Abstract
Background and Objective
Chronic localized pancreatic inflammation in the form of chronic pancreatitis is an established risk factor for human pancreatic ductal adenocarcinoma (PDAC) development. Constitutive activation of inflammation-related signal transducer and activator of transcription (Stat)3 signaling has been implicated in the development and progression a number of malignancies, including PDAC. Although, the Janus Kinase (Jak)/Stat pathway is a potential drug target, clinicopathological, molecular, and prognostic features of Stat3-activated PDAC remain uncertain. Our aim was to determine the clinicopathological impact of this inflammatory pathway in resectable PDAC.
Methods
Using a tissue microarray-based cohort of PDAC from 86 patients undergoing pancreaticoduodenectomy with curative intent and complete clinicopathological data available, we evaluated expression of the interleukin-6 receptor (IL-6R)/Jak/Stat pathway by immunohistochemistry. IL-6R, Jak, phospho (p)-Jak, Stat3, pStat3Tyr705, and pStat3Ser727 were assessed in PDAC and pancreatic intraepithelial neoplasia. A Cox regression multivariate analysis model was used to determine factors influencing survival. Activation of the IL-6R/Jak/Stat3 pathway was compared with the systemic inflammatory response as measured by serum C-reactive protein levels.
Results
High pJak was associated with reduced overall survival in multivariate analysis when compared with those with moderate or low expression (p = 0.036; hazard ratio (HR) = 1.68) as was pStat3Tyr705 (p < 0.001; HR = 2.66) independent of lymph node status and tumor grade. Patients with a combination of pJakhigh/pStat3Tyr705 high expression had an especially poor prognosis (median survival of 8.8 months; 95 % CI, 4.4–13.2). While the IL-6R/Jak/Stat pathway did not correlate with serum C-reactive protein levels, high pStat3 expression was associated with a reduction in the density of the local tumoral immune response.
Conclusion
Activation of the Jak/Stat3 pathway via phosphorylation was associated with adverse outcome following resection of PDAC with curative intent supporting potential roles for pJak and pStat3 as prognostic biomarkers markers and therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) remains one of the most aggressive of all malignancies, with overall 5-year survival in the order of 3 %. Patients with potentially resectable disease are the minority (10–15 %) because of locoregional extension or metastatic disease at presentation.1,2 Clinical trials have demonstrated that single agent and combination chemotherapeutics tested so far, have limited impact on the natural history of the disease.
Our own group and others have reported that the presence of an elevated systemic inflammatory, response as measured by serum C-reactive protein levels, is associated with poor outcome in both resectable3 and non-resectable4 pancreatic cancer. The main stimulus to hepatic production of C-reactive protein is interleukin 6 (IL-6); a pleotropic cytokine released in response to a variety of inflammatory stimuli. Elevated C-reactive protein is associated with increased systemic monocyte IL-6 production in patients with pancreatic cancer,5 and elevated IL-6 has been demonstrated in the serum of cachexic patients with pancreatic cancer as well as in the tumor microenvironment.
Chronic localized pancreatic inflammation in the form of chronic pancreatitis (CP) is an established risk factor for human PDAC development6 and via IL-6 has been demonstrated to accelerate pancreatic intra-epithelial neoplasia (PanIN) and PDAC development in Kras murine models.7 Additionally, low-grade systemic inflammation-associated co-morbidities including cigarette smoking and obesity are established contributors to pancreatic cancer risk.8 It appears therefore that chronic inflammation is associated with both an increased cancer risk and, in the case of pancreatic cancer, a worse cancer survival. It remains unclear whether systemic inflammation functions as a tumor promoter or rather it is a reaction to the presence of localized or disseminated PDAC.
The cellular effects of cytokines including IL-6 are in part mediated via activation of signal transducer and activator of transcription 3 (Stat3), phosphorylation of which occurs via the Janus-activated kinase (Jak) family of tyrosine kinases, themselves activated by cytokine receptors.9,10 Stat3 mediates a complex milieu of biological responses in proliferation, apoptosis and inflammation.10 It is constitutively activated in a variety of human cancers, with inflammation-associated tumorigenesis supported by Stat3 in the lung11 and colon.12 Stat3 signaling is a principal intrinsic pathway for cancer related inflammation in the tumor microenvironment, suspected to induce cancer-promoting inflammation and inhibit anti-tumor immunity.13,14
Stat3 is aberrantly activated in human PDAC, influences proliferation in PDAC cell lines 15 and is implicated in a Pdx1 murine model of acinar to ductal transition.16 Recent evidence suggests that Stat3 is critical for spontaneous and pancreatitis-accelerated PDAC precursor formation.17 Thus, accumulating evidence has implicated Jak and Stat3 as promising targets for cancer therapy and chemoprevention18,19 however better understanding of the mechanism and consequence of their activation in pancreatic cancer is required.
It is our hypothesis that the poor outcome observed in PDAC associated with an elevated systemic inflammatory response is related to persistent activation of the IL-6R/Jak/Stat signaling pathway. In this study, we have assessed expression and activation of the IL-6R/Jak/Stat components in a cohort of PDAC patients resected with curative intent. We aimed to identify whether upregulation of components of this cascade are associated with clinicopathological features including survival and to identify if upregulation of this pathway is associated with the presence of a systemic inflammatory response.
Methods
Patient Characteristics
All resectional surgery was performed in the West of Scotland Pancreatic Unit, Glasgow Royal Infirmary, UK, during a 10-year period (1st June 1995 to 31st July 2004). All patients underwent either classical or pylorus-preserving PD, performed by a team of three surgeons. Surgical death was defined as in-hospital mortality. This analysis was limited to patients undergoing PD for PDAC with curative intent. Other lesions (e.g., ampullary, duodenal or distal bile duct adenocarcinomas, or intrapapillary mucinous neoplasms) were excluded.
