Abstract
Purpose
This study was undertaken to determine whether neoadjuvant radiotherapy is associated with an increased risk of anastomotic leak for rectal cancer patients undergoing restorative resection.
Methods
From 1980 to 2010, patients who underwent restorative resection for rectal cancer (tumors within 15 cm of anal verge) were identified from a prospective institutional database and grouped based on whether they received neoadjuvant radiotherapy (+RT) or not (−RT). The main outcome was anastomotic leak documented by imaging (contrast leak), intra-operative or clinical (signs of peritonitis) findings and confirmed by staff surgeon assessment. Using multivariate (MV) analysis risk factors for leak were identified, presented as OR (95 % CI).
Results
One thousand eight hundred sixty-two patients were included in the analysis, 28 % in the +RT group. Eighty-six percent of +RT patients received neoadjuvant chemoradiotherapy. The overall leak rate was 6.3 %, with no significant difference in +RT and −RT groups (8 % vs 5.7 %, p = 0.06). The +RT group had a lower mean age at surgery (58 vs 63 year, p < 0.001), more male (75 % vs 62 %, p < 0.001) and more ASA 3/4 (44 % vs 35 %, p < 0.001) patients, greater use of defunctioning ostomy (87 % vs 44 %, p < 0.001) and colo-anal anastomosis (77 % vs 34 %, p < 0.001). Mean tumor distance from the anal verge was lower in +RT group (6.6 vs 9.7 cm, p < 0.001). On MV analysis, male sex (OR 1.64 (1.03–2.62), p = 0.038), ASA 4 (OR 4.70 (2.07–10.7), p < 0.001), tumor distance from anal verge ≤ 5 cm (OR 2.49 (1.37–4.52), p = 0.003), and tumor size at surgery ≥ 4 cm (OR 1.75 (1.15–2.65), p = 0.009) were independently associated with leak. +RT was not independently associated with leak (OR 1.44 (0.85–2.46), p = 0.18), while defunctioning ostomy did not reduce leak occurrence (OR 0.75 (0.44–1.28), p = 0.29).
Conclusions
The findings suggest that neoadjuvant radiotherapy is not independently associated with an anastomotic leak for rectal cancer patients undergoing restorative resection and support a selective policy towards the use of a defunctioning ostomy on a case by case basis based on intra-operative judgment and consideration of tumor location, size, and patient characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Current consensus in the management of locally advanced rectal cancer advocates the use of a multi-modal approach to treatment, with pre-operative conventionally fractionated radiotherapy and concurrent chemotherapy1–3 (CRT) followed by high quality mesorectal excision (TME) surgery4 to achieve the lowest possible local recurrence rates. Anastomotic leak after rectal cancer surgery is one of the most important potential complications of anterior resection, with the consequent risk of early and late mortality, morbidity, and implications for maintenance of intestinal continuity and quality of life.5–8 Previous studies have identified risk factors for anastomotic leak such as male gender, malnutrition, pre-operative weight loss, steroid use, peri-operative transfusion, and importantly pelvic radiotherapy. Studies in experimental animals have demonstrated reduced colonic anastomotic integrity following the administration of high dose radiotherapy,9,10 and reduced blood flow to colorectal anastomoses.11 It is also recognized that leak rates after anterior resection are increased following the formation of low pelvic anastomoses.12–14
Defunctioning ileostomy is widely used in rectal cancer surgery,12,15,16 with the intention of ameliorating the consequences of anastomotic leak, should this occur. In a meta-analysis of 4 randomized studies, comprising a total of 358 patients, the presence of defunctioning stoma significantly reduced clinical anastomotic leak (i.e., need for intervention should leak occur) after rectal cancer surgery with an odds ratio of 0.32 [0.17, 0.59]. It should be noted that the rate of clinically relevant anastomotic leaks (up to 28 % in non-defunctioned patients) in the only large study included in the meta-analysis was substantially higher than that generally reported by large centers.12–14 This raises questions about the results of the meta-analysis potentially being skewed by the findings of the larger study. The meta-analysis also identified a benefit for stoma creation in terms of re-operation, but no benefit in terms of improved mortality was observed.17
Due to the risk of complications that can occur in the creation and closure of defunctioning stomas and the need for readmission,18–22 most units have adopted a selective approach to defunctioning anastomoses in anterior resections, with recommendations for the creation of a defunctioning stoma for anastomoses within 6 cm of the anal verge.16,23 Given the current emphasis on enhanced recovery, minimally invasive colorectal surgery24,25 and patients’ desire for cosmesis and stoma avoidance, it is necessary to re-examine the strategy of defunctioning rectal resections and the indications for defunctioning patients who receive multi-modal treatment for rectal cancer. As stated above, it is likely that more patients will now receive neoadjuvant treatment for rectal cancer; however, there is no clear consensus for the routine use of defunctioning stomas in these patients. While there is evidence to suggest that radiotherapy may reduce anastomotic integrity it is not clear whether radiotherapy is an independent risk factor for leak following rectal resection, and how radiotherapy interplays with other potential risk factors such as gender, site of lesion and patient age. The aim of this study is to investigate the risk of anastomotic leak in patients undergoing restorative rectal cancer resection in the presence of radiotherapy and to determine if the creation of a defunctioning ostomy protects against this potential risk.
