Abstract
Background
Surgical treatment for locally recurrent rectal cancer is challenging, and the value of laparoscopic surgery in such cases is unknown. The purpose of this study was to compare the feasibility of laparoscopic surgery with that of open surgery for locally recurrent rectal cancer.
Methods
Thirty patients with local rectal cancer recurrence at the anastomotic site or lateral pelvic lymph nodes were evaluated. Perioperative outcomes were compared between the laparoscopic (n = 13) and open (n = 17) groups.
Results
The median operation time was significantly longer (381 vs. 241 min) but the median estimated blood loss tended to be smaller (110 vs. 450 mL) in the laparoscopic than in the open group. There was only one converted case (7.7 %). The R0 resection rate (100 vs. 94 %) and postoperative complications (31 vs. 24 %) were not significantly different between the two groups. The median times to flatus (1 vs. 2 days), first stool (2 vs. 5 days), and oral intake (2 vs. 5 days) were significantly shorter in the laparoscopic than in the open group.
Conclusion
Laparoscopic surgery for locally recurrent rectal cancer has short-term benefits over open surgery and has potential as a treatment option for locally recurrent rectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent advances in neoadjuvant chemoradiotherapy (CRT) and wide acceptance of total mesorectal excision have significantly improved the oncologic outcomes of patients with rectal cancer.1 , 2 Current studies report 5-year local recurrence rates of 5 to 10 % in contrast to the 20 to 30 % reported in previously published studies.3 – 7 Despite these advances, treatment of locally recurrent rectal cancer (LRRC) remains an important clinical problem. Radical surgery for LRRC is associated with potential difficulties in relation to anatomical complexity and was historically associated with high morbidity and mortality.4 , 8 Technical difficulties and the extent of salvage surgery depend on the site of recurrence, contact and relationship with or without fixation to surrounding structures, and influences of previous operations and/or CRT.
Laparoscopic surgery is an accepted treatment method for primary colorectal cancer. The increasing experience of dedicated surgeons and the progressive improvements in technology have recently made it possible to extend the indications for laparoscopic surgery to patients who could previously only undergo open surgery9 and to patients with locally advanced rectal cancer.10 – 12 However, there are very few studies on the safety and feasibility of laparoscopic surgery for LRRC.13 – 15 The objective of the present study was to assess the feasibility and safety of laparoscopic surgery for LRRC compared with those of open surgery.
Patients and Methods
Patients were included in the present study if they had undergone resection with curative intent for LRRC by a laparoscopic or open approach between July 2005 and October 2013. This retrospective study was approved by our institutional review board. Laparoscopic surgery for primary colorectal cancer was introduced at our institution in July 2005. Initially, the contraindications to laparoscopic surgery included bulky tumors, tumors invading adjacent organs, and tumors with lateral pelvic lymph node metastasis. However, the indications for laparoscopic surgery were gradually extended in accordance with the increased experience of our teams, and there are no definite contraindications to laparoscopic surgery at present. The final indications were determined at our team meetings. Laparoscopic surgery for LRRC was initiated in July 2010 and was performed only in cases of recurrence at the anastomotic site (AS) (n = 8) or lateral pelvic lymph nodes (LPLN) (n = 5) in our study period. Laparoscopic pelvic exenteration with or without sacrectomy for LRRC was not performed in the study period, although we have experiences of such procedures in patients with primary rectal cancer.10 – 12 For comparison of laparoscopic surgery for LRRC, we included only patients who underwent open salvage surgery for LRRC at the AS (n = 8) or LPLN (n = 9). All enrolled patients had undergone curative resection for primary rectal cancer. Patients with LRRC who had synchronous distant metastasis principally amenable to surgery were included. Cases of palliative surgery for LRRC were not included in this study.
The clinical features of patients who underwent primary and salvage surgery were fully reviewed, including sex distribution, the age at the time of primary surgery, location of primary cancer, type of operation for primary cancer, operative procedures for primary cancer, pathological stage, performance or nonperformance of adjuvant chemotherapy after the primary surgery, age at the time of salvage surgery, body mass index (kg/m2), American Society of Anesthesiologists (ASA) classification score, interval between operations for primary and recurrent cancers, site of recurrence, and performance or nonperformance of neoadjuvant therapy before salvage surgery. The perioperative and postoperative outcomes of patients who underwent salvage surgery were also investigated, including type of surgical procedure for recurrent cancer, adjacent structures removed en bloc during resection, performance or nonperformance of combined resection, operation time, estimated blood loss, performance or nonperformance of blood transfusion, conversion to open surgery, pathological margin status of specimen, time to first flatus, time to first stool, time to first oral intake, rate of postoperative complications, postoperative hospital stay, relapse-free survival, disease-specific survival, and overall survival after salvage surgery. Data were compared between patients who underwent laparoscopic (n = 13) and open (n = 17) surgery for LRRC.