The decision to perform resection was made by a multi-disciplinary team including surgeons, oncologists, radiologists and pathologists. The criteria for resectability were: (a) CT evidence of localised tumor in the head of the pancreas; (b) no greater than 180° circumferential involvement of superior mesenteric vein; and (c) no overt arterial involvement.20
Postoperatively, all patients were considered for adjuvant therapy. In the earlier years of the study, patients were considered for the European Study of Pancreatic and Ampullary Cancer (ESPAC)-1 randomization; in the later years, they were considered for ESPAC-3 randomization. There was a range of five treatment options across both these studies, including 5-FU with folinic acid, gemcitabine, radiotherapy, 5-FU with radiotherapy and no therapy. Those patients reported as having received adjuvant chemotherapy achieved at least 50 % of intended dosage. None of the cohort received neoadjuvant therapy as it was not used within our institution during the study period.
Pathological microscopic assessment and reporting was performed as previously described.21 Resection margin positivity (R1) was defined according to the British Royal College of Pathologists (RCPath) guidelines as the presence of tumor ≤ 1 mm from a circumferential margin or surface of the pancreatic resection specimen, whether by direct invasion or by tumor within a lymph node when assessed by microscopy of a hematoxylin-and-eosin-stained slide.22 In addition to traditional histopathological features we have recently evaluated and categorized the degree of immune cell infiltrate in PDAC,23 with a dense immune cell infiltrate associated with a significantly prolonged survival following resection.
Tissue Microarray Construction
Following patient identification the relevant haematoxylin and eosin (H&E) slides were obtained from the pathology archive and under the guidance of a consultant pathologist (K.O.) the areas of tumor and normal pancreatic ductal tissue were marked. The corresponding paraffin tissue blocks were then retrieved. The tissue microarrays (TMAs) were constructed using a manual tissue arrayer (Beecher Instruments© Microarray technology). Three cores of tumor and two cores of normal ductal tissue from resection, along with control tissue, were spread over three TMAs; 3-μm thick sections were cut using a Leica© RM 2135 microtome prior to staining. These sections were then floated onto a water bath and heated to 45 °C. Following heating the sections were applied to salinized slides, to improve tissue adherence.
Immunohistochemistry
The specificity of all antibodies used in this study was confirmed by western blotting.24 The six antibodies associated with the Jak/Stat signaling pathway analyzed were IL-6R, Jak1, pJak1, and Stat3 and the two active forms of Stat3, pStat3Tyr705, and pStat3Ser727. Following de-waxing and re-hydration in xylene and decreasing concentrations of alcohol, antigen retrieval took place. Two methods of antigen retrieval were used, with sections microwaved under pressure (15 psi) in TE solution (5 mM Tris base pH 8.0 and 1 mM Sodium EDTA) for Jak1, 3332, Cell Signaling Technology; pJak1, New England Bio-Labs; pStat3Tyr705, 9131, Cell Signaling Technology; and pStat3Ser727, 9134, Cell Signaling Technology. Or incubated in 10 mM citrate buffer (epitope retrieval solution × 10, Dako, Denmark) in a calibrated water bath at 96 °C for 20 min for IL-6R, C20, SC-661, Santa Cruz; and Stat3, 9132, Cell Signaling Technology. Next, blocking of endogenous peroxidase activity was performed using 0.3 % hydrogen peroxide solution for a period of 10 minutes, followed by the blocking of non-specific background staining with 1.5 % normal horse serum (Vector Labs, USA) in tri-phosphate-buffered saline (TBS) for 20 min at room temperature. One antibody (pJak1) required further blocking with Avidin and Biotin (Vector Labs, USA) for 15 minutes each. The slides were then incubated overnight with the primary antibody at different concentrations at either 4 °C (IL-6R (1:500) and Stat3 (1:100)) or room temperature (Jak1 (1:200), pJak1 (1:25), pStat3Tyr705 (1:50), and pStat3Ser727 (1:50)) in a moisture chamber). A positive and negative control was included in each immunohistochemistry run, negative slides being incubated in an antibody diluent solution (Dako, Denmark). For pAktSer473 (1:100; pAkt44-622G, Biosource, Camarillo, CA) antigen retrieval required heating in Tris/EDTA buffer (10 mmol/L Trizma Base, 0.25 mmol/L, EDTA) at 96 °C for 20 min. Nonspecific background staining was blocked using 2.5 % horse serum in TBS for 1 h with primary incubation overnight at 4 °C. Staining was developed using EnVision kit (Dako, Denmark) and Chromagen was detected using 3,3 V-diaminobenzidine (Vector Labs, USA). The measurement of p53 and mTor expression in this cohort had been performed as part of a previous study.25,26
Tumor Evaluation and Scoring
IL6-R/Jak/Stat pathway protein expression was evaluated in the pancreatic tumor epithelium and within PanIN lesions. Tissue staining was scored blindly by two independent observers (S.M.D. and P.M.) using a weighted histoscore method,27 also known as the H score system.28 The TMA cores were examined and expression score calculated as follows (1 × percent cells staining weakly positive) + (2 × percent cells staining moderately positive) + (3 × percent cells staining strongly positive). The maximum score was 300. An interclass correlation coefficient (ICCC) for each protein was calculated to confirm consistency between observers and the mean of the two observers’ scores were used for analysis. An ICCC of 0.7 or greater is considered excellent with an ICCC of 1 indicating identical scoring.27
Measurement of C-Reactive Protein in Serum
Preoperative C-reactive protein measurements were available from the patients whose tumors were included in the TMA. Circulating C-reactive protein measurements were performed as described previously.3
Statistical Analysis
The relationships between categorical variables were analysed using the Mantel–Haenszel (χ 2) test. The Mann–Whitney U test was used to compare continuous variables. The principal outcome measure was length of overall survival as measured from time of the original surgery. Length of survival following surgery and cause of death were obtained from our database and validated using the NHS Scotland Information Services Department (http://www.isdscotland.org). Kaplan–Meier survival analysis was used to analyze the overall survival from the time of surgery with a Log-rank test performed to compare curves. To ensure mature follow-up of these data, all patients were prospectively followed until death and data censored in December 2011 by which time all except a single patient had died. A Cox proportional-hazards model was used for multivariate analysis to adjust for competing risk factors, and the hazard ratio (HR) with 95 % confidence intervals (CIs) reported as an estimate of the risk of disease-specific death. Only variables found to be significant on univariate analysis at P < 0.10 were included in multivariate analysis in a backwards-stepwise fashion. Statistical significance was set at a P ≤ 0.05. Protein expression correlation was performed using Spearman’s rank correlation test. All statistical analyses were performed using SPSS version 19.0 (IBM Corporation, NY, USA).
