Abstract
Background
Fibrolamellar carcinoma (FLC) and conventional hepatocellular carcinoma (HCC) share the same American Joint Committee on Cancer (AJCC) staging. The worse survival with HCC is attributed to the underlying cirrhosis.The aim of this study was to compare stage-matched prognosis after resection of FLC and non-cirrhotic HCC.
Methods
Outcomes after resection of 65 consecutive patients with FLC and 158 non-cirrhotic patients with HCC were compared. Patients were staged according to the 7th edition AJCC staging.
Results
The AJCC stage distributions for FLC and HCC demonstrated a predominance of stage IV disease in FLC and stage I in HCC (FLC stage I—23 %, II—15 %, III—15 %, IV—46 % vs. HCC stage I—42 %, II—32 %, III—20 %, IV—6 %, p < 0.001). Among stage IV FLC patients, 81 % had isolated nodal metastases, which did not affect overall survival (OS) or recurrence-free survival (RFS). In FLC, OS was significantly affected by the number of tumors and vascular invasion (p < 0.05). Recurrent disease developed in 56 (86 %) FLC patients and was treated with repeat surgical resection in 25 (45 %) patients. Vascular invasion was associated with recurrent FLC, with 3-year RFS rates of 9 % and 35 %, with and without vascular invasion (p = 0.034). With respect to RFS, the AJCC staging did not stratify FLC patients, compared to non-cirrhotic HCC.
Conclusions
When compared to non-cirrhotic HCC, patients with FLC are not adequately stratified by AJCC staging with respect to RFS. Our results support classifying lymph node metastases in FLC as regional disease, rather than systemic disease. Important prognostic factors in FLC are the number of tumors and vascular invasion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibrolamellar hepatocellular carcinoma (FLC) accounts for 0.85 % of all primary hepatic malignancies in the USA, and its incidence rate is 0.02 cases per 100,000 person-years, which is about 100 times less common than that of conventional hepatocellular carcinoma (HCC).1 FLC occurs most commonly in adolescents and young adults without chronic liver disease or known risk factors. Histologically, FLC is characterized by well-differentiated neoplastic hepatocytes and lamellar bands of fibrosis.2 The most important prognostic factor is surgical resection, which results in 5-year overall survival rates between 30 % and 76 %.3 , 4 More patients with FLC are candidates for surgical resection than those with HCC, owing to their young age and absence of cirrhosis. Unlike conventional HCC, lymph node metastases are common in FLC, occurring in up to 70 % of patients.4 Recurrence rates as high as 100 % have been reported after surgical resection of FLC, but durable survival can be achieved with resection of recurrent disease.
Previously, FLC was considered a variant of conventional HCC. However, recent molecular studies highlight the unique tumor biology of FLC. Honeyman et al. identified a chimeric transcript in FLC, DNAJB1-PRKACA, which increases adenosine 3′,5′-monophosphate-dependent protein kinase A activity.5 This transcript has been identified in 79–100 % cases of FLC, but not in any other cancer type.6
FLC and conventional HCC share the same American Joint Committee on Cancer (AJCC) staging.7 Historically, FLC was thought to be an indolent tumor with improved prognosis compared to conventional HCC, but more recent data suggest that the higher overall survival is due to the younger age and absence of cirrhosis in patients with FLC.2 The objective of this study was to compare prognosis after resection of FLC compared to non-cirrhotic conventional HCC. We found that the AJCC staging did not stratify FLC patients with respect to recurrence-free survival. Nodal metastases, which are classified as stage IV disease, did not significantly affect overall or recurrence-free survival after resection of FLC.
Materials and Methods
Patients evaluated at the University of Texas MD Anderson Cancer Center between November 1990 and March 2015 with pathology data available after potentially curative initial surgical resection were identified from a prospectively maintained hepatobiliary database. During the same time period, 240 patients with conventional HCC underwent hepatic resection with curative intent. Absence of cirrhosis was confirmed by review of surgical pathology in 158 patients with conventional HCC. Clinicopathologic data were recorded from computerized medical records. The study was approved by the Institutional Review Board.
Major hepatectomy was defined as anatomic resection of ≥3 Couinaud segments. Patients were followed after resection with history, physical examination, laboratory evaluation, and axial imaging every 3–4 months for the first 2 years, and every 4–6 months thereafter.
Staging
Pathological staging was performed according to the 7th edition of the AJCC Staging Manual for HCC.7 Stage I is defined as a solitary tumor without vascular invasion. Stage II is solitary tumor with vascular invasion or multiple tumors ≤5 cm. Stage III includes multiple tumors >5 cm, major vascular invasion, and/or invasion of adjacent organs. Stage IV includes lymph node and distant metastases.
