Abstract
Background
Posthepatectomy liver failure (PHLF) is a major complication after hepatectomy. As there was no standardized definition, the International Study Group of Liver Surgery (ISGLS) defined PHLF as increased international normalized ratio and hyperbilirubinemia on or after postoperative day 5 in 2010. We evaluated the impact of the ISGLS definition of PHLF on hepatocellular carcinoma (HCC) patients.
Methods
We retrospectively analyzed 210 consecutive HCC patients who underwent curative hepatectomy at our facility from 2005 to 2010. The median follow-up period after hepatectomy was 35.2 months.
Results
Thirty-nine (18.6 %) patients fulfilled the ISGLS definition of PHLF. Overall survival (OS) rates at 1, 3, and 5 years in patients with/without PHLF were 69.1/93.5, 45.1/72.5, and 45.1/57.8 %, respectively (P = 0.002). Recurrence-free survival (RFS) rates at 1, 3, and 5 years in patients with/without PHLF were 40.9/65.9, 15.7/38.3, and 15.7/20.3 %, respectively (P = 0.003). Multivariate analysis revealed that PHLF was significantly associated with both OS (P = 0.047) and RFS (P = 0.019). Extent of resection (P < 0.001), intraoperative blood loss (P = 0.002), and fibrosis stage (P = 0.040) were identified as independent risk factors for developing PHLF.
Conclusion
The ISGLS definition of PHLF was associated with OS and RFS in HCC patients, and long-term survival will be improved by reducing the incidence of PHLF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the third most common cause of cancer-related deaths in the world.1 Hepatectomy, which can lead to long-term survival in patients with HCC, is widely accepted as the best treatment option for advanced HCC.2, 3 Although surgical techniques and perioperative management have greatly improved mortality rates after hepatectomy in recent years,4, 5 morbidity rates still remain high.6–12
Among several complications that can occur after surgery, posthepatectomy liver failure (PHLF) is one of the most common causes of hepatectomy-related mortality. The incidence of PHLF has been reported to vary from 4 to 19 %; this wide range can be attributed to differences in patient populations and the procedures performed6–8, 10–12 as well as the lack of a universally accepted definition. Some studies have demonstrated that postoperative complications affect long-term survival after hepatectomy in patients with HCC,7, 9–11 but as the definitions for postoperative complications differ, there are no widely accepted risk factors or methodologies to control these events. To standardize the definition of PHLF, the International Study Group of Liver Surgery (ISGLS) proposed a definition for PHLF based on increased international normalized ratio (INR) and hyperbilirubinemia on or after postoperative day 5, together with a grading system of severity considering the impact on patients' clinical management in 2010.13 This definition was subsequently confirmed in 2011.14 In the validation study, all patients who underwent liver resection were included in an analysis and accordingly the patients had several different liver diseases. However, as liver status is influenced by underlying disease, which may affect the incidence of PHLF itself, we considered it relevant to investigate PHLF according to underlying disease.
In the present study, we focused on patients with HCC and assessed the ISGLS definition of PHLF and the impact of PHLF on long-term prognosis and identified risk factors in this patient population.
Methods
Patients and Preoperative Factors
From January 2005 to December 2010, 279 consecutive patients with HCC who underwent an initial hepatectomy at Kobe University Hospital were included in this study. Sixty-nine patients were excluded from the study (patients with reductive hepatectomy, 15, 16 n = 43; patients with a macroscopically positive resection margin, n = 17; patients with distant metastasis, n = 9). The remaining 210 patients with complete gross resection were retrospectively analyzed.