Methods
All patients who underwent rectal cancer resection at the Cleveland Clinic Foundation from 1980 to 2010 were identified from the prospectively maintained Cleveland Clinic cancer database. Patients were grouped according to whether they received neoadjuvant radiotherapy (+RT) or no neoadjuvant radiotherapy (−RT), prior to rectal cancer resection. This study was approved by the Institutional Review Board and is HIPPA compliant.
Outcome Measurement
The primary outcome of interest was the occurrence of anastomotic leak following surgery. Anastomotic leak was defined by imaging, clinical findings, or operative findings, and therefore any type of leak (clinical and subclinical leak) was considered as the primary outcome. The following criteria were used to define leak: (a) the presence of anastomotic separation or pelvic abscess on post-operative imaging with contrast enema or CT scan, (b) postoperative physical signs of abdominal sepsis with a staff surgeon documenting a diagnosis of leak, or (c) intra-operative diagnosis made by a staff surgeon during abdominal exploration or examination under anesthesia.
Inclusion and Exclusion Criteria
Patients were included if they underwent transabdominal restorative rectal cancer resection with tumor site at 15 cm or less from the anal verge. All included patients underwent resection with curative intent. Patients with pathologic diagnoses other than adenocarcinoma were excluded. The usual practice at our institution is to perform a high ligation of the inferior mesenteric artery with the utilization of well vascularized colon (usually left) for the colorectal or colon-anal anastomosis. Splenic flexure mobilization is performed for additional colon length when indicated. Patients were excluded if they underwent transanal local excision of tumor, abdominoperineal excision of rectum or ileal pouch anal or rectal anastomosis. Patients undergoing resection for recurrent cancer were also excluded. A long-course neoadjuvant radiotherapy regime is used at the Cleveland Clinic, utilizing 45 Gy over 5 weeks, with surgery performed at 4–6 weeks after completion of treatment.
Study Variables
Data on patient demographics, ASA grade, height of tumor, clinical tumor stage as determined by a combination of clinical, endorectal ultrasound and/or magnetic resonance imaging, use of chemotherapy, use of adjuvant radiotherapy, type and level of anastomosis, type of stoma, and surgeon volume were collected. In the cases with a stapled anastomosis, an anastomosis located 3 cm or less from the anal verge was defined as a colo-anal anastomosis. Pathological tumor variables included size of tumor, TNM stage, and distal margin. Considering the duration of the study period over which patients underwent surgery, details pertaining to the quality of mesorectal excision were not uniformly available for all patients. Secondary endpoints were length of inpatient stay, 30-day mortality and type of intervention required for anastomotic leak (CT guided drainage, examination under anesthesia, exploratory laparotomy). Quality of life was assessed prospectively using the SF-36 questionnaire and fecal incontinence severity index (FISI).
Statistical Analysis
Statistical analysis was performed using R software (www.r-project.org). Categorical variables are summarized as frequencies and percentages. Quantitative variables are summarized as mean ± standard deviation. Tests for association between −RT and +RT groups and categorical variables were performed using the Chi-square method. For quantitative variables the Wilcoxon rank sum method was used. A p value <0.05 was accepted as statistically significant. Multivariate models were generated using the forward stepwise method, with a univariate entry cutoff of p = 0.05 for inclusion.