All patients underwent evaluation by our multidisciplinary team meeting, and neoadjuvant therapy was performed in 13 patients (43 %). Neoadjuvant therapy included long-course oral 5-fluorouracil-based CRT with a total dose of 45 Gy (six patients) or 50.4 Gy (two patients) in eight patients, systemic chemotherapy followed by long-course CRT in one patient, systemic chemotherapy followed by short-course radiotherapy (5 × 5 Gy) in one patient, and systemic chemotherapy in three patients. The lateral pelvic area was usually included in the radiation target volume.
Laparoscopic surgery was performed using a five-port technique, as we previously described.16 , 17 Hand-assist technique was not used in any patient. Regarding the laparoscopic surgery for LRRC at AS, the dissection around the reconstructed colon and anastomotic site was performed sufficiently down to the pelvic floor. In low anterior resection, the rectum was transected using a linear stapler intracorporeally, and the specimen was extracted through an umbilical port site, which was extended to about 4 cm. The anastomosis was completed intracorporeally by double-stapling technique.16 , 17 In intersphincteric resection, the specimen was extracted through the anus, and a hand-sewn colo-anal anastomosis was performed. In abdominoperineal resection, the specimen was extracted through the perineal incision. Laparoscopic LPLN dissection (LPLD) was performed for local recurrence at the LPLN in a similar fashion with LPLD for LPLN metastasis in primary advanced low rectal cancer, as we previously described18 (Fig. 1). The internal, external, and obturator lymph nodes were basically dissected en bloc with exposure of landmark structures such as the external iliac artery/vein, internal obturator muscle, pelvic plexus, common iliac artery bifurcation, levator ani muscle, and sciatic nerve (Fig. 2). The decision to resect the internal iliac artery or its branching arteries such as the umbilical, superior or inferior vesical, or obturator artery en bloc with LPLN was at the surgeon’s discretion, but we usually resected the adjacent arteries if metastatic LPLN invasion was suspected. The obturator nerve was consistently preserved.7 If a patient presented with lymph node swelling on only one pelvic side, LPLD was performed on the same side; bilateral LPLD was conducted only in patients with suspected cancer metastasis in the bilateral LPLN.
Magnetic resonance images of a patient with recurrence at the right lateral pelvic lymph node. a Before chemoradiotherapy for recurrence at the right lateral pelvic lymph node (white arrow). b After chemoradiotherapy, the tumor was reduced in size (white arrow). This patient underwent laparoscopic right lateral pelvic lymph node dissection combined with seminal vesicle and pelvic plexus resection
The data are presented as median values with ranges. Categorical variables were compared using the chi-square test or Fisher’s exact test as appropriate. Continuous variables were analyzed with the Mann–Whitney U-test. Survival analysis was performed using the Kaplan–Meier method with the log-rank test. All p values of <0.05 were considered as statistically significant.
Results
The study population comprised of 30 patients (21 men and nine women) with LRRC. Table 1 shows the clinical characteristics of patients included in the present study. The 30 patients included 13 (43.3 %) who underwent laparoscopic surgery and 17 (56.7 %) who underwent open surgery for LRRC. There were no significant differences in the sex distribution, age at the time of primary surgery, location of primary cancer, type of primary operation, operative procedures for primary cancer, pathological stage, and performance or nonperformance of adjuvant chemotherapy after primary operation. Laparoscopic surgery was performed in half of the patients with primary rectal cancer. The surgical procedures for primary cancer were low anterior resection in 26 of the 30 patients (86.7 %), including one patient who underwent concurrent unilateral pelvic lymph node dissection, abdominoperineal resection in two (6.7 %), intersphincteric resection in one (3.3 %), and subtotal colectomy in one (3.3 %). Only one patient developed recurrence at the LPLN after LPLD. Our study also included four patients with stage IV disease; three had liver metastasis and one had para-aortic lymph node metastasis. All four patients underwent simultaneous radical resection. No patients underwent preoperative CRT or systemic chemotherapy for primary rectal cancer. Adjuvant chemotherapy after primary surgery was performed in 15 of the 30 patients.
