Abstract
Background
Race/ethnicity has long been suspected to affect survival in patients with gastric adenocarcinoma. However, the clinicohistopathological impact of race or ethnicity on early gastric cancer (EGC) is not known.
Methods
From 2000 to 2013, 286 patients underwent gastrectomy and 104 patients had pathological confirmation of EGC. A retrospective analysis of pathological and clinical prognostic indicators was performed.
Results
The study population consisted of 38 (37 %) Asian Americans and 66 (63 %) non-Asian Americans. Of these, 2 (5.3 %) Asian Americans and 19 (28.8 %) non-Asian Americans had pathological confirmation of lymph node metastasis (LNM) (p = 0.004). Univariate analysis comparing the clinicohistopathological characteristics in each group did not reveal significant difference regarding histotype, tumor size, grade, location, morphology, or lymphovascular invasion, except for the LNM rate and mean body mass index (23.2 versus 26.6, p < 0.001). Multivariate analysis showed that non-Asian race/ethnicity (odds ratio (OR), 9.09; 95 % confidence interval (CI), 1.12–71.43; p = 0.038), younger age (OR, 1.11; 95 % CI, 1.01–1.12; p = 0.046), and lymphovascular invasion (OR, 13.9; 95 % CI, 2.40–79.99; p = 0.003) were significant predictors for LNM.
Conclusions
This study demonstrated that Asian American race in EGC is associated with a significantly decreased rate of LNM in comparison to non-Asian Americans, despite similar histopathological characteristics of each group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of early gastric cancer (EGC), defined as invasive gastric adenocarcinoma confined to the mucosa (T1a) or submucosa (T1b) of the stomach irrespective of lymph node metastasis (LNM) or tumor size, originated in Japan in 1962.1,2 In other words, EGC is not necessarily “early stage” gastric cancer. Gastrectomy with lymphadenectomy is the gold standard for curative-intent resection for EGC, although lymph node (LN) dissection is not always required and endoscopic or local surgical resection may be an alternative treatment option for patients with negligible risk of LNM.
Race/ethnicity has long been suspected to influence survival in patients with gastric adenocarcinoma. The overall 5-year survival after curative-intent gastrectomy in Eastern Asian countries, even stratified by stage, has been consistently more favorable compared to the 5-year overall survival seen in studies performed in the West.3–5 The cause of these outcome disparities in gastric cancer between patients in Eastern Asian and Western countries has been extensively debated. One theory hypothesizes that this discrepancy in outcomes originates from the difference in tumor biology.6 Other theories suggest that variations in patient management, including the quality of the surgery performed, perioperative chemoradiotherapy, the interpretation of histopathology, and resultant stage migration, can be important contributors to differences in survival between patients.7,8
The evidence for endoscopic resection for EGC has mostly been derived from studies conducted in Japan where there is a high prevalence of EGC. More extended indications have been recently proposed to account for the development of new technology such as endoscopic submucosal dissection (ESD).9 However, as these studies have been performed largely in countries with racial homogeneity that is significantly different from the racial composition of Western populations such as in the USA, caution should be used when applying these guidelines to patient populations outside of Asia. Unfortunately, comparable data looking at endoscopic treatment for EGC from Western countries is sparse. Clearly, US institutions performing ESD for EGC are still very limited due to its technical challenge, device unavailability, and lack of standardized algorithm for training or patients with EGC with suitable stage. Despite all the obstacles, ESD applications are continuing to grow in the West.9,10 Therefore, investigations addressing the discrepancies in tumor biology and aggressiveness conducted in racially diverse Western countries are needed to identify appropriate selection criteria for minimally invasive treatments in the West.
The aim of the present study is to compare the histopathological characteristics between EGC in Asian American and non-Asian American populations diagnosed and treated in a large urban teaching hospital in New York City, to assess if race/ethnicity should influence our current treatment strategies for EGC.
Methods
The Institutional Review Board approved all aspects of the present study.