Demographic data were collected prior to surgery and included age, gender, performance status according to the Eastern Cooperative Oncology Group (ECOG),17 body mass index (BMI), alcohol consumption, and presence of diabetes mellitus. For the evaluation of preoperative liver function, all patients had several blood tests before hepatectomy, including hepatitis B surface antigen (HBs-Ag), hepatitis C virus antibody (HCV-Ab), complete blood count, total bilirubin (normal range, 0.3–1.0 mg/dl), albumin (normal range, 4.1–5.0 g/dl), prothrombin time (normal range, 79–130 %), and retention rate of indocyanine green at 15 min (ICGR15; normal range, ≤10 %). For the evaluation of HCC and fibrosis, abdominal ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI) were applied. Preoperative upper gastrointestinal endoscopy was performed routinely to assess esophageal varices. Portal hypertension was defined as the presence of esophageal varices and/or a platelet count of <10 × 104/ml in association with splenomegaly.18 Splenomegaly was defined as length of spleen of more than 10 cm as estimated by preoperative CT.19
Surgical Procedures
Selection criteria for hepatectomy included the extent of comorbidity, Child-Pugh status A or B, and remnant liver volume of more than 35 % of the whole liver. For further analysis, hepatectomy was categorized into two groups: major (n = 106) and minor (n = 104) resection. Major resections consisted of three extended right hepatectomies (1.4 %), 36 right hepatectomies (17.1 %), ten extended left hepatectomies (4.8 %), seven left hepatectomies (3.3 %), four central resections (1.9 %), and 46 sectionectomies (21.9 %). Minor resections consisted of 104 segmentectomies or less (49.5 %). For the analysis of the incidence of ISGLS definition of PHLF categorized by extent of hepatectomy and fibrosis stage, hepatectomy was additionally categorized into three groups: segments < 2 (including segmentectomy or less), 2 ≤ segments ≤ 3 (including left hepatectomy, central resection and sectionectomy), and segments > 3 (including extended right hepatectomy, right hepatectomy and extended left hepatectomy). Blood transfusions were defined as transfusions of concentrated red blood cells, fresh-frozen plasma, or platelets but excluded albumin.
Pathologic Evaluation
For all patients, a final diagnosis of HCC was pathologically confirmed after hepatectomy using surgically removed liver tissue. Tumor stage was assessed using the seventh edition of the International Union Against Cancer (UICC) classification.20 The degree of hepatic fibrosis was assessed by a single pathologist using the METAVIR scoring system: F0, absent; F1, portal fibrosis without septa; F2, portal fibrosis with rare septa; F3, numerous septa; and F4, cirrhosis.21 In four patients, hepatic fibrosis stage was not available because of the limited size of the resected livers.
Postoperative Morbidity and Mortality
Overall morbidity was defined as postoperative complications which occurred during hospital stay after hepatectomy. PHLF was diagnosed based on the ISGLS definition.13 In brief, the ISGLS definition of PHLF is increased INR and hyperbilirubinemia on or after postoperative day 5. PHLF is further categorized into three grades of severity: grade A, PHLF resulting in abnormal laboratory parameters but requiring no change in the clinical management of the patient; grade B, PHLF resulting in a deviation from the regular clinical management but manageable without invasive treatment; and grade C, PHLF resulting in a deviation from regular clinical management and requiring invasive treatment. Data on serum bilirubin levels and INR on or after postoperative day 5 were available for a total of 210 patients as blood tests were routinely performed on postoperative days 1, 3, 5, and 7 at least and thereafter based on patient condition. Therefore, the ISGLS definition was applied in 100 % of our patients. Other postoperative complications, excluding ISGLS definition of PHLF, were defined as events which deviated from the normal postoperative course and which required pharmacological, surgical, endoscopic, or radiological interventions. The surgical complication of coagulopathy (INR > 1.5) was treated by the administration of FFP or vitamin K, while encephalopathy was treated with enteral lactulose and branched-chain amino acids. Diuretics and albumin were used to treat massive ascites. Infectious complications were treated with antibiotics on the basis of the culture and sensitivity test results. Overall morbidities were additionally classified according to the Clavien–Dindo classification.22 Mortality was defined as death during hospital stay after hepatectomy.
