Abstract
Background
Enhanced recovery after surgery (ERAS) protocols have improved patient experience and outcomes in a variety of fields, including bariatric surgery. Given the increasing opioid epidemic in the USA, we sought to determine the impact of our own ERAS protocol on narcotic usage following laparoscopic sleeve gastrectomy.
Methods
Retrospective chart review was performed on patients undergoing primary laparoscopic sleeve gastrectomy for 6 months before and after implementation of an ERAS protocol. Our protocol strongly discouraged the use of narcotics in the postoperative period. Specific outcomes of interest were postoperative narcotic usage, length of stay, complications, and readmissions.
Results
Patient characteristics were similar in the two groups. ERAS implementation did not correlate with changes in length of stay, complications, or readmissions. However, ERAS implementation was associated with dramatic reductions in the use of intravenous narcotics (100% vs 47%, p < 0.01) and oral schedule 2 narcotics (56% vs 6%, p < 0.01), with an increase in the usage of tramadol (0% vs 36%, p < 0.01). After ERAS implementation, 52% of patients were managed without the use of schedule 2 narcotics (0% pre-ERAS, p < 0.01) and 33% received no narcotics of any kind (0% pre-ERAS, p < 0.01).
Conclusion
Implementation of an ERAS protocol for laparoscopic sleeve gastrectomy is associated with a dramatic reduction in the use of narcotics in the postoperative period. This has implementation for the usage of narcotics for laparoscopic surgery and potential elimination of narcotics for certain patients and procedures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
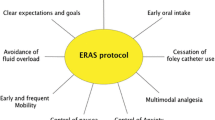
Since its first development for colorectal surgery in the 1990s, enhanced recovery after surgery (ERAS) protocols have been applied to numerous surgical subspecialties, including the field of bariatric surgery.1,2,3,4 ERAS pathways optimize the patient’s experience and outcomes through a variety of pre-, intra-, and postoperative interventions.5, 6 Preoperatively, ERAS protocols focus on optimizing nutrition, setting realistic expectations, and patient education.7 During surgery, protocols focus on issues such as local anesthesia and nociceptor inhibition, use of nasoenteric tubes, and even surgical technique.8, 9 Postoperatively, patients are treated with early enteral nutrition, increased ambulation, and multimodal pain control.4, 6, 9
ERAS protocols in bariatric surgery are unique in that they have remained relatively heterogeneous in terms of both their components as well as their measured outcomes.10 In light of the persistent opioid epidemic, one increasingly valued outcome is the amount of narcotics patients receive both in hospital as well as after discharge. Data suggest that up to 10% of all opioid naïve patients who are discharged with a prescription for narcotics are still using narcotics 1 year after surgery.11,12,13 Specifically, bariatric surgery patients may be up to 45% more likely to abuse opioids postoperatively than patients undergoing non-bariatric surgeries.14, 15
To address this specific concern, many published ERAS pathways for bariatric surgery aim to limit postoperative narcotic use. However, most still include opioids as part of their multimodal pain control approach, either through patient-controlled anesthesia (PCA) or through intermittent dosing of opioids.2, 16,17,18,19,20,21 This study is a retrospective review of the ERAS implementation at our center, where narcotic medications were removed from the default protocol, and schedule II narcotics were heavily discouraged. The goal of this protocol was to minimize, if not eliminate, the need for narcotics in the postoperative period.
Methods
Patient Population
This was a retrospective review of opioid-naïve patients undergoing primary sleeve gastrectomy before and after implementation of the ERAS protocol on July 1, 2017. Patients were excluded if they underwent a revision bariatric procedure (laparoscopic band converted to sleeve) or combined procedure (i.e., cholecystectomy). Patients were also excluded if they were already taking narcotics prior to their surgery (24 total patients). We examined two cohorts of patients. The pre-ERAS group included all patients in the 6 months before ERAS implementation, January 1–June 30, 2017. We then allowed a 3-month adjustment period because adherence to the new ERAS protocol was noted to be initially inconsistent. Thus, the post-ERAS group represented patients undergoing primary sleeve gastrectomy between October 1, 2017 and March 31, 2018.
Preoperative patient characteristics were examined to compare homogeneity between the two groups. These included age, gender, race, body mass index (BMI) closest to surgery, and American Society of Anesthesiologists (ASA) classification. Information on postoperative outcomes and narcotic usage were also gathered via retrospective chart review. This included hospital length of stay, occurrence of any complication, hospital readmissions within 30 days, outpatient visits for intravenous (IV) hydration, and postoperative utilization of IV morphine, IV hydromorphone, and oral oxycodone, hydrocodone, and tramadol.
Enhanced Recovery After Surgery Protocol
The ERAS protocol used at our institution was formulated based on discussions with colleagues at multiple institutions, and is demonstrated in Table 1. An order set was included in our electronic medical record for these patients and used by all physicians. At their preoperative clinic visit, patients were educated on the ERAS protocol and the goal to avoid narcotics in the postoperative period. They received gabapentin 300 mg three times daily for 3 days before surgery and celecoxib 200 mg once the day before surgery. On the morning of surgery, they consumed one glycemic endothelial drink 2–3 h before surgery, gabapentin 300 mg 2 h before surgery, and acetaminophen 975 mg 1 h before surgery.
We do not routinely use intraabdominal drains for sleeve gastrectomy and no patients in the study period received them. The only change intraoperatively was the use of laparoscopic-guided transversus abdominis plane (TAP) blocks performed by the operating surgeons after abdominal insufflation and before placement of working ports. This was done with 25 mL 0.25% bupivacaine with epinephrine on each side for a total of 50 mL. We discussed with our anesthesia providers the goal of limiting intraoperative narcotic usage; however, due to the heterogeneity of anesthesia staff and the negligible amount of intraoperative narcotics used prior to ERAS implementation, there was no appreciable difference following protocol use and this area was eliminated from the final analysis.
Postoperatively, the ERAS protocol included changes in medication usage and other aspects of patient care. Patients did not receive a urinary catheter and we abandoned the use of gastroesophageal contrast studies. Nursing protocols included incentive spirometry teaching along with early and frequent ambulation. For pain control, high-dose acetaminophen as needed was automatically selected in the order set, and nonsteroidal anti-inflammatory drugs (NSAIDs) were encouraged and frequently used. IV narcotics were discouraged but available on request. The only oral narcotic in the order set was tramadol, and the use of oxycodone and hydrocodone was discouraged. IV and oral ondansetron and promethazine were available for nausea control. Simethicone, senna-docusate, and milk of magnesia were also available as needed.
Patients were prescribed tramadol (50 mg) at discharge rather than other opioids. The number was not standardized and residents generally prescribed between 10 and 30 tablets. A large number of patients report not taking the tramadol after discharge; in fact, many do not even fill the prescription. It is a rare event for a patient to request a refill on this medication after discharge.
Tramadol is a synthetic opioid, structurally similar to morphine, that has proven effectiveness for the treatment acute and chronic pain.22 However, tramadol exerts a clinically insignificant effect on respiratory depression and gastrointestinal motility compared to other narcotic medications. The United States Drug Enforcement Administration categorizes drugs and other chemicals into categories based on abuse or dependency potential, with Schedule I representing the drugs with the highest abuse potential and Schedule V the lowest.23 According to this categorization, tramadol is a Schedule IV narcotic (“low potential for abuse and low risk of dependence”) while morphine, hydromorphone, oxycodone, and hydrocodone are Schedule II narcotics (“high potential for abuse, with use potentially leading to severe psychological or physical dependence”). It is for these reasons that our ERAS protocol focused on tramadol for pain control and minimized the role of Schedule II narcotics.
Statistical Analysis
This study was discussed with our Institutional Review Board and did not meet the regulatory criteria for research involving human subjects, and was thus exempt from oversight. Patient information was collected in a de-identified fashion. Categorical data were compared using chi-square tests and continuous variables were compared using unpaired t tests and Wilcoxon rank sum tests. Statistical analysis was performed using SAS software (version 9.4, SAS Institute Inc., Cary, NC). An alpha level of 0.05 was used for significance.
Results
The preoperative characteristics of the pre- and post-ERAS patient cohorts are represented in Table 2. More sleeve gastrectomies were performed in the 6-month post-ERAS period (203 vs 125 cases). There were no clinically significant differences between the patient cohorts. The majority of patients were white in both groups, although patient race was more poorly recorded in the pre-ERAS cohort.
Postoperative outcomes are summarized in Table 3. Implementation of the ERAS protocol was not associated with a change in common outcomes such as length of stay, incidence of any complications, 30-day readmissions, or outpatient visits to the IV hydration clinic. There were no staple line leaks during the study period.
There was a substantial reduction in the use of postoperative narcotics associated with use of the ERAS protocol. All patients received IV narcotics prior to ERAS, while less than 50% of patients did following ERAS implementation. The use of oral narcotics was significantly reduced as well. Tramadol usage was increased in the post-ERAS group, which was by design. Also, scheduled acetaminophen and NSAIDs were universally used following the implementation of the ERAS protocol. This corresponded with a dramatic reduction in the use of oral schedule II narcotics. Most striking, implementation of the ERAS protocol resulted in a 52% reduction in the use of schedule II narcotics, with 33% of patients requiring only acetaminophen and NSAIDs for pain control. When averaged across patients, there was a 77% reduction in the use of any narcotics in the postoperative period (46.3 vs 10.8 oral morphine equivalents per patient).
Discussion
Patients undergoing laparoscopic sleeve gastrectomy with an ERAS protocol had significantly less postoperative opioid consumption compared to those not treated with this protocol. The most remarkable results include a 77% reduction in overall opioid usage and 33% of patients receiving no narcotics in the postoperative period. There were no differences in postoperative lengths of stay, readmission rates, and suggesting patients were not discharged with suboptimal pain control.
The ERAS protocol used in this study included preoperative, intraoperative, and postoperative phases. The preoperative phase included extensive nutrition counseling, oral gabapentin for 3 days prior to surgery, celecoxib 1 day before surgery, a high carbohydrate drink 2–3 h prior to surgery, and acetaminophen plus gabapentin administration in the preoperative area immediately prior to proceeding to the operating room. The intraoperative phase, generally, included adhering to basic surgical principles; goal directed fluid administration, maintaining adequate oxygenation, avoiding hypothermia and minimal tissue handling. Postoperatively, the main components include the use of a multimodal analgesia regimen, trying to avoid opioids as much as possible, early enteral nutrition, and encouraging early ambulation. Some elements of other ERAS protocols were unnecessary for laparoscopic sleeve gastrectomy (bowel preparation, epidural administration, tubes, and drains) and were thus omitted.
Our focus in this study was on the difference in opioid use pre- and post-ERAS implementation. The opioid epidemic currently affecting the USA is multifactorial, but certainly involves the use and abuse of prescription opioid medications. The increase in prescription-opioid-related overdoses rose in association with increases opioid prescribing starting in the 1990s.24 Opioid use for acute pain after surgery is certainly not the cause of the epidemic, but it cannot be easily separated from this epidemic either. For instance, a study looking at opioid use 1 year after surgery showed a 44% increase in chronic use in patients who were prescribed opioid within 7 days of surgery compared to those who were not.11 Bariatric surgery patients are at an especially high risk for chronic addiction. Many of these patients have chronic knee and back pain secondary to their morbid obesity and have been shown to have higher rates of persistent opioid use compared to patients undergoing other general surgical procedures.15 Quality and patient safety are also affected as opioid-related adverse drug events, such as respiratory depression and failure, contribute to increased patient morbidity and cost.25 Thus, it should be the goal of any responsible surgeon to attempt to minimize postoperative use both in the hospital setting and after discharge. One third of our patients did not require any postoperative opioid analgesia when using the ERAS pathway. This is in comparison to 100% of patients prior to ERAS implementation. This suggests that it is feasible to target, as a goal, an opioid-free hospital stay.
However, some patients will need a medication stronger than acetaminophen or NSAIDs to manage their postoperative pain, and tramadol is a good alternative to classic oral opioids. Tramadol has a dual analgesic mechanism with weak opioid receptor activity and monoamine reuptake inhibition. Its side effect profile is therefore more favorable with less addictive properties: less nausea and less constipation than classic opioids, with comparable pain control.22, 26, 27 We made a conscious effort to encourage use of tramadol as a first-line agent in patients who had persistent pain after the use of non-opioid alternatives.
Our study was somewhat limited in its scope, a result of the retrospective design. We did not set out to determine what elements of the ERAS pathway were able to lead to less opioid use, or how patients’ opioid consumption was affected over longer time periods. Our primary endpoints, total morphine equivalents used and number of patients who avoided opioids completely, were only studied in the immediate postoperative period. Additionally, we did not show significant changes in length of stay, readmission rates, or complication rates. This is likely due to the short length of stay and low rates of complications and readmissions even in our pre-ERAS time period.
Conclusion
ERAS implementation has been associated with improvements in quality measured in a variety of ways.28 This study contributes to the existing literature documenting the improvements in quality by significantly decreasing in-hospital opioid use after implementing an ERAS protocol for laparoscopic sleeve gastrectomy. We feel an opioid-free hospital stay and postoperative course should be the goal when performing this operation and this study proves that it is feasible. Moreover, these findings may potentially be extrapolated to a multitude of laparoscopic procedures in an effort to curb the current overuse of schedule II opioids for surgical pain control.
References
Małczak P, Pisarska M, Piotr M, Wysocki M, Budzyński A, Pędziwiatr M. Enhanced Recovery after Bariatric Surgery: Systematic Review and Meta-Analysis. Obes Surg. 2017;27(1):226–35. doi:https://doi.org/10.1007/s11695-016-2438-z.
Egli F, Hofer S, Greminger P, Rhyner K. [Combined GM-CSF and erythropoietin therapy in myelodysplastic syndrome]. Schweiz Med Wochenschr. 1989;119(49):1777–80.
Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–17.
King AB, Spann MD, Jablonski P, Wanderer JP, Sandberg WS, McEvoy MD. An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea. Surg Obes Relat Dis. 2018;14(6):849–56. doi:https://doi.org/10.1016/j.soard.2018.02.010.
Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, Francis N et al. Guidelines for perioperative care in elective colonic surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations. World J Surg. 2013;37(2):259–84. doi:https://doi.org/10.1007/s00268-012-1772-0.
Gerrish AW, Fogel S, Lockhart ER, Nussbaum M, Adkins F. Opioid prescribing practices during implementation of an enhanced recovery program at a tertiary care hospital. Surgery. 2018;164(4):674–9. doi:https://doi.org/10.1016/j.surg.2018.06.034.
Cavallaro PM, Milch H, Savitt L, Hodin RA, Rattner DW, Berger DL et al. Addition of a scripted pre-operative patient education module to an existing ERAS pathway further reduces length of stay. Am J Surg. 2018;216(4):652–7. doi:https://doi.org/10.1016/j.amjsurg.2018.07.016.
Varadhan KK, Lobo DN, Ljungqvist O. Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin. 2010;26(3):527–47, x. doi:https://doi.org/10.1016/j.ccc.2010.04.003.
Bakker N, Cakir H, Doodeman HJ, Houdijk AP. Eight years of experience with Enhanced Recovery After Surgery in patients with colon cancer: Impact of measures to improve adherence. Surgery. 2015;157(6):1130–6. doi:https://doi.org/10.1016/j.surg.2015.01.016.
Singh PM, Panwar R, Borle A, Goudra B, Trikha A, van Wagensveld BA et al. Efficiency and Safety Effects of Applying ERAS Protocols to Bariatric Surgery: a Systematic Review with Meta-Analysis and Trial Sequential Analysis of Evidence. Obes Surg. 2017;27(2):489–501. doi:https://doi.org/10.1007/s11695-016-2442-3.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30. doi:https://doi.org/10.1001/archinternmed.2011.1827.
Kelly MA. Current Postoperative Pain Management Protocols Contribute to the Opioid Epidemic in the United States. Am J Orthop (Belle Mead NJ). 2015;44(10 Suppl):S5–8.
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251.
Li L, Wu LT. Substance use after bariatric surgery: A review. J Psychiatr Res. 2016;76:16–29. doi:https://doi.org/10.1016/j.jpsychires.2016.01.009.
Mohanty S, Lee JS, Ross RA, Stricklen A, Carlin AM, Ghaferi AA. New Persistent Opioid Use after Bariatric Surgery. American College of Surgeons Clinical Congress. 2017. https://www.facs.org/media/press-releases/2017/ghaferi. Accessed August 15 2018.
Awad S, Carter S, Purkayastha S, Hakky S, Moorthy K, Cousins J et al. Enhanced recovery after bariatric surgery (ERABS): clinical outcomes from a tertiary referral bariatric centre. Obes Surg. 2014;24(5):753–8. doi:https://doi.org/10.1007/s11695-013-1151-4.
Lemanu DP, Singh PP, Berridge K, Burr M, Birch C, Babor R et al. Randomized clinical trial of enhanced recovery versus standard care after laparoscopic sleeve gastrectomy. Br J Surg. 2013;100(4):482–9. doi:https://doi.org/10.1002/bjs.9026.
Barreca M, Renzi C, Tankel J, Shalhoub J, Sengupta N. Is there a role for enhanced recovery after laparoscopic bariatric surgery? Preliminary results from a specialist obesity treatment center. Surg Obes Relat Dis. 2016;12(1):119–26. doi:https://doi.org/10.1016/j.soard.2015.03.008.
Mannaerts GH, van Mil SR, Stepaniak PS, Dunkelgrün M, de Quelerij M, Verbrugge SJ et al. Results of Implementing an Enhanced Recovery After Bariatric Surgery (ERABS) Protocol. Obes Surg. 2016;26(2):303–12. doi:https://doi.org/10.1007/s11695-015-1742-3.
Matłok M, Pędziwiatr M, Major P, Kłęk S, Budzyński P, Małczak P. One hundred seventy-nine consecutive bariatric operations after introduction of protocol inspired by the principles of enhanced recovery after surgery (ERAS®) in bariatric surgery. Med Sci Monit. 2015;21:791–7. doi:https://doi.org/10.12659/MSM.893297.
Pimenta GP, Capellan DA, de Aguilar-Nascimento JE. Sleeve Gastrectomy With or Without a Multimodal Perioperative Care. A Randomized Pilot Study. Obes Surg. 2015;25(9):1639–46. doi:https://doi.org/10.1007/s11695-015-1573-2.
Klotz U. Tramadol--the impact of its pharmacokinetic and pharmacodynamic properties on the clinical management of pain. Arzneimittelforschung. 2003;53(10):681–7. doi:https://doi.org/10.1055/s-0031-1299812.
DEA. Drug Scheduling. https://www.dea.gov/druginfo/ds.shtml. Accessed July 25 2018.
Guy GP, Zhang K, Bohm MK, Losby J, Lewis B, Young R et al. Vital Signs: Changes in Opioid Prescribing in the United States, 2006-2015. MMWR Morb Mortal Wkly Rep. 2017;66(26):697–704. doi:https://doi.org/10.15585/mmwr.mm6626a4.
Shafi S, Collinsworth AW, Copeland LA, Ogola GO, Qiu T, Kouznetsova M et al. Association of Opioid-Related Adverse Drug Events With Clinical and Cost Outcomes Among Surgical Patients in a Large Integrated Health Care Delivery System. JAMA Surg. 2018;153(8):757–63. doi:https://doi.org/10.1001/jamasurg.2018.1039.
O'Connor EC, Mead AN. Tramadol acts as a weak reinforcer in the rat self-administration model, consistent with its low abuse liability in humans. Pharmacol Biochem Behav. 2010;96(3):279–86. doi:https://doi.org/10.1016/j.pbb.2010.05.018.
Preston KL, Jasinski DR, Testa M. Abuse potential and pharmacological comparison of tramadol and morphine. Drug Alcohol Depend. 1991;27(1):7–17.
Wick EC, Grant MC, Wu CL. Postoperative Multimodal Analgesia Pain Management With Nonopioid Analgesics and Techniques: A Review. JAMA Surg. 2017;152(7):691–7. doi:https://doi.org/10.1001/jamasurg.2017.0898.
Acknowledgements
The authors would like to acknowledge Kristina Arnold for her assistance with data acquisition and Koffi Wima for his assistance with data analysis.
Author information
Authors and Affiliations
Contributions
RH designed the study and drafted the manuscript; RH, AS, and KS acquired the data; all authors interpreted the data, revised the manuscript, gave final approval of the manuscript, and are accountable for the work and its integrity.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hoehn, R.S., Seitz, A.P., Singer, K.E. et al. Enhanced Recovery Protocol for Laparoscopic Sleeve Gastrectomy: Are Narcotics Necessary?. J Gastrointest Surg 23, 1541–1546 (2019). https://doi.org/10.1007/s11605-018-04091-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-04091-y