Patient Selection
From January 1, 2000 to November 30, 2013, 1,020 patients were registered in the Gastric Cancer Registry of Continuum Cancer Center, a major urban teaching hospital in New York City. Of these, 286 patients underwent curative-intent gastrectomies and 104 (10.2 % of all registered patients and 36.4 % of patients who underwent gastrectomy) had pathological confirmation of EGC by our pathologists. Demographic data (age at diagnosis, gender, comorbidity data, body mass index (BMI), race, and ethnicity), preoperative diagnostic workup including reports of gastroscopy and its biopsy results, endoscopic ultrasonography and abdominal computerized tomography, and treatment-related/histopathological variables were retrospectively reviewed. Patients with concurrent malignancy in other organs, those with gastroesophageal junction tumors, and those who received neoadjuvant therapy were excluded from the study. Staging was performed according to the American Joint Committee on Cancer (AJCC) staging system.11 Patients were grouped by race and ethnicity as identified by patient report and/or medical records. The standard lymphadenectomy employed by our institution includes D1 or greater. LNs were separated and retrieved from the specimen by pathologists. Complications were graded 1–5 on the basis of the modified classification of complications.12 The highest-ranked complication for each case was used for the analysis.
Statistical Analysis
Continuous variables were expressed as mean ± 1 standard deviations. Categorical variables were presented as proportions and absolute numbers. Differences between groups were detected using the chi-square test for categorical variables and Student’s t test or the Mann–Whitney U test for continuous variables. Logistic regression analysis was used to identify the multivariate predictors of LNM. The clinically relevant variables were entered into the final model. Correlation analysis between each variable was performed (Pearson or Spearman as appropriate) to ensure no violation of the assumption of multicollinearity (the cut-off correlation coefficient < 0.7). The model fit and predictive power were validated with the Hosmer and Lemeshow goodness-of-fit test and c-statistic, respectively. Results are presented as an odds ratio (OR) with corresponding 95 % confidence intervals (CI). A p value <0.05 was considered to be statistically significant. All p values were results of two-tailed tests. The statistical analysis was performed using IBM SPSS Statistics for Windows, version 22 (SPSS, Inc., IBM Corporation, Armonk, NY, USA).
Propensity Matching
All patients were subjected to propensity matching using the sequential nearest neighbor selection technique. Propensity matching employed the following variables: age, gender, tumor depth, size, tumor grade, morphology, histotype, tumor location, and BMI. Lymphovascular invasion was not included for the matching because of the collinearity with LN positivity. Thirty-seven matched pairs (n = 74) were identified and were compared in this study. The SAS system v9.2 (SAS Institute, Cary NC) was used for the propensity matching.
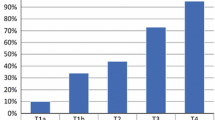
Results
The study population was comprised of 104 patients (43 females) ages 38–86 years with a mean age of 65 ± 12 years. Of the 104 patients, 38 (37 %) were of Asian descent, 26 (25 %) were White, 26 (25 %) Hispanic or Latino, 13 (13 %) African-American, and 1 (1 %) was Native Hawaiian or Pacific Islander. Subjects were grouped by race and ethnicity into 38 Asian Americans and 66 non-Asian Americans. Demographic, clinical, histopathological, and treatment variables in each group are shown in Table 1, and histopathological variables are further displayed in Table 2. BMI was significantly lower in Asian Americans compared to the non-Asian American group (23.2 ± 2.5 versus 26.6 ± 4.9; p < 0.001). Gastric resections included 22 (21 %) total gastrectomies, 1 (1 %) proximal gastrectomy, and 81 (78 %) distal subtotal gastrectomies. Twenty-three (60.5 %) Asian Americans and 33 (50.0 %) non-Asian Americans had T1a lesions on final pathology and 15 (39.4 %) Asian Americans and 33 (50.0 %) non-Asian Americans had T1b lesions, respectively (p = 0.30). A total of 21 (20.2 %) patients had LNM: 2 (5.3 %) Asian Americans and 19 (28.8 %) non-Asian Americans (p = 0.004). When analyzed by T stage, 1 (4.4 %) Asian and 3 (9.1 %) non-Asians with T1a lesions and 1 (6.6 %) Asian and 16 (48.5 %) non-Asians with T1b lesions had associated LNM (p = 0.50 and 0.005, respectively). Two (5.3 %) Asian Americans and 16 (24.2 %) non-Asian Americans received adjuvant chemotherapy with or without radiotherapy (p = 0.014). The mean number of LNs retrieved was 15.7 ± 11.7 in Asian Americans and 17.6 ± 13.3 in non-Asian Americans, respectively (p = 0.58). Subgroup analysis comparing the histopathological characteristics in each group did not reveal significant difference in histology type, tumor location, tumor grade, size, morphology, or presence of lymphovascular invasion. Multivariate analysis showed that non-Asian race/ethnicity (OR, 9.09; 95 % CI, 1.12–71.43; p = 0.038), younger age (OR, 1.11; 95 % CI, 1.01–1.12; p = 0.046), and presence of lymphovascular invasion (OR, 13.9; CI, 2.40–79.99; p = 0.003) were significant predictors for LNM (Table 3). Table 4 shows the predictors of positive lymph nodes for the 74 propensity-matched Asian and non-Asian American patients. The two groups were closely matched for age, gender, depth, tumor grade and size, histology type, and BMI, while the incidence of positive nodal disease remained higher for the non-Asian American group (p = 0.043; OR, 4.11).
