Abstract
There are limited data regarding predictive factors of postoperative venous thromboembolism (VTE) in patients undergoing colorectal resection. We sought to identify associations between patient comorbidities and postoperative VTE in colorectal resection. The National Surgical Quality Improvement Program (NSQIP) database was used to examine clinical data of patients experiencing postoperative VTE after colorectal resection from 2005 to 2011. Multivariate analysis using logistic regression was performed to quantify risk factors of VTE. We sampled 116,029 patients undergoing colorectal resection. The rate of VTE was 2 % (2,278) with 0.2 % (182) having deep vein thrombosis (DVT) and pulmonary embolism (PE). The first week after operation was the most common time for postoperative VTE. A significant number of patients suffering DVT and PE were diagnosed after index hospital discharge (PE 34.6 %, DVT 29.3 %). The most important risk factors identified for DVT include (P < 0.05) ASA score >2 (adjusted odds ratio (AOR) 1.77) and hypoalbuminemia (serum albumin level <3.5 mg/dl) (AOR 1.69). The most important factors had associations with PE include (P < 0.05) DVT (AOR 14.60) and disseminated cancer (AOR 1.70). Ulcerative colitis (AOR 1.48, P = 0.01) and stage 4 cancer (AOR 1.29, P = 0.02) have associations with DVT. Open colorectal procedures have higher risk of DVT compared to laparoscopic procedures (AOR 1.33, P < 0.01). Postoperative VTE occurs in 2 % of colorectal resections. Thirty percent of VTE events were diagnosed after discharge. Prophylactic treatment of VTE after discharge may have benefits in high-risk patients. Thirteen and eleven perioperative risk factors have associations with DVT and PE, respectively. Emergent admission, open procedures, ulcerative colitis, and stage 4 cancer patients have increased risk of DVT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Postoperative venous thromboembolism, with a current prevalence of 1.4–2.4 % in colorectal surgery patients, is one of the most important potentially preventable conditions which increases morbidity, mortality, hospitalization length, and hospital charges for patients.1–4 VTE has been reported on more than 572,000 death certificates annually in the USA, and pulmonary embolism (PE) has been described as one of the most preventable causes of mortality.5 It is important to recognize the risk factors for development of VTE in order to decrease the morbidity and mortality.
A number of previous studies have identified risk factors influencing postoperative VTE rates with the goal of decreasing postoperative venous thromboembolic events, primarily via prophylaxis. Some of the VTE predictors include age >50 years, pregnancy, malignancy, history of myocardial infarction (MI), diabetes, and obesity.6 Using previously identified risk factors, the American Society of Clinical Oncology introduced a guideline for assessing and managing the VTE risks in hospitalized cancer patients in 2007.7 This guideline was updated in 2013.8
The increased incidence rate of VTE events after operation has been previously identified.6 High rate of VTE following colorectal surgery due to the higher frequency of risk factors has been reported by some studies.6 Also, the rate of PE following colorectal operations has been estimated to be as much as four times higher than other surgical patients.9 However, a large nationwide study analyzing the rate of VTE in colorectal surgery is lacking.
There is also current controversy regarding the appropriate prophylactic prevention in colorectal patients, particularly the utilization of VTE prophylaxis following patient discharge. Although some studies reported a high rate of VTE after discharge of patients, prolonged prophylactic treatment of VTE is still contraversial.9 Furthermore, a large nationwide study analyzing the rate of VTE in colorectal surgery after discharge is lacking. Therefore, we aim to report the incidence, risk factors, and 30-day outcomes of VTE in patients undergoing colorectal procedures.
