Abstract
The prognostic implications of the expression patterns of three tumor markers, alpha-fetoprotein (AFP), the Lens culinaris agglutinin-reactive fraction of AFP (AFP-L3) and des-γ-carboxy prothrombin (DCP), have been evaluated in patients with hepatocellular carcinoma (HCC). From January 1994 to December 2014, 1182 consecutive patients underwent hepatic resection and surgical microwave ablation for HCC at our institution. This study analyzed 475 patients within the Milan criteria and Child–Pugh class A. Cumulative overall survival (OS) and disease-free survival (DFS) rates were analyzed relative to the number of positive tumor markers. OS and DFS at 5 years postoperatively were 85.3 and 44.2% in triple-negative patients, 79.4 and 48.0% in single-positive patients, 56.2 and 32.9% in double-positive patients, and 61.7 and 35.7% in triple-positive patients with statistical significance. OS in triple-negative or single-positive patients was 85.3%, and that in all double- or triple-positive patients was 58.0% (P < 0.0001); DFS at 5 years postoperatively in these two groups was 45.9 and 34.0%, respectively (P < 0.0013). Both double- and triple-positive tumor markers are associated with early recurrence and poor survival in HCC patients within the Milan criteria and Child–Pugh class A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide, and the third leading cause of cancer-related deaths 1. HCC often occurs in patients with chronic hepatitis or liver cirrhosis, such as hepatitis C virus infection or hepatitis B virus infection 2. Curative treatment modalities for HCC include hepatectomy, local ablation, and liver transplantation, with the therapeutic strategy determined mainly by the tumor number, tumor size, and liver function. The Milan criteria, namely a solitary tumor of 5 cm or less in diameter or three lesions or fewer with a largest diameter of 3 cm, no macroscopic vascular invasion and no extrahepatic involvement, was the most well-established criteria for liver transplantation for HCC 3. HCC within the Milan criteria is defined as early stage and has been reported associated with a low recurrence rate and good prognosis 4. However, we have encountered patients within the Milan criteria with poor prognosis and early recurrence after curative treatment. Although several studies have evaluated the prognostic factors in these patients 4 , 5, determination of the malignant potential of HCC within the Milan criteria before curative treatment remains an important issue.
In addition to imaging methods, such as ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI), three tumor markers are measured when diagnosing HCC in Japan: alpha-fetoprotein (AFP), Lens culinaris agglutinin-reactive fraction of AFP (AFP-L3) and des-γ-carboxy prothrombin (DCP), also called protein induced by vitamin K absence/antagonist-II (PIVKA-II). These tumor makers are useful not only for the detection and diagnosis of HCC but for evaluating the malignant potential of these tumors and predicting patient prognosis 6 , 7.
Although several studies have evaluated the association between the number of positive tumor markers and prognosis in patients with HCC 8 – 10, those studies included patients with Child-Pugh class B and those who exceeded the Milan criteria. Because HCC often occurs in patients with chronic hepatitis or liver cirrhosis, liver function, as well as tumor malignancy, is important in determining patient prognosis 2. Accordingly, this study retrospectively evaluated the influence of the expression pattern of these three tumor markers on the prognosis of patients with HCC who met the Milan criteria and had Child-Pugh class A liver function.
Methods
Patients and Diagnosis
From July 1994 to December 2014, 1182 patients underwent hepatic surgery, including hepatectomy and surgical microwave ablation (microwave coagulo-necrotic therapy [MCN]), for primary HCC in the Department of Hepato-Biliary-Pancreatic Surgery at Kyushu Medical Center. Preoperative serum samples from 986 of these patients were available, including from 475 patients who were within the Milan criteria and had Child-Pugh class A liver function. HCCs in each patient were preoperatively diagnosed and staged by several imaging modalities, including US, dynamic CT and/or enhanced MRI, with the final diagnosis of HCC confirmed by pathologic examination of tumor biopsy and/or resected specimens. This retrospective study was conducted in accordance with the Declaration of Helsinki and the ethical guidelines for clinical studies of the Ministry of Health, Labor and Welfare in Japan. The study protocol was approved by the Ethics Committee on Clinical Investigations of Kyushu Medical Center.