Discussion
This study represents the first analysis describing the discrepancies in clinicopathological features of EGC between Asian and non-Asian Americans. The racially and culturally diverse New York metropolitan population allowed for the wide variety of races/ethnicities necessary to conduct this unique study.
Historically, it has long been postulated that race/ethnicity influences the outcomes of patients with gastric cancer. It was hypothesized that these observed favorable outcomes in Asians may reflect a less aggressive tumor biology.13 In addition, multi-institutional and multi-national comparisons have been attempted to further elucidate the superior survival in Asians and multiple factors have been suggested, including differences in tumor histological type, disease location, environmental factors, Helicobacter pylori status, extent of lymphadenectomy, or pathological interpretation.7,14–19 However, they have been confounded by inherent inconsistencies both in the approach to their investigation and institution-related variability in patient care.5 As such, the validity of the hypothesis that Asian race is an independent predictor of favorable outcome still remains undetermined, despite those previous extensive investigations. Stage migration, potentially induced by differences in the quality of surgery and pathological interpretation, has also clearly been a factor further fueling this unsettled debate between previous studies. Western pathologists consider invasion into the lamina propria of the mucosa mandatory for the diagnosis of carcinoma, whereas nuclear and structural features are more important for the Japanese.7,20 Therefore, EGC lesions diagnosed in Japan may be diagnosed as high grade dysplasia in the West. This may also contribute to the relatively high incidence of EGC and, at least partially, the corresponding superior prognosis and early detection in Japan compared with Western countries. Also, differences in the extent of LN retrieval from fresh specimens can also impact the stage assignment and account for stage-adjusted survival discrepancies.21 In Asian centers, surgeons meticulously dissect specimens after surgery and harvest the LNs from various stations prior to delivering the specimen to the pathologists,22 unlike the standard practice in the USA where the pathologist dissects the specimen. This effort, of which many clinicians in the West may not be aware, of scrutinizing the specimens is likely another explanation for consistently higher quantity of LN retrieval in the Eastern series besides the routinely performed more extensive lymphadenectomy. In the current study, all patients underwent gastrectomy by a set number of US surgeons and had their specimens examined by US pathologists from the same department. This study minimized the potential for stage migration and/or disparities in the patient care, which were all non-adjustable confounding factors in previous studies. In addition, this study examines EGC from multiple races/ethnicities all treated in the USA unlike previous EGC studies exclusively from Eastern countries.
As described, there have been thus far no studies addressing the impact of race/ethnicity on the incidence of LNM among those with EGC, despite previous extensive debates. There have been several excellent studies investigating the discrepancy in outcomes between Asian and non-Asian.3–5 However, comparing stage-specific or race/ethnicity-specific LNM rate was not the primary purpose of these studies. They only grouped their subjects into three categories, which precludes investigation into stage-specific management: localized (T1–3, N0), regional (T4 or N+), or distant disease. More importantly, they lacked information regarding neoadjuvant treatment status. Comparison of each corresponding LN status without knowing neoadjuvant treatment status is impossible.