Materials and Methods
This study was performed utilizing the American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database10 from January 1, 2005, to December 31, 2011. ACS NSQIP is a nationally validated, risk-adjusted, outcome-based program to measure and improve the quality of surgical care in the USA.10 ACS NSQIP provides preoperative to 30-day postoperative surgical outcomes based on clinical data. We looked at patients who had undergone colorectal resections for the diagnosis of benign or malignant colorectal tumor, diverticular diseases, Crohn’s disease, and ulcerative colitis using the appropriate procedural and diagnosis codes as specified by the International Classification of Diseases, 9th revision, clinical modifications (ICD-9-CM). Patients who had colorectal procedures were defined based on the following Current Procedural Terminology (CPT) codes: 44140–44156, 44204–44212, 45110, 45126, and 45395. Patients who underwent surgery without colon or rectal resection and patients younger than 18 years were excluded from this study. Patients’ diagnosis was defined based on the following ICD-9 codes: malignant neoplasm of the colon (153.0–153.4, 153.6, 153.7, and 230.3), malignant neoplasm of the rectum (154.0, 154.1, and 230.4), benign neoplasm of the colon and rectum (211.3, 211.4), diverticulosis or diverticulitis (562.10–562.13), Crohn’s disease (555.0, 555.1, 555.2, and 555.9), and ulcerative colitis (556.0–556.9).
Preoperative factors that were analyzed include patient characteristics (age, sex, and race) and 13 comorbidity conditions including steroid use for chronic condition, history of severe chronic obstructive pulmonary disease (COPD), ascites, alcohol abuse more than two drinks per day in 2 weeks before admission, hypertension requiring medication, American Society of Anesthesiologists (ASA) score more than two, serum albumin level <3.5 mg/dl (hypoalbuminemia), body mass index (BMI) >30, disseminated cancer, cerebrovascular accident (CVA) or stroke with or without neurologic deficit, congestive heart failure (CHF), and history of myocardial infarction (MI). Other factors analyzed include chemotherapy for malignancy in the last 30 days before operation, radiotherapy for malignancy in the last 90 days before operation, anesthesia length, hospitalization length, admission type, postsurgical complications (superficial surgical site infection (SSI), deep incisional SSI, organ space SSI, wound disruption, pneumonia, unplanned intubation, ventilator dependency more than 48 h, urinary tract infection, cardiac arrest requiring cardiopulmonary resuscitation (CPR), myocardial infarction, acute renal failure, and hospitalization more than 30 days), pathologic conditions (colon cancer, rectal cancer, diverticulosis or diverticulitis, Crohn’s disease, ulcerative colitis, and benign colorectal tumor), type of surgical resection (total colectomy, partial colectomy, abdominoperineal resection (APR), and pelvic exenteration), and surgical techniques (laparoscopic vs. open). The overall rate of postoperative VTE by procedure type and diagnosis were examined. Risk-adjusted analysis was performed to identify preoperative comorbidities and postoperative complications which have independent associations with VTE following colorectal surgery. Male gender and age <70 years were used as reference data points for comparison in line with the literature.1,11
Statistical Analysis
Statistical analysis was performed with SPSS® software, version 22 (SPSS Inc., Chicago, IL). Logistic regression was used to describe the weights assigned to preoperative variables that best discriminate patients with VTE from those without. P values less than 0.05 were considered statistically significant. For each association, the adjusted odds ratio (AOR) with a 95 % confidence interval was calculated and reported to estimate the relative risk associated with VTE. Adjustments were made for age, sex, race, steroid use, COPD, ascites, chemotherapy, radiotherapy, alcohol abuse, hypertension, ASA score more than 2, hypoalbuminemia, body mass index >30, disseminated cancer, CVA or stroke with or without neurologic deficit, CHF, history of MI, surgical technique, hospitalization length, anesthesia length, type of the procedure, and pathology conditions. Logistic regression analysis was also used to estimate the association between VTE and other postoperative complications.
Results
We sampled 116,029 patients who underwent colorectal resection from 2005 to 2011. The mean age of patients was 62 ± 15 years old (Table 1); the majority of the patients were Caucasian (78 %) and female (51.6 %). Most common comorbidities included hypertension (50.6 %) and obesity with body mass index (BMI) more than 30 (31.6 %). Demographic data of patients are reported in Table 1.
