Abstract
Background
Extraosseous Ewing's sarcoma (EES) is a mesenchyme-derived small blue cell tumor, which is distinguished by its rarity, aggressiveness, dismal prognosis, and distinct pathogenesis. Occurring almost exclusively among children and young adults, EES can arise from a variety of organs and portends a rapid clinical deterioration and high likelihood of recurrence.
Discussion
We present the first reported case of a primary pancreatic Ewing's sarcoma in a patient with concomitant portal vein thrombosis. The atypical presentation of this extraordinarily rare tumor underscores the imperative to maintain EES in the differential diagnosis of suspicious, indistinct pancreatic lesions in young patients. In addition, we review the available literature describing additional cases of primary pancreatic Ewing's sarcoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Ewing's sarcoma family of tumors (ESFT) encompasses Ewing's sarcoma of bone, Askin's tumor, primitive neuroectodermal tumor (PNET), and extraosseous Ewing's sarcoma (EES). This malignant conglomerate displays aggressive dissemination, rapid clinical deterioration, as well as similar susceptibility to treatment modalities. From the initial systematic classification over three decades ago, EES/PNETs have been reported in a continually broadening array of organs, including the lung, kidney, heart, uterus, bladder, salivary glands, vagina, prostate, stomach, pancreas, and esophagus.1,2 In this report, we describe a unique clinical presentation, perioperative diagnostic workup, surgical treatment, and histopathological features of this rare pancreatic neoplasm while reviewing the available literature on the subject.
Case Report
A 23-year-old man, with no prior medical history, presented to the Emergency Department with a 3-day history of sudden-onset upper abdominal pain accompanied by nausea. The patient denied prior similar episodes and any history of pancreatitis while acknowledging daily alcohol consumption and frequent marijuana use.
Physical exam revealed an afebrile, normotensive patient with marked left upper quadrant tenderness but no palpable masses or signs of peritoneal irritation. Laboratory chemistries were within normal limits. A computed tomography (CT) scan of the abdomen and pelvis with contrast was obtained as part of his initial workup (Fig. 1a, b). The study revealed a complex mass within the distal body and proximal tail of the pancreas measuring 5.8 × 5.4 cm with marked associated inflammation. Additional findings included a non-occlusive portal vein thrombosis (Fig. 1b). Subsequent endoscopic ultrasound (EUS) confirmed the presence of a cystic lesion with papillary projections, septations, and a solitary mural nodule; portal vein thrombosis was also visualized (Fig. 2). A fine needle aspiration biopsy was not obtained as there was a clear indication for resection with the presumed diagnosis of a cystic pancreatic neoplasm in a young symptomatic healthy patient. Moreover, during preoperative evaluation, portal vein thrombosis was considered to be a fibrin thrombus secondary to a paraneoplastic hypercoagulable state and not hematogenous infiltration of the tumor.
The patient was taken to the operating room and a laparoscopic distal pancreatectomy with splenectomy was performed. The procedure was completed uneventfully, although there was severe pancreatic inflammation surrounding the tumor. Once the splenic vessels had been isolated and divided separately, pancreatic parenchymal transection was performed with a linear stapler buttressed with absorbable mesh.
Gross pathology showed an ovoid 5.6 × 5.0 × 3.0-cm tumor revealing a large trabeculated cavity which contained fluid and coagulated blood. Necrosis was noted within the central part of the tumor. The splenic vein proximal to the lesion was dilated and contained a pale tan to red–brown thrombus, representing vascular invasion of the splenic vein. Marked lymphadenopathy was also noted along the splenic vessels.
Microscopically, the pancreatic tumor was characterized by sheets of small blue cells showing irregular nuclei, nuclear grooves, and scant cytoplasm (Fig. 3a). Frequent mitotic figures were observed up to ten to 12 mitoses per ten high-power fields. Of particular interest was an island of tumor cells that was observed within the lumen of the splenic vein, surrounded by fibrin, platelets, and other blood elements (Fig. 3). Nodal metastasis was observed in one out of 24 lymph nodes. Although the pancreatic and peripheral margins were free of tumor involvement, the tumor thrombosis extended to the splenic vein margin.
Immunohistochemical studies demonstrated diffuse positivity for CD99 (Fig. 3b), cytokeratin AE1/AE3, Cam 5.2, CK19, vimentin, and BCL-2, as well as focal positivity for neuron-specific enolase (NSE), EMA, and cyclin D1. In contrast, the neoplastic cells were nonreactive for S100, CD10, alpha-antitrypsin, E-cadherin, CD56, beta-catenin, calretinin, inhibin, CD34, progesterone receptor, CK/7, CA19.9, synaptophysin, and chromogranin. Additionally, periodic acid-Schiff staining with and without diastase revealed glycogen in the cytoplasm of the tumor cells. Collectively, the phenotypic profile of the tumor diverged strikingly from common pancreatic neoplasms. Additional molecular analysis demonstrated the presence of the EWSR1–FLT1 fusion transcript via RT-PCR, supporting the diagnosis of Ewing sarcoma/PNET.
