Abstract
Background
Although minimally invasive surgery (MIS) has been associated with improved postoperative clinical outcomes, the widespread use of MIS by procedure and hospital has been limited. We sought to report on national trends postoperative clinical outcomes for minimally invasive liver and pancreatic surgery.
Methods
Patients undergoing an elective liver or pancreatic resection were identified using the Nationwide Inpatient Sample between 2002 and 2012. Multivariable regression analysis was used to compare postoperative outcomes, and total hospital costs between patients who underwent a MIS versus an open resection over the study time period.
Results
A total of 47,685 patients were identified; 21,280 (44.6 %) patients underwent a hepatic resection while 26,405(55.4 %) patients underwent a pancreatic resection. MIS was performed in 2674 (5.6 %) patients and increased from 2.6 % in 2002 to 9.6 % in 2012 (p < 0.001); this trend was observed for both pancreatic and liver resections (both p < 0.001). Over the study time period, use of MIS was consistently associated with improved postoperative outcomes including decreased postoperative morbidity (open vs. MIS: 32.9 vs. 29.6 %) and a shorter length-of-stay (≤4 days; MIS, 21.4 %; Open, 13.7 %; both p < 0.05). The median costs associated with MIS decreased over time compared with the open surgical approach and were on average $572 lower than the cost associated with open surgery.
Conclusion
Compared to open resection, MIS was associated with lower postoperative morbidity, a shorter length-of-stay, and lower cost. The use of MIS should be encouraged in order to improve postoperative outcomes and decrease healthcare spending via value enhancement.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the past decade, the use of minimally invasive surgery (MIS) for several gastrointestinal and cardiothoracic surgical procedures has increased.1 – 4 The increase in utilization of MIS approaches has largely been attributed to patient demand, as well as data demonstrating improved perioperative outcomes associated with MIS compared with traditional open surgery.5 – 7 For example, Vanounou et al. reported a shorter length-of-stay (LOS), as well as a reduced postoperative morbidity, among patients undergoing laparoscopic versus open hepatic resection.8 Similarly, Delaney et al. reported fewer complications, lower mortality, and shorter intensive care unit stays among patients undergoing laparoscopic colectomy compared with patients who underwent an open colectomy.3
Of particular interest and debate has been the potential increased cost associated with MIS surgery, which may contribute to a more limited acceptance of MIS. Specifically, while several reports have suggested comparable healthcare costs for certain MIS versus open surgical procedures, other investigators have reported higher overall costs associated with MIS.4 , 8 , 9 In turn, these authors have suggested that some of the increased costs may be offset via healthcare savings derived from improved perioperative outcomes associated with MIS.4 , 8 , 9 To this point, Nakajima et al. reported lower overall hospital charges associated with minimal invasive thoracic surgery compared with open thoracotomy.9 Although previous reports have compared perioperative clinical outcomes following MIS hepato-pancreatico-biliary (HPB) surgery, data examining the trends in the overall utilization of MIS as well as the potential financial implications associated with the use of MIS HPB surgery are lacking. Given this, the objective of the current study was to examine national trends in the utilization of MIS among patients undergoing liver and pancreatic resection. More specifically, we sought to compare perioperative clinical outcomes, as well as financial costs among patients undergoing MIS versus open liver and pancreatic resection.
Methods
Data Sources and Patient Population
A retrospective cohort study was performed using data from the National (formerly Nationwide) Inpatient Sample (NIS). The NIS is maintained by the Agency for Healthcare Research and Quality and represents the largest all-payer inpatient care database in the USA including information from over 7 million hospital stays.10 Data contained within the NIS is publicly available, de-identified, and compliant with the Health Insurance Portability and Accountability Act of 1996.10 Additional details regarding the data elements contained within the NIS have been previously described.10 This study was approved by the Johns Hopkins University Institutional Review Board.