Results
Clinicopathological Characteristics of the Patient Cohort
Ninety-two patients were identified as having had a pancreaticoduodenectomy for PDAC. The 90-day mortality was 6.5 % (six patients), with 5.4 % (five patients) dying within 30 days of operation. These six patients were excluded from further analysis, as biomarker expression did not affect their survival, leaving 86 patients in the study. The median age of these patients at the time of surgery was 64 (range, 38–77) years. The majority of patients in the TMA cohort had tumors that were T3, <30 mm, low-grade, lymph node positive, resection margin positive, with perineural invasion and venous invasion (Table 1). Only three patients had a background of pre-existing CP. Of the 23 patients who received adjuvant therapy, 10 patients (43 %) received adjuvant treatment during the period 1995–1999 compared with 13 patients (57 %) during the period 2000–2004.
The overall median survival in this group was 16.9 months (95 % CI, 12.4–22.7). Clinicopathological features significantly associated with survival according to univariate Cox survival analysis included lymph node status, tumor grade, venous invasion and resection margin status (P < 0.05) (Table 2). There were two instances of postoperative, noncancer-related mortality that occurred as a result of pneumonia and cerebrovascular vascular accident, occurring at 14 and 44 months of follow-up, respectively.
Protein Expression
The variation in observer scoring was calculated by ICCC. Scorer variation in this study achieved an ICCC of 0.82. For the six IL-6R/Jak/Stat pathway proteins examined in this study, expression was seen in all three cellular compartments for IL-6R and pJak1. Cytoplasmic and membrane expression only was seen for Jak1 and non-activated Stat3. Both active forms of Stat3 (pStat3Tyr705 and pStat3Ser727) had protein expression observed in the cytoplasmic and nuclear compartments only (Fig. 1).
Association of IL-6R/Jak/Stat Pathway with Clinicopathological Features
While the nuclear expression of pJak1 did not significantly correlate with any clinicopathological variables, high pStatTyr705 was more frequently associated with R1 status, while high pStat3Ser727 was more frequently associated with lower grade tumors (Supplemental Table 1). The degree of immune cell infiltrate was evaluated in along with components of the IL-6RJak/Stat pathway. In those tumors with evidence of a dense immune cell infiltrate, the frequency of high nuclear pJak and high nuclear pStat3Tyr705 expression was significantly reduced (Supplemental Table 1). There appeared to be no significant association between the tumor expression of components of the IL-6R/Jak/Stat pathway and preoperative circulating levels of C-reactive protein (Supplementary Table 1).
To determine if protein expression levels were associated with survival, the patient cohort was initially split into tertiles according to expression of each protein. Kaplan–Meier survival graphs were plotted comparing tumors with combined low and moderate levels of specific protein expression to those patients with high levels. For Jak1, pJak1, Stat, pStat3Tyr705, and pStat3Ser727, the cytoplasmic and nuclear compartments were evaluated. For IL-6R, the cytoplasmic and membranous compartments were evaluated.
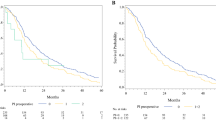
In univariate Cox regression analysis (Table 2), high membranous IL-6R expression (n = 30) was associated with significantly decreased survival compared with low expression (n = 55) following resection (HR, 1.29 (95 % CI, 1.02–1.66); P = 0.048). High nuclear pJak1 expression (n = 30) was associated with significantly reduced survival compared with low expression (n = 55) following resection (HR, 1.74 (95 % CI, 1.08–2.8), P = 0.023). High nuclear pStatTyr705 expression (n = 29) was associated with significantly reduced survival compared with low expression (n = 57) following resection (HR, 2.09 (95 % CI, 1.26–3.50), P = 0.005). High nuclear pStatSer727 expression (n = 30) was associated with significantly decreased survival compared with low expression (n = 56) following resection (HR, 1.42 (95 % CI, 1.10–1.83), P = 0.007). Kaplan–Meier survival curves illustrating the significant prognostic factors in univariate analysis are shown in Fig. 2. No other assessment of protein expression associated significantly with overall survival following resection.
Kaplan–Meier survival curves illustrating the prognostic influence of the IL-6R/Jak/Stat pathway on resected PDAC. a High membranous expression of IL-6R was associated with a poor outcome (low, 26.4 months versus high, 12.3 months; P = 0.046). b High nuclear pJak1 expression was associated with a poor outcome (low, 19.6 months versus high, 11.1 months; P = 0.022). c High nuclear pStat3Tyr705 expression was associated with poor outcome (low, 21.0 months versus high, 10.3 months; P = 0.006). d High nuclear pStat3Ser727 expression was associated with poor outcome (low, 20.1 months versus high, 10.1 months; P = 0.004). Log-rank analysis was used to compare survival curves
In order to further evaluate survival outcome we undertook survival analysis at 6 and 12 months between the groups for all studied markers (Supplementary Table 2). While there was no significant difference in survival at 6 months between any of the groups, at 12 months follow-up however, there was a significantly reduced survival for patients with high expression of nuclear pJak1 (P = 0.014), high expression of pStat3Tyr705 (P = 0.004), high expression of pStat3Ser727 (P < 0.0001), and high expression of membranous IL-6R (P = 0.039).
Most importantly, in multivariate analysis, high pJak1 expression (HR, 1.68 (95 % CI, 1.04–2.73), P = 0.036) and high pStat3Tyr705 expression (HR, 2.66 (95 % CI, 1.55–4.59), P = 0.001) remained independent predictors of poor survival when considered individually along with pathological variables. When expression of the pJak1 and pStat3Tyr705 were placed in the Cox proportional-hazards model together, each continued to provide independent prognostic information (Table 2).
Combination of Components of Jak/Stat Pathway
pJak1 and pStat3Tyr705 expression data were then combined to stratify the cohort into four groups. The combination of pJak1high/pStat3Tyr705 high (n = 16) was associated with an especially deleterious influence on overall survival following resection (median overall survival, 8.8 months (95 % CI, 4.4–13.1)) (Fig. 3). A multivariate Cox proportional-hazards model confirmed that pJak1high/pStat3Tyr705 high was an independent predictor of poor outcome (HR, 3.02 (95 % CI, 1.57–5.77), P = 0.001).