2,278 (2 %) patients experienced postoperative VTE, with 1.2 % (1,338) having isolated deep vein thrombosis (DVT), 0.7 % (758) having isolated PE, and 0.2 % (182) having diagnosis of DVT and PE. 19.8 % of patients with PE had a diagnosis of DVT at least 1 day before the diagnosis of PE.
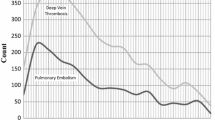
The first week after the operation was the most common time for postoperative VTE (Fig. 1). Of the patients who had DVT or PE, 36.5 and 43.8 %, respectively, were diagnosed in the first week postoperatively.
Notably, 34.6 % of patients with PE and 29.3 % of patients with DVT were diagnosed after discharge. The rates of in-hospital VTE in open and laparoscopic surgery were 1.8 and 0.6 % respectively. However, the rates of posthospital discharge VTE in open and laparoscopic surgery were 0.7 and 0.5 % respectively.
For patients with VTE, the median length of stay in the hospital was 17 days, while for patients without VTE was 6 days. The adjusted mean difference in hospitalization was 1 week longer (confidence interval (CI) 6.67–8.02, P < 0.01).
For patients with VTE, the mean anesthesia time was 248 min with a standard deviation of 125, while for patients without it was 233 min with a standard deviation of 105 min. The adjusted mean difference in anesthesia time was statistically significant (mean difference = 10 min, CI 4.32–15.40, P < 0.01).
The unadjusted mortality rate in patients with or without PE was 8.3 and 4.1 %, respectively, while the adjusted risk of mortality in patients with PE was greater than for those without PE (AOR 1.60, CI 1.21–2.12, P < 0.01). The unadjusted mortality rate in patients with or without DVT was 9.2 and 4.1 %, respectively, while the adjusted risk of mortality in patients with DVT was not statistically greater than patients without (AOR 1.09, CI 0.87–1.36, P = 0.42).
The risk-adjusted analysis for factors associated with DVT is reported in Table 2. Age more than 70 was a predictor of DVT (AOR 1.33, P < 0.05). Also, black or African-American race had higher rate of postoperative DVT. Among comorbid conditions, ASA score >2 (AOR 1.77, P < 0.05), hypoalbuminemia (AOR 1.69, P < 0.05), disseminated cancer (AOR 1.29, P = 0.02), steroid use (AOR 1.23, P = 0.03), and obesity (AOR 1.15, P = 0.03) have association with postoperative DVT. Open colorectal procedures had higher risk of postoperative DVT compared to laparoscopic procedures (AOR 1.33, P < 0.01). Emergently admitted patients had higher risk of postoperative DVT compared to nonemergently admitted patients (AOR 1.55, P < 0.01). Among pathologic conditions, ulcerative colitis has associations with postoperative DVT (AOR 1.48, P = 0.01), but malignancy only in the presence of metastasis (disseminated cancer) had association with postoperative DVT (Table 2). Types of the colorectal procedures did not have significant associations with postoperative DVT. However, anesthesia length more than 150 min had associations with postoperative DVT.
The risk-adjusted analysis for factors associated with PE is reported in Table 3. The strongest risk factor of PE was DVT (AOR 14.60, P < 0.01). Also, seven factors including disseminated cancer (AOR 1.70, P < 0.05), age more than 70 (AOR 1.32, P < 0.01), emergency admission (AOR 1.24, P = 0.02), open surgery (AOR 1.73, P < 0.01), hypoalbuminemia (AOR 1.21, P = 0.02), steroid use (AOR 1.48, P < 0.01), and obesity (AOR 1.34, P < 0.01) had association with postoperative PE.
The risk-adjusted analysis for postoperative complications associated with DVT and PE is reported in Tables 4 and 5. Complications showing the strongest associations with DVT included hospitalization more than 30 days (AOR 3.37, P < 0.05) and unplanned intubation (AOR 2.30, P < 0.05). Also, complications showing the strongest associations with PE included cardiac arrest (AOR 3.93, P < 0.05) and unplanned intubation (AOR 3.43, P < 0.05).