International Classification of Disease (ICD-9-CM) procedure codes (Supplemental Table 1) were used to identify patients who underwent a liver or pancreatic resection between 2002 and 2012. Patients undergoing an emergent operation were excluded from the final study population. MIS was classified as liver or pancreatic resections and sub-classified as either robotic or laparoscopic approach. Preoperative comorbidity was classified using the Charlson comorbidity index (CCI) and patients were categorized into five categories according to their CCI score (CCI = 0, 1, 2, 3, and ≥4). Perioperative complications were defined as the occurrence of one or more complications categorized using previously validated codes for perioperative complications. In particular, complications included surgical site infections, wound or fascial dehiscence, pneumonia, sepsis, myocardial infarctions, and gastrointestinal bleeding (Supplemental Table 2). LOS was examined as a continuous variable as well as a categorical and binary variable. Specifically, LOS was dichotomized at the 75th percentile for each procedure group (liver and pancreas) whereby an “extended LOS” was defined as LOS ≥8 days following a liver resection and ≥10 days following a pancreatic resection. Discharge disposition was categorized such that a patient who was discharged home was classified as a “routine discharge,” while patients discharged to facilities requiring additional care was classified as a “non-routine discharge.”
For each patient record, the NIS collects total charges submitted, which represent the total amount charged by hospitals for an inpatient episode of care including perioperative and hospital charges. Cost-to-charge ratios represent the ratio between the total charges submitted and the actual costs of care; cost-to-charge ratios are calculated by the Agency for Healthcare Research and Quality using data collected under the Healthcare Cost Report Information System for Medicare. Using hospital-specific cost-to-charge ratios, total inpatient hospitalization costs for each episode of care were estimated. All financial variables were inflation adjusted and reported to 2012 US dollars using the Gross Domestic Product Implicit Price Deflator.11 , 12
Statistical Analysis
Continuous variables were compared using the non-parametric Kruskal-Wallis test while categorical variables were compared using Pearson’s chi-squared test. Multivariable logistic regression analysis was used to evaluate perioperative clinical outcomes including perioperative morbidity, LOS, mortality, and discharge disposition between MIS and open surgery. Specifically, independent models were built for each type of surgery (liver and pancreas) and each model adjusted for all patient and hospital characteristics. Multivariable linear regression analysis was used to compare total inpatient costs between patients who underwent MIS versus open surgery. As cost data were non-normal and right-skewed, a Modified Park test was performed to determine the most appropriate modeling technique to be used.13The final multivariable model used a log link function with an underlying gamma distribution while adjusting for patient and hospital characteristics. Statistical significance was determined by a p value of <0.05 and all statistical analyses were performed using the STATA statistical software package, version 14.0 for windows.
Results
Baseline Patient Characteristics
A total of 47,685 patients were identified who underwent a liver or pancreatic resection between 2002 and 2012. Patient characteristics stratified by the surgical approach and the surgical procedure are presented in Table 1. Overall, 21,280 (44.6 %) patients underwent a liver resection, while 26,405 (55.4 %) patients underwent a pancreatic resection. Among the entire cohort, 52.4 % (n = 24,938) of the patients were female and 76.7 % (30,232) patients were Caucasian. Comorbidity was common with 46.6 % (n = 22,195) of patients presenting with a CCI score of ≥4. Private insurance was the most common payer type with 48.3 % (22,980) of patients enrolled in private healthcare plans followed by 56.4 % of patients enrolled in either Medicare or Medicaid.
Trends in the Use of MIS
A total of 45,011 (94.4 %) individuals had an open resection while MIS was performed in 2674 (5.6 %) patients. The use of MIS varied by the type of surgical resection and was more frequently performed among patients undergoing a pancreatic resection as 7.3 % (1777 out of 24,628) of all patients undergoing a pancreatic resection underwent a MIS compared with 4.4 % (897 out of 20,383) of patients undergoing a liver resection. As illustrated in Fig. 1a–c, the proportion of patients undergoing a MIS increased over the study period. Specifically, 2.6 % of all patients in 2002 underwent a MIS HPB procedure compared with 9.6 % of all patients undergoing surgery in 2012; in contrast, there was a steady decline in the number of open resections observed from 97.4 % in 2002 to 90.5 % in 2012 (p < 0.001). Trends in the use of MIS were also noted across different types of HPB surgery (i.e., liver vs. pancreas). For example, among patients undergoing a liver resection, 2.3 % of patients underwent a MIS in 2002 compared with 7.0 % of patients undergoing a MIS in 2012 (p < 0.001). A greater increase in the use of MIS was observed among patients undergoing a pancreatic resection with the proportion of patients undergoing a MIS increasing from 3.1 % in 2002 to 13.9 % in 2012 (p < 0.001). Of note, this trend was most pronounced among patients who underwent a distal pancreatectomy (2002 vs. 2012: 3.6 vs. 14.9 %, Fig. 1d).