Statistical Analysis
Overall and recurrence-free survival rates were calculated from date of initial surgical resection using the Kaplan-Meier method and compared using the log-rank test. Categorical variables were compared using the chi-square test. Continuous variables were compared using the Wilcoxon rank-sum test. Statistical analyses were conducted using JMP software (version 11.0.0; SAS Institute Inc., Cary, NC).
Results
Comparison Between Fibrolamellar Carcinoma and Non-cirrhotic Conventional Hepatocellular Carcinoma
A comparison of clinicopathologic characteristics between patients with surgically resected FLC (n = 65) and non-cirrhotic conventional HCC (n = 158) is shown in Table 1. Non-cirrhotic conventional HCC was associated with significantly older age, non-Caucasian race, viral hepatitis, smaller tumors, and fewer major hepatectomies. The frequency of nodal metastases was 1 % among patients with conventional HCC, compared to 43 % with FLC (p < 0.001), resulting in higher prevalence of stage IV disease in FLC compared to conventional HCC (46 % vs. 6 %, p < 0.001).
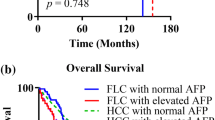
Five-year and median overall survival rates after resection of non-cirrhotic conventional HCC were 67 % and 137 months (95 % confidence interval [CI], 89–184 months), similar to 5-year and median overall survival rates of 58 % and 81 months (95 % CI, 42–120 months) after resection of FLC (Fig. 1). In contrast, recurrence-free survival was significantly longer for patients with conventional HCC, whose 5-year and median recurrence-free survival rates were 55 % and 108 months, compared to 10 % and 11 months (95 % CI, 8–14 months) after resection of FLC (p < 0.001). AJCC staging stratified recurrence-free survival for patients with conventional HCC but not FLC (Fig. 2).
Stage IV Disease in Fibrolamellar Carcinoma Patients
Among the 31 patients presenting with stage IV disease, 25 (81 %) patients had isolated nodal metastases, 3 (5 %) had isolated pulmonary metastases, and 3 (5 %) had nodal and extrahepatic metastases in the lung (n = 2) and diaphragm (n = 1). Eleven patients presented with metastases in multiple nodal basins. At presentation, nodal basins most commonly involved were the hepatoduodenal ligament (n = 22), gastrohepatic ligament (n = 9), celiac (n = 5), retroperitoneal (n = 5), and cardiophrenic (n = 4). All 9 patients with metastases in gastrohepatic ligament nodes had primary tumors in the left liver.
Predictors of Survival and Recurrence in Fibrolamellar Carcinoma Patients
On univariate analysis, predictors of overall survival were the presence of vascular invasion and multiple tumors (Table 2). Five-year overall survival rates were 25 % vs. 67 % with multiple vs. solitary tumors, respectively (p = 0.001), and 45 % vs. 72 %, with and without vascular invasion (p = 0.040). Lymph node metastases were not significantly associated with overall survival; 5-year overall survival rates were 42 % and 67 %, with and without nodal metastases (p = 0.15, Fig. 3).
Recurrent disease was observed in 56 (86 %) patients after resection of FLC. Longer recurrence-free survival was associated with absence of vascular invasion and age > 25 years. Three-year recurrence-free survival rates were 9 % vs. 35 %, with and without vascular invasion (p = 0.034). The most common sites of first recurrence were intra-abdominal and/or intrathoracic lymph nodes (n = 17), liver (n = 11), lungs (n = 11), liver and lymph nodes (n = 7), and peritoneum (n = 5). Surgical resection of recurrent disease was associated with median overall survival of 122 months, compared to 37 months without surgical resection (p = 0.001, Fig. 4). Among the 31 patients who did not undergo resection of recurrent disease, 12 (39 %) patients had widespread, unresectable disease and/or progression on systemic therapy.
Discussion
Fibrolamellar carcinoma (FLC) has been considered a variant of conventional hepatocellular carcinoma (HCC) and shares the same American Joint Committee on Cancer (AJCC) staging system. However, unlike conventional HCC, FLC occurs most commonly in adolescents and young adults without underlying liver disease and normal serum alpha-fetoprotein levels. Historically, FLC was considered an indolent disease due to case reports of long-term survival after resection or transplantation.1 , 8 However, more recent data demonstrate that the perceived better prognosis with FLC over HCC is due to the younger age and absence of cirrhosis in FLC patients.9 In this study, we compared patients undergoing surgical resection of FLC and non-cirrhotic conventional HCC. Similar to previous reports, we found that patients with FLC had similar overall survival as patients with non-cirrhotic HCC but significantly shorter recurrence-free survival. FLC patients presented with more advanced stage, primarily due to lymph node metastases, which did not affect prognosis. Despite high recurrence rates, durable overall survival was achieved with surgical resection of recurrent disease.