Measurement of HCC Tumor Markers
Serum concentrations of AFP, AFP-L3, and DCP were measured within 1 week before surgery. Serum AFP concentrations were measured using a chemiluminescent enzyme immunoassay (Siemens Immulite AFP IV, Mitsubishi Chemical Medience, Tokyo, Japan). Serum AFP-L3 concentrations were determined by lectin affinity electrophoresis coupled with antibody-affinity blotting (AFP-L3 Test Wako, Wako Pure Chemical Industries, Ltd., Osaka, Japan), with AFP-L3 concentrations expressed as a percentage of total AFP (AFP-L3/total AFP × 100). Serum DCP concentrations were determined by chemiluminescent enzyme immunoassays (Lumipulse PIVKA-II Eisai, Eisai, Tokyo, Japan). Based on previous studies, the upper limits of the normal ranges of AFP, AFPL3, and DCP in our institution were 20 ng/mL, 10%, and 40 mAU/mL, respectively 8 , 10. Tumor markers higher than the upper normal range were defined as positive markers for HCC. Patients were classified according to the number of positive tumor markers as “triple negative”, “single positive”, “double positive”, or “triple positive”.
Treatment and Surveillance
MCN and hepatectomy were performed by the same surgical team of dedicated liver surgeons led by at least one consultant specialist. We have opted for MCN for locoregional therapy with surgical approaches since 1994, and the procedure for MCN is well established. For the patients with the tumor of 3 cm or less in diameter, MCN was considered as the first choice treatment, regardless of liver function 11. Hepatectomy was considered in patients with a small number of tumors located in regions suitable for hepatectomy, such as the surface or edge of the liver. Hepatectomy was also considered the primary treatment for patients having tumors >3 cm in diameter. MCN was generally selected for patients with tumors >3 cm in diameter, insufficient liver function, or high operative risk associated with general condition, and as well as for patients who refused hepatectomy.
All MCN procedures were performed as reported 11 – 13. Microwaves at a frequency of 2450 MHz were generated by a Microtaze generator (Alfresa Pharma, Osaka, Japan). MCN requires repeat electrode insertion and irradiation from the tumor edge to the tumor center to avoid increases in intratumoral pressure, as the latter may cause multiple scattered recurrences or intrahepatic dissemination. Therefore, an open approach, such as thoracotomy, laparotomy, or laparoscopy, was used for MCN in all patients who underwent routine intraoperative US to identify lesions and monitor the effects of treatment.
Postoperative follow-up every 2 months included US and laboratory parameters, including tumor markers (AFP, AFP-L3, and DCP), with radiological assessment (dynamic CT or enhanced MRI) performed every 3–5 months. All patients were followed-up at our institution, for a median of 51.8 months (range, 4.1–212.2 months) until June 2015. When recurrent tumors were found, regardless of the type of recurrence, MCN or hepatectomy was again attempted, based on the same criteria used to select treatment for the initial tumor. However, if hepatectomy or MCN was thought unsuitable for the treatment of multiple recurrences, TACE or hepatic arterial infusion chemotherapy was performed. Patient with distant metastases were usually treated with the molecular targeting agent sorafenib.
Statistical Analysis
Continuous variables were compared using unpaired t tests and categorical variables using Fisher’s exact test or the χ 2 test. Overall survival (OS) was defined as the interval from surgery to death or the date of the last or most recent follow-up visit. Disease-free survival (DFS) was defined as the interval from initial treatment to the first treatment for recurrence. Survival curves were calculated by the Kaplan–Meier method and compared by the log-rank test. A Cox proportional hazard’s model was used for multivariate analyses of factors related to survival and recurrence. Variables analyzed included age, sex, presence of hepatitis B surface antigen (HBsAg), presence of hepatitis C antibody (HCVAb), serum concentrations of albumin and total bilirubin, prothrombin time (PT), indocyanine green dye retention rate at 15 min (ICGR15), maximum tumor size, number of tumors, surgical procedures, and number of positive tumor markers. The cut-off values for albumin, total bilirubin, and PT were essentially based on Child-Pugh score 14, and the cut-off value of ICGR15 was based on the definition of liver damage, as determined by the General Rules for the Clinical and Pathological Study of Primary Liver Cancer developed by the Liver Cancer Study Group of Japan 15.
All statistical analyses were performed using the JMP 12 software package (SAS Institute Inc., Cary, NC, USA). All P values were derived from two-tailed tests, with P < 0.05 considered statistically significant.