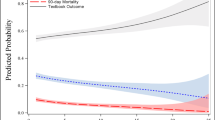
Postoperative Outcomes by Surgical Approach: MIS Vs. Open
Overall, postoperative morbidity was 32.7 % (15,608); the incidence of complications was lower among patients undergoing a MIS (MIS vs. open: 29.6 vs. 32.9 %, p < 0.001, Table 2). Interestingly, this pattern in postoperative morbidity persisted when stratified by the type of surgical procedure and was more pronounced among patients undergoing a pancreatic resection (Fig. 2a, b). On multivariable analysis, after adjusting for patient and hospital characteristics (Supplemental Tables 3a and 3b), only MIS pancreatic surgery was associated with a 16 % decreased odds for developing a postoperative complication (odds ratio [OR] = 0.84, 95 % CI 0.70–0.99). A similar trend was noted in the association between MIS and risk of morbidity following liver resection (OR = 0.92, 95 % CI 0.77–1.09). Similarly, MIS was also associated with a 13 and 33 % lower odds of an extended LOS for liver and pancreatic surgery, respectively (liver: OR = 0.87, 95 % CI 0.72–1.05; pancreas: OR = 0.67, 95 % CI 0.54–0.83, Table 3).
The overall cost for surgery was $26,146 and ranged from $26,201 following open HPB surgery to $25,173 following MIS. Of note, the median cost of MIS increased from $15,517 (IQR, $23,078–9710) in 2002 to $20,693 (IQR, $28,925–$15,365) in 2012, while the median costs associated with open surgery increased from $14,887 (IQR, $21,571–$10,698) in 2002 to $21,265 (IQR, $32,186–$15,221) in 2012 (Fig. 3a). Interestingly, costs associated with MIS and open surgery were comparable over time among patients who did not develop a postoperative complication (Fig. 3b). On multivariable analysis adjusting for patient and hospital characteristics as well as the development of postoperative complications, use of MIS was associated with a 6 % lower inpatient hospitalization cost (coefficient, 0.94; 95 % CI 0.88–0.99); this effect was more pronounced among patients undergoing pancreatic resection (coefficient, 0.92; 95 % CI 0.85–0.99) compared with patients undergoing a liver resection (coefficient, 0.99; 95 % CI 0.92–1.07, Table 3).
Discussion
Use of MIS following multiple gastrointestinal and thoracic operations has been observed to increase in recent years.14 Although MIS has been advocated as a means to improve postoperative outcomes including postoperative pain, morbidity, mortality, and LOS, the widespread implementation of the MIS approach has been limited due to concerns regarding the costs associated with MIS.15 To date, most studies that have examined trends and patterns of use of MIS following liver and pancreas surgery have not specifically examined the financial impact of minimally invasive HPB surgery. In the current study, trends in the use of MIS were evaluated using a large, nationally representative sample of patients undergoing a liver or pancreatic resection. Of note, the use of MIS increased among patients undergoing both liver and pancreatic surgical procedures with a more pronounced increase in the use of MIS for pancreatic resections. Consistent with previous reports, use of MIS was also associated with improved postoperative outcomes in the form of lower morbidity and a shorter LOS. Perhaps of greater interest, the costs of MIS remained relatively constant over the study time period and were comparable to the costs associated with open surgery in 2002. Furthermore, when accounting for differences in patient characteristics and postoperative outcomes, MIS was associated with a 6 % lower cost compared with open surgery.