Discussion
Postoperative VTE following colorectal resection is associated with a poor prognosis and significant increased morbidity and hospitalization length. Although postoperative DVT does not independently affect mortality rate, the mortality rate of patients who suffer from PE is significantly increased. In line with the literature, VTE was also found to be significantly associated with increased mean hospitalization period of the affected patients (mean difference = 7 days, CI 6.67–8.02).
Prophylactic treatment of VTE is recommended for high-risk patients after hospital discharge. We found that 34.6 % of patients with PE and 29.3 % of patients with DVT are diagnosed after discharge. We believe our data may support prophylactic treatment of VTE for high-risk patients after hospital discharge in colorectal surgery.8 Even though most VTE events occur during the first week after surgery, the rate of VTE events is still significant during the subsequent weeks following hospital discharge (Fig. 1). However, the high rate of posthospital discharge VTE can be related to the fact that the actual time of occurrence of the DVT and PE may be earlier than the reported day because of delay in diagnosis. Further studies should be planned to see if the high rate of posthospital discharge VTE is related to the late development of DVT and PE complications or a late diagnosis of a previous complication.
The rate of VTE is high in the first 2 weeks of surgery. Our results show most VTE events occur during the first 2 weeks after surgery (Fig. 1). Considering that a large number of patients in colorectal surgery are discharged from the hospital during the first week of surgery, such patients may have an increased risk of postdischarge VTE. Further studies should be planned to evaluate the benefit of prophylactic treatment of VTE on patients discharged from hospital during the first week of surgery.
Evaluating the efficiency of the anticoagulation treatment for DVT in patients who have DVT and at least two other risk factors of PE is suggested. 19.8 % of patients with PE had a diagnosis of DVT at least 1 day before report of PE. It appears that the routine treatment of DVT was not enough to prevent the incidence of PE in such patients. Our results show 97.8 % of such patients had at least two risk factors of PE other than DVT including age >70, emergency admission, open surgery, hypoalbuminemia, disseminated cancer, steroid use, and obesity. Patients who already have DVT and have at least two other risk factors of PE may benefit from closer monitoring for PE.
Our data, which represents one of the largest series to date on this topic, identifies significant risk factors for DVT following colorectal operation. Our study identified 12 predictors associated with DVT. In terms of patient demographic factors, age >70 and black or African-American race have associations with postoperative DVT. Older age has been reported as a risk factor of DVT by the literature.1,6 Among comorbid conditions, seven factors have associations with DVT including ASA >2, hypoalbuminemia, disseminated cancer, obesity, and steroid use. Obesity and malignancy have been introduced as a predictor of DVT by literature previously.1,6 However, in terms of malignancy, our results show that only the presence of distant metastasis (disseminated cancer) has an association with DVT. Among pathologic conditions, ulcerative colitis had significant associations with postoperative DVT. This corroborated and confirmed the report of increased risk of developing DVT or PE in inflammatory bowel disease patients by Bernstein.12 However, we did not find a statistically significant association between Crohn’s disease and postoperative DVT. That could be explained by the limited number of patients with Crohn’s disease in our study or by more aggressive prophylactic treatment in this group. Crohn’s disease has been introduced as a risk factor of VTE by literature.12 Among procedural factors, open surgical technique had a higher risk of postoperative DVT compared to laparoscopic technique. The higher risk of VTE events after open surgery has been previously recognized.1 Our results show that open colorectal procedures are associated with 33 % increased risk of DVT and 73 % increased risk of PE compared to laparoscopic procedures. In addition, we found that following discharge, patients who underwent open surgery still had a higher ongoing risk of VTE compared to laparoscopic procedures (0.6 vs. 0.5 %, AOR 1.33, P = 0.03), despite longer hospital stays. Also, among procedural factors, anesthesia length more than 150 min is a predictor of postoperative DVT. We confirmed the report of longer operation time in patients who have postoperative VTE by Flordal.13 Flordal, with a study of 2,070 patients undergoing abdominal surgery, revealed that an operating time longer than 150 min was a significant risk factor of VTE events. However, there is no independent association between types of colorectal procedures (e.g., segmental colectomy vs. APR) and postoperative VTE. Finally, hospitalization length independent of other risk factors has been associated with DVT events. However, our results suggest that prolonged hospitalization is one of the outcomes of DVT events rather than a reason for DVT (most of the DVT events occur during the first week after surgery and the incidence of DVT decreases over time with continued hospitalization). Interestingly, there was not any significant association between the length of hospitalization before surgery and DVT events following colorectal operation (AOR 1.003, P = 0.33).