Results
From 1980 to 2010, a total of 1,862 patients underwent restorative rectal cancer resection and were included in the study. 1,338 (71.9 %) patients did not receive neoadjuvant radiotherapy (−RT group) and 524 (28.1 %) patients received neoadjuvant radiotherapy (+RT group). In the +RT group 448 (85.5 %) patients received neoadjuvant chemoradiotherapy. Five surgeons contributed >100 cases each, comprising 73 % of the sample. Baseline characteristics and details of anastomotic configuration in −RT and +RT groups stratified by the creation or otherwise of a defunctioning ostomy are given in Table 1. In the +RT group, there were significantly more males, patients were younger at the time of surgery, more patients had a lower third rectal cancer site and more patients had a colo-anal anastomosis (including straight, colopouch or coloplasty configuration). In the −RT group, a diverting colostomy was performed in 80 (6 %) patients and a diverting ileostomy in 514 (38.4 %). Post-operative (adjuvant) radiotherapy was given to 155 (11.5 %) of patients in the −RT group. In the +RT group, a diverting colostomy was performed in 25 (4.8 %) patients and a diverting ileostomy in 430 (82.1 %).
Four hundred and twenty-five patients in the cohort underwent surgery prior to 1989, 629 between 1990 and 1999 and 808 between 2000 and 2010. The cumulative occurrence of leak during these time periods was 7.3 %, 5.9 %, and 6.2 %, respectively (p = 0.64). In 1,623 patients, a stapled anastomosis was performed and in 118 patients a handsewn anastomosis with leak rates of 4.4 % and 4.3 %, respectively (p = 0.94). Overall, 118 (6.3 %) patients had an anastomotic leak, 76 (5.7 %) in the −RT group vs. 42 (8 %) in the +RT group (p = 0.06). Outcomes for the two groups are provided in Table 2. There was no statistically significant difference in occurrence of anastomotic leak between −RT and +RT groups when patients were subcategorized according to presence of diverting ostomy, tumor location, and colo-anal vs colorectal anastomosis. There was no significant difference in 30-day mortality in −RT vs +RT patients, however +RT patients did have a shorter length of inpatient stay. In the −RT group, 31 (5.2 %) of undiverted patients developed anastomotic leak, in the +RT group, 8 (11.6 %) of undiverted patients developed a leak. Table 3 describes the management of leaks in undiverted patients in −RT and +RT groups. The overall frequency of exploratory laparotomy for leak patients that were undiverted was 77.8 % in the −RT group and 37.5 % in the +RT group. Table 4 describes the management of leaks in diverted patients in −RT and +RT groups. The overall frequency of exploratory laparotomy for leak patients that were diverted was 12 % in the −RT group and 9.1 % in the +RT group.
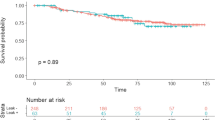
The 10-year local recurrence rates in the −RT group were 4.2 % in defunctioned and 6.4 % in non-defunctioned patients. In the +RT group, it was 5.1 % defunctioned and 4.8 % in non-defunctioned patients (p = 0.94). The risk of local recurrence was significantly increased in patients who sustained anastomotic leak; OR = 3.29 (1.71–6.32, p = 0.001). In +RT patients with a leak, the increased risk of local recurrence was greater; OR = 6.01 (2.16–16.76, p = 0.002) than in −RT patients with a leak; OR = 2.32 (0.96–5.62, p = 0.06). There was no statistical difference in distal margin between patients in the −RT vs +RT groups (1.16 ± 0.87 cm vs 1.00 ± 0.68 cm, p = 0.52) or in patients who sustained a leak vs those without a leak (1.10 ± 0.99 cm vs 1.08 ± 0.76 cm, p = 0.94).