Although the acceptance of MIS for hepatic and pancreatic surgical procedures has been slower compared with other abdominal surgical procedures such as cholecystectomy and colectomy, there has been an increase in the use of HPB MIS in recent years.8 The slow uptake of the MIS approach has undoubtedly been multifactorial and may have been related to concerns among surgeons regarding an increased risk of hemorrhage and difficulty in securing hemostasis, pulmonary embolism, and bile leakage.8 These concerns have, however, not been borne out as experience in MIS among surgeons has increased and more advanced surgical instruments and techniques have been developed.8 The current study is important because it provides further evidence that MIS is safe and can offer favorable outcomes among patients undergoing liver and pancreatic procedures. Zeh et al. reported potential advantages of a minimally invasive approach for pancreatic surgical procedures including reduced perioperative morbidity, reduced length of hospital stay, reduced blood loss, and a better acceptance of prophylactic pancreatectomy.16 Taking hepatic and pancreatic surgical procedures as a whole, data in the current study demonstrated a lower incidence of perioperative complications associated with MIS versus open resection (29.6 vs. 32.9 %). Considering hepatic and pancreatic surgical procedures separately, MIS still had more favorable outcomes compared with open resections. For example, patients who had an open resection for hepatic procedures were more likely to have an extended length of hospital stay versus patients who underwent MIS (23 vs. 20 %). Similarly, compared with patients who had an open resection, patients who had a MIS pancreatic resection had lower rates of postoperative complications (26 vs. 32 %), lower risk of sepsis (1 vs. 4 %), and were less likely to have an extended hospital stay (15 vs. 24 %). Consistent with our findings, Koffron et al. in their single institution experience, demonstrated that patients who underwent a MIS liver resection had a shorter length of hospital stay, lower overall complications (9.3 vs. 22 %), and lower blood loss compared with patients who underwent an open liver resection.17
Of note, there was an increased utilization of MIS among patients undergoing hepatic and pancreatic operations over time (2.6 % in 2002 and 9.5 % in 2012 for hepatic and pancreatic surgeries combined, 2.3 % in 2002 and 7 % in 2012 for hepatic surgeries alone, 3.1 % in 2002 and 13.9 % in 2012 for pancreatic surgeries alone). This observed increase in the use of MIS may be attributed to an increasing level of experience among surgeons in performing these operations using a MIS approach. Perhaps more importantly, we also examined the costs associated with MIS, as this topic has been of particular interest due to concerns regarding the potentially higher economic burden associated with MIS. To the best of our knowledge, little evidence has been provided in the literature comparing the trends in cost s associated with MIS versus open resection for hepatic and pancreatic surgical procedures. In the current study, the median cost of MIS in 2002 was $630 higher than the cost of an open resection for hepatic and pancreatic surgeries ($15,517 vs $14,887). Interesting, over time the difference in costs comparing MIS versus an open approach changed. Specifically, by 2012, the median cost of MIS was $572 lower than the cost of an open resection ($20,693 vs $21,265). The reason for the change in costs over time may related to a decrease in the cost of instruments, shorter operative times, as well as lower rates of perioperative complications. Perioperative surgical complications can increase the overall in-hospital cost; in turn, analyzing the median cost of uncomplicated hepatic and pancreatic surgeries may present a more appropriate comparison of median in-hospital costs associated with MIS versus open surgery. To this point, we compared costs among patients who did not experience a postoperative complication and noted that the median in-hospital costs of MIS versus open HPB surgery were comparable over the study time period. Furthermore, on multivariable analysis that adjusted for patient and hospital characteristics, as well as postoperative outcomes, MIS was associated with a 6 % lower total cost. Collectively, our results suggest that MIS HPB surgery was not associated with increased costs; rather, there was a modest cost savings achieved with the use of MIS.
The current study should be interpreted with several limitations, most of which are related to the use of administrative data including incomplete coding of data.18 Similarly, as with all retrospective surgery studies, there was undoubtedly some selection bias regarding who underwent an MIS versus an open HPB procedure. Specifically, as the NIS does not contain detailed clinical or provider data, we were unable to account for factors that may have influenced the use MIS including disease severity, and the extent of the surgeon’s training and experience in performing minimally invasive procedures. Furthermore, while the NIS is an all-payer database that allows for comparison of hospitals from across the country, all possible contractual discounts and agreements between the providers and the payers could not be accounted for.
In conclusion, the use of MIS for hepatic and pancreatic surgical procedures increased over the last decade. Compared with open resection, MIS was associated with lower postoperative morbidity, as well as lower total in-hospital costs. In fact, over time, the costs associated with MIS decreased and were comparable to the costs associated with open surgery. As such, the use of an MIS HPB approach should be strongly considered when assessing patients with liver and pancreatic conditions as the MIS approach may decrease healthcare spending via value enhancement.
References
Raghunandan Venkat, Barish H. Edil, Richard D. Schulick, Anne O. Lidor, Martin A. Makary, Christopher L. Wolfgang. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique. Ann Surg 2012; 255:1048–1059.
Antonio Ivan Lazzarino, Kamal Nagpal, Alex Bottle, Omar Faiz, Krishna Moorthy, Paul Aylin. Open versus minimally invasive esophagectomy trends of utilization and associated outcomes in England. Ann Surg 2010; 252: 292–298.
