Abstract
Background
Many Crohn's disease patients require surgery. Intraoperative detection of new lesions may lead to change in planned surgery. This study aimed to determine whether magnetic resonance enterography can optimize surgical planning and guide decision making in Crohn's disease.
Methods
Seventy-five patients with complicated Crohn's disease were enrolled and underwent preoperative magnetic resonance enterography. Analysis included imaging accuracy and change in surgical strategy due to discordance with imaging findings.
Results
Surgery was performed laparoscopically in 39/75 patients (52 %), with conversion to open surgery required in six (15 %). Concordance between observers was excellent (kappa value >0.8). Magnetic resonance enterography accuracy for stenosis, abscess, and fistula were all above 85 % in per-patient analysis. In 68/75 cases (90.7 %) surgery was correctly predicted. Conversely, in 7/75 cases (three false-positives and four false-negatives) surgical strategy (type of resection or strictureplasty, n = 5) and/or surgical approach (conversion from laparoscopy to open surgery, n = 2) changed due to discordance with magnetic resonance enterography findings.
Conclusion
Surgical strategy and approach are correctly predicted by magnetic resonance enterography in the majority of patients with complicated Crohn's disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Crohn's disease (CD) is a chronic inflammatory disease that can affect almost any part of the gastrointestinal tract.1 Most patients with CD will eventually develop stricturing or perforating complications and, despite advances in therapy in recent years, the majority of patients with CD will still require surgery at some point.1 – 3
Laparoscopy in CD allows benefits such as reduced pain, lower risk of incisional hernia and adhesions, and cosmetic advantages, compared with laparotomy.4 , 5 However, the laparoscopic approach may result in an incomplete evaluation of the entire bowel (both small and large) and concerns have been raised that lesions not detected preoperatively may be missed, particularly those located in occult segments or proximal small bowel lesions, due to limited tactile ability, technical difficulty resulting from mesenteric inflammation, and the presence of fistulas and/or abscesses.6 – 8
Therefore, in order to obtain an accurate disease assessment, identifying any lesions or complications such as fistulas and stenosis that might potentially be undetectable during a laparoscopic procedure, it is crucial to use an accurate and reliable preoperative imaging technique when planning the surgical strategy for the treatment of CD.9 – 11
Over- and understaging are both associated with suboptimal surgical planning: overstaging may lead to a primary open approach in cases in which laparoscopy may be suitable, while understaging may lead to unnecessary and potentially harmful laparoscopic approach in cases in which such an approach is inappropriate.
Currently available evidence suggests that magnetic resonance enterography (MRE) is useful for assessing and monitoring disease activity, for guiding decision making in terms of medical or surgical therapies and, subsequently, in patients who are candidates for surgery, to appropriately plan the operation.12 – 14
MRE has a number of advantages as a technique for preoperative imaging, including high resolution, high sensitivity, specificity, and accuracy for the diagnosis of CD, for the evaluation of the extent of disease, and of CD complications. Moreover, the absence of ionizing radiation allows repeat procedures and frequent follow-up, which is particularly important because patients are generally young and disease recurrence and re-operations are common.15 For these reasons, MRE is now the imaging modality of choice for the complete evaluation of CD, while CT enterography remains a valid alternative if MR is not available.
The aim of this study was to assess the sensibility, specificity, accuracy, positive predictive value, and negative predictive value of MRE for detecting CD complications deserving surgery (stenoses, fistulas, abscesses), in order to optimize preoperative surgical planning for CD. We also aimed to determine the utility of preoperative staging with MRE in order to minimize intraoperative detection of new findings and modification of the approach (laparoscopic versus open) in a tertiary care surgical experienced in both IBD surgery and laparoscopic techniques.
Patients and Methods
Study Design
In this prospective study, 75 consecutive patients with complicated CD who were candidates to surgery were enrolled at our institution between September 2011 and August 2012. All patients in our study group were addressed to surgery for symptomatic disease in spite of optimized medical therapy.
MRE was performed in all patients in accordance with a standardized protocol within 30 days before surgery. Analysis included MRE diagnostic accuracy (per segment and per patient) for complicated disease (defined as the presence of strictures, fistulas and/or abscesses) and whether or not any change in the planned surgical strategy was required due to discordance with MRE findings.
Exclusion criteria were as follows: absence of histologically confirmed CD; age <18 years; emergency surgery; contraindications to MRI such as the presence of a pace-maker, metal clip, or Swan–Ganz catheter. All patients provided written informed consent for undergoing the MRE procedure, the surgical procedure, and for participation in the study.