The patient was discharged from the hospital on post-operative day 7 after complete systemic anti-coagulation had been achieved due to his portal vein thrombosis. He was re-admitted 4 days later with abdominal pain but no signs of sepsis. A symptomatic peri-pancreatic fluid collection caused by a pancreatic fistula from the staple line was successfully treated with pancreatic stenting and endoscopic cyst-gastrostomy. The patient was subsequently discharged home on a regular diet and referred to Medical Oncology for further adjuvant therapy.
Discussion
The pathogenesis of ESFT results from reciprocal chromosomal translocations invariably involving the EWSR1 gene with a member of the ET-family transcription factors, such as FLI1, ERG, ETV1, ETV4, and FEV.3 The genetic analysis of the patient's tumor demonstrated the presence of the most common genetic aberration associated with EES, t(11;22)(q24;q12), which transposes the EWSR1 gene within close proximity to the FLI1 gene, producing a novel transcript and chimeric protein.3 The resulting in-frame fusion protein functions as an oncogene by facilitating global transcriptional dysregulation.3
Together EESs and PNETs comprise a subtype of histologically indistinguishable childhood malignancies, which require immunohistochemical and genetic analysis for definitive diagnosis and classification. The immunohistochemical profile of EES/PNETs consists of universal, diffuse overexpression of the membrane-bound glycoprotein CD99 (MIC2); however, EES can be distinguished by the absence of markers of neuroendocrine differentiation that are typical of PNETs. Notably, this patient's tumor did not express neuroendocrine markers, such as synaptophysin, chromogranin, or S-100; however, there was observed focal positivity to NSE. Therefore, the immunohistochemical profile of the tumor is most consistent with EES.
While highly unlikely, the possibility that the patient's tumor represents a pancreatic metastasis from an unknown primary source must be entertained. To date, only three cases of pancreatic metastasis from Ewing's sarcoma have been reported in the literature,4 all of which originated from an osseous focus. Our patient did not demonstrate any clinical, laboratory, or radiographic evidence of a separate primary lesion in the bone or elsewhere that could have disseminated to the pancreas; therefore, we are highly confident that this tumor is derived primarily and exclusively from the pancreas.
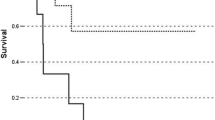
The existing medical literature on EES/PNETs invariably describes an aggressive clinical course with early distant metastasis. Moreover, the high rate of recurrence after surgical resection implies that there is likely subclinical metastatic dissemination at diagnosis,5 indicating a role for systemic therapy in this patient population. A retrospective analysis of 24 patients with confirmed EES concluded that age at diagnosis along with the type and extent of surgical resection was a more accurate prognostic indicator than the tumor size or presence of metastatic disease. Furthermore, the overall 5-year survival rate and disease-free survival rate of patients with EES is estimated to be 61 and 54 %, respectively.6 Regarding pancreatic Ewing's sarcoma specifically, there is a paucity of data concerning the prognosis and natural history of this disease, largely due to its miniscule incidence; thus, statistically powerful analyses to guide treatment are severely hindered. Unfortunately, given its rarity, limited data exist concerning the prognosis, treatment efficacy, and clinical outcomes of patients with primary pancreatic Ewing's sarcoma.
Only 21 cases, including this one, of EES/PNETs arising in the pancreas have been reported in the literature to date (Table 1). The mean age at diagnosis was 20.4 years with no significant sex predilection (11 males, nine females). The most common presenting symptom was abdominal pain with or without jaundice, with other less frequent presentations including precocious puberty (two), dyspepsia (one), anemic symptoms (one), and gallstone pancreatitis (one). Following surgical resection, the majority of patients received adjuvant chemotherapy (65 %), with a subset (20 %) receiving a combination of chemotherapy and radiation. Interestingly, none of these cases reported portal vein thrombosis, either at clinical presentation or after surgical intervention. To the best of our knowledge, this is the first reported case of a pancreatic Ewing's sarcoma presenting with concomitant venous tumor thrombosis.
Tumor vein thrombosis has been reported in less common pancreatic tumors such as intraductal papillary–mucinous carcinoma, pancreatic acinar cell adenocarcinoma, and pancreatic neuroendocrine tumors.18 It is important to distinguish portal vein tumor thrombosis from the more common fibrin thrombus since the presence of the former has reportedly been associated with a higher risk of liver metastasis and poorer clinical outcomes.19
Conclusion
Collectively, the reported cases of primary and metastatic Ewing's sarcoma of the pancreas further reinforce the imperative to include these rare tumors in the differential diagnosis of suspicious, indistinct pancreatic neoplasms. As previously reported by Finan et al., this case also illustrates the importance of associated pancreatitis as a risk factor for post-operative pancreatic fistula following laparoscopic distal pancreatic resections.19 Lastly, the phenomenon of tumor vein thrombosis should be carefully considered in this patient population when determining surgical intervention and oncological management of this rare disease.