Results
Patient Characteristics and Numbers of Positive Tumor Markers
The 475 patients included 300 men (63.2%) and 175 women (36.8%), of mean age 68.5 ± 9.4 years (range, 41–91 years). The etiology underlying HCC was hepatitis C virus infection in 321 patients (67.6%) and hepatitis B virus infection in 75 (15.8%). Of these 475 patients, 378 (79.6%) underwent MCN, 85 (17.9%) underwent hepatectomy, and 12 (2.5%) underwent both simultaneously. Serum AFP, AFP-L3, and DCP concentrations over the upper normal ranges were observed in 206 (43.5%), 130 (27.5%), and 200 (42.1%) patients, respectively. According to qualitative evaluation of these three tumor markers, 154 patients (32.4%) were triple negative, 171 patients (36.0%) were single positive [AFP (n = 70), AFP-L3 (n = 10), DCP (n = 91)], 84 patients (17.7%) were double positive [AFP and AFP-L3 (n = 41), AFP and DCP (n = 30), DCP and AFP-L3 (n = 10)], and 66 patients (13.9%) were triple positive (Fig. 1). Table 1 shows the demographic and clinical characteristics of these patients according to the number of positive tumor markers. Among these 4 groups, no significant differences were observed in age, HBsAg, HCVAb, serum level of albumin, total bilirubin, prothrombin time, number of tumors, or surgical procedures. On the contrary, sex, ICGR15, and the maximum size of the tumor were different among the four groups.
Comparison of Pathological Findings According to the Number of Positive Tumor Markers
Pathological findings after surgery were compared according to the number of positive tumor markers (Fig. 2). Poorly differentiated tumor (triple negative, 4.0%; single positive, 10.1%; double positive, 12.0%; triple positive, 13.0%) and microvascular invasion (triple negative, 17.4%; single positive, 34.8%; double positive, 57.1%; triple positive, 66.7%) were significantly different among the four groups.
Patient Prognosis
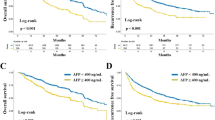
Overall Survival Based on Elevations in each Tumor Maker
Figure 3 shows the overall survival curves based on elevations in each tumor marker. The overall survival rates in patients with any elevated tumor marker was significantly lower than that in patients without any elevated tumor markers (AFP P < 0.0001, AFP-L3 P < 0.0001, and DCP P = 0.040, respectively).
Overall Survival and Disease-Free Survival Based on Surgical Procedure
The overall survival rates for all 475 patients were 98.3, 87.2, 74.7, and 44.5%, at 1, 3, 5, and 10 years after surgery, respectively. The overall survival rates for the patients treated with MCN were 98.1, 87.3, 74.8, and 43.7%, at 1, 3, 5, and 10 years, respectively, and in those for the patients treated with hepatectomy, the rates were 98.7, 88.6, 73.3, and 43.3%. There were no significant differences among the surgical procedures (P = 0.828).
The disease-free survival rates for all 475 patients were 90.9, 63.0, 42.2, and 24.4%, at 1, 3, 5, and 10 years after surgery, respectively. The disease-free survival rates for the patients treated with MCN were 91.6, 61.9, 41.3, and 25.1%, at 1, 3, 5, and 10 years, respectively, and in those for the patients treated with hepatectomy, the rates were 89.0, 69.7, 48.7, and 27.6%. There were no significant differences among the surgical procedures (P = 0.274).
Overall Survival Based on the Number of Positive Tumor Markers
The overall survival rates at 1, 3, 5, and 10 years after surgery were 99.3, 93.4, 85.3, and 59.5% in triple negative patients, 98.8, 90.1, 79.4, and 42.2% in single positive, 98.8, 81.8, 56.2, and 31.7% in double positive, and 93.8, 73.3, 61.7, and 28.1% in triple positive, respectively (Fig. 4a). The triple positive group had significantly worse overall survival compared with triple negative and single positive (P = 0.0001 and 0.014, respectively). In contrast, there were no significant differences between double positive and triple positive (P = 0.868).