Kaplan–Meier survival curves for 85 patients according to combined pJak1 and pStat3Tyr705 status in PDAC. A combination of pJak1high/pStat3Tyr705 high resulted in a significantly reduced overall survival. For pJak1low/pStat3Tyr705 low versus pJak1high/pStat3Tyr705 high, P < 0.001. For pJak1low/pStat3Tyr705 low versus pJak1low/pStat3Tyr705 high, P = 0.018. Log-rank analysis was used to compare survival curves
Expression IL-6R/Jak/Stat in PanINs
While there was evidence of high pJak1 and pStat3Tyr705 expression in 84 and 87 % of early PanIN lesions, respectively, IL-6R was rarely expressed in the PanINs associated with these tumors.
Relationship of L-6R/Jak/Stat Activation with Signaling Pathways in PDAC
IL-6R membranous expression correlated weakly with nuclear pStatSer727 (Spearman’s rho = 0.242, P = 0.027). Furthermore, cytoplasmic IL-6R expression correlated with pJak1 expression (Spearman’s rho = 0.223, P = 0.042) and nuclear pStatTyr705 (Spearman’s rho = 0.343, P = 0.003). There was a significant correlation between nuclear pJak1 expression and both nuclear pStatTyr705 (Spearman’s rho = 0.461, P = 0.001) and nuclear pStatSer727 (Spearman’s rho = 0.295, P = 0.006). Nuclear pJak expression was correlated strongly correlated with cytoplasmic expression (Spearman’s rho = 0.61, P < 0.0001); however, nuclear expression associated more strongly with prognosis.
To determine whether Jak/Stat activation in PDAC correlated with other related signaling pathways the expression of non-activated and activated Jak1 and Stat3 was assessed in the context of mTor, pAkt, and p53 protein expression. There was no significant correlation between cytoplasmic mTor expression and any component of the IL-6R/Jak/Stat pathway. pStatTyr705 expression was found to correlate significantly with pAkt expression (Spearman’s rho = 0.331, P = 0.002). Furthermore, pAkthigh/pStatTyr705 high expression (n = 16) was associated with an especially poor outcome (median overall survival 9.1 months (95 % CI, 6.3–11.7)).
p53Low expression in combination with pStat3Tyr705 low expression was associated with a favorable outcome (median, 21.5 months (95 % CI, 9.1–33.5)). However, p53high/pStat3Tyr705 high expression had a negative impact on survival following resection (median, 9.0 months (95 % CI, 1.9–16.1), P = 0.013). We noted that pStat3Tyr705 high/p53low was an uncommon combination (n = 7) associated with a poor outcome (median, 10.3 months (95 % CI, 2.3–18.2)) (Fig. 4).
Kaplan–Meier survival curves for 86 patients according to combined p53 and pStat3Tyr705 status in PDAC. A combination of p53high/pStat3Tyr705 high resulted in a significantly reduced overall survival. For p53low/pStat3Tyr705 low versus p53high/pStat3Tyr705 high, P = 0.013. For p53low/pStat3Tyr705 low versus p53low/pStat3Tyr705 high, P = 0.002. Log-rank analysis was used to compare survival curves
Discussion
Tumor-associated inflammation has been recognized as an important hallmark of cancer,29 either through initiation, extrinsic cause or supporting the intrinsic microenvironment during tumor progression.30 Survival following resection of PDAC remains poor and in contrast to developments in other solid malignancies, molecular features of PDAC that predict utility of targeted therapies have yet to be defined. The disease is associated with significant peritumoral inflammation, with inflammatory pathways implicated in both tumorigenesis and tumor promotion. Furthermore, studies in human PDAC have established that systemic inflammation, assessed by C-reactive protein levels, is associated with significantly poorer outcome.3,31 Subsequently, this study was conducted to examine the prognostic influence of activation of the IL-6R/Jak/Stat signaling pathway in PDAC and assess the relationship between systemic inflammation and activation of these intra-tumoral inflammatory pathways.
The IL-6R is predominantly located in the cell membrane; however, the IL-6/IL-6 receptor complex enter the cell by endocytosis as part of the protein-recycling process,32 a potential method of downregulating receptors once the ligand has produced the appropriate signal.32 Therefore as the IL-6R, unlike the other signaling proteins in the pathway does not have a phosphorylated form, the localization of the IL-6R to the cytoplasm may be used as a surrogate marker for activation. The current data demonstrate that high IL-6R membranous expression was associated with poor overall survival following resection in univariate analysis, providing novel insight into expression of membrane bound IL-6R in human PDAC. Potentially this association may be explained by an upregulation as a result of pathway activation. Upregulation of the signal-transducing component of the IL-6R complex, gp130 has been demonstrated in both human PDAC cell lines and human PDAC tissue at the mRNA level.33 Certainly, antibodies to gp130 have been shown to inhibit pStat3 in a dose-dependent manner in PDAC cell lines.33 Ebrahimi and colleagues examined circulating IL-6 in patients with PDAC, establishing a correlation with poor performance status, increased weight loss, and independent prediction of poor survival,34 a finding consistent with a specific polymorphism reported to be overrepresented in such patients.35 While there was no obvious relationship between components of the Jak/Stat pathway and circulating C-reactive protein, we did not measure circulating IL-6, the principal but not sole regulator of serum C-reactive protein levels, and it is possible that this may be a potential link between systemic inflammation and pancreatic progression as demonstrated in a Kras murine model.36
A number of upregulated inflammatory and oncogenic pathways in PDAC converge on the transcription factors NF-κB and Stat3,37 suggesting that these are excellent potential direct therapeutic targets for inhibition. Stat3 is aberrantly activated in a variety of human cancers playing a crucial role in cell proliferation, invasion and tumor-promoting inflammation.10 The Jak1 and Stat3 proteins become activated in sequence, upon the binding of IL-6 to the IL-6R.38 Stat3 is phosphorylated at two different sites, tyrosine 705 and serine 727 positions. Jak1 phosphorylates Stat3 at tyrosine 705, while the kinase(s) that mediate serine phosphorylation remain to be determined. Immunohistochemical staining in our cohort of patients has demonstrated that both phosphorylated forms of Stat3, pStat3Tyr705 and pStat3Ser727 are found in the cytoplasmic and nuclear cellular compartments. While expression of activated components of the IL-6R/Jak/Stat pathway demonstrated only limited correlation with pathological features of PDAC, there were significant associations of nuclear pJak1 and pStat3 at both sites with poor overall survival in univariate analysis. pStat3Ser727 expression was associated with low-grade tumors suggesting that elevated pStat3Ser727 expression in PDAC and the poor outcome associated with this phenotype is not simply the result of tumor de-differentiation. These data provide strong evidence for pStat3Tyr705 in particular having a significant role in PDAC.