The current report affirms prior studies showing epidemiologic differences between patients with FLC and non-cirrhotic conventional HCC. FLC patients were younger, more often Caucasian, and none had viral hepatitis. Compared to HCC, FLC tumors were larger, requiring more frequently a major hepatectomy. In a Surveillance, Epidemiology, and End Results (SEER) database analysis, Eggert et al. compared 183 patients with FLC and 31,278 patients with conventional HCC.10 Most FLC patients were non-Hispanic white (60 %) and under 40 years of age (60 %), in contrast to HCC patients, who were 50 % non-Hispanic white and only 2 % under age 40. Surgical resection was performed more often in FLC patients (41 vs. 8 %, p < 0.0001).
Our data demonstrate that despite shorter recurrence-free survival after resection of FLC, overall survival rates are similar, with a 5-year overall survival of 58 % for patients with FLC and 67 % with non-cirrhotic HCC. In a systematic review and meta-analysis, Njei et al. demonstrated that for all patients, FLC was associated with improved overall survival compared to HCC.9 However, in subgroup analysis limited to non-cirrhotic patients, the 5-year overall survival was similar between FLC and HCC. The results of our study support aggressive surgical resection for recurrent FLC, which was associated with median overall survival of 122 months, compared to 37 months with non-surgical therapies for recurrence. Similarly, Maniaci et al. described aggressive multimodality therapy for recurrent FLC, including re-resection in 7 of 10 patients, resulting in median overall survival of 9.3 years.11 In the current series, among patients who did not undergo resection of recurrent disease, 39 % had widespread, unresectable disease and/or progression on systemic therapy. These results highlight the importance of tumor biology in determining resectability and patient survival.
In this study, prognostic factors for overall survival were the number of tumors and vascular invasion, which define AJCC stages I–III for conventional HCC. Size >5 cm, another key element in AJCC stage, was not a significant prognostic factor among patients with FLC, whose median tumor size was 10.5 cm. In our previous report of 94 patients with FLC, including 48 % who did not undergo surgical resection, the number of tumors, but not AJCC stage, was significantly associated with overall survival.12 In the current series, AJCC stage did not stratify recurrence-free survival for patients with FLC. Among the factors that define AJCC stage, vascular invasion was the sole factor associated with recurrence. FLC patients with vascular invasion had a 3-year recurrence-free survival of 9 %, compared to 35 % without vascular invasion (p = 0.034).
Among our patients with FLC, 46 % presented with stage IV disease, primarily due to lymph node metastases. For conventional HCC, lymph node metastases are considered a sign of systemic disease and associated with poor prognosis. However, in this study of patients undergoing resection of FLC, lymph node metastases did not significantly affect overall or recurrence-free survival. These results are in contrast to previous reports showing worse prognosis with nodal metastases. In a study of 41 FLC patients, including 13 unresectable patients, Stipa et al. observed median overall survival rates of 46 and 117 months, with and without lymph node metastases (p = 0.047).13 We found similarly a longer 5-year overall survival of 67 % without nodal metastases, compared to 42 % with nodal metastases, but this did not reach statistical significance (p = 0.15). Prolonged survival can be achieved after resection of nodal metastases. Our results support classifying lymph node metastases in FLC as regional disease, rather than systemic disease.
A limitation of this study is the small number of patients with FLC. Thus, the lack of difference in survival with and without lymph node metastases may be the result of a type II error. Another limitation is its retrospective nature and small number of patients with FLC. However, we present the largest single-institution series in the literature of patients with surgically resected FLC.
In conclusion, we demonstrate that among patients undergoing surgical resection, FLC is associated with higher recurrence rates but similar overall survival, compared to non-cirrhotic conventional HCC. Repeat surgical resection for recurrent FLC is associated with prolonged survival and should be performed, when feasible. Almost half of the FLC patients in this series presented with stage IV disease, primarily due to lymph node metastases, which did not significantly affect prognosis. AJCC stage was not a significant predictor of recurrence-free survival after resection of FLC. Together, these data suggest that the AJCC staging system for HCC can be modified to better stratify survival and recurrence for FLC patients.
References
El-Serag HB, Davila JA. Is fibrolamellar carcinoma different from hepatocellular carcinoma? A US population-based study. Hepatology. 2004;39(3):798–803.
Torbenson M. Review of the clinicopathologic features of fibrolamellar carcinoma. Adv Anat Pathol. 2007;14(3):217–23.
