nature, IE has been referred to as the gold standard and last resort for detecting obscure gastrointestinal bleeds.13 It can allow for complete exploration of the small bowel, with identification of lesions in many patients.30,31 In fact, IE has a diagnostic yield as high as 80%.31 In GIBA patients, in our series, almost half underwent IE in an attempt to identify/confirm the lesion and it was most frequently performed (80%) through a planned enterotomy. This diagnostic modality was helpful in confirming suspected palpable lesions or those found and marked with ink from previous enteroscopy. When no lesion was found, IE was useful in confirming the absence of any lesion and thereby prevented any unnecessary intestinal resection. In patients with GIBA, IE accompanied by manual/laparoscopic palpation can be an effective additional approach to identify appropriate candidates for intestinal resection, but may not have utility in identifying lesions in OP patients.
Pathology and Recurrent Symptoms in Patients with Small Bowel Lesions
The most common pathology among GIBA patients was arteriovenous malformation (angioectasia) similar to previous reports7,11 while Meckel’s/jejunal diverticulosis and carcinoid tumors made up almost half of the pathology seen in the OP group (Fig. 1).
Among all patients, approximately one-fifth had recurrent symptoms after surgical resection (Table 5). Among GIBA patients with recurrent symptoms, seven had angioectasias found in the resected specimen and two returned with GIBA symptoms from newly diagnosed angioectasias. These most likely represent either missed lesions, multifocal lesions or the development of new lesions, which are commonly associated with angioectasias.32
Surgical intervention provides alleviation of presenting symptoms in patients with GIBA and OP. Because of the high recurrence of GIBA symptoms in patients with angioectasia after SBR, these lesions should be managed with medical or endoscopic approaches along with ongoing follow-up, surveillance, and a multidisciplinary collaboration with GI medicine.
Study Strengths and Limitations
This study offers insights into the diagnosis and surgical management of small bowel lesions, which are rare. Although it is a retrospective cohort from a single tertiary care center, it is one of the largest compilations of small bowel lesions in the current literature. We stratified small bowel lesions by their presenting symptoms (GIBA and OP). Because these small bowel lesions present differently, we also found that they differ in their diagnostic workup. In addition, this study demonstrates that laparoscopic-assisted small bowel resection offers an effective treatment modality for patients with small bowel lesions. This study does have several limitations that must be kept in mind in interpreting the present study findings, however. These include a relatively small sample size, retrospective design, and some patient loss to follow-up. The small study size might not be large enough to detect all the differences between study groups. Lastly, we had a relatively high incidence of no pathology found. This is in part due to the nature of small bowel lesions being notoriously difficult to detect. In addition, certain lesions such as angioectasias can be difficult to localize intraoperatively compared to masses that can be palpated. This could be an additional explanation for the high incidence of negative pathology.
Conclusions
Small bowel lesions are rare and differ in presentation and management. Groups can be divided based on patient’s presenting symptomatology into GIBA and OP. The surgical workup of GIBA patients should include VCE and IE for diagnosis and lesion confirmation, respectively. Capsule studies are an appropriate first line intervention in these patients and further deep enteroscopic techniques can aid in lesion identification if capsule is otherwise negative or there is a need for procedural intervention at the time of diagnostic endoscopy. Angioectasias often prove difficult to manage operatively with higher rates of recurrence of GIBA. If angioectasia are diagnosed, medical or endoscopic management of these lesions may be the preferred approach.
In patients who present with OP, CT of the abdomen and pelvis is the single best diagnostic modality. Regardless of presentation, surgical intervention provides alleviation of symptoms in patients with GIBA and OP; however, GIBA patients might be more amenable to minimally invasive operative approaches.