Follow-up
After discharge, all patients were followed at the outpatient clinic with laboratory tests and CT or MRI performed every 3 to 6 months for the first 5 years and thereafter at least once every 12 months until death. Recurrence of HCC was defined as the appearance of a new lesion with the radiologic features of HCC. Overall survival (OS) was defined as the interval between hepatectomy and death or the last follow-up. Recurrence-free survival (RFS) was defined as the interval from the date of resection until detection of tumor recurrence, death, or last follow-up. For patients who survived during our analysis, the date of last follow-up was set as January 31, 2012. Two patients (1.0 %) were lost to follow-up.
Statistical Analysis
Continuous data were expressed as the median and range. Differences between patients’ characteristics were compared by χ 2 or Fischer’s exact tests. PHLF grades were compared using χ 2 and Kruskal–Wallis tests. OS and RFS were estimated by Kaplan–Meier method, and differences in the survival curves were analyzed by log-rank test. Univariate and multivariate Cox proportional hazard regression models were performed to identify independent prognostic factors. Multivariate logistic regression analysis was used to identify independent risk factors. In this study, all factors analyzed in the univariate analysis were included in the subsequent multivariate analysis. Statistical significance was considered when the two-sided P value was <0.05. All statistical analyses were performed using JMP version 9.0 (SAS Institute Inc, Cary, NC, USA) software.
Results
Patient Characteristics and Operative Results
The characteristics of all patients are shown in Table 1. The patient population consisted of 175 men and 35 women, with a median age of 69 years (range, 32–87 years). Postoperative complications are summarized in Table 2. A total of 119 complications were observed in 71 patients (33.8 %). The most common complication was ISGLS definition of PHLF which occurred in 39 patients (18.6 %), followed by pleural effusion in 16 patients (7.6 %) and wound infection in 12 patients (5.7 %). The median hospital stay was 16 days (range, 9–121 days).
Patient characteristics according to the presence or absence of ISGLS definition of PHLF are summarized in Table 3. Factors associated with PHLF were older age, male sex, advanced stage HCC, higher preoperative bilirubin levels, pre-existing portal hypertension, and major resection with greater blood loss and transfusion requirements (P < 0.05).
Perioperative Outcomes Categorized by PHLF Grade
Based on the ISGLS of PHLF, ten (4.8 %), 26 (12.4 %), and three (1.4 %) patients were classified as grade A, B, and C, respectively. We identified a mortality rate of 1.4 % (n = 3) in our study. All patients who died fulfilled the PHLF criteria (grade B, n = 1; grade C, n = 2). Table 4 shows clinical outcomes categorized by PHLF grade. Median hospital stay was 15 days for patients without PHLF, which was significantly shorter than in those with PHLF (grade A, 17 days; grade B, 23 days; grade C, 55 days; P < 0.001). Although ISGLS definition of PHLF was the most common complication, we also documented an additional 80 complications other than PHLF, the association with PHLF of which was also analyzed (Table 4). The incidence of these complications increased with PHLF grade (P < 0.001).
Long-Term Prognosis for Patients with PHLF
The median follow-up period after hepatectomy was 35.2 months (range, 1.7–80.7 months). Figure 1a shows OS categorized by the presence or absence of ISGLS definition of PHLF. OS rates at 1, 3, and 5 years in patients without PHLF were 93.5, 72.5, and 57.8 %, while OS rates in patients with PHLF were 69.1, 45.1, and 45.1 %, respectively (P = 0.002). There were four patient deaths, and one patient was lost to follow-up within 90 days after hepatectomy. OS was estimated excluding these five patients: the 1-, 3-, and 5-year OS rates in patients without PHLF were equal to the values obtained including these patients, and they were 77.0, 50.2, and 50.2 % in those with PHLF (P = 0.043; Fig. 1b). RFS rates at 1, 3, and 5 years in patients without PHLF were 65.9, 38.3, and 20.3 %, while RFS rates in patients with PHLF were 40.9, 15.7, and 15.7 %, respectively (P = 0.003; Fig. 2).