We have recently demonstrated that a dense peritumoral infiltrate was associated with a significantly prolonged survival following resection.23 A potential explanation for these data may be that Stat3 propagates several levels of crosstalk between tumor cells and their immunological microenvironment, leading to tumor-induced immunosuppression. Stat3 constitutive activity in tumor cells is able to inhibit the maturation of antigen presenting cells, including dendritic cells and macrophages, at least partly through the production of soluble energizing factors, such as IL-10 and VEGF and the reduced secretion of pro-inflammatory mediators.10
Recently, there has been strong evidence of pro-inflammatory cytokine production in myeloid cells, in particular IL-6, driving Stat3 activation which subsequently cooperates with mutated Kras to promote acinar ductal metaplasia resulting in murine PanIN formation, with supporting data demonstrated in human specimens.36 Additionally, a critical role for Stat3 in murine PDAC initiation highlights the potential for Stat3 to integrate inflammation-associated processes including pancreatitis driven PanIN development and potentially may serve as a therapeutic target for preventing inflammation-associated PDAC formation at the earliest stage.17
Data from the current study demonstrated a significant correlation between IL-6R, pJak, and pStat3 expression supporting findings from the previous animal models. The finding in the present study that IL-6R is not expressed in early human PanIN lesions present in adjacent tissue to the PDAC when compared with pJak and pStat3 expression suggests that the latter aberrations are relatively early events, supporting findings of the recent murine models implicating Stat3 in PDAC tumorigenesis.17,33,36 This apparent integral role for Stat3 at early stages of PDAC tumorigenesis but with evidence of a more restricted pattern of expression in later stage human PDAC provided by the present cohort suggests that Stat3 may have variable roles during PDAC tumor evolution and progression, potentially influencing immunoediting of the cellular infiltrate within the microenvironment as the tumor progresses. Despite the attractive demonstration of an integral role for Stat3 tumorigenesis in mouse models, these are not a true recapitulation of the clinical scenario and further detailed assessment within human PDAC and human CP specimens will be necessary before definite conclusions are drawn. While CP is an established risk factor for PDAC, in our unit the frequency of pancreatic malignancy in patients with established CP is relatively low, possibly as a result of the reduced life expectancy associated with this group of patients. The rate of resection for PDAC originating on a background of CP is even less common in our experience as a result of extensive comorbidities and local complications (venous colateralization). In the studied cohort, only three patients had a background of pre-existing CP. Unfortunately, such limited numbers restricted our ability to compare IL-6R/Jak/Stat pathway activation with tumors that did not originate on the background of CP.
It should be noted that Stat3 activation is further regulated by a variety of factors in addition to IL-6, including its endogenous inhibitor Socs3.10 Deletion of Socs3 entirely in the murine KrasG12D model resulted in profound Stat3 phosphorylation and subsequent acceleration of PDAC development.36 Further characterization of Socs3 expression in human PDAC is therefore of interest.
We noted there to be significant staining for pJak in the nucleus. While traditionally Jak is localized to the cytoplasmic compartment, there is increasing evidence supporting a role for nuclear translocation of the Jak proteins. When these events occur during critical windows in cellular development, and when the amplitude and duration of Jak activity are properly regulated, these roles are essential in determining cell fate and proliferation. Besides their canonical role as activators of the Stat transcription factors, the Jaks are now known to affect gene expression by activating other transcription factors and exerting epigenetic actions by phosphorylating histone H3.39 Furthermore there is evidence that nuclear Jak2 may play a role in preventing the epithelial-to-mesenchymal transition associated with carcinoma metastasis.40
The finding of a poor outcome associated with Stat3Tyr705 high and p53high expression is in keeping with findings of an orthotopic model of pancreatic ductal cells from KrasG12D mutant mice with p53 inactivation in which Stat3 knockdown reduced PDAC development.33 The low frequency of Stat3Tyr705 high/p53low tumors may support the concept that abnormal p53 is necessary for activation of Stat3 in the majority.41 Certainly, further work will be required to define the functional role of Stat3 in advanced human pancreatic cancer.
To date, there has been only limited assessment of prognostic utility of Stat3 expression in human PDAC specimens42 with limited cohort size preventing survival analysis. Therefore, the present human PDAC cohort represents the largest study investigating the expression of the Jak/Stat pathway.
It is likely that PDAC progression and hence prognosis is continually influenced by extrinsic inflammation. Systemic activation of COX-2, NF-KB, nitric oxide synthetase, production of IL-1, IL-6, IL-8, TNF-α, and free radical oxygen formation 43 have all been associated with PDAC progression. Obese individuals have an elevated incidence and poorer prognosis associated with pancreatic cancer 44 and have been observed to have higher circulating levels of pro-inflammatory adipokines including resistin and leptin (a ligand of the gp130 receptor),45 while at the same time lower level of the anti-inflammatory adipokine adiponectin.46 Furthermore, the upregulation of IL-6 and downregulation of Socs3 expression in the lungs of mice exposed to cigarette smoke 47 provides further evidence of role played by IL6-R/Jak/Stat3 signaling in the integration of extrinsic and intrinsic inflammatory factors.