MRE images were blindly and independently assessed by two experienced radiologists and radiological findings were correlated with intraoperatively detected lesions and prospectively collected in a Microsoft Excel® database.
MRE Technique and Interpretation of Radiological Findings
All patients underwent 1.5 T (Siemens Symphony, Erlangen, Germany) and 3 T (Siemens Verio, Erlangen, Germany) imaging. During the hour prior to undergoing the imaging procedures, all patients received oral PEG 1,500 mL, intravenous glucagon or hyoscine butylbromide (1/2 vial, to reduce intestinal movements), followed by T2 imaging acquisition. Due to the short half life of intravenous glucagon and hyoscine butylbromide, patients received a repeat dose of these agents to ensure satisfactory reduction in intestinal movements throughout the procedure, followed by intravenous gadolinium administration with T1 fat-saturated imaging acquisition. The total length of the examination was about 30 min.
Two experienced radiologists blindly and independently assessed MRE images using a dedicated form, following the indication of the current literature for the definition of CD complications.15 , 16
Surgical Technique
All operations were performed by the same surgical team experienced in both IBD surgery and laparoscopic surgery. Laparoscopic approach was indicated in the absence of active abdominal sepsis or repeated major surgical operations, especially in cases with history of septic postoperative complications.
For laparoscopic surgery, a classical multiport approach or a single-port approach (periumbilical 3-cm incision) was used. After each operation, the surgeon completed a form recording the following parameters (according to the findings reported by the radiologists): disease location and extent, stenosis, abscess, and fistula presence. It was then reported any change in the planned surgical strategy due to discordance with MRE findings.
A laparoscopic operation was considered as converted whenever an enlargement of the mini-laparotomy beyond 4 cm was required.
Statistical Analysis
Statistical analysis was performed using MedCalc®, MedCalc Statistical Software, Ostend, Belgium. Analysis included calculation of sensitivity, specificity, accuracy, positive predictive value, and negative predictive value and MRE accuracy (per segment and per patient). These values were calculated with a confidence interval (CI) of 95 % using the McNemar test. The correlation between the two radiologist's interpretations was analyzed using Cohen's coefficient kappa:
-
K <0.20 = poor concordance
-
Κ between 0:21 and 00:40 = modest concordance
-
Κ between 0.41 and 0.60 = moderate concordance
-
Κ between 0.61 and 0.80 = good concordance
-
Κ >0.80 = excellent concordance.
Results
Patients
A total of 75 consecutive patients (33 females) underwent preoperative MRE (1.5 T in 29 patients and 3 T in 46 patients) during the 4 weeks before surgery. Median patient age was 44 years (range 21–75). The majority of patients had disease localized to the terminal ileum (n = 53). Intestinal obstruction was the most common surgical indication (n = 48), followed by fistula or abscess (n = 22). The most frequent type of surgery was ileocolic resection (n = 54). Of the 75 patients, 39 (52 %) underwent laparoscopic surgery, of whom conversion to open surgery was required in 6 (15 %) (see Table 1).
MRE Findings
Overall, MRE findings had an accuracy of at least 88 % for both observers 1 and 2 for all bowel segments and for all findings, with an excellent rate of concordance between observers (kappa value > 0.8).
Sensitivity and Specificity of MRE
In 68 of 75 patients (90.7 %) both the approach and the strategy were correctly predicted by MRE. Conversely, in the remaining seven cases (9.3 %) the surgical strategy and/or approach were changed due to discordance with MRE findings. MRE predicted two cases of enterocolic fistulas and one of an anastomotic stricture that were not subsequently found surgically, with three cases of enteric fistulas (involving the colon, duodenum, and bladder) and one abdominal abscess detected surgically that were not predicted by MRE. As a result of such discordance between MRE prediction and surgical findings, the surgical strategy was altered in seven cases (three false positives and four false negatives), with the surgical approach (conversion from laparoscopy to open surgery) altered in two cases (see Table 2). Other causes for conversions to open surgery were not related to intraoperatively detected bowel lesions but to massive adhesions due to previous operations (n = 2) or to very thickened mesenteries responsible for large inflammatory masses which needed a enlargement of the planned mini-laparotomy (n = 2).
Per Patient Analysis
The sensitivity for stenoses was very high at 96 % for both observers 1 and 2, although specificity was lower at 67 % for both observers. Sensitivity and specificity of MRE for abscess were 40 and 99 %, respectively, for both observers, with corresponding values for fistulas of 67 and 94 %, respectively, for observer 1, and 71 and 96 %, respectively for observer 2. Interobserver concordance was high for all findings (further details are provided in Table 3).