As the association between ISGLS definition of PHLF and OS was newly identified, we performed univariate (Table 5) and multivariate (Table 6) Cox regression analyses to investigate other prognostic factors for OS. In the univariate analysis, UICC stage ≥ III, blood transfusions, PHLF, and complications other than PHLF were identified as significant prognostic factors for OS. In the multivariate analysis, however, age >65 years, UICC stage ≥ III, and PHLF were identified as independent prognostic factors. For RFS, univariate analysis revealed that UICC stage ≥ III, PHLF, and complications other than PHLF were significant prognostic factors (Table 5). Multivariate analysis revealed that UICC stage ≥ III and PHLF were independent prognostic factors for RFS (Table 6).
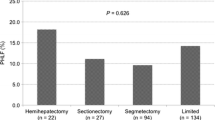
Risk Factors for Developing PHLF
As ISGLS definition of PHLF was identified as an independent prognostic factor for OS and RFS, we performed a multivariate logistic regression analysis to search for risk factors for developing PHLF. Among the prognostic factors tested, major hepatectomy, intraoperative blood loss >1,000 ml, and fibrosis stage ≥3 were identified as independent risk factors for developing PHLF (Table 7). As the extent of resection and fibrosis stage are factors which can be accessed before surgery, the incidence of PHLF categorized by these two factors was analyzed (Table 8). The incidence of PHLF increased in association with both the extent of resection and fibrosis stage.
Discussion
Posthepatectomy liver failure is a major prognostic factor for patients who have undergone hepatectomy. In 2010, the ISGLS defined PHLF as an increase in INR and concomitant hyperbilirubinemia on or after postoperative day 5.13 In this study, we assessed the definition limited solely with HCC patients and revealed that perioperative morbidity and mortality increased with higher grades of PHLF. OS and RFS associated with the incidence of PHLF, and the extent of resection, intraoperative blood loss, and fibrosis stage were identified as independent risk factors for developing PHLF.
Using the ISGLS definition of PHLF, the first validation study was performed in 2011 with all the patients who underwent liver resection for several different liver diseases by the group who identified the definition.14 Eleven percent of patients was reported to fulfill the ISGLS definition, and the mortality rate was 4.3 %. By contrast, the definition was met by 19 % of our study population, and the mortality rate was only 1.4 %. We speculate that these differences may have arisen from background differences in patient liver status. In the original validation study, patients mainly had metastatic disease, and accordingly 71 % of patients did not have hepatic fibrosis. In contrast, all of our patients had HCC, and accordingly half of them had a fibrosis stage of 3 or 4. This preoperative difference in hepatic fibrotic status also led to differences in the procedures performed: 80 % of their patients underwent major resection (resection of two or more anatomical segments), while 50 % of our patients underwent minor resection (resection of fewer than two segments). Despite the higher incidence and lower mortality, the ISGLS definition of PHLF successfully associated with perioperative morbidity and mortality with HCC patients, thus proving the feasibility to use the definition with HCC patients.
As our findings validated the use of the ISGLS definition of PHLF in patients with HCC, we next analyzed the impact of this definition on long-term survival and clearly proved statistical associations with OS (Fig. 1a) and RFS (Fig. 2). To elucidate the impact of PHLF on long-term survival, OS excluding the patients who died or were lost to follow-up within 90 days was also estimated. A statistical difference by the presence or absence of PHLF was observed, suggesting that PHLF affects long-term survival even after the patients have recovered from liver failure (Fig. 1b). Multivariate Cox regression analysis indicated that age, UICC stage, and PHLF were independent prognostic factors for OS, and UICC stage and PHLF were independent prognostic factors for RFS (Table 6). Moreover, it is interesting to note that the occurrence of postoperative complications, excluding ISGLS definition of PHLF, was not identified as an independent predictor for poorer OS or RFS. Previous reports show that complications affect long-term survival after hepatectomy in HCC patients.7, 9–11 Since our results show that ISGLS definition of PHLF affects long-term survival whereas complications other than PHLF do not, it should be emphasized that ISGLS definition of PHLF is a stronger predictor of prognosis than any other types of complication.