The utility of the Jak/Stat pathway as a therapeutic target is supported by knockdown of Stat3 and Jak2 inhibition abrogating growth of a variety of solid tumor xenografts, including pancreatic.48 Inhibition of Stat3 in human PDAC cells accelerates apoptosis and constrains chemoresistance,19 in addition to inhibiting tumor growth, invasion 46 and angiogenesis potentially via reduced MMP7 expression.49 Additionally, there is evidence that Stat3 activation may represent a biomarker of resistance to targeted therapies to the Src and EGFR pathways.50 Moreover, therapeutic targeting of the Jak/Stat pathway with Jak2 inhibitors has proven useful in a murine model of PDAC and within human PDAC cell lines.33 As a combination of high expression of pJak1 and pStat3 described a sub-group of patients with an especially poor outcome this may potentially support a strategy to inhibit IL-6R/Jak/Stat signaling at multiple points of the pathway simultaneously. Potentially tumor expression of this pathway could be assessed in samples collected using endoscopic ultrasound guidance. This would enable biomarker stratification in resectable and nonresectable cohorts.
We acknowledge that the R1 rate reported in this manuscript is higher than in much of the literature. Certainly, recent studies suggest that if pathological assessment is detailed and standardized, margin involvement is found in greater than 75 % of resections for pancreatic cancer. In particular, the use of a detailed standardized histopathological protocol to assess pancreaticoduodenectomy specimens resulted in an R1 rate of 84 %, which correlated with outcome following resection with curative intent.51 We have previously reported an R1 rate of 74 % in our own cohort of 147 patients.21 The reasons for underestimation of R1 involvement within the literature are manifold and include controversy regarding the definition of microscopic margin involvement and lack of detailed standardized pathological examination protocol.
While detailed and mature follow-up data were available for all patients, this study was limited by the lack of a standardized adjuvant chemotherapy protocol. Furthermore, we acknowledge that the rate of adjuvant chemotherapeutic allocation is relatively low in this cohort, a reflection of post-operative morbidity delaying administration, poor performance status and patients declining further therapy. Following the results of randomized trial evidence (ESPAC-1 study), the allocation of adjuvant therapy in our cohort has increased. Certainly, investigation of the IL-6R/Jak/Stat pathway requires further evaluation in a cohort with higher rates of adjuvant therapy. While long-term preoperative anti-inflammatory medication including aspirin and statin data would have been valuable unfortunately this information was not available for all patients.
With regards to the ultimate driver of inflammation, tumor hypoxia may provide a potential explanation. An important hypoxic stress pathway is regulated by HIF-1α52 that is, in turn, a potent stimulator of IL-6 production from the tumor and immune infiltrating cells.53 Further investigation will be required to develop the relationship between hypoxia and inflammation in pancreatic cancer.
In summary, while these data do not support the hypothesis that measureable systemic inflammation in PDAC is related to activation of this cytokine-mediated pathway, they do support the concept that the IL-6R/Jak/Stat pathway is activated and is integral in human PDAC, as has been suggested in murine models. The personalization of PDAC management has the potential to improve the current dismal prognosis.54 We have provided the strongest evidence to date that activation of the Jak/Stat pathway is associated with poor prognosis following resection of PDAC and could serve as a biomarker to guide targeted therapies including Jak inhibitors. Undoubtedly, more profound understanding of components of the inflammatory cytokine milieu including interaction with the tumor-associated immune cell infiltrate will be necessary to unravel the relationship between inflammation, pancreatic cancer, and poor outcome.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin 2008; 58(2):71–96
Sener SF, Fremgen A, Menck HR, Winchester DP. Pancreatic cancer: a report of treatment and survival trends for 100,313 patients diagnosed from 1985–1995, using the National Cancer Database. J Am Coll Surg 1999; 189(1):1–7.
Jamieson NB, Denley SM, Logue J, Mackenzie DJ, Foulis AK, Dickson EJ, Imrie CW, Carter R, McKay CJ, McMillan DC. A prospective comparison of the prognostic value of tumor- and patient-related factors in patients undergoing potentially curative surgery for pancreatic ductal adenocarcinoma. Annals of Surgical Oncology 2011; 18(8):2318–28.
Glen P, Jamieson NB, McMillan DC, Carter R, Imrie CW, McKay CJ. Evaluation of an inflammation-based prognostic score in patients with inoperable pancreatic cancer. Pancreatology 2006; 6(5):450–3.
Martignoni ME, Kunze P, Hildebrandt W, Kunzli B, Berberat P, Giese T, Kloters O, Hammer J, Buchler MW, Giese NA, Friess H. Role of mononuclear cells and inflammatory cytokines in pancreatic cancer-related cachexia. Clin Cancer Res 2005; 11(16):5802–8.
Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW, Lankisch PG, Andersen JR, Dimagno EP, Andren-Sandberg A, Domellof L. Pancreatitis and the risk of pancreatic cancer. International Pancreatitis Study Group. N Engl J Med 1993; 328(20):1433–7.
Guerra C, Schuhmacher AJ, Canamero M, Grippo PJ, Verdaguer L, Perez-Gallego L, Dubus P, Sandgren EP, Barbacid M. Chronic pancreatitis is essential for induction of pancreatic ductal adenocarcinoma by K-Ras oncogenes in adult mice. Cancer Cell 2007; 11(3):291–302.
Coughlin SS, Calle EE, Patel AV, Thun MJ. Predictors of pancreatic cancer mortality among a large cohort of United States adults. Cancer Causes Control 2000; 11(10):915–23
Aggarwal BB, Kunnumakkara AB, Harikumar KB, Gupta SR, Tharakan ST, Koca C, Dey S, Sung B. Signal transducer and activator of transcription-3, inflammation, and cancer: how intimate is the relationship? Ann N Y Acad Sci 2009; 1171:59–76.
Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer 2009; 9(11):798–809.
Yeh HH, Lai WW, Chen HH, Liu HS, Su WC. Autocrine IL-6-induced Stat3 activation contributes to the pathogenesis of lung adenocarcinoma and malignant pleural effusion. Oncogene 2006; 25(31):4300–9.
Morikawa T, Baba Y, Yamauchi M, Kuchiba A, Nosho K, Shima K, Tanaka N, Huttenhower C, Frank DA, Fuchs CS, Ogino S. STAT3 expression, molecular features, inflammation patterns, and prognosis in a database of 724 colorectal cancers. Clin Cancer Res 2011; 17(6):1452–62.