References
Gunjan D, Sharma V, Rana SS, Bhasin DK (2014) Small bowel bleeding: a comprehensive review. Gastroenterol Rep (Oxf) 2:262-275
Ma JJ, Wang Y, Xu XM, Su JW, Jiang WY, Jiang JX, Lin L, Zhang DQ, Ding J, Chen L, Jiang T, Xu YH, Tao G, Zhang HJ (2016) Capsule endoscopy and single-balloon enteroscopy in small bowel diseases: Competing or complementary? World J Gastroenterol 22:10625-10630
Ciresi DL, Scholten DJ (1995) The continuing clinical dilemma of primary tumors of the small intestine. Am Surg 61:698-702; discussion 702-693
Coco C, Rizzo G, Manno A, Mattana C, Verbo A (2010) Surgical treatment of small bowel neoplasms. Eur Rev Med Pharmacol Sci 14:327-333
Gill SS, Heuman DM, Mihas AA (2001) Small intestinal neoplasms. J Clin Gastroenterol 33:267-282
Ojha A, Zacherl J, Scheuba C, Jakesz R, Wenzl E (2000) Primary small bowel malignancies: single-center results of three decades. J Clin Gastroenterol 30:289-293
Zhang BL, Chen CX, Li YM (2012) Capsule endoscopy examination identifies different leading causes of obscure gastrointestinal bleeding in patients of different ages. Turk J Gastroenterol 23:220-225
Talamonti MS, Goetz LH, Rao S, Joehl RJ (2002) Primary cancers of the small bowel: analysis of prognostic factors and results of surgical management. Arch Surg 137:564-570; discussion 570-561
de Leusse A, Vahedi K, Edery J, Tiah D, Fery-Lemonnier E, Cellier C, Bouhnik Y, Jian R (2007) Capsule endoscopy or push enteroscopy for first-line exploration of obscure gastrointestinal bleeding? Gastroenterology 132:855-862; quiz 1164-1165
Laine L, Sahota A, Shah A (2010) Does capsule endoscopy improve outcomes in obscure gastrointestinal bleeding? Randomized trial versus dedicated small bowel radiography. Gastroenterology 138:1673-1680.e1671; quiz e1611-1672
Raju GS, Gerson L, Das A, Lewis B (2007) American Gastroenterological Association (AGA) Institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology 133:1694-1696
Singh A, Marshall C, Chaudhuri B, Okoli C, Foley A, Person SD, Bhattacharya K, Cave DR (2013) Timing of video capsule endoscopy relative to overt obscure GI bleeding: implications from a retrospective study. Gastrointest Endosc 77:761-766
Bonnet S, Douard R, Malamut G, Cellier C, Wind P (2013) Intraoperative enteroscopy in the management of obscure gastrointestinal bleeding. Digestive and Liver Disease 45:277-284
Apostolopoulos P, Liatsos C, Gralnek IM, Kalantzis C, Giannakoulopoulou E, Alexandrakis G, Tsibouris P, Kalafatis E, Kalantzis N (2007) Evaluation of capsule endoscopy in active, mild-to-moderate, overt, obscure GI bleeding. Gastrointestinal endoscopy 66:1174-1181
Teshima CW, Kuipers EJ, van Zanten SV, Mensink PB (2011) Double balloon enteroscopy and capsule endoscopy for obscure gastrointestinal bleeding: an updated meta-analysis. Journal of gastroenterology and hepatology 26:796-801
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377-381
Lee SS, Oh TS, Kim HJ, Chung JW, Park SH, Kim AY, Ha HK (2011) Obscure gastrointestinal bleeding: diagnostic performance of multidetector CT enterography. Radiology 259:739-748
Zhang BL, Jiang LL, Chen CX, Zhong BS, Li YM (2010) Diagnosis of obscure gastrointestinal hemorrhage with capsule endoscopy in combination with multiple-detector computed tomography. J Gastroenterol Hepatol 25:75-79
Thompson JS (2002) Contrast Radiography and Intestinal Obstruction. Annals of Surgery 236:7-8
Triester SL, Leighton JA, Leontiadis GI, Gurudu SR, Fleischer DE, Hara AK, Heigh RI, Shiff AD, Sharma VK (2006) A meta-analysis of the yield of capsule endoscopy compared to other diagnostic modalities in patients with non-stricturing small bowel Crohn's disease. Am J Gastroenterol 101:954-964
Cheifetz AS, Lewis BS (2006) Capsule endoscopy retention: is it a complication? J Clin Gastroenterol 40:688-691
Liao Z, Gao R, Xu C, Li ZS (2010) Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc 71:280-286
Domagk D, Mensink P, Aktas H, Lenz P, Meister T, Luegering A, Ullerich H, Aabakken L, Heinecke A, Domschke W, Kuipers E, Bretthauer M (2011) Single- vs. double-balloon enteroscopy in small-bowel diagnostics: a randomized multicenter trial. Endoscopy 43:472-476