There were no significant differences in the age at the time of salvage surgery, body mass index, ASA status, interval between operations for primary and recurrent cancer, and site of recurrence. The rate of an ASA score of II tended to be higher in the laparoscopic group than in the open surgery group (p = 0.0606). Twenty-five patients (83.3 %) were asymptomatic at the time of recurrence, and the local recurrences were discovered during a routine postoperative follow-up examination. In 80 % of cases, rectal cancer recurrence occurred within 3 years of the primary surgery. The median interval between primary surgery and salvage surgery was 21 months (range, 3–70 months). The site of recurrence was the AS in 16 of 30 patients (53.3 %) and LPLN in 14 patients (46.7 %). Neoadjuvant therapy before salvage surgery was performed in 13 of 30 patients (43.3 %) and tended to be more frequently performed in the laparoscopic group (p = 0.0785).
Table 2 summarizes the surgical outcomes of salvage surgery. Operative procedures, en bloc removal of adjacent structures, and the performance of combined resection were not significantly different between the two groups. The operation time was significantly longer in the laparoscopic group than in the open group (381 vs. 241 min). The estimated volume of blood loss tended to be smaller in the laparoscopic than in the open group (p = 0.0752), but the necessity of blood transfusion was not significantly different between the two groups. Only one patient (7.7 %) in the laparoscopic group required conversion to open surgery due to severe adhesions. All patients in the laparoscopic group underwent R0 resection, but only one in the open group had microscopic focal margin involvement (R1 resection). No patient required reoperation and no death occurred in either group.
Table 3 summarizes the postoperative outcomes of salvage surgery. The times to first flatus (p = 0.0390), first stool (p = 0.0012), and first oral intake (p = 0.0030) were significantly shorter in the laparoscopic than in the open group. The rate of postoperative complications (31 vs. 24 %) and the length of postoperative hospital stay (15 vs. 14 days) did not differ significantly between the two groups.
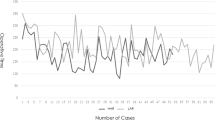
Figure 3 shows the survival rates after salvage surgery. The median follow-up time was 27 months (range, 3–99 months). The 2-year relapse-free survival rates in the laparoscopic and open groups were 73.4 and 64.7 %, respectively, and were not significantly different between the two groups (Fig. 3a). Disease-specific survival (Fig. 3b) and overall survival (Fig. 3c) were not also significantly different between the two groups.
Discussion
Acceptable outcomes and high safety rates of laparoscopic surgery for rectal cancer when performed by experienced surgeons have been reported.16 , 17 However, reports on the safety of laparoscopic surgery for LRRC are scarce.13 – 15
Park et al. recently compared the perioperative outcomes of laparoscopic surgery for recurrent colorectal cancer (n = 15) with those of open surgery (n = 26).15 Seven of the 15 cases involved LRRC. The site of recurrence was the AS in three cases, LPLN in two, para-aortic lymph nodes in one, and ovary in one. To the best of our knowledge, the current report is the first and largest study to analyze the short-term feasibility and safety of laparoscopic surgery for LRRC compared with open surgery. The present study demonstrated that the significantly faster gastrointestinal recovery and estimated blood loss tended to be smaller in the laparoscopic than in the open group. The efficacy of laparoscopic surgery for rectal cancer has already been demonstrated,19 and the present study has shown for the first time that these benefits are also present in laparoscopic surgery for LRRC.
The patterns of local recurrence of rectal cancer have many variations, and the required operative procedures depend on the site of recurrence, relationship with adjacent structures, and presence or absence of fixation to the pelvic wall. Surgery for LRRC usually requires extended resection, including total pelvic exenteration, abdominosacral resection, and combined resection with adjacent organs. Although we previously reported our experiences with laparoscopic performance of these extended surgeries for primary rectal cancer,10 – 12 these operations for LRRC remain to be very complex and challenging procedures. On the other hand, radical resection for recurrence at the AS or LPLN without fixation to the pelvic wall is relatively suitable for performance by laparoscopic surgery. In the current study, we targeted patients with local recurrence limited to the AS or LPLN.
The incidence of recurrence at the AS has been found to range from 1.8 to 7.5 %.20 – 22 Complete resection with a safe surgical margin that includes the previous AS is the main principle of surgical treatment for recurrence at the AS. The planes of dissection may not be obvious because of fibrosis from previous operations, and severe adhesions may develop between the reconstructed colon and surrounding tissues. In particular, adhesions around the AS after double-stapling anastomosis were critically severe, and it was very difficult to dissect the proper layer with either laparoscopic surgery or open laparotomy. To achieve a safe resection margin around the tumor, we often performed combined resection of adjacent structures such as the seminal vesicle, vagina, or levator ani muscle depending on the location of the tumor. We consider that the magnified, clear view obtained by laparoscopy is a great advantage with respect to providing a more accurate image of the dissection, especially at the deep pelvic floor, than that obtained with open surgery. The median operative time for local recurrence at the AS was similar between the two groups (369 vs. 312 min, p = 0.3177), but the median estimated amount of blood loss was significantly smaller in the laparoscopic group (n = 8) than in the open group (n = 8) (108 vs. 575 mL, p = 0.0356). The present study showed that laparoscopic surgery for LRRC at the AS is safe and feasible.