In this study, ISGLS definition of PHLF affected both OS and RFS. We speculate that PHLF-affected patients had less functional liver reserve, which limited additional treatments when recurrence was detected. However, there is no clear reason for the observed correlation between PHLF and poorer RFS. One possible explanation might be up-regulation of cytokines after liver injury.23 Among these cytokines, hepatocyte growth factor (HGF), which is a key component for liver regeneration,24 is implicated in the development and progression of HCC25 and is associated with a poorer prognosis after hepatectomy.26 Since we did not measure HGF serum levels in our study, the validity of this suggestion would be proved as future study.
As an association between ISGLS definition of PHLF and long-term prognosis was demonstrated, we finally investigated risk factors for the development of PHLF. Multivariate logistic regression analysis indicated that the extent of hepatectomy, intraoperative blood loss, and fibrosis stage were independent risk factors for developing PHLF (Table 7). The result additionally verified the feasibility of PHLF as previous studies have already demonstrated the direct relation between PHLF and extent of surgery, blood loss, and degree of fibrosis.27 One criticism to the definition of PHLF might be that as PHLF is a postoperative event which can be identified 5 days after hepatectomy, the clinical value as a prognostic factor is comparatively low. However, by identifying the risk factors, HCC patients for hepatectomy can now be stratified based on the extent of resection and background fibrosis stage, which can be accessed before surgery (Table 8). For patients with fibrosis stage 0–2, hepatectomy can be performed with a lower risk of developing ISGLS definition of PHLF. However for patients with fibrosis stage 3 or 4, it is likely that more than 50 % of patients will develop PHLF after right hepatectomy, which is associated with poorer OS and RFS. Accordingly, the extent of hepatectomy should be decided only after a careful discussion with the patient about benefits and risk. As fibrosis stage was assessed from the resected liver in the study, prospective analysis of methods to assess fibrosis stage before surgery is in progress.
One limitation of this study is its single-center retrospective design. The other limitation is that almost half of the patients underwent minor resection. This patient population might lower the incidence of PHLF, which eventually decreases the statistical power. Our data must be confirmed with a larger population in the future.
In conclusion, we have demonstrated for the first time the validity of the ISGLS definition of PHLF, its association with OS and RFS, and the risk factors for developing PHLF in patients with HCC. Long-term survival in HCC patients will be improved by reducing the incidence of PHLF, which can be achieved by selecting patients for hepatectomy based on the extent of resection required and fibrosis stage.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011; 61: 69–90.
de Lope CR, Tremosini S, Forner A, Reig M, Bruix J. Management of HCC. J Hepatol 2012; 56: S75-87.
Ishizawa T, Hasegawa K, Aoki T, Takahashi M, Inoue Y, Sano K, et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 2008; 134: 1908–1916.
Poon RT, Fan ST, Lo CM, Ng IO, Liu CL, Lam CM, et al. Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 2001; 234: 63–70.
Taketomi A, Kitagawa D, Itoh S, Harimoto N, Yamashita Y, Gion T, et al. Trends in morbidity and mortality after hepatic resection for hepatocellular carcinoma: an institute’s experience with 625 patients. J Am Coll Surg 2007; 204: 580–587.
Capussotti L, Muratore A, Amisano M, Polastri R, Bouzari H, Massucco P. Liver resection for hepatocellular carcinoma on cirrhosis: analysis of mortality, morbidity and survival—a European single center experience. Eur J Surg Oncol 2005; 31: 986–993.
Chok KS, Ng KK, Poon RT, Lo CM, Fan ST. Impact of postoperative complications on long-term outcome of curative resection for hepatocellular carcinoma. Br J Surg 2009; 96: 81–87.