Bromberg J, Wang TC. Inflammation and cancer: IL-6 and STAT3 complete the link. Cancer Cell 2009; 15(2):79–80.
Ferrone C, Dranoff G. Dual roles for immunity in gastrointestinal cancers. J Clin Oncol 2010; 28(26):4045–51.
Scholz A, Heinze S, Detjen KM, Peters M, Welzel M, Hauff P, Schirner M, Wiedenmann B, Rosewicz S. Activated signal transducer and activator of transcription 3 (STAT3) supports the malignant phenotype of human pancreatic cancer. Gastroenterology 2003; 125(3):891–905.
Miyatsuka T, Kaneto H, Shiraiwa T, Matsuoka TA, Yamamoto K, Kato K, Nakamura Y, Akira S, Takeda K, Kajimoto Y, Yamasaki Y, Sandgren EP, Kawaguchi Y, Wright CV, Fujitani Y. Persistent expression of PDX-1 in the pancreas causes acinar-to-ductal metaplasia through Stat3 activation. Genes Dev 2006; 20(11):1435–40.
Fukuda A, Wang SC, Morris JPt, Folias AE, Liou A, Kim GE, Akira S, Boucher KM, Firpo MA, Mulvihill SJ, Hebrok M. Stat3 and MMP7 contribute to pancreatic ductal adenocarcinoma initiation and progression. Cancer Cell 2011; 19(4):441–55.
Aggarwal BB, Vijayalekshmi RV, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res 2009; 15(2):425–30.
Lin L, Hutzen B, Zuo M, Ball S, Deangelis S, Foust E, Pandit B, Ihnat MA, Shenoy SS, Kulp S, Li PK, Li C, Fuchs J, Lin J. Novel STAT3 phosphorylation inhibitors exhibit potent growth-suppressive activity in pancreatic and breast cancer cells. Cancer Res 2010; 70(6):2445–54.
Neoptolemos JP, Stocken DD, Dunn JA, Almond J, Beger HG, Pederzoli P, Bassi C, Dervenis C, Fernandez-Cruz L, Lacaine F, Buckels J, Deakin M, Adab FA, Sutton R, Imrie C, Ihse I, Tihanyi T, Olah A, Pedrazzoli S, Spooner D, Kerr DJ, Friess H, Buchler MW. Influence of resection margins on survival for patients with pancreatic cancer treated by adjuvant chemoradiation and/or chemotherapy in the ESPAC-1 randomized controlled trial. Ann Surg 2001; 234(6):758–68.
Jamieson NB, Foulis AK, Oien KA, Going JJ, Glen P, Dickson EJ, Imrie CW, McKay CJ, Carter R. Positive mobilization margins alone do not influence survival following pancreatico-duodenectomy for pancreatic ductal adenocarcinoma. Ann Surg 2010; 251(6):1003–10.
The Royal College of Pathologists. Standards and Minimum Datasets for Reporting Cancers. Minimum Dataset for the Histopathological Reporting of Pancreatic, Ampulla of Vater and Bile Duct Carcinoma. London: The Royal College of Pathologists, 2002.
Jamieson NB, Mohamed M, Oien KA, Foulis AK, Dickson EJ, Imrie CW, Carter CR, McKay CJ, McMillan DC. The relationship between tumor inflammatory cell infiltrate and outcome in patients with pancreatic ductal adenocarcinoma. Ann Surg Oncol 2012; 19(11):3581–90.
Tam L, McGlynn LM, Traynor P, Mukherjee R, Bartlett JM, Edwards J. Expression levels of the JAK/STAT pathway in the transition from hormone-sensitive to hormone-refractory prostate cancer. Br J Cancer 2007; 97(3):378–83.
Morton JP, Timpson P, Karim SA, Ridgway RA, Athineos D, Doyle B, Jamieson NB, Oien KA, Lowy AM, Brunton VG, Frame MC, Evans TR, Sansom OJ. Mutant p53 drives metastasis and overcomes growth arrest/senescence in pancreatic cancer. Proc Natl Acad Sci U S A 2010; 107(1):246–51.
Kennedy AL, Morton JP, Manoharan I, Nelson DM, Jamieson NB, Pawlikowski JS, McBryan T, Doyle B, McKay C, Oien KA, Enders GH, Zhang R, Sansom OJ, Adams PD. Activation of the PIK3CA/AKT pathway suppresses senescence induced by an activated RAS oncogene to promote tumorigenesis. Mol Cell 2011; 42(1):36–49.
Kirkegaard T, Edwards J, Tovey S, McGlynn LM, Krishna SN, Mukherjee R, Tam L, Munro AF, Dunne B, Bartlett JM. Observer variation in immunohistochemical analysis of protein expression, time for a change? Histopathology 2006; 48(7):787–94.
McCarty KS, Jr., Szabo E, Flowers JL, Cox EB, Leight GS, Miller L, Konrath J, Soper JT, Budwit DA, Creasman WT, et al. Use of a monoclonal anti-estrogen receptor antibody in the immunohistochemical evaluation of human tumors. Cancer Res 1986; 46(8 Suppl):4244s–4248s.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell 2011; 144(5):646–74.
Maniati E, Bossard M, Cook N, Candido JB, Emami-Shahri N, Nedospasov SA, Balkwill FR, Tuveson DA, Hagemann T. Crosstalk between the canonical NF-kappaB and Notch signaling pathways inhibits Ppargamma expression and promotes pancreatic cancer progression in mice. J Clin Invest 2011; 121(12):4685–99.
Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O’Reilly DS, Foulis AK, Horgan PG, McMillan DC. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer 2011; 47(17):2633–41.
Nesbitt JE, Fuller GM. Differential regulation of interleukin-6 receptor and gp130 gene expression in rat hepatocytes. Mol Biol Cell 1992; 3(1):103–12.
Corcoran RB, Contino G, Deshpande V, Tzatsos A, Conrad C, Benes CH, Levy DE, Settleman J, Engelman JA, Bardeesy N. STAT3 plays a critical role in KRAS-induced pancreatic tumorigenesis. Cancer Res 2011; 71(14):5020–9.