Conor P. Delaney, Eunice Chang, Anthony J. Senagore, Michael Broder. Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg 2008; 247: 819–824.
Terrence M. Fullum Joseph A. Ladapo Bijan J. Borah Candace L. Gunnarsson. Comparison of the clinical and economic outcomes between open and minimally invasive appendectomy and colectomy: evidence from a large commercial payer database. Surg Endosc 2010; 24:845–853.
E. M. Burns, A. Currie, A. Bottle, P. Aylin, A. Darzi and O. Faiz. Minimal-access colorectal surgery is associated with fewer adhesion-related admissions than open surgery. British Journal of Surgery 2013; 100: 152–159.
Giuseppe R. Nigri, Alan S. Rosman, Niccolò Petrucciani, Alessandro Fancellu, Michele Pisano, Luigi Zorcolo et al., Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies. Surg Endosc 2011; 25:1642–1651.
Manish M. Tiwari, Jason F. Reynoso, Albert W. Tsang, Dmitry Oleynikov. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 2011; 254:927–932.
Tsafrir Vanounou, Jennifer L. Steel, Kevin Tri Nguyen, Allan Tsung, J. Wallis Marsh, David A. Geller et al., Comparing the clinical and economic impact of laparoscopic versus open liver resection. Ann Surg Oncol; 2010 17:998–1009.
Jun Nakajima, Shinichi Takamoto, Tadasu Kohno, Toshiya Ohtsuka. Costs of videothoracoscopic surgery versus open resection for patients with of lung carcinoma. Cancer 2000; 89:2497–501.
The national inpatient sample database documentation. Available at: https://www.hcup-us.ahrq.gov/db/nation/nis/nisdde.jsp. Retrieved June 30, 2016.
Cost-to-charge ratio files: 2011 Nationwide Inpatient Sample (NIS) User Guide. Rockville (MD): Agency for Healthcare Quality and Research. Available at: https://www.hcup-us.ahrq.gov/db/state/CCR2011NISUserGuide.pdf. Retrieved June 6, 2016.
Medical Expenditure Panel Survey: using appropriate price indices for analyses of health care expenditures or income across multiple years. Agency for Healthcare Research and Quality; 2013. Available at: http://meps.ahrq.gov/mepsweb/about_meps/Price_Index.shtml. Retrieved June 6, 2016.
Method of cost estimation in CEA: Available at: http://www.uphs.upenn.edu/dgimhsr/documents/acadhlth.glick.061008.pdf. Retrieved June 10, 2016.
McCoy AC, Gasevic E, Szlabick RE, Sahmoun AE, Sticca RP. Are open abdominal procedures a thing of the past? An analysis of graduating general surgery residents’ case logs from 2000 to 2011. J Surg Educ. 2013 Nov-Dec. 70(6):683–9.
Brandon C. Chapman, Kristen DeSanto, Bulent Salman, Barish H. Edil. Open and minimally invasive pancreatic surgery—a review of the literature. Transl Cancer Res 2015; 4(6):582–607.
H.J. Zeh III, David L. Bartlett, A. James Moser. Robotic-assisted major pancreatic resection. Advances in Surgery 2011; 45: 323–340.
Alan J. Koffron, Greg Auffenberg, Robert Kung, Michael Abecassis. Evaluation of 300 minimally invasive liver resections at a single institution. Ann Surg 2007; 246: 385–394.
Haut ER, Pronovost PJ, Schneider EB. Limitations of administrative databases. JAMA 2012; 307:2589; 2589–90.
Author Contributions
Study, Concept, and Design: All authors
Acquisition, Analysis, and Interpretation of Data: All authors
Drafting of Manuscript: All authors
Critical Review of Manuscript: All authors
Final Approval for Submission: All authors
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Supplemental Table 1
(DOCX 16 kb)
Supplemental Table 2
(DOCX 16 kb)
Supplemental Table 3
(DOCX 33 kb)
Supplemental Table 4
(DOCX 37 kb)
Supplemental Table 5
(DOCX 36 kb)
Rights and permissions
About this article
Cite this article
Okunrintemi, V., Gani, F. & Pawlik, T.M. National Trends in Postoperative Outcomes and Cost Comparing Minimally Invasive Versus Open Liver and Pancreatic Surgery. J Gastrointest Surg 20, 1836–1843 (2016). https://doi.org/10.1007/s11605-016-3267-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3267-z