Overall survival and disease-free survival curves based on the number of positive tumor markers. *P < 0.05 by the log-rank test. a Overall survival was significantly poorer in the group of triple positive than in the group of triple negative (P = 0.0001) or the group of single positive (P = 0.014), but there were no significant differences between the group of double positive and the group of triple positive (P = 0.868). b Disease-free survival was also significantly poorer in the group of triple positive than in the group of triple negative (P = 0.017) or the group of single positive (P = 0.027), but there were no significant differences between the group of double positive and the group of triple positive (P = 0.852)
Disease-Free Survival Based on the Number of Positive Tumor Markers
The disease-free survival rates at 1, 3, 5, and 10 years after surgery were 95.3, 73.9, 44.2, and 24.1% in triple negative patients, 93.9, 63.9, 48.0, and 25.0% in single positive, 87.9, 49.1, 32.9, and 25.0% in double positive, and 75.9, 52.5, 35.7, and 25.1% in triple positive, respectively (Fig. 4b). The triple positive group had significantly lower disease-free survival compared with triple negative and single positive (P = 0.017 and 0.027, respectively). Conversely, there were no significant differences between double positive and triple positive (P = 0.852).
Patients were subsequently divided into the group of triple negative or single positive and the group of double or triple positive and their OS and DFS rates compared. The postoperative 1, 3, 5, and 10 years OS rates were 99.0, 91.7, 82.5, and 51.5%, respectively in the group of triple negative or single positive, and 97.3, 78.0, 58.0, and 30.5%, respectively in the group of double positive or triple positive (P < 0.0001; Fig. 5a). In addition, the postoperative 1, 3, 5, and 10 years DFS rates were 94.6, 68.8, 45.9, and 24.4%, respectively, in the group of triple negative or single positive, and 82.8, 50.5, 34.0, and 25.2%, respectively, in the group of double positive or triple positive (P = 0.0013, Fig. 5b).
Overall survival curves and disease free survival curves compared the group of triple negative or single positive and the group of double or triple positive. a The group of double positive or triple positive had significantly worse overall survival compared with the group of triple negative or single positive (P < 0.0001). b The group of double positive or triple positive had significantly lower disease-free survival compared with the group of triple negative or single positive (P = 0.0013)
Factors Associated with Overall Survival Rates
The factors associated with OS were evaluated by univariate and multivariate analyses (Table 2). Univariate analysis revealed that HCVAb positivity, total bilirubin concentration > 1.0 mg/dl, PT > 80%, ICGR15 > 15%, and double or triple positive tumor markers were significantly associated with poor survival. Multivariate analysis showed that HCVAb positivity (relative risk [RR] 1.98, 95% confidence interval [95% CI], 1.32–3.05; P = 0.0006), ICGR15 > 15% (RR 1.54, 95% CI, 1.04–2.30; P = 0.028), and double- or triple-positive tumor markers (RR 2.36, 95% CI, 1.64–3.28; P < 0.0001) were independent risk factors for OS.
Factors Associated with Disease-Free Survival Rates
The factors associated with DFS were also evaluated by univariate and multivariate analyses (Table 3). Univariate analysis revealed that HCVAb positivity, total bilirubin concentration > 1.0 mg/dl, PT >80%, ICGR15 > 15%, the presence of multiple tumors, and double- or triple-positive tumor markers were significantly predictive of poor DFS. Multivariate analysis showed that HCVAb positivity (RR 1.63, 95% CI, 1.21–2.24; P = 0.0012), ICGR15 > 15% (RR 1.38, 95% CI, 1.04–1.89; P = 0.034), the presence of multiple tumors (RR 1.47, 95% CI, 1.11–1.94; P = 0.008), and double- or triple-positive tumor markers (RR 1.61, 95% CI, 1.21–2.10; P = 0.0009) were independent risk factors for DFS.
Discussion
In the present study, we investigated the significance of three tumor markers for HCC (AFP, AFP-L3, and DCP) in predicting outcomes in patients with HCC within the Milan criteria and with Child-Pugh class A liver function undergoing curative treatment, such as hepatectomy and/or local thermal ablation. Our results demonstrated that patients who were double- or triple-positive tumor markers had significantly poorer DFS and OS than patients who were triple negative or single positive.