Minimizing risk for LNM is the most critical prerequisite for performing limited local treatment of EGC; however, data on risk factors for LNM in Western patients with EGC is scarce. EGC is less commonly diagnosed in the USA than in Asian countries, where universal health insurance affords easier access to nationwide screening; the low incidence of gastric cancer in the West is clearly a contributing factor to the paucity of the data on EGC in the West. In a retrospective review of 165 patients undergoing surgical resection for T1 gastric tumors at a major US cancer center, multivariate analysis revealed the presence of submucosal invasion, venous invasion, and size equal to or greater than 4.5 cm were significantly associated with an increased risk for LNM.23 Race/ethnicity was not assessed in this study, and the vast majority of these patients were Caucasians. Moreover, those tumors that were 4.5 cm and larger and had penetrated into the submucosa (n = 16) had an astonishing 56 % incidence of LNM.
In the present study, the Asian American group had a significantly lower rate of LNM compared to that of the non-Asian Americans (2 (5.3 %) versus 19 (28.8 %) (p = 0.004)), despite similar histopathological characteristics of each group (Table 2). Of note, 9 out of 19 (13.6 %) patients in the non-Asian American group were N2 disease. This point is further emphasized by multivariate analysis of potential predictors for LNM, which revealed that younger age and presence of lymphovascular invasion are significant predictors of LNM, while Asian American race is a significant protective factor for nodal metastasis with an odds ratio of 0.11 (p = 0.038). Similar results were demonstrated after propensity matching (Table 4), which was further employed to strengthen our results. Large tumor size and lymphovascular invasion are known predictors of LNM in EGC.24,25 Although very young patients with gastric adenocarcinoma are known to have a more severe form of the disease,26 the odds ratio of 1.11 indicates a weak association from our study, which had only 11 (10.6 %) patients who were less than 50 years old.
Another remarkable difference between the two groups was the BMI. Theoretically, increased BMI could result in inadequate LN collection and/or identification, leading to potential under-staging of the disease.27 Nevertheless, the LNM rate in non-Asian Americans who demonstrated significantly higher BMI was significantly greater in this study, despite potential inadequate LN sampling and subsequent under-staging. In fact, this study did not show any difference in the adequacy of LN retrieval between the two groups, although inadequate LN sampling due to obesity might have been offset by the higher rate of open laparotomy approach in the non-Asian group (61 versus 88 %, p = 0.001). Regardless of the race/ethnicity, there was no statistical correlation between BMI and the number of LN retrieved. To date, there have been only a few studies investigating the influence of BMI on gastric cancer. The most recent US study demonstrated an increase of postoperative complications associated with a higher BMI but did not demonstrate differences in nodal positivity or survival.27 Moreover, Asian series of gastrectomy for gastric adenocarcinoma comparing obese to non-obese patients have also demonstrated no correlation between obesity and LNM rate,28,29 suggesting higher BMI alone has little influence on the nodal positivity in gastric cancer.
One potential significant factor resulting in inferior outcomes in non-Asians is the increasingly high proportion of both proximal and diffuse tumors in the West, where total gastrectomy has been associated with twice the mortality of a subtotal resection.30 In the present study, there was no statistical difference between each group in terms of the location of the tumor and the proportion of total gastrectomy. Clearly, there were less postoperative complications in Asian American group, perhaps these may be attributed mostly to differences in medical comorbidities and BMI of each patient in addition to less frequent open approach. Patients in non-Asian American group were observed to receive adjuvant therapy more often than Asian Americans and is a reflection of the higher LNM rate in non-Asian Americans.
There is no compelling hypothesis formulated to explain this observed difference of LNM rate between the two groups. Strong et al. compared US patients with node-negative EGC with similarly staged Koreans.31 The survival did not differ significantly between them, suggesting that gastric adenocarcinoma is a heterogeneous disease and when similar subtypes are compared, these differences disappear. In comparison, we postulate that this well-known survival advantage in Asian populations is due to less aggressive tumor biology predominantly related to differences in metastatic potential as shown in this study. This fact might have been consistently masked in the previous studies which included a large number of patients with advanced disease that can frequently demonstrate LNM regardless of race/ethnicity. If the biology of gastric cancer in patients of Asian and non-Asian populations are truly different, clinical data of EGC utilizing a study population consisting exclusively of Asian patients treated in their respective countries may simply not be applicable to patients in Western countries.
Study Limitations
There are several limitations to this study. Our investigation is limited by its small population and retrospective nature. Although the difference in histopathological characteristics of each group did not show any statistical significance in our study, this may not reflect the true histopathological difference among the general population. In addition, most patients (92 %) in our Asian American cohort are Chinese descent and thus may not represent the general Asian American population. Based upon previous observation, the differences in survival were apparent even among different Asian ethnic subgroups. Specifically, Korean American patients demonstrated the highest overall survival following surgical resection for gastric cancer.32,33 Clearly, additional large-scale studies involving patients with broad categories of Asian/non-Asian ethnicity are necessary to further validate our results.