Our data identifies eight risk factors for PE following colorectal operation. The strongest predictor of PE is DVT. Conversely, the association between other identified risk factors and PE was very weak compared to the association between DVT and PE. In terms of demographic factors, age >70 has the strongest associations with PE. Among comorbid conditions, hypoalbuminemia, disseminated cancer, steroid use, and obesity have associations with PE. Among pathologic conditions, colon cancer and presence of metastatic cancer have associations with PE. Furthermore, emergent admission and open surgical technique had significant association with PE. Finally, our data shows patients with PE have a significantly longer hospital stay. However, prolonged hospitalization is one of the outcomes of PE events rather than a reason for PE DVT (most of the PE events occur during the first week after surgery) (Fig. 1).
Patients who develop postoperative complications will need specific consideration and evaluation with regard to VTE prevention. We found that patients who had a postoperative complication after surgery had higher rates of VTE events, even with seemingly simple complications like postoperative urinary tract infections. Respiratory complications of ventilator dependency, unplanned intubation, and pneumonia had the highest associations with postoperative DVT events.
Study Limitations
This study is a large retrospective review and is subject to the usual retrospective study biases such as selection bias. Population of the study was selected from the NSQIP database on the basis of ICD-9 and CPT codes at almost 500 hospitals in the USA between the years 2005 and 2011, and there is a wide variety of in-hospital settings and surgeons’ expertise that can affect the study outcome. Patients in this study did not form a homogeneous group, and their primary diagnoses varied broadly. Another limitation is the lack of information about the use and method of prophylactic treatment of VTE as well as duration of prophylactic treatment of VTE in the study that can overestimate or underestimate associations between examined factors and postoperative VTE. Due to the restriction of the database, some of the potentially important predictors that have associations with postoperative VTE were not included in this study (i.e., previous VTE, estrogen therapy).6 The actual time of occurrence of the DVT and PE may be earlier than the reported day because of delay in diagnosis, and that can affect our study results. Patients cannot be tracked long-term as we do not have data beyond 30 days from the date of surgery. Also, coding errors may exist because of the use of discharge data (ICD-9 codes).14 Despite these limitations, this study is one of the first reports on risk factors of VTE in colorectal resection procedures in this population subset.
Conclusion
Colorectal resection complicated by postoperative VTE is uncommon (incidence rate of 2 %) but carries an associated high mortality, morbidity, and prolonged hospitalization length. The first week after an operation was the most common time for postoperative VTE; however, 34.6 % of patients with PE and 29.3 % with DVT were diagnosed after discharge. Obesity has association with both postoperative DVT and PE. After adjustment of results, postoperative DVT predictors include black or African-American race, age >70, emergent admission, anesthesia length >150 min, ASA score greater than 2, obesity, hypoalbuminemia, disseminated cancer, steroid use, and open procedures (compared to laparoscopic procedures). Also, seven factors of DVT—disseminated cancer, age >70, emergency admission, open surgery, hypoalbuminemia, steroid use, and obesity—had association with postoperative PE. Open surgery has a higher risk of VTE events compared to laparoscopic surgery, even after hospital discharge; however, there is no independent association between types of colorectal procedure and postoperative VTE. Among pathologic conditions, ulcerative colitis and metastatic cancer (disseminated cancer) have association with postoperative DVT and colon cancer and metastatic cancer (disseminated cancer) have associations with postoperative PE. In the presence of a postoperative pulmonary complication, the risk of VTE increases.