Simon EP, Freije CA, Farber BA, Lalazar G, Darcy DG, Honeyman JN, Chiaroni-Clarke R, Dill BD, Molina H, Bhanot UK, La Quaglia MP, Rosenberg BR, Simon SM. Transcriptomic characterization of fibrolamellar hepatocellular carcinoma. Proc Natl Acad Sci. 2015;112(44):E5916-25.
Chun YS, Zimmitti G. Fibrolamellar variant of hepatocellular carcinoma. Recent Results Cancer Research. 2013;190:101–10.
Honeyman JN, Simon EP, Robine N, Chiaroni-Clarke R, Darcy DG, Lim, II, Gleason CE, Murphy JM, Rosenberg BR, Teegan L, Takacs CN, Botero S, Belote R, Germer S, Emde AK, Vacic V, Bhanot U, LaQuaglia MP, Simon SM. Detection of a recurrent DNAJB1-PRKACA chimeric transcript in fibrolamellar hepatocellular carcinoma. Science. 2014;343(6174):1010–4.
Cornella H, Alsinet C, Sayols S, Zhang Z, Hao K, Cabellos L, Hoshida Y, Villanueva A, Thung S, Ward SC, Rodriguez-Carunchio L, Vila-Casadesus M, Imbeaud S, Lachenmayer A, Quaglia A, Nagorney DM, Minguez B, Carrilho F, Roberts LR, Waxman S, Mazzaferro V, Schwartz M, Esteller M, Heaton ND, Zucman-Rossi J, Llovet JM. Unique genomic profile of fibrolamellar hepatocellular carcinoma. Gastroenterology. 2015;148(4):806–18 e10.
Edge SB, American Joint Committee on Cancer. AJCC cancer staging manual. 7th ed. New York: Springer; 2010.
Ang CS, Kelley RK, Choti MA, Cosgrove DP, Chou JF, Klimstra D, Torbenson MS, Ferrell L, Pawlik TM, Fong Y, O’Reilly EM, Ma J, McGuire J, Vallarapu GP, Griffin A, Stipa F, Capanu M, Dematteo RP, Venook AP, Abou-Alfa GK. Clinicopathologic characteristics and survival outcomes of patients with fibrolamellar carcinoma: data from the fibrolamellar carcinoma consortium. Gastrointest Cancer Res. 2013;6(1):3–9.
Njei B, Konjeti VR, Ditah I. Prognosis of Patients With Fibrolamellar Hepatocellular Carcinoma Versus Conventional Hepatocellular Carcinoma: A Systematic Review and Meta-analysis. Gastrointest Cancer Res. 2014;7(2):49–54.
Eggert T, McGlynn KA, Duffy A, Manns MP, Greten TF, Altekruse SF. Fibrolamellar hepatocellular carcinoma in the USA, 2000–2010: A detailed report on frequency, treatment and outcome based on the Surveillance, Epidemiology, and End Results database. United European Gastroenterol J. 2013;1(5):351–7.
Maniaci V, Davidson BR, Rolles K, Dhillon AP, Hackshaw A, Begent RH, Meyer T. Fibrolamellar hepatocellular carcinoma: prolonged survival with multimodality therapy. Eur J Surg Oncol. 2009;35(6):617–21.
Kaseb AO, Shama M, Sahin IH, Nooka A, Hassabo HM, Vauthey JN, Aloia T, Abbruzzese JL, Subbiah IM, Janku F, Curley S, Hassan MM. Prognostic indicators and treatment outcome in 94 cases of fibrolamellar hepatocellular carcinoma. Oncology. 2013;85(4):197–203.
Stipa F, Yoon SS, Liau KH, Fong Y, Jarnagin WR, D’Angelica M, Abou-Alfa G, Blumgart LH, DeMatteo RP. Outcome of patients with fibrolamellar hepatocellular carcinoma. Cancer. 2006;106(6):1331–8.
Acknowledgments
This research was supported, in part, by the National Institutes of Health through MD Anderson Cancer Center’s Support Grant, CA016672. Drs. Yamashita, Vauthey, Kaseb, Aloia, Conrad, Hassan, Passot, Raghav, Shama, and Chun drafted the work, gave final approval of the manuscript, and agreed to be accountable for all aspects of the work. Drs. Yamashita, Vauthey, and Chun made substantial contributions to the conception and design of the work. Drs. Kaseb, Aloia, Conrad, Hassan, Passot, Raghav, and Shama made substantial contributions to the acquisition of data for the work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the Institutional Review Board.
Rights and permissions
About this article
Cite this article
Yamashita, S., Vauthey, JN., Kaseb, A.O. et al. Prognosis of Fibrolamellar Carcinoma Compared to Non-cirrhotic Conventional Hepatocellular Carcinoma. J Gastrointest Surg 20, 1725–1731 (2016). https://doi.org/10.1007/s11605-016-3216-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3216-x