Per-Segment Analysis
A per-segment analysis was performed by dividing the gastrointestinal tract into different segments (small bowel, ascending colon, transverse colon, descending and sigmoid colon, rectum). MRE was extremely sensitive and accurate for the detection of complicated disease (ranging from 0.83 to 1.00), and specificity values were also very high. Specificity of small bowel complications was 0.40 (Table 4; Supplementary Tables a–c).
Discussion
This is the first prospective study focused on the role of MRE in the planning of surgical strategy in Crohn's disease patients already addressed to surgery. In this study, we have shown that preoperative MRE correctly predicts surgical strategy in the majority of patients undergoing surgery for complicated CD. This is important because surgery is still required for many patients with CD, and intraoperative detection of new lesions is common and may lead to a change in the planned approach or strategy. MRE is especially valuable before laparoscopic surgery, since unrecognized lesions may lead to conversion to open surgery. Minimally invasive surgery and strictureplasty may reduce the negative impact of surgery in patients with CD, limiting scars and bowel loss.17 Moreover, body image and cosmesis following surgery for CD are better preserved with laparoscopic surgery than with open surgery.17 – 19
MRE was able to identify correctly CD-related complications in 56 of 73 subjects with positive findings at surgery (76.7 %). In 14 subjects (19.1 %), MRE was able to detect at least some, but not all, complications present (i.e. stricture but not fistula in a stricturing penetrating disease). Anyway, the overall accuracy in terms of detecting complicated disease was 0.93 (95 % CI 0.84–0.98).
Discrimination and relative contribution of inflammation and fibrosis of a CD stricture does impact on indication to medical versus surgical treatment, but, since all our patients were addressed to surgery after optimal medical therapy, this was not relevant for the present study. We therefore considered only the presence of strictures, fistulas, and abscesses.
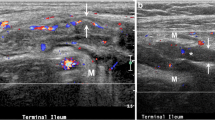
In our study, MRE accurately predicted surgical findings in the majority of patients, with high sensitivity for the detection of strictures (Figs. 1 and 2) and high specificity for the detection of fistulas (Figs. 3 and 4). In a previous study investigating the utility of MRE in planning surgical procedures in CD, the sensitivity and specificity of MRE for bowel stenosis were 95 and 72 %, respectively, with corresponding values for fistulae of 71 and 76 %, respectively, and for intra-abdominal abscesses of 92 and 90 %, respectively.12 In the current study, while sensitivity and specificity findings were similar to these previous findings for bowel stenosis, we found similar sensitivity for fistulae, at 68 % but specificity was higher at 96 %. For prediction of abscesses, our study demonstrated low sensitivity at only 40 %, although there was high specificity at 98 %. Of our three false negative subjects, one had an enteric fistula, which may have resulted in an abscess developing prior to surgery but after the patient had undergone MRE (Fig. 5). We cannot definitively exclude the possibility that all the other abscesses not seen on MRE developed between the time of MRE and the surgical procedure.
On the per-segment analysis, MRE had 50 % sensitivity for rectal localization. This finding of poor sensitivity in rectal localization on per-segment analysis is consistent with our previous results on MRE of the rectum20 where MRE was shown to be less sensitive than CT in detecting rectal disease. Furthermore, while MRE sensitivity, negative predictive value and accuracy for small bowel complications were excellent (100, 100, and 93 %, respectively), specificity was low (40 %, Table 4): multidisciplinary analyzing these data, we concluded that the radiologists interpreted in some cases the appearance of normal peristaltic movements as further short CD localizations. On the contrary, a negative finding of MRE for small bowel complications was highly reliable for the surgeon (100 %).
In 9.3 % of cases MRE provided erroneous information, such that surgical findings were unexpected and resulted in changes in the planned surgical strategy. In two cases, MRE provided false positive results for the presence of entero-sigmoid fistula, with one false-positive stenosis (preanastomotic stricture without dilation of the ileum above in a patient with persistent occlusive symptoms). Regarding the cases of entero-sigmoid fistula in two patients conventionally operated (2/36, 5.5 %) MRE resulted falsely positive for ileo-sigmoidal fistulization together with a surrounding inflammatory mass, which, at the moment of surgery already shrinked, so that, at surgery, a laparoscopic approach appeared to have been feasible. Additionally, even if we routinely performed colonoscopy to all CD patient candidates to surgery, in our clinical practice, we do not completely rely on endoscopic findings to exclude the presence of small ileo-sigmoid fistulas.
Additionally, there were four lesions that were not detected on MRE imaging: three fistulae and one abscess.