Conclusions
The present study has demonstrated that Asian Americans with EGC are associated with a lower rate of LNM compared to non-Asian Americans despite similar histopathological characteristics of each group and treatment at the same US institution, providing new insight into the unsettled debate of racial discrepancies in gastric cancer outcomes. This study highlights the potential role of race/ethnicity when considering the applicability of endoscopic or limited surgical gastric resection for EGC in non-Asian populations. Although endoscopic dissection is an emerging alternative treatment for selected EGC in the East, non-Asian populations should be treated endoscopically with extreme caution in light of the findings in this study. Non-Asian race/ethnicity may be an independent prohibitive risk for LNM. Larger studies of EGC in non-Asian patients are needed to better guide treatment decisions in this patient population that appear to have more aggressive tumor biology.
References
Carter KJ, Schaffer HA, Ritchie WP. Early gastric cancer. Ann Surg 1984;199:604–9.
Murakami T. Early cancer of the stomach. World J Surg. 1979;3:685–92.
Theuer CP, Kurosaki T, Ziogas A, Butler J, Anton-Culver H. Asian patients with gastric carcinoma in the United States exhibit unique clinical features and superior overall and cancer specific survival rates. Cancer. 2000;89:1883–92.
Kim J, Sun CL, Mailey B, Prendergast C, Artinyan A, Bhatia S, Pigazzi A, Ellenhorn JD. Race and ethnicity correlate with survival in patients with gastric adenocarcinoma. Ann Oncol. 2010;21:152–60.
Gill S, Shah A, Le N, Cook EF, Yoshida EM. Asian ethnicity-related differences in gastric cancer presentation and outcome among patients treated at a canadian cancer center. J Clin Oncol. 2003;21:2070–6.
Leung WK, Wu MS, Kakugawa Y, Kim JJ, Yeoh KG, Goh KL, Wu KC, Wu DC, Sollano J, Kachintorn U, Gotoda T, Lin JT, You WC, Ng EK, Sung JJ. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol. 2008;9:279–87.
Schlemper RJ, Itabashi M, Kato Y, Lewin KJ, Riddell RH, Shimoda T, Sipponen P, Stolte M, Watanabe H, Takahashi H, Fujita R. Differences in diagnostic criteria for gastric carcinoma between Japanese and western pathologists. Lancet. 1997;349:1725–9.
Brar S, Law C, McLeod R, Helyer L, Swallow C, Paszat L, Seevaratnam R, Cardoso R, Dixon M, Mahar A, Lourenco LG, Yohanathan L, Bocicariu A, Bekaii-Saab T, Chau I, Church N, Coit D, Crane CH, Earle C, Mansfield P, Marcon N, Miner T, Noh SH, Porter G, Posner MC, Prachand V, Sano T, van de Velde C, Wong S,Coburn N. Defining surgical quality in gastric cancer: a RAND/UCLA appropriateness study. J Am Coll Surg. 2013;217:347–57.
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Fukami N. ESD Around the World: United States. Gastrointest Endosc Clin N Am. 2014;24:313–320.
American Joint Committee on Cancer. Cancer staging manual. 7th ed. Chicago: Springer; 2010.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Strong VE, Song KY, Park CH, Jacks LM, Gonen M, Shah M, Coit DG, Brennan MF. Comparison of gastric cancer survival following R0 resection in the United States and Korea using an internationally validated nomogram. Ann Surg. 2010;251:640–6.
Karpeh MS, Leon L, Klimstra D, Brennan MF. Lymph node staging in gastric cancer: is location more important than Number? An analysis of 1,038 patients. Ann Surg. 2000;232:362–371.
Theuer CP. Asian gastric cancer patients at a southern California comprehensive cancer center are diagnosed with less advanced disease and have superior stage-stratified survival. Am Surg. 2000;66:821–826.
Noguchi Y, Imada T, Matsumoto A, Coit DG, Brennan MF. Radical surgery for gastric cancer. A review of the Japanese experience. Cancer. 1989;64:2053–2062.