Kawano Y, Sasaki A, Kai S, Endo Y, Iwaki K, Uchida H, et al. Short- and long-term outcomes after hepatic resection for hepatocellular carcinoma with concomitant esophageal varices in patients with cirrhosis. Ann Surg Oncol 2008; 15: 1670–1676.
Kusano T, Sasaki A, Kai S, Endo Y, Iwaki K, Shibata K, et al. Predictors and prognostic significance of operative complications in patients with hepatocellular carcinoma who underwent hepatic resection. Eur J Surg Oncol 2009; 35: 1179–1185.
Mizuguchi T, Nagayama M, Meguro M, Shibata T, Kaji S, Nobuoka T, et al. Prognostic impact of surgical complications and preoperative serum hepatocyte growth factor in hepatocellular carcinoma patients after initial hepatectomy. J Gastrointest Surg 2009; 13: 325–333.
Okamura Y, Takeda S, Fujii T, Sugimoto H, Nomoto S, Nakao A. Prognostic significance of postoperative complications after hepatectomy for hepatocellular carcinoma. J Surg Oncol 2011; 104: 814–821.
Yang T, Zhang J, Lu JH, Yang GS, Wu MC, Yu WF. Risk factors influencing postoperative outcomes of major hepatic resection of hepatocellular carcinoma for patients with underlying liver diseases. World J Surg 2011; 35: 2073–2082.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 2011; 149: 713–724.
Reissfelder C, Rahbari NN, Koch M, Kofler B, Sutedja N, Elbers H, et al. Postoperative course and clinical significance of biochemical blood tests following hepatic resection. Br J Surg 2011; 98: 836–844.
Ku Y, Iwasaki T, Tominaga M, Fukumoto T, Takahashi T, Kido M, et al. Reductive surgery plus percutaneous isolated hepatic perfusion for multiple advanced hepatocellular carcinoma. Ann Surg 2004; 239: 53–60.
Ku Y. Isolated hepatic perfusion for extensive liver cancers. In: Blumgart LH, ed. Surgery of the liver, biliary tract, and pancreas, 4th ed. Philadelphia: Saunders, 2007; pp 1312–20.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982; 5: 649–655.
Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology 2005; 42: 1208–1236.
Bezerra AS, D'Ippolito G, Faintuch S, Szejnfeld J, Ahmed M. Determination of splenomegaly by CT: is there a place for a single measurement? AJR Am J Roentgenol 2005; 184: 1510–1513.
Sobin LH, Gospodarowicz MK, Wittekind C, eds. Internatinal Union Against Cancer (UICC): TNM classification of malignant tumours, 7th ed. New York: Wiley-Blackwell, 2010.
Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology 1996; 24: 289–293.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213.
Tilg H, Kaser A, Moschen AR. How to modulate inflammatory cytokines in liver diseases. Liver Int 2006; 26: 1029–1039.
Michalopoulos GK, DeFrances MC. Liver regeneration. Science 1997; 276: 60–66.
Whittaker S, Marais R, Zhu AX. The role of signaling pathways in the development and treatment of hepatocellular carcinoma. Oncogene 2010; 29: 4989–5005.
Chau GY, Lui WY, Chi CW, Chau YP, Li AF, Kao HL, et al. Significance of serum hepatocyte growth factor levels in patients with hepatocellular carcinoma undergoing hepatic resection. Eur J Surg Oncol 2008; 34: 333–338.
Schreckenbach T, Liese J, Bechstein WO, Moench C. Posthepatectomy liver failure. Dig Surg 2012; 29: 79–85.
Disclosures
All authors listed on this manuscript have no financial disclosure.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fukushima, K., Fukumoto, T., Kuramitsu, K. et al. Assessment of ISGLS Definition of Posthepatectomy Liver Failure and Its Effect on Outcome in Patients with Hepatocellular Carcinoma. J Gastrointest Surg 18, 729–736 (2014). https://doi.org/10.1007/s11605-013-2423-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2423-y