All of these necessitated changes in the planned surgical approach. In the two cases of false-positive results of fistula, planned entero-sigmoid fistula surgery was modified to ileocolic resection, with the one false-positive of stenosis resulting in a change in planned surgery from resection and stricturoplasty to simply adhesiolysis. In these cases, the impact on the patient of these incorrect results was minimal, with the actual surgical procedures performed being less complicated than expected. In those cases, the decision to proceed to an open approach was related to multiple prior operations for septic complications; however, such false-positive findings may potentially have resulted in a decision to use an open surgical approach rather than the less-invasive laparoscopic approach. For those patients in whom MRE provided false negative results, reliance on MRE results alone for surgical planning (without completing an intraoperative bowel exploration) may lead to miss relevant complications and to repeat surgery in the future.
It can be speculated whether a routine laparoscopic exploration may be considered even in patients with MRE findings apparently contraindicating a minimally invasive approach. This strategy is, in our opinion, reasonable, since patients could profit a lot also from hybrid procedures, in which part of the operation is performed laparoscopically. According to the different definitions of conversion, this hybrid approach could increase conversion rates. This does not absolutely represent a failure of the operation, but has to be considered as an advantage for the patient since it is a less-invasive alternative to straight-open surgery.
Finally, to the best of our knowledge, this is the largest study conducted to date assessing the accuracy of MRE in complicated Crohn's disease, using surgery as a reference. There is currently no standard diagnostic procedure that can be considered to be a reference standard for the detection of disease complications in surgical CD patients. However, our results suggest that using MRE prior to surgery may be used as such a standard to diagnose disease complications in CD and to plan the appropriate surgical strategy and approach in subjects with complicated CD. Preoperative MRE allows for optimized surgical planning, with the correct surgical approach chosen in the vast majority of cases. The additional costs of routinely performing MRE have to be balanced with its potential benefits; nevertheless, this cost analysis was not performed in the present study.
In conclusion, preoperative imaging using MRE is a useful technique to correctly predict surgical strategy and approach in the majority of patients with complicated CD.
References
Podolsky, D. K. (2002). "Inflammatory bowel disease." The New England journal of medicine 347(6): 417–429.
Cosnes, J., S. Cattan, et al. (2002). "Long-term evolution of disease behavior of Crohn's disease." Inflammatory bowel diseases 8(4): 244–250.
Etienney, I., Y. Bouhnik, et al. (2004). "Crohn's disease over 20 years after diagnosis in a referral population." Gastroenterologie clinique et biologique 28(12): 1233–1239.
Alabaz, O., A. J. Iroatulam, et al. (2000). "Comparison of laparoscopically assisted and conventional ileocolic resection for Crohn's disease." The European journal of surgery = Acta chirurgica 166(3): 213–217.
Benoist, S., Y. Panis, et al. (2003). "Laparoscopic ileocecal resection in Crohn's disease: a case-matched comparison with open resection." Surgical endoscopy 17(5): 814–818.
Bernell, O., A. Lapidus, et al. (2000). "Risk factors for surgery and postoperative recurrence in Crohn's disease." Annals of surgery 231(1): 38–45.
Otterson, M. F., S. J. Lundeen, et al. (2004). "Radiographic underestimation of small bowel stricturing Crohn's disease: a comparison with surgical findings." Surgery 136(4): 854–860.
Uchikoshi, F., T. Ito, et al. (2004). "Advantages of laparoscope-assisted surgery for recurrent Crohn's disease." Surgical endoscopy 18(11): 1675–1679.
Nolan, D. J. (1997). "The true yield of the small-intestinal barium study." Endoscopy 29(6): 447–453.
Maconi, G., G. M. Sampietro, et al. (2003). "Contrast radiology, computed tomography and ultrasonography in detecting internal fistulas and intra-abdominal abscesses in Crohn's disease: a prospective comparative study." The American journal of gastroenterology 98(7): 1545–1555.
Parsi, M. A., B. A. Lashner, et al. (2004). "Type of fistula determines response to infliximab in patients with fistulous Crohn's disease." The American journal of gastroenterology 99(3): 445–449.
Pozza, A., M. Scarpa, et al. (2011). "Magnetic resonance enterography for Crohn's disease: what the surgeon can take home." Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 15(10): 1689–1698.
Malgras, B., P. Soyer, et al. (2012). "Accuracy of imaging for predicting operative approach in Crohn's disease." The British journal of surgery 99(7): 1011–1020.
Fiorino, G., L. Peyrin-Biroulet, et al. (2013). MRE and colonoscopy findings in early Crohn's disease predict the course of the disease: a prospective observational cohort study. 8th Congress of ECCO the European Crohn's and Colitis Organisation. Vienna, Austria.