The incidence of local recurrence in the lateral pelvic area (0.2–6.6 %) and the proportion of all local recurrences (6.0–82.7 %) has been reported to range widely and unequally7 , 21 , 23 – 25 because the clinical backgrounds and therapeutic strategies for primary rectal cancer differed among previous reports. The treatment policy for the LPLN differs and remains controversial between Japan and Western countries. In Japan, LPLN are considered to be regional lymph nodes, and LPLD combined with total mesorectal excision is recommended as the standard treatment for advanced low rectal cancer. In our institution, suspected LPLN metastasis is treated by a combination of preoperative CRT and selective LPLD based on pretreatment imaging results.7 We experienced more than 70 cases of laparoscopic LPLD for primary rectal cancer during the study period, and the technique of laparoscopic LPLD has been standardized.7 In the present study, only one patient developed LPLN recurrence after previous LPLD for primary rectal cancer; therefore, the lateral pelvic area had not undergone any previous dissection procedures, and techniques similar to laparoscopic LPLD for primary rectal cancer can be applied in most patients. The median operation time for local recurrence at the LPLN was longer in the laparoscopic group (n = 5) than in the open group (n = 9) (388 vs. 175 min, p = 0.0051). In the laparoscopic group, one patient had severe adhesion after previous open surgery, another had severe fibrosis in the lateral pelvic area because of previous LPLD, and another underwent additional para-aortic lymph node dissection. This is why the operation time was longer in the laparoscopic group than in the open group. However, the present study suggests that laparoscopic surgery for LRRC at the LPLN can be safely performed by experienced surgeons in laparoscopic LPLD.
We immediately converted to open surgery due to severe adhesion in one patient (7.7 %) in the laparoscopic group. The patient underwent open low anterior resection for primary rectal cancer and required re-operation (drainage and construction of ileostomy) for postoperative anastomotic leakage and pan-peritonitis. Patients who are anticipated to have extensive severe adhesions might not be good candidates for laparoscopic surgery for LRRC.
Limitations of the present study include the fact that it included a relatively small number of patients and that the patient backgrounds between the laparoscopic and open groups potentially differed. In addition, the follow-up period was too short to evaluate the long-term outcomes after salvage surgery, and further follow-up was required. However, the present study shows the feasibility and safety of laparoscopic surgery for LRRC at the AS or LPLN, with short-term benefits such as significantly faster gastrointestinal recovery and smaller estimated blood loss.
Conclusion
Our study shows that laparoscopic surgery for LRRC has short-term benefits compared with open surgery, and laparoscopic surgery could be considered as a treatment option for LRRC in selected patients.
References
Heald R., Ryall RD. Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1986;327:1479–1482.
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, Karstens J-H, Liersch T, Schmidberger H, Raab R. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004;351:1731–40.
Kapiteijn E, van de Velde CJH. Developments and quality assurance in rectal cancer surgery. Eur J Cancer 2002;38:919–936.
Palmer G, Martling A, Cedermark B, Holm T. A population-based study on the management and outcome in patients with locally recurrent rectal cancer. Ann Surg Oncol 2007;14:447–454.
Nielsen MB, Laurberg S, Holm T. Current management of locally recurrent rectal cancer. Colorectal Dis 2011;13:732–742.
Silberfein EJ, Kattepogu KM, Hu C-Y, Skibber JM, Rodriguez-Bigas MA, Feig B, Das P, Krishnan S, Crane C, Kopetz S, Eng C, Chang GJ. Long-term survival and recurrence outcomes following surgery for distal rectal cancer. Ann Surg Oncol 2010;17:2863–2869.
Akiyoshi T, Ueno M, Matsueda K, Konishi T, Fujimoto Y, Nagayama S, Fukunaga Y, Unno T, Kano A, Kuroyanagi H, Oya M, Yamaguchi T, Watanabe T, Muto T. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21;189-196.
Vermaas M, Ferenschild FTJ, Verhoef C, Nuyttens JJME, Marinelli AWKS, Wiggers T, Kirkels WJ, Eggermont AMM, de Wilt JHW. Total pelvic exenteration for primary locally advanced and locally recurrent rectal cancer. Eur J Surg Oncol 2007;33:452–458.