Three tumor markers for HCC, such as AFP, AFP-L3, and DCP, are individually used for detection of tumors and are also useful for evaluating tumor invasiveness or prognosis. AFP is the most widely used tumor marker for HCC, with elevated AFP correlating with a higher incidence of HCC and poor patient prognosis 6 , 16. AFP-L3 positivity has been associated with a larger number of tumors and a more highly malignant potential 17 , 18, and elevated DCP has been reported to correlate with a higher prevalence of portal vein invasion 7. The combination of these three tumor markers has been reported useful in evaluating patients with HCC, with the number of positive tumor markers associated with patient survival and tumor recurrence 8 – 10. These studies, however, evaluated patients with early to advanced HCC, included patients with Child-Pugh class B liver function, or included relatively few patients. In addition to the malignant potential of tumors, liver function is an important factor affecting the prognosis of patients with HCC. This study, which included 475 patients with early stage HCC within the Milan criteria and Child-Pugh class A liver function, clearly revealed the prognostic significance of the number of positive tumor markers. Previous reports have set the various cut-off values as median value, value calculated from receiver–operator characteristic analysis, upper or lower normal limit value, and values based on other reports. In this study, we defined the cut off values, 20 ng/ml for AFP, 10% for AFP-L3, and 40 mAU/ml for DCP, as the upper limits of normal in previous studies 8 – 10. This was because these values were objective and similar in different institutions.
This study revealed pathological differences among patients with different numbers of positive tumor markers. In addition to increases in tumor size, the prevalence of poorly differentiated tumors and microvascular invasion increased as the number of positive tumor markers increased, indicating an association between these markers and the high malignant potential of HCC. In this study, microvascular invasion was positive in more than half of the patients who were double or triple positive tumor markers, suggesting that the number of positive tumor markers reflects HCC progression, including microvascular invasion, not detected by preoperative imaging modalities. Our results also indicate that measuring these HCC markers is useful not only in detecting HCC but in evaluating tumor invasiveness.
Furthermore, our results may also be useful for selecting the appropriate therapeutic modality. An appropriate preoperative treatment strategy should be selected for patients at high risk of early recurrence or poor survival. The ability to predict early recurrence or poor overall survival may result in the selection of candidates for perioperative adjuvant chemotherapies or liver transplantation. However, there has been little evidence of neoadjuvant chemotherapy for HCC.
There were some limitations of the present study. First, this study included two treatment modalities, hepatectomy, and surgical microwave ablation. Although hepatectomy remains the first option for the treatment of HCC 19 , 20, local thermal ablation, such as microwave ablation and radiofrequency ablation, has become more common. 21 , 22 Operative microwave ablation, termed microwave coagulo-necrotic therapy (MCN), has been used in Japan since 1988. Saitsu et al. 23 started MCN from 1988 and first reported the efficacy of MCN for HCC in 1991. We have opted for MCN for the treatment of HCC and previously reported the feasibility and safety of MCN in patients with HCC 11. In agreement with previous findings, we found no significant differences in OS rates between patients treated with MCN and hepatectomy in this study. However, as treatment was assigned by the decision of each individual patient, some confounding factors might influence survival in this point. Second, we have repeated treatments multiple times for recurrences after first curative treatment. Though the time to recurrence after treatment is an important factor for prognosis, it is difficult to analyze the influence of treatment performed after the recurrence. Additionally, recurrence after curative treatment can include intrahepatic metastasis from the primary tumor and multicentric occurrence of new tumors that differ from the primary lesion 24. The malignant potential of the primary tumor is associated with intrahepatic metastasis, but not with multicentric tumors, which were due to the existence of chronic hepatitis or cirrhosis. In the previous studies, intrahepatic metastasis from primary tumor has been shown to mainly occur as early recurrence within 2 years after curative treatment, whereas multicentric tumors occur later, more than 2 years after curative treatment 25 , 26. The higher early recurrence rate after surgery of the group of double or triple positive tumor markers suggested that intrahepatic metastasis could occur more in the group of double or triple positive tumor marker than in the group of triple negative or single positive. However, it is difficult to differentiate precisely between intrahepatic metastasis and multicentric occurrence in clinical practice. Therefore, multivariate analyses were performed in this study to adjust these confounders. In the multivariate analyses, double- or triple-positive tumor markers were found to be an independent risk factor for early recurrence and poor survival. Our results may therefore be clinically informative for predicting tumor recurrence and survival after curative treatment. Further studies are warranted to confirm this association in other populations.
In conclusion, preoperative evaluation of three tumor markers for HCC may predict the malignant potential of the tumor and outcomes in patients who fulfill the Milan criteria and have Child–Pugh class A. Our study of 475 patients treated with curative treatment found that not only triple-positive tumor markers but double-positive tumor markers were independent risk factors for early recurrence and poor survival for the patients with early stage HCC fulfilled the Milan criteria and Child–Pugh class A.
References
Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006;24:2137–2150.
Taura N, Fukushima N, Yastuhashi H, Takami Y, Seike M, Watanabe H, Mizuta T, Sasaki Y, Nagata K, Tabara A, Komorizono Y, Taketomi A, Matsumoto S, Tamai T, Muro T, Nakao K, Fukuizumi K, Maeshiro T, Inoue O, Sata M. The incidence of hepatocellular carcinoma associated with hepatitis C infection decreased in Kyushu area. Med Sci Monit. 2011;17:PH7–11.
Mazzaferro V, Regalia E, Doci R, Andrela S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;344:693–700.
Kamiyama T, Nakanishi K, Yokoo H, Kamachi H, Tahara M, Suzuki T, Shimamura T, Furukawa H, Matsushita M, Todo S. Recurrence patterns after hepatectomy of hepatocellular carcinoma: implication of Milan criteria utilization. Ann Surg Oncol. 2009;16:1560–1571.
Sakaguchi T, Suzuki S, Morita Y, Oishi K, Suzuki A, Fukumoto K, Inaba K, Nakamura S, Konno H. Impact of the preoperative des-gamma-carboxy prothrombin level on prognosis after hepatectomy for hepatocellular carcinoma meeting the Milan criteria. Surg Today. 2010;40:638–645.
Kumada T, Nakano S, Takeda I, Kiriyama S, Sone Y, Hayashi K, Katoh H, Endoh T, Sassa T, Satomura S. Clinical utility of Lens culinaris agglutinin-reactive alpha-fetoprotein in small hepatocellular carcinoma: special reference to imaging diagnosis. J Hepatol. 1999;30:125–130.
Koike Y, Shiratori Y, Sato S, Obi S, Teratani T, Imamura M, Yoshida H, Shiina S, Omata M. Des-γ-carboxy prothrombin as a useful predisposing factor for the development of portal venous invasion in patients with hepatocellular carcinoma: a prospective analysis of 227 patients. Cancer. 2001;91:561–569.
Toyoda H, Kumada T, Kiriyama S, Sone Y, Tanikawa M, Hisanaga Y, Yamaguchi M, Kaneoka Y, Washizu J. Prognostic significance of simultaneous measurement of three tumor markers in patients with hepatocellular carcinoma. Clin Gastroenterol Hepatol. 2006;4:111–117.
Kiriyama S, Uchiyama K, Ueno M, Ozawa S, Hayami S, Tani M, Yamaue H. Triple positive tumor markers for hepatocellular carcinoma are useful predictors of poor survival. Ann Surg. 2011;254:984–991.
Nakagawa S, Beppu T, Okabe H, Okabe H, Sakamoto K, Kuroki H, Mima K, Nitta H, Imai K, Hayashi H, Sakamoto Y, Hashimoto D, Chikamoto A, Ishiko T, Watanabe M, Baba H. Triple positive tumor markers predict recurrence and survival in early stage hepatocellular carcinoma. Hepatol Res. 2014;44:964–974.
Takami Y, Ryu T, Wada Y, Saitsu H. Evaluation of intraoperative microwave coagulo-necrotic therapy (MCN) for hepatocellular carcinoma: a single center experience of 719 consecutive cases. J Hepatobiliary Pancreat Sci. 2013;20:332–341.
Ryu T, Takami Y, Tsutsumi N, Tateishi M, Mikagi K, Wada Y, Saitsu H. Simultaneous microwave coagulo-necrotic therapy (MCN) and laparoscopic splenectomy for the treatment of hepatocellular carcinoma with cirrhotic hypersplenism. Surg Today. 2016; doi: 10.1007/s00595-016-1411-1418.
Wada Y, Takami Y, Tateishi M, Ryu T, Mikagi K, Saitsu H. Efficacy of surgical treatment using microwave coagulo-necrotic therapy for unresectable multiple colorectal liver metastases. OncoTargets Ther. 2016;9:937–943.
Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649.
Liver Cancer Study Group of Japan. General rules for the clinical and pathological study of primary liver cancer, 3rd English edn. Tokyo: Kanehara Shuppan, 2010.
Tateyama M, Yatsuhashi H, Taura N, Motoyoshi Y, Nagaoka S, Yanagi K, Abiru S, Yano K, Komori A, Migita K, Nakamura M, Nagahara H, Sasaki Y, Miyakawa Y, Ishibashi H. Alpha-fetoprotein above normal levels as a risk factor for the development of hepatocellular carcinoma in patients infected with hepatitis C virus. J Gastroenterol 2011;46:92–100.
Farinati F, Marino D, De Giorgio M, Baldan A, Cantarini M, Cursaro C, Rapaccini G, Del Poggio P, Di Nolfo MA, Benvegnu L, Zoli M, Borzio F, Bernardi M, Trevisani F. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither. Am J Gastroenterol 2006;101:524–532.
Kobayashi M, Hosaka T, Ikeda K, Seko Y, Kawamura Y, Sezaki H, Akuta N, Suzuki F, Suzuki Y, Saitoh S, Arase Y, Kumada H. Highly sensitive AFP-L3% assay is useful for predicting recurrence of hepatocellular carcinoma after curative treatment pre- and postoperatively. Hepatol Res 2011;41:1036–1045.
Takayama T, Makuuchi M, Hirohashi S, Sakamoto M, Yamamoto J, Shimada K, Kosuge T, Okada S, Takayasu K, Yamasaki S. Early hepatocellular carcinoma as an entity with a high cure rate of surgical cure. Hepatology. 1998;28:1241–1246.
Belghiti J, Hiramatsu K, Benoist S, Massault PP, Sauvanet A, Farges O. Seven hundred forty-seven hepatectomies in the 1990s: an update to evaluate the actual risk of liver resection. J Am Coll Surg. 2000;191:38–46.
Liang P, Wang Y. Microwave ablation of hepatocellular carcinoma. Oncology. 2007;72:124–131.
Tateishi R, Shiina S, Teratani T, Obi S, Sato S, Koike Y, Fujishima T, Yoshida H, Kawabe T, Omata M. Percutaneous radiofrequency ablation for hepatocellular carcinoma. An analysis of 1000 cases. Cancer. 2005;103:1201–1209.
Saitsu H, Yoshida M, Taniwaki S, Sato H, Okami N, Matsumoto A, Shigetomi K, Sugiyama T, Okuda Y, Nakayama K. Laparoscopic coagulo-necrotic therapy using microtase for small hepatocellular carcinoma. Jpn J Gastroenterol. 1991;88:2727.
Takenaka K, Kawahara N, Yamamoto K, Kajiyama K, Maeda T, Itasaka H, Shirabe K, Nishizaki T, Yanaga K, Sugimachi K. Results of 280 liver resections for hepatocellular carcinoma. Arch Surg 1996;131:71–76.
Kobayashi A, Miyagawa S, Miwa S, Nakata T. Prognostic impact of anatomical resection on early and late intrahepatic recurrence in patients with hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 2008;15:515–1521.
Yamamoto J, Kosuge T, Takayama T, Shimada K, Yamasaki S, Ozaki H, Yamaguchi N, Makuuchi M. Recurrence of hepatocellular carcinoma after surgery. Br J Surg 1996;83:1219–1222.
Author information
Authors and Affiliations
Contributions
Study conception and design: Ryu, Takami, and Saitsu Acquisition of data: Ryu, Wada, Tateishi, Matsushima, and Mikagi Analysis and interpretation of data: Ryu, Takami, and Saitsu Drafting of manuscript: Ryu Critical revision: Saitsu
Corresponding author
Ethics declarations
This retrospective study was conducted in accordance with the Declaration of Helsinki and the ethical guidelines for clinical studies of the Ministry of Health, Labor and Welfare in Japan. The study protocol was approved by the Ethics Committee on Clinical Investigations of Kyushu Medical Center.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Grant Support
None
Rights and permissions
About this article
Cite this article
Ryu, T., Takami, Y., Wada, Y. et al. Double- and Triple-Positive Tumor Markers Predict Early Recurrence and Poor Survival in Patients with Hepatocellular Carcinoma within the Milan Criteria and Child-Pugh Class A. J Gastrointest Surg 21, 957–966 (2017). https://doi.org/10.1007/s11605-017-3394-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-017-3394-1