Predictors of Anastomotic Leak
Univariate factors associated with anastomotic leak are presented in Table 5. Using forward stepwise inclusion, the following factors were identified as independent predictors of anastomotic leak (given as OR [95 % CI]): ASA grade 4 4.70 (2.07–10.7), p < 0.001; tumor in the lower third of the rectum 2.49 (1.37–4.52), p = 0.003; tumor size at surgery over 4 cm 1.75 (1.15–2.65), p = 0.009; and male gender 1.64 (1.03–2.62), p = 0.038. Neoadjuvant radiotherapy 1.44 (0.85–2.46), p = 0.18; pathologic T4 disease 0.60 (0.18–2.01), p = 0.4; M1 disease 1.54 (0.89–2.68), p = 0.13 were not independently associated with anastomotic leak. Creation of a diverting ostomy 0.75 (0.44–1.28), p = 0.29 was also not independently associated with a reduced risk of anastomotic leak.
Quality of Life and Bowel Function
Table 6 summarizes quality of life and bowel function in undiverted vs diverted patients in the −RT and +RT groups respectively. Questionnaires were returned at median 3.9 (1.9–4.9) years in −RT group and 2.9 (0.9–2.8) in the +RT group. There were no significant differences in the physical and mental SF-36 summary scores between undiverted and diverted patients in the −RT and +RT groups. In the −RT group, an increased nocturnal stool frequency and increased frequency of pad use was observed in diverted patients. In the +RT group, an increased frequency of major stool incontinence was observed in diverted patients
Discussion
In this large single institution series, we have analyzed the risk of anastomotic leak in patients undergoing restorative rectal cancer resection with curative intent. The objective of this study was to examine the effect of neoadjuvant radiotherapy on anastomotic leak rate in these patients. While there is a sound scientific basis for anticipating an increased anastomotic leak rate in patients receiving neoadjuvant radiotherapy, this finding has not been firmly established by clinical studies, with conflicting reports in the literature. In a large series, Enker and colleagues did not observe an increased leak rate in 150 patients undergoing low anterior resection with neoadjuvant radiotherapy.26 In a large randomized study, Sauer and colleagues also did not observe an increased postoperative leak rate in patients receiving neoadjuvant vs adjuvant chemoradiotherapy who underwent sphincter preserving surgery.1 However other reports containing smaller numbers (n = 37–50) of patients receiving neoadjuvant radiotherapy have described an increased risk of leak in these patients.27,28
The findings of the current study therefore agree with the larger studies mentioned, as we have also not been able to demonstrate an association with neoadjuvant radiotherapy and leak. Whilst there was a very close statistical trend towards increased crude leak rate in +RT patients, on multivariate analysis radiotherapy was not a predictor for anastomotic leak. Furthermore in subgroup analysis, neoadjuvant radiotherapy did not significantly increase leak rate after low (colo-anal) anastomosis, after surgery for lower third rectal cancer or in patients who were not diverted. In addition we did not observe an increased requirement for exploratory laparotomy in +RT patients who developed a leak, although the pelvic abscess rather than peritonitis in this group may be due to increased frequency of low defunctioned anastomoses. The use of radiotherapy did not appear to adversely affect the management of patients who developed a leak and is unlikely to influence the degree of sepsis in these patients. As stated, it is the absence of diversion in patients who sustain a leak that increases the necessity for major surgery.17 In diverted +RT patients that did have a leak, we observed a much lower requirement for major abdominal surgery (9.1 %) compared with undiverted patients (37.5 %). The requirement of exploratory laparotomy for undiverted −RT patients was however even higher than those who were diverted (77.8 vs 12 %).
The current study does have limitations, in that it retrospectively analyzes data in pre-selected patient groups, with the decision to divert left to the operating surgeon, and therefore only 13.4 % of patients in the +RT group were undiverted. A lower threshold for the diversion of +RT patients may also have been responsible for the higher need for exploratory laparotomy for the −RT patients who were not diverted and suffered a leak. Ideally, a prospective randomized study of diversion in +RT patients would provide a sound scientific method of determining the role of diversion in this setting. However, it would be inadvisable to conduct such a study as +RT patients frequently possess adverse tumor characteristics which would influence the decision to divert. In view of the fact that the vast majority of +RT patients in our tumor registry were diverted, we chose to include all anastomotic leaks as our principal outcome measure, rather than the rate of symptomatic or clinically relevant leak that has been reported in studies investigