Abstract
Background
Although proposed as a means for quality improvement, little is known regarding the economic consequences of volume-based referral. The objective of the current study was to investigate the relationship between inpatient costs and hospital volume.
Methods
Patients undergoing elective liver surgery were identified using the Nationwide Inpatient Sample from 2001 to 2012. Multivariable hierarchical regression analyses were performed to calculate and compare risk-adjusted costs and postoperative outcomes across hospital volume terciles.
Results
A total of 27,813 patients underwent surgery at 2207 hospitals. Although costs were comparable across the three volume groups (all p > 0.05), patients who developed a postoperative complication incurred a higher overall cost (complication vs. no complication; median costs $17,974 [IQR 13,865–25,623] vs. $41,731 [IQR 27,008–64,266], p < 0.001). In contrast, while the incidence of postoperative complications (low vs. intermediate vs. high; 22.0 vs. 19.2 vs. 13.0 %, p < 0.001) and subsequent failure-to-rescue (low vs. intermediate vs. high; 16.6 vs. 24.7 vs. 15.1 %, p < 0.001) was lower at high-volume hospitals, costs associated with “rescue” were substantially higher at high-volume hospitals (low vs. intermediate vs. high; $39,289 vs. $36,157 vs. $48,559, both p < 0.001).
Conclusions
Compared with lower volume hospitals, improved outcomes among patients who developed a complication at high-volume hospitals were associated with an increased cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Healthcare costs currently account for 18 % of the US gross domestic product.1 However, the quality of care in the US ranks lows.2 A potential strategy to address this mismatch in value of care is to appropriately match patients to hospitals that have the expertise, resources, and systems to effectively manage their respective conditions.3 , 4 As such, the selective referral of patients to high-volume centers has been proposed for high-risk elective procedures.5 – 10 Although these efforts may serve to reduce operative mortality, little is known regarding the potential economic implications of these volume-based referral strategies. For example, reports suggest that higher volume hospitals may achieve lower costs for care via improved efficiency, economies of scale or via the prevention of costly postoperative complications.11 , 12 In contrast, other studies have raised concerns that high-volume hospitals may achieve improved postoperative outcomes as a result of increased resource utilization, thereby serving to increase healthcare costs.13
Liver resection represents an ideal procedure for targeted efforts to improve the value for care. While the number of liver resections performed annually has steadily increased over the past two decades, morbidity following liver surgery still remains high.14 , 15 Specifically, up to 40 % of patients experience postoperative complications with postoperative complications and subsequent failure-to-rescue (FTR) following liver surgery noted to vary by hospital volume.14 Additionally, as liver resections are performed at hospitals of varying size and complexity, this heterogeneity represents an opportunity to determine whether different subsets of patients can safely and efficiently be treated at hospitals with varying levels of resources, size, and expertise.14 Although essential to understanding the financial consequences of volume-based referral, data comparing hospital costs at high- versus low-volume hospitals performing liver surgery are lacking. Therefore, using a large nationally representative dataset, the current study sought to evaluate the relationship between inpatient surgical costs and hospital volume among patients undergoing elective liver surgery.
Methods
Data Source and Patient Population
This cross-sectional study was performed using patient and hospital discharge data from the Healthcare Cost and Utilization Project (HCUP)-Nationwide Inpatient Sample (NIS) from January 1, 2001, through to December 31, 2012. Maintained by the Agency for Healthcare Research and Quality (AHRQ), the NIS represents the largest in-patient, all-payer database in the USA, including information from over eight million in-patient admissions annually, collected from more than 1000 hospitals in 46 states. Using a stratified sampling methodology based on hospital-level characteristics (geographic region, teaching status, hospital size, and urban vs. rural location), the NIS is a 20 % representative sample of all in-patient hospital visits in the USA.
International Classification of Disease, Ninth Revision, Clinical Manifestation (ICD-9-CM) procedure codes “50.22” and “50.3” were used to identify patients older than 18 years undergoing a liver resection. To ensure the homogeneity of the patient population, patients undergoing any concomitant surgery, or surgery performed on an emergent basis were excluded from the study population. Patient comorbidity was classified according to the Charlson comorbidity index (CCI), and patients were categorized into five groups (CCI; 0, 1, 2, 3, ≥4).16 Using unique hospital identifiers, individual hospitals were identified. An annual surgical volume was calculated for each hospital for each active year, categorizing hospitals into volume terciles representing an equal number of hospitals. Specifically, hospitals performing 1–4 liver resections per year were categorized as low-volume hospitals, 5–14 liver resections per year as intermediate-volume hospitals and hospitals performing ≥15 liver resections per year as high-volume hospitals.
Postoperative complications were described using previously validated ICD-9-CM diagnosis codes.10 Specifically, postoperative complications included respiratory failure, pneumonia, acute myocardial infarction, cardiac arrest, acute renal failure, sepsis, stroke, venous thromboembolism, gastrointestinal hemorrhage, and surgical site infections.10 FTR was defined as in-hospital mortality following the development of a postoperative complication.10 , 14
Statistical Analysis
Continuous variables were described as medians with interquartile range (IQR) and compared using the nonparametric Kruskal-Wallis test. Categorical variables were expressed as whole numbers and proportions and compared using the Pearson’s chi-squared test.
Total hospital charges were inflation adjusted and reported as 2012 US dollars using the consumer price index maintained by the US Department of Labor.17 As hospital charges may be confounded by payer policies, total hospital costs were calculated using hospital-specific cost-to-charge ratios developed by the Agency for Healthcare Research and Quality (AHRQ). Multivariable, hierarchical linear regression analyses were performed to calculate risk-adjusted in-patient costs accounting for patient case mix and hospital characteristics. Following the hierarchical structure where patients are clustered within hospitals each with their own respective characteristics and policies, a random effect intercept was specified at the hospital level. As positively skewed, total hospital costs were log-transformed and treated as the dependent variable within the model. The natural log of costs was subsequently used to calculate risk-adjusted costs. Secondary binary outcomes such as the development of postoperative complications, in-hospital mortality, and FTR were risk-adjusted using a hierarchical multivariable logistic regression adjusting for patient- and hospital-level characteristics while also accounting for the clustering of patients to hospitals. Similarly, a risk-adjusted length of stay (LOS) was calculated using a hierarchical multivariable Poisson regression adjusting for patient and hospital characteristics. Model discrimination was assessed using area under the receiver operating characteristic curve. Statistical significance for all tests was defined as p < 0.05. All analyses were performed using STATA, version 14.0, for Windows (StataCorp, College Station, TX).
Results
Patient Characteristics
A total of 27,813 patients underwent a liver resection at 2207 hospitals and met inclusion criteria. The median age of the entire cohort was 60 years (IQR, 47–69) with a majority of patients being male (n = 14,934, 53.7 %, Table 1). Preoperative comorbidity was commonly noted among all patients with more than 58 % of patients presenting with a CCI score ≥4 (n = 16,146, 58.1 %). More than 70 % of patients were Caucasian (n = 16,979, 73.1 %), while 12.7 % (n = 2,958) of patients were black and 5.6 % (n = 1,294) Hispanic. Overall, Medicare was the most common payor (n = 13,250, 47.7 %) followed by private payors (n = 10,501, 37.8 %) and Medicaid (n = 2,676, 9.6 %). A partial hepatectomy was performed in two thirds of patients (n = 18,748, 67.4 %) with the remaining one third of patients undergoing a hepatic lobectomy (n = 9063, 32.6 %). Minimally invasive surgery was performed in 6.4 % of patients (n = 1789).
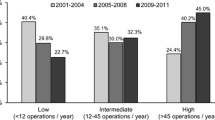
Among the 2207 hospitals identified in the study cohort, 55.6 % (n = 1,223) were large hospitals with a hospital bed size of 100 beds or more. While 85.4 % (n = 1338) of hospitals were located in an urban location, only 39.9 % (n = 625) of hospitals were affiliated with a teaching facility (Table 2). Annual hospital volume for each hospital ranged from 1 to 364 elective liver resections performed per year. A total of 952 hospitals (43.1 %) were categorized as low-volume hospitals while 590 hospitals (26.7 %) were categorized as intermediate-volume hospitals and 665 (30.1 %) as high-volume hospitals (Fig. 1). High-volume hospitals were proportionally more likely to be larger hospitals (low vs. intermediate vs. high; 45.0 vs. 57.9 vs. 68.8 %, p < 0.001), located in an urban setting (low vs. intermediate vs. high; 74.1 vs. 89.9 vs. 98.1 %, p < 0.001), and affiliated with a teaching hospital (low vs. intermediate vs. high; 17.5 vs. 37.2 vs. 75.3 %, p < 0.001).
Among all patients undergoing a liver surgery, 87.1 % (n = 24,309) were treated at high-volume hospitals while 7.5 % (n = 2030) were treated at intermediate-volume hospitals and 5.4 % (n = 1474) treated at low-volume hospitals (Fig. 1). Patients treated at high-volume hospitals were younger (low vs. intermediate vs. high; median age 63 years [IQR 51–74] vs. 63 years [51–73] vs. 60 years [47–69], p < 0.001), and more likely to be male (low vs. intermediate vs. high; 45.0 vs. 41.0 vs. 55.3 %, p < 0.001) compared with patients at low- and intermediate-volume hospitals. Interestingly, while comorbidity was commonly noted among all patients, patients presenting to low-volume hospitals were more likely to present with preexisting comorbidity (low vs. intermediate vs. high; CCI ≥ 4; 62.0 vs. 55.4 vs. 58.0 %, p < 0.001). Of note, patients presenting to high-volume hospital were also more likely to present with underlying cirrhosis (low vs. intermediate vs. high; 7.5 vs. 8.1 vs. 9.2 %, p = 0.006). Patients presenting to high-volume hospitals were proportionally more likely to be insured by private insurers (low vs. intermediate vs. high; 35.5 vs. 36.6 vs. 38.0 %, p < 0.001) and were more likely to be categorized in the highest income quartile (low vs. intermediate vs. high; 47.8 vs. 45.0 vs. 52.7 %, p < 0.001). High-volume hospitals also treated the greatest proportion of patients in the lowest income quartile (low vs. intermediate vs. high; 2.5 vs. 5.5 vs. 9.3 %, p < 0.001). Patients presenting to high-volume centers were more likely to undergo a hepatic lobectomy compared with low and intermediate hospitals (low vs. intermediate vs. high; 15.1 vs. 23.7 vs. 34.4 %, p < 0.001), as well as have surgery using a minimally invasive approach (low vs. intermediate vs. high; 4.3 vs. 2.6 vs. 6.9 %, p < 0.001),
Postoperative Outcomes by Volume
Among all patients who underwent surgery, postoperative complications were observed in 19.8 % (n = 5498) of patients. Patients treated at high-volume hospitals were less likely to develop a postoperative complication with the risk-adjusted incidence of postoperative complications noted to be 20.5 % at high-volume hospitals versus 25.0 and 26.0 % at low- and intermediate-volume hospitals, respectively (both p < 0.001, Fig. 2). Of note, volume-based differences in the incidence of postoperative complications remained on sensitivity analysis when excluding patients with a diagnosis of cirrhosis (Supplemental Material, Table 1). While the LOS was comparable among patients treated at all three volume strata (all p > 0.05), patients who developed a postoperative complication had a longer risk-adjusted LOS compared with patients who did not. This trend was noted across all three volume groups (all p < 0.05).
The overall risk-adjusted in-hospital mortality was noted to be 2.3 % among all patients and decreased across the volume terciles (low vs. intermediate vs. high; 9.0 vs. 7.6 vs. 1.3 %, all p < 0.05). Further, FTR (calculated as the proportion of the patients who died among patients who developed a postoperative complication) also varied by hospital volume. Specifically, the rate of FTR was 15.1 % at high-volume hospitals, 24.7 % at intermediate-volume hospitals, and 16.6 % at low-volume hospitals (both p < 0.01).
Inpatient Costs
The median costs for liver surgery among all patients was $20,097 (IQR 14,023–32,912). Risk-adjusted costs for surgery were comparable across the volume groups (low vs. intermediate vs. high; $17,050 vs. $21,473 vs. $18,342, all p > 0.05, Fig. 2). Of note, the proportion of procedures performed with a cost greater than 75 % of the cohort was higher at high-volume centers versus low-volume centers (low vs. intermediate vs. high; 27.1 vs. 29.9 vs. 32.1 %, p < 0.001).