Schwarz RE, Zagala-Nevarez K. Ethnic survival differences after gastrectomy for gastric cancer are better explained by factors specific for disease location and individual patient comorbidity. Eur J Surg Oncol. 2002;28:214–9.
Bollschweiler E, Boettcher K, Hoelscher AH, Sasako M, Kinoshita T, Maruyama K, Siewert JR. Is the prognosis for Japanese and German patients with gastric cancer really different? Cancer. 1993;71:2918–25.
Yao JC, Schnirer II, Reddy S, Chiang S, Najam A, Yu C, Giacco G, Hess K, Rashid A, Xie K, Lynch P, Ajani JA. Effects of sex and racial/ethnic group on the pattern of gastric cancer localization. Gastric Cancer. 2002;5:208–12.
Schlemper RJ, Kato Y, Stolte M. Review of histological classifications of gastrointestinal epithelial neoplasia: differences in diagnosis of early carcinomas between Japanese and Western pathologists. J Gastroenterol. 2001;36:445–56.
Bunt AM, Hermans J, Smit VT, van de Velde CJ, Fleuren GJ, Bruijn JA. Surgical/pathologic-stage migration confounds comparisons of gastric cancer survival rates between Japan and Western countries. J Clin Oncol. 1995;13:19–25.
Kodera Y. Surgery for gastric cancer: Has the East versus West issue been solved? Dig Surg. 2013;30:92–5.
Hochwald SN, Brennan MF, Klimstra DS, Kim S, Karpeh MS. Is lymphadenectomy necessary for early gastric cancer? Ann Surg Oncol. 1999;6:664–70.
Seto Y, Nagawa H, Muto T. Impact of lymph node metastasis on survival with early gastric cancer. World J Surg. 1997;21:186–9.
Li H, Lu P, Lu Y, Liu C, Xu H, Wang S, Chen J. Predictive factors of lymph node metastasis in undifferentiated early gastric cancers and application of endoscopic mucosal resection. Surg Oncol. 2010;19:221–6.
Smith BR, Stabile BE. Extreme aggressiveness and lethality of gastric adenocarcinoma in the very young. Arch Surg. 2009;144:506–10.
Bickenbach KA, Denton B, Gonen M, Brennan MF, Coit DG, Strong VE. Impact of obesity on perioperative complications and long-term survival of patients with gastric cancer. Ann Surg Oncol. 2013;20:780–7.
Sugimoto M, Kinoshita T, Shibasaki H, Kato Y, Gotohda N, Takahashi S, Konishi M. Short-term outcome of total laparoscopic distal gastrectomy for overweight and obese patients with gastric cancer. Surg Endosc. 2013;27:4291–6.
Lin YS, Huang KH, Lan YT, Fang WL, Chen JH, Lo SS, Hsieh MC, Li AF, Chiou SH, Wu CW. Impact of body mass index on postoperative outcome of advanced gastric cancer after curative surgery. J Gastrointest Surg. 2013;17:1382–91.
Griffin SM. Gastric cancer in the East: same disease, different patient. Br J Surg. 2005;92:1055–6.
Strong VE, Song KY, Park CH, Jacks LM, Gonen M, Shah MA, Coit DG, Brennan MF. Comparison of disease-specific survival in the United States and Korea after resection for early-stage node-negative gastric carcinoma. J Surg Oncol. 2013;107:634–40.
Nelson R, Ko EB, Arrington A, Lee W, Kim J, Garcia-Aguilar J, Kim J. Race and correlations between lymph node number and survival for patients with gastric cancer. J Gastrointest Surg. 2013;17:471–81.
Kim J, Mailey B, Senthil M, Artinyan A, Sun CL, Bhatia S. Disparities in gastric cancer outcomes among Asian ethnicities in the USA. Ann Surg Oncol. 2009;16:2433–41.
Coman RM, Gotoda T, Draganov PV. Training in endoscopic submucosal dissection. World J Gastrointest Endosc. 2013;5:369–78.
Conflict of Interest
The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukuhara, S., Yabe, M., Montgomery, M.M. et al. Race/Ethnicity Is Predictive of Lymph Node Status in Patients with Early Gastric Cancer. J Gastrointest Surg 18, 1744–1751 (2014). https://doi.org/10.1007/s11605-014-2590-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2590-5