References
Wick MR NO. Ectopic neural and neuroendocrine neoplasms. Semin Diagn Pathol. 2003 20(4):305–323.
Colovic RB GN, Micev MT, Matic SV, Atkinson HD, Latincic SM. Perigastric extraskeletal Ewing's sarcoma: a case report. World J Gastroenterol. 2009;15(2):245–247.
Jain S XR, Prieto VG, Lee P. Molecular classification of soft tissue sarcomas and its clinical applications. Int J Clin Exp Pathol. 2010;3(3):416–428.
François Bertucci JA, & Marc Giovannini. Pancreatic metastasis from osteosarcoma and Ewing sarcoma: literature review. Scandinavian Journal of Gastroenterology. 2012.
Bose P. MP, Gillies E., Holter J. Extraosseous Ewing's sarcoma of the pancreas. Int J Clin Oncol. 2012;17:399–406.
Welsch T MG, Aulmann S, Mueller SA, Buechler MW, Schmidt J, Kienle P. Huge primitive neuroectodermal tumor of the pancreas: report of a case and review of the literature. World J Gastroenterol. 2006;12(37):6070–6073.
Movahedi-Lankarani S. HRH, Westra, W.H., and Klimstra D.S. Primitive neuroectodermal tumors of the pancreas: a report of seven cases of a rare neoplasm. Am J Surg Pathol. 2002;26:1040–1047.
Bulchmann G, Schuster T., Haas, R.J., and Joppich I. Primitive neuroectodermal tumor of the pancreas. An extremely rare tumor. Case report and review of the literature. Klin Padiatr. 2000;212:185–188.
Takeuchi M, Kuwae, Y., Hamana, K., Oue K., Kubota A., Kawa K., Nakayama M. Primitive neuroectodermal tumor of the pancreas. Arch Histopathol. 2003;10:23–26.
Jing H LF, Chen L, Zhang T, and Zhao Y. Detection of recurrent pancreatic primitive neuroectodermal tumor by Tc-99m hydrazinonicotinyl-Tyr3-octreotide scan. Clin Nucl Med. 2011;36:54–55.
Perek S, Perek, A., Sarman, K., Tuzun H., and Buyukunal E. Primitive neuroectodermal tumor of the pancreas. A case report of an extremely rare tumor. Pancreatology. 2003;2:352–356.
Menon B.S. JE, Mohamed M. Pancreatic primitive neuroectodermal tumor associated with precocious puberty. Pediatr Blood Cancer. 2009;53:518–519.
Schutte W.P KPJ. Precocious puberty because of a pancreatic neuroecodermal tumor. J Pediatr Surg. 2006;41:1916–1918.
Lutteges J, Pierre, E., Zamboni, G., Lietz H., Kussmann J., Kloppel G. Malignant non-epithelial tumors of the pancreas. Pathologe. 1997;18:233–237.
Doi H IS, Hiraoka A, Ichiryu M, Nakahara H, Ochi H, Tanabe A, Kodama A, Hasebe A, Miyamoto Y, Ninomiya T, Horiike N, Takamura K, Kawasaki H, Kameoka C, Kan M, Doi S, Soga Y, Tamura H, Maeda T, Asaki A, Seno S, Iguchi H, Hasegawa T. Primitive neuroectodermal tumor of the pancreas. Intern Med. 2009;45(5):329–333.
Danner DB HR, Pitt HA, Hayashi R, Griffin CA, and Perlman EJ. Primitive neuroectodermal tumor arising in the pancreas. Modern Pathology. 1994;7(2):200–204.
Maxwell L. HA, Jackson C., et al. Uncommon presentation of rare disorder—duodenal ulcer secondary to invasive pancreatic primitive neuroectodermal tumor: case report and review of literature. J Pediatr Hematol Oncol. 2011;33(7):543–548.
Yoshito T OI, Hiroaki O, Hidetoshi E, Terumasa Y, Yo S, Kentaro K, Ko T, Shingo N, Isao M, Masayuki O, Masahiko Y, Shingi I. Intraductal papillary-mucinous carcinoma of the pancreas with tumor thrombus in the portal vein: a report of two cases. Hepato-Gastroeneterology. 2007;54:1585–1588.
Finan K.R. CEE, Kim E.J., Wesley M.M., Arnoletti P.J., Heslin M.J., Christein J.D. Laparoscopic and open distal pancreatectomy: a comparison of outcomes. Am Surg 2009;75(8):679–680.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reilly, C., Zenoni, S., Hasan, M.K. et al. Primary Pancreatic Ewing's Sarcoma with Portal Vein Tumor Thrombosis. J Gastrointest Surg 17, 1015–1019 (2013). https://doi.org/10.1007/s11605-012-2098-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2098-9