To further explore the relationship between hospital volume and costs, inpatient costs were compared among patients who developed a postoperative complication versus patients who did not. Overall, the cost of liver surgery was over twofold higher among patients who developed a postoperative complication versus patients who had an uncomplicated postoperative course (complication vs. no complication; median costs $17,974 [IQR 13,865–25,623] vs. $41,731 [IQR 27,008–64,266], p < 0.001). This pattern of higher costs among patients with postoperative complications was noted across all three volume terciles (Fig. 3). Among patients who developed a postoperative complication, risk-adjusted in-patient costs were higher at high-volume hospitals compared with low- and intermediate-volume hospitals (low vs. intermediate vs. high; $48,868 vs. $37,756 vs. $56,356, both p < 0.001). Of note, among patients discharged alive following a postoperative complication, risk-adjusted costs were higher at high-volume centers versus low- and intermediate-volume hospitals (low vs. intermediate vs. high; $39,289 vs. $36,157 vs. $48,559, both p < 0.001, Table 3), while the risk-adjusted LOS was noted to be shorter at high-volume hospitals (low vs. intermediate vs. high; 11.6 vs. 9.9 vs. 7.7 days, both p < 0.001). In contrast among patients who died following a postoperative complication (FTR), risk-adjusted time to death was over twofold shorter at high-volume hospitals compared with low- and intermediate-volume hospitals (low vs. intermediate vs. high; 15.1 vs. 13.7 vs. 4.9, both p < 0.001). When adjusted for LOS, risk-adjusted costs for patients experiencing an in-hospital mortality following a postoperative complication (FTR) was lower at high-volume hospitals compared with patients treated at low- and intermediate-volume hospitals (low vs. intermediate vs. high; $109,118 vs. $95,803 vs. $84,589, both p < 0.001, Table 4). Among patients who did not develop a postoperative complication, differences in costs were less pronounces across volume strata.
Discussion
In an era of cost-containment, efforts are increasingly focused on improving the value of surgical care by enhancing quality while containing rising healthcare costs. One possible approach to achieving this elusive goal is the selective referral of patients undergoing high-risk procedures to high-volume centers.5 – 7 , 13 While the effect of procedural volume on outcomes such as morbidity and mortality have been well described, little is known regarding the potential economic consequences of these volume-based referral strategies.5 , 7 , 10 , 12 , 18 – 20 The current study is important because it utilized a nationally representative cohort of 27,813 patients undergoing elective liver surgery to evaluate the relationship between hospital volume and total inpatient costs. The current study demonstrated that patients treated at high-volume hospitals had improved postoperative outcomes in the form of a lower incidence of postoperative complications, lower FTR rates, and a lower postoperative mortality. Perhaps more importantly, the data demonstrated that, while postoperative outcomes were better at higher volume hospitals, the proportion of patients incurring the highest overall inpatient costs was also higher at high-volume hospitals versus low- and intermediate-volume hospitals. The higher costs seen at high-volume centers were largely attributable to the increased costs among patients who experienced a complication. In turn, we noted that patients with complications had an increased likelihood of being “rescued” and discharged home earlier at high-volume hospitals compared with patients who experienced a complication at an intermediate- or low-volume hospital. Collectively, data from the current study suggest that while global costs for liver surgery were higher at high-volume centers, the increased cost was largely attributable to the subset of patients who had a complication. In turn, the higher costs among patients who had a complication at a high-volume hospital translated into better outcomes including a lower FTR rate compared with low-volume centers.