Gourtsoyiannis, N. C., J. Grammatikakis, et al. (2006). "Imaging of small intestinal Crohn's disease: comparison between MR enteroclysis and conventional enteroclysis." European radiology 16(9): 1915–1925.
Florie, J., M. N. Wasser, et al. (2006). "Dynamic contrast-enhanced MRI of the bowel wall for assessment of disease activity in Crohn's disease." AJR. American journal of roentgenology 186(5): 1384–1392.
Scarpa, M., C. Ruffolo, et al. (2009). "Intestinal surgery for Crohn's disease: predictors of recovery, quality of life, and costs." Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 13(12): 2128–2135.
Dunker, M. S., A. M. Stiggelbout, et al. (1998). "Cosmesis and body image after laparoscopic-assisted and open ileocolic resection for Crohn's disease." Surgical endoscopy 12(11): 1334–1340.
Maartense, S., M. S. Dunker, et al. (2006). "Laparoscopic-assisted versus open ileocolic resection for Crohn's disease: a randomized trial." Annals of surgery 243(2): 143–149; discussion 150–143.
Fiorino G, Bonifacio C, Peyrin-Biroulet L, Minuti F, Repici A, Spinelli A, Fries W, Balzarini L, Montorsi M, Malesci A, Danese S. Prospective comparison of computed tomography enterography and magnetic resonance enterography for assessment of disease activity and complications in ileocolonic Crohn's disease. Inflamm Bowel Dis. 2011 May;17(5):1073–80. doi: 10.1002/ibd.21533. Epub 2010 Nov 8.
Acknowledgments
The authors would like to acknowledge Marie Cheeseman. This work was supported by Alcesti Scarpellini and FIRMAD (Fondazione Italiana per la Ricerca sulle Malattie dell’Apparato Digerente).
Conflict of Interest
The authors were involved in all the different phases of the study (including enrolment of patients), data analysis and writing of the manuscript. The authors did not receive honoraria for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Discussant
Dr. Guilherme M. R. Campos (Madison, WI): The paper is an important contribution as it evaluated one of the larger cohorts of patients with Crohn's, as to study accuracy of MR enterography and used a robust reference standard: surgical findings. One of the limitations of the study though, is related to the very use of surgical findings as the reference standard; as any study employing surgery as reference, will suffer from verification bias, as only highly abnormal tests resulting in reference application will be evaluated. Second is the need to better delineate the tests and algorithm used to choose open versus laparoscopic approach and also the criteria for conversion. In addition, the decision for conversion involves too many variables, and what maybe always an open procedure or a conversion in some hands, maybe a standard laparoscopic procedure in others. Lastly, the differentiation of active versus fibrotic Crohn's by MR, and validating MR findings with histological evaluation is not presented in the current analyses.
My questions are: Because MR had a few false positives, should a diagnostic lap be considered in selected patients to confirm the MR findings? And second, should MR completely replace CT enterography or are there clinical scenarios in which CT would be preferred? Thank you.
Closing Discussant
Dr. Antonino Spinelli: Thank you Dr. Campos for your comments and for your questions.
(1) Regarding the first point of the bias intrinsic in using surgery as a reference, that would be the case if our aim would have been to generally assess activity, and not complications as we actually wanted to do.
(2) I agree with you that the choice of the approach (lap or open) is very “operator dependent,” but in the present study, our aim was not to say what should be approached laparoscopically and what not, but to analyze whether MRE can help the single surgeon to correctly choose his approach for that single patient, given his own indication to lap or open surgery.
(3) Active inflammatory vs fibrotic disease remains a challenge for GE and surgeons dealing with CD and we actually have an ongoing study in which we assess inflammation and fibrosis on surgical specimen correlating them with exactly the same bowel segment at MRE.
Two brief answers at your last two questions:
(1) I do not think that a diagnostic lap (or a lap look) should be performed as a standard, because our aim is to correctly and directly address patients to the most appropriate surgical approach, but I agree that in selected cases, it can be done (e.g., in patients with doubtful MRE finding of e–e fistula).
(2) Regarding CT enterography and MRE, we published a couple of years ago prospective comparison, showing that they were able to obtain similar results and that therefore, due to the radiation exposition hazards, MRE should be preferred.
Rights and permissions
About this article
Cite this article
Spinelli, A., Fiorino, G., Bazzi, P. et al. Preoperative Magnetic Resonance Enterography in Predicting Findings and Optimizing Surgical Approach in Crohn's Disease. J Gastrointest Surg 18, 83–91 (2014). https://doi.org/10.1007/s11605-013-2404-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2404-1