Mensink PB, Haringsma J, Kucharzik T, Cellier C, Perez-Cuadrado E, Monkemuller K, Gasbarrini A, Kaffes AJ, Nakamura K, Yen HH, Yamamoto H (2007) Complications of double balloon enteroscopy: a multicenter survey. Endoscopy 39:613-615
Messer I, May A, Manner H, Ell C (2013) Prospective, randomized, single-center trial comparing double-balloon enteroscopy and spiral enteroscopy in patients with suspected small-bowel disorders. Gastrointest Endosc 77:241-249
Xin L, Liao Z, Jiang YP, Li ZS (2011) Indications, detectability, positive findings, total enteroscopy, and complications of diagnostic double-balloon endoscopy: a systematic review of data over the first decade of use. Gastrointest Endosc 74:563-570
Cangemi DJ, Patel MK, Gomez V, Cangemi JR, Stark ME, Lukens FJ (2013) Small bowel tumors discovered during double-balloon enteroscopy: analysis of a large prospectively collected single-center database. J Clin Gastroenterol 47:769-772
Fry LC, Neumann H, Kuester D, Kuhn R, Bellutti M, Malfertheiner P, Monkemuller K (2009) Small bowel polyps and tumours: endoscopic detection and treatment by double-balloon enteroscopy. Aliment Pharmacol Ther 29:135-142
Lee BI, Choi H, Choi KY, Byeon JS, Jang HJ, Eun CS, Cheon JH, Shin SJ, Kim JO, Lee MS, Choi JH (2011) Clinical characteristics of small bowel tumors diagnosed by double-balloon endoscopy: KASID multi-center study. Dig Dis Sci 56:2920-2927
Bonnet S, Douard R, Malamut G, Cellier C, Wind P (2013) Intraoperative enteroscopy in the management of obscure gastrointestinal bleeding. Dig Liver Dis 45:277-284
Voron T, Rahmi G, Bonnet S, Malamut G, Wind P, Cellier C, Berger A, Douard R (2017) Intraoperative Enteroscopy: Is There Still a Role? Gastrointest Endosc Clin N Am 27:153-170
Somsouk M, Gralnek IM, Inadomi JM (2008) Management of obscure occult gastrointestinal bleeding: a cost-minimization analysis. Clin Gastroenterol Hepatol 6:661-670
Author information
Authors and Affiliations
Contributions
All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
JG: Contributed to study design, data acquisition, data analysis, data interpretation, drafting and revising the manuscript, and final approval of the manuscript
CRS: Contributed to study design, data acquisition, data analysis, data interpretation, drafting and revising the manuscript, and final approval of the manuscript
AF: Contributed to study design, data analysis, drafting and revising the manuscript, and final approval of the manuscript
KB: Contributed to study design, data analysis, drafting and revising the manuscript, and final approval of the manuscript
DHM: Contributed to study design, data acquisition, drafting and revising the manuscript, and final approval of the manuscript
MM: Contributed to study design, data acquisition, drafting and revising the manuscript, and final approval of the manuscript
KP: Contributed to study design, data acquisition, drafting and revising the manuscript, and final approval of the manuscript
DS: Contributed to study design, data acquisition, drafting and revising the manuscript, and final approval of the manuscript
DRC: Contributed to study design, data interpretation, critical revision of the manuscript, and final approval of the manuscript
DEL: Contributed to study design, data interpretation, critical revision of the manuscript, and final approval of the manuscript
MAC: Contributed to study design, data interpretation, critical revision of the manuscript, and final approval of the manuscript
Corresponding author
Ethics declarations
Grant Support
University of Massachusetts Center for Clinical and Translational Sciences TL1 Training Grant.
Grant # TL1TR001454
National Presentation
Society of American Gastrointestinal and Endoscopic Surgery (SAGES) Annual Meeting on March 24, 2017, in Houston Texas
Author Disclosures
Drs. Green, Schlieve, Friedrich, Baratta, Ma, Min, Patel, Cahan and Cave as well as Mr. Stein, have no conflicts of interest or financial ties to disclose. Dr. Litwin is on the surgical advisory board for Titan Medical.
Rights and permissions
About this article
Cite this article
Green, J., Schlieve, C.R., Friedrich, A.K. et al. Approach to the Diagnostic Workup and Management of Small Bowel Lesions at a Tertiary Care Center. J Gastrointest Surg 22, 1034–1042 (2018). https://doi.org/10.1007/s11605-018-3668-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3668-2