Data from the current study contributes significantly to the limited body of research examining the potential economic impact of volume-based referral among patients undergoing complex elective surgery. In contrast to previous work that demonstrated similar costs across hospital volume strata, the current study noted that, among a subset of patients, risk-adjusted costs were higher among patients undergoing surgery at high-volume centers. In their report on patients undergoing complex, elective cardiac and vascular surgery, Birkmeyer et al. reported no differences in inpatient costs between high- and low-volume hospitals.19 The authors did note, however, that—rather than hospital volume—the development of postoperative complications was more predictive of higher inpatient costs and therefore accounted for the observed variations in costs.19 Similarly, while Nathan and colleagues reported no differences in payments among Medicare enrollees undergoing complex cancer surgery at high- and low-volume hospitals, there were significant differences in payments among patients who developed a postoperative complication versus those patients who did not.13 Paradoxically, in the current study, we noted that despite a lower incidence of postoperative complications at high-volume centers, inpatient costs were higher at high-volume hospitals. To explore and account for this relationship, we performed a stratified sensitivity analysis comparing costs among patients who developed a postoperative complication versus patients who did not. In addition, we further compared the costs of patients “rescued” from a postoperative complication with the cost of patients who died after a complication (FTR). We found that, while the cost of care at high-volume hospitals was comparable to that at low-volume hospitals among patients who did not develop a postoperative complication, costs were substantially higher among patients who did develop a postoperative complication. Specifically, when compared with low- and intermediate-volume hospitals, risk-adjusted costs were on average over $8000 higher at high-volume hospitals among patients discharged alive following a postoperative complication. The higher costs of “rescue” at these hospitals reaffirms that the higher quality of care at high-volume hospitals may be due in part to greater resource utilization and therefore may serve to increase the overall costs of care.3 , 12 , 13 , 19 Data from the current study suggest that while improved outcomes were achieved at higher volume hospitals, these superior results came at a substantially increased cost. As such, policy makers and physicians must ensure the appropriate matching of patients and hospitals while also promoting policies that target low-quality care and not just higher spending.
The ACA of 2012 aims to penalize hospitals providing a low-quality of care via financial penalties for the development of preventable postoperative complications while also curtailing spending via the introduction of a bundled payment system.20 Our data echo growing concerns that under such paradigms, high-volume hospitals may be disproportionately penalized for providing a higher level of care.21 , 22 For example, in the current study, we noted that while overall morbidity was lower at high-volume centers, the higher rates of rescue observed at higher volume centers was associated with an increased overall cost. It is therefore possible that new payment paradigms may actually serve to disincentivize the higher level of care provided at these hospitals. To this point, Rajaram et al. in their report demonstrated that under current policies, large, teaching hospitals are up to 2.5 times more likely to incur financial penalties compared with lower volume, nonteaching hospitals.23 Further, if payers reduce payments to hospitals for costs related to surgical complications and subsequent rescue, hospitals will be forced to examine how the increase resource utilization associated with surgical complications affects their profits and margins. Hospital and policymakers will have to consider if these “bundled” payments are appropriately matched to average patient episode costs when there are no complications, or in instances with the incremental costs associated with rescue.21 , 22 Therefore, to prevent potentially risk-averse behavior and selection of patients least predisposed to surgical complications, it is in the best economic interest for health care systems to develop adequately risk-adjusted payment paradigms that focus not only reduction of surgical complications, but also appropriate financial remuneration for the complex management necessary to avoid FTR.
The current study has several limitations. First, the analyses utilized administrative data that may have limited our ability to perform adequate risk adjustment.21 Specifically, while the use of NIS allowed for nationally representative results, the analysis was limited by the finite number of clinical variables present as well as the omission of important liver-specific variables from the dataset. For example, data pertaining to disease severity (e.g., tumor grade), extent of liver resection or the development of liver specific complications are not captured within the NIS and therefore may have resulted in some potential confounding. However, all multivariable models demonstrated appropriate discrimination when assessed using AUC. Further, the dataset lacked data assessing post-discharge costs, which may have contributed to greater differences in costs between hospital volume strata.22 Lastly, provider level differences, which have shown to effect overall variations in outcomes, could not be accounted for.23
In conclusion, current fee-for-service paradigms may misalign financial incentives and quality improvement efforts. As we shift to a value-driven method of reimbursement through accountable care organizations and bundled payments, administrators, healthcare providers, and policymakers should focus on improving the quality of patient care via targeting potentially avoidable postoperative complications, while promoting financial incentives to reduce surgical error and lowering costs.
References
Health expenditure, total (% of GDP) | Data | Table. http://data.worldbank.org/indicator/sh.xpd.totl.zs. Accessed August 8, 2015.