Ebrahimi B, Tucker SL, Li D, Abbruzzese JL, Kurzrock R. Cytokines in pancreatic carcinoma: correlation with phenotypic characteristics and prognosis. Cancer 2004; 101(12):2727–36.
Talar-Wojnarowska R, Gasiorowska A, Smolarz B, Romanowicz-Makowska H, Kulig A, Malecka-Panas E. Clinical significance of interleukin-6 (IL-6) gene polymorphism and IL-6 serum level in pancreatic adenocarcinoma and chronic pancreatitis. Dig Dis Sci 2009; 54(3):683–9.
Lesina M, Kurkowski MU, Ludes K, Rose-John S, Treiber M, Kloppel G, Yoshimura A, Reindl W, Sipos B, Akira S, Schmid RM, Algul H. Stat3/Socs3 activation by IL-6 transsignaling promotes progression of pancreatic intraepithelial neoplasia and development of pancreatic cancer. Cancer Cell 2011; 19(4):456–69.
Li N, Grivennikov SI, Karin M. The unholy trinity: inflammation, cytokines, and STAT3 shape the cancer microenvironment. Cancer Cell 2011; 19(4):429–31.
Schindler C, Darnell JE, Jr. Transcriptional responses to polypeptide ligands: the JAK-STAT pathway. Annu Rev Biochem 1995; 64:621–51.
Zouein FA, Duhe RJ, Booz GW. JAKs go nuclear: emerging role of nuclear JAK1 and JAK2 in gene expression and cell growth. Growth Factors 2011; 29(6):245–52.
Nilsson J, Helou K, Kovacs A, Bendahl PO, Bjursell G, Ferno M, Carlsson P, Kannius-Janson M. Nuclear Janus-activated kinase 2/nuclear factor 1-C2 suppresses tumorigenesis and epithelial-to-mesenchymal transition by repressing Forkhead box F1. Cancer Res 2010; 70(5):2020–9.
Lin J, Jin X, Rothman K, Lin HJ, Tang H, Burke W. Modulation of signal transducer and activator of transcription 3 activities by p53 tumor suppressor in breast cancer cells. Cancer Res 2002; 62(2):376–80.
Doucas H, Mann CD, Sutton CD, Garcea G, Neal CP, Berry DP, Manson MM. Expression of nuclear Notch3 in pancreatic adenocarcinomas is associated with adverse clinical features, and correlates with the expression of STAT3 and phosphorylated Akt. J Surg Oncol 2008; 97(1):63–8.
Farrow B, Sugiyama Y, Chen A, Uffort E, Nealon W, Mark Evers B. Inflammatory mechanisms contributing to pancreatic cancer development. Ann Surg 2004; 239(6):763–9.
Bracci PM. Obesity and pancreatic cancer: overview of epidemiologic evidence and biologic mechanisms. Mol Carcinog 2012; 51(1):53–63.
Hursting SD, Berger NA. Energy balance, host-related factors, and cancer progression. J Clin Oncol 2010; 28(26):4058–65.
Kowalska I, Straczkowski M, Nikolajuk A, Adamska A, Karczewska-Kupczewska M, Otziomek E, Kinalska I, Gorska M. Insulin resistance, serum adiponectin, and proinflammatory markers in young subjects with the metabolic syndrome. Metabolism 2008; 57(11):1539–44.
Halappanavar S, Stampfli MR, Berndt-Weis L, Williams A, Douglas GR, Yauk CL. Toxicogenomic analysis of mainstream tobacco smoke-exposed mice reveals repression of plasminogen activator inhibitor-1 gene in heart. Inhal Toxicol 2009; 21(1):78–85.
Hedvat M, Huszar D, Herrmann A, Gozgit JM, Schroeder A, Sheehy A, Buettner R, Proia D, Kowolik CM, Xin H, Armstrong B, Bebernitz G, Weng S, Wang L, Ye M, McEachern K, Chen H, Morosini D, Bell K, Alimzhanov M, Ioannidis S, McCoon P, Cao ZA, Yu H, Jove R, Zinda M. The JAK2 inhibitor AZD1480 potently blocks Stat3 signaling and oncogenesis in solid tumors. Cancer Cell 2009; 16(6):487–97.
Li H, Huang C, Huang K, Wu W, Jiang T, Cao J, Feng Z, Qiu Z. STAT3 knockdown reduces pancreatic cancer cell invasiveness and matrix metalloproteinase-7 expression in nude mice. PLoS One 2011; 6(10):e25941.
Nagaraj NS, Washington MK, Merchant NB. Combined blockade of Src kinase and epidermal growth factor receptor with gemcitabine overcomes STAT3-mediated resistance of inhibition of pancreatic tumor growth. Clin Cancer Res 2011; 17(3):483–93.
Verbeke CS, Leitch D, Menon KV, McMahon MJ, Guillou PJ, Anthoney A. Redefining the R1 resection in pancreatic cancer. Br J Surg 2006; 93(10):1232–7.
Poon E, Harris AL, Ashcroft M. Targeting the hypoxia-inducible factor (HIF) pathway in cancer. Expert Rev Mol Med 2009; 11:e26.
Lang SA, Moser C, Gaumann A, Klein D, Glockzin G, Popp FC, Dahlke MH, Piso P, Schlitt HJ, Geissler EK, Stoeltzing O. Targeting heat shock protein 90 in pancreatic cancer impairs insulin-like growth factor-I receptor signaling, disrupts an interleukin-6/signal-transducer and activator of transcription 3/hypoxia-inducible factor-1alpha autocrine loop, and reduces orthotopic tumor growth. Clin Cancer Res 2007; 13(21):6459–68.
Majewski IJ, Bernards R. Taming the dragon: genomic biomarkers to individualize the treatment of cancer. Nat Med 2011; 17(3):304–12.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presentation: This work has been presented in part at the 46th Annual Pancreas Club Meeting, San Diego, Friday 18th May 2012.
Rights and permissions
About this article
Cite this article
Denley, S.M., Jamieson, N.B., McCall, P. et al. Activation of the IL-6R/Jak/Stat Pathway is Associated with a Poor Outcome in Resected Pancreatic Ductal Adenocarcinoma. J Gastrointest Surg 17, 887–898 (2013). https://doi.org/10.1007/s11605-013-2168-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2168-7