Based on our findings, patients developing postoperative complications or having multiple risk factors especially ASA score >2 and hypoalbuminemia are at a heightened risk of postoperative DVT even after hospital discharge. Thus, prophylactic treatment of DVT for high-risk patients after hospital discharge may have benefits. Furthermore, patients who already have a DVT and have the risk factors of age >70, hypoalbuminemia, disseminated cancer, steroid use, obesity, emergent admission, and open surgical technique are at a heightened risk of developing PE. These patients may be candidates for tighter screening postoperatively compared to the general surgical population.
These associations and findings need to be validated in future prospective randomized trials to ensure that postsurgical patients with high risk factors for VTE receive the appropriate and optimal screening, prophylaxis, and treatment.
References
Buchberg B, Masoomi H, Lusby K, et al. Incidence and risk factors of venous thromboembolism in colorectal surgery: does laparoscopy impart an advantage? Arch Surg. 2011;146(6):739–743.
Anderson FA, Wheeler HB, Goldberg RJ, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991;151(5):933–938.
Duff J, Walker K, Omari A, Stratton C. Prevention of venous thromboembolism in hospitalized patients: analysis of reduced cost and improved clinical outcomes. J Vasc Nurs. 2013;31(1):9–14.
Shapiro R, Vogel JD, Kiran RP. Risk of postoperative venous thromboembolism after laparoscopic and open colorectal surgery: an additional benefit of the minimally invasive approach? Dis Colon Rectum. 2011;54(12):1496–1502.
Horlander KT, Mannino DM, Leeper KV. Pulmonary embolism mortality in the United States, 1979–1998: an analysis using multiple-cause mortality data. Arch Intern Med. 2003;163(14):1711–1717.
McNally MP, Burns CJ. Venous thromboembolic disease in colorectal patients. Clin Colon Rectal Surg. 2009;22(1):34–40.
Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol. 2007;25(34):5490–5505.
Lyman GH, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(17):2189–2204.
Huber O, Bounameaux H, Borst F, Rohner A. Postoperative pulmonary embolism after hospital discharge. An underestimated risk. Arch Surg. 1992;127(3):310–313.
National Surgical Quality Improvement Program [home page on the Internet] Chicago, IL: American College of Surgeons; 2005. [cited 2012 Jan 17]. Available from: www.acsnsqip.org.
Moghadamyeghaneh Z, Mills SD, Pigazzi A, Carmichael JC, Stamos MJ. Risk Factors of Postoperative Upper Gastrointestinal Bleeding Following Colorectal Resections. J Gastrointest Surg. 2014.
Bernstein CN, Blanchard JF, Houston DS, Wajda A. The incidence of deep venous thrombosis and pulmonary embolism among patients with inflammatory bowel disease: a population-based cohort study. Thromb Haemost. 2001;85(3):430–434.
Flordal PA, Berggvist D, Burmark US, Ljungström KG, Törngren S. Risk factors for major thromboembolism and bleeding tendency after elective general surgical operations. The Fragmin Multicentre Study Group. Eur J Surg. 1996;162(10):783–789.
Lorence DP, Ibrahim IA. Benchmarking variation in coding accuracy across the United States. J Health Care Finance. 2003;29(4):29–42.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as a lunchtime poster presentation at the Tripartite Colorectal Meeting 2014 last July 1, 2014, in Birmingham, UK.
Rights and permissions
About this article
Cite this article
Moghadamyeghaneh, Z., Hanna, M.H., Carmichael, J.C. et al. A Nationwide Analysis of Postoperative Deep Vein Thrombosis and Pulmonary Embolism in Colon and Rectal Surgery. J Gastrointest Surg 18, 2169–2177 (2014). https://doi.org/10.1007/s11605-014-2647-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2647-5