Law WL, Lee YM, Chu KW. Previous abdominal operations do not affect the outcomes of laparoscopic colorectal surgery. Surg Endosc 2005;19:326–330.
Nagasue Y, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Nagasaki T, Nagata J, Mukai T, Ikeda A, Ono R, Yamaguchi T. Laparoscopic versus open multivisceral resection for primary colorectal cancer: comparison of perioperative outcomes. J Gastrointest Surg 2013;17:1299–1305.
Mukai T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Ikeda A, Yamaguchi T. Laparoscopic total pelvic exenteration with en bloc lateral lymph node dissection after neoadjuvant chemoradiotherapy for advanced primary rectal cancer. Asian J Endosc Surg 2013;6:314–317.
Nagasaki T, Akiyoshi T, Ueno M, Fukunaga Y, Nagayama S, Fujimoto Y, Konishi T, Yamaguchi T. Laparoscopic abdominosacral resection for locally advanced primary rectal cancer after treatment with mFOLFOX6 plus bevacizumab, followed by preoperative chemoradiotherapy. Asian J Endosc Surg 2014;7:52-55.
Lu A, Wang M, Hu W, Li J, Zang L, Mao Z, Dong F, Feng B, Ma J, Zong Y, Zheng M. Experience of laparoscopic salvage surgery for locally recurrent rectal cancer. Zhonghua Wai Ke Za Zhi 2006;44:597–599.
Kim S, Neve R, Joh Y. Relaparoscopy for salvage surgery in anastomotic recurrence of rectal cancer: feasible and safe. Dis Colon Rectum 2008;1713:1712–1713.
Park SY, Choi G-S, Jun SH, Park JS, Kim HJ. Laparoscopic salvage surgery for recurrent and metachronous colorectal cancer: 15 years’ experience in a single center. Surg Endosc 2011;25:3551–3558.
Akiyoshi T, Kuroyanagi H, Oya M, Konishi T, Fukuda M, Fujimoto Y, Ueno M, Miyata S, Yamaguchi T. Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery 2009;146:483–489.
Kuroyanagi H, Oya M, Ueno M, Fujimoto Y, Yamaguchi T, Muto T. Standardized technique of laparoscopic intracorporeal rectal transection and anastomosis for low anterior resection. Surg Endosc 2008;22:557–561.
Konishi T, Kuroyanagai H, Oya M, Ueno M, Fujimoto Y, Akiyoshi T, Yoshimatsu H, Watanabe T, Yamaguchi T, Muto T. Lateral lymph node dissection with preoperative chemoradiation for locally advanced lower rectal cancer through a laparoscopic approach. Surg Endosc 2011;25:2358-2359.
Morino M, Parini U, Giraudo G, Salval M, Brachet CR, Garrone C. Laparoscopic total mesorectal excision: a consecutive series of 100 patients. Ann Surg 2003;237:335–342.
Sagar PM, Pemberton JH. Surgical management of locally recurrent rectal cancer. Br J Surg 1996;83:293–304.
Kusters M, Beets GL, van de Velde CJH, Beets-Tan RGH, Marijnen CaM, Rutten HJT, Putter H, Moriya Y. A comparison between the treatment of low rectal cancer in Japan and The Netherlands, focusing on the patterns of local recurrence. Ann Surg 2009;249:229–235.
Matsuda A, Kishi T, Musso G, Matsutani T, Yokoi K, Wang P, Uchida E. The effect of intraoperative rectal washout on local recurrence after rectal cancer surgery: a meta-analysis. Ann Surg Oncol 2013:20:856–863.
Kim TH, Jeong S-Y, Choi DH, Kim DY, Jung KH, Moon SH, Chang HJ, Lim SB, Choi HS, Park JG. Lateral lymph node metastasis is a major cause of locoregional recurrence in rectal cancer treated with preoperative chemoradiotherapy and curative resection. Ann Surg Oncol 2008;15:729–737.
Roels S, Duthoy W, Haustermans K, Penninckx F, Vandecaveye V, Boterberg T, De Neve W. Definition and delineation of the clinical target volume for rectal cancer. Int J Radiat Oncol Biol Phys 2006;65:1129–1142.
Syk E, Torkzad MR, Blomqvist L, Ljungqvist O, Glimelius B. Radiological findings do not support lateral residual tumour as a major cause of local recurrence of rectal cancer. Br J Surg 2006;93:113–119.
Conflict of Interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagasaki, T., Akiyoshi, T., Ueno, M. et al. Laparoscopic Salvage Surgery for Locally Recurrent Rectal Cancer. J Gastrointest Surg 18, 1319–1326 (2014). https://doi.org/10.1007/s11605-014-2537-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2537-x