Explaining High Health Care Spending in the United States: An International Comparison of Supply, Utilization, Prices, and Quality - The Commonwealth Fund. http://www.commonwealthfund.org/publications/issue-briefs/2012/may/high-health-care-spending.aspx. Accessed August 8, 2015.
Miller DC, Ye Z, Gust C, et al. Anticipating the Effects of Accountable Care Organizations for Inpatient Surgery. JAMA Surg. 2013;148(6):549.
Wakeam E, Hyder JA, Lipsitz SR, et al. Outcomes and Costs for Major Lung Resection in the United States: Which Patients Benefit Most From High-Volume Referral? Ann Thorac Surg. June 2015.
Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128–1137.
Birkmeyer JD, Stukel TA, Siewers AE, et al. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349(22):2117–2127.
Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361(14):1368–1375.
Schrag D, Cramer LD, Bach PB, et al. Influence of hospital procedure volume on outcomes following surgery for colon cancer. JAMA. 2000;284(23):3028–3035. http://www.ncbi.nlm.nih.gov/pubmed/11122590. Accessed May 1, 2015.
Schrag D, Panageas KS, Riedel E, et al. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann Surg. 2002;236(5):583–592.
Ghaferi AA, Birkmeyer JD, Dimick JB. Complications, failure to rescue, and mortality with major inpatient surgery in medicare patients. Ann Surg. 2009;250(6):1029–1034. http://www.ncbi.nlm.nih.gov/pubmed/19953723. Accessed April 26, 2015.
Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. Cochrane database Syst Rev. 2006;(1):CD005033.
Birkmeyer JD, Skinner JS, Wennberg DE. Will volume-based referral strategies reduce costs or just save lives? Health Aff (Millwood). 21(5):234–241. http://www.ncbi.nlm.nih.gov/pubmed/12224888. Accessed August 8, 2015.
Nathan H, Atoria CL, Bach PB, et al. Hospital volume, complications, and cost of cancer surgery in the elderly. J Clin Oncol. 2015;33(1):107–114.
Spolverato G, Ejaz A, Hyder O, et al. Failure to rescue as a source of variation in hospital mortality after hepatic surgery. Br J Surg. 2014;101(7):836–846.
Mayo SC, Pulitano C, Marques H, et al. Surgical management of patients with synchronous colorectal liver metastasis: a multicenter international analysis. J Am Coll Surg. 2013;216(4):707–716; discussion 716–718.
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. http://www.ncbi.nlm.nih.gov/pubmed/3558716. Accessed July 10, 2014.
Bureau of Labor Statistics USD of L. CPI Inflation Calculator. http://www.bls.gov/data/inflation_calculator.htm.
Birkmeyer JD, Gust C, Dimick JB, et al. Hospital Quality and the Cost of Inpatient Surgery in the United States. Ann Surg. 2012;255(1):1–5.
Regenbogen SE, Gust C, Birkmeyer JD. Hospital Surgical Volume and Cost of Inpatient Surgery in the Elderly. J Am Coll Surg. 2012;215(6):758–765.
Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364(22):2128–2137.
Haut ER, Pronovost PJ, Schneider EB. Limitations of administrative databases. JAMA. 2012;307(24):2589; author reply 2589–2590.
Arbaje AI, Wolff JL, Yu Q, et al. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist. 2008;48(4):495–504. http://www.ncbi.nlm.nih.gov/pubmed/18728299. Accessed February 16, 2015.
Gani F, Lucas DJ, Kim Y, et al. Understanding Variation in 30-Day Surgical Readmission in the Era of Accountable Care: Effect of the Patient, Surgeon, and Surgical Subspecialties. JAMA Surg. August 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None
Author Contributions
Study concept and design—–Gani, Pawlik; acquisition of data—Gani, Pawlik; analysis and interpretation—Gani, Pawlik; drafting of manuscript—Gani, Pawlik; critical revision—Gani, Pawlik.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Gani, F., Pawlik, T.M. Assessing the Costs Associated with Volume-Based Referral for Hepatic Surgery. J Gastrointest Surg 20, 945–952 (2016). https://doi.org/10.1007/s11605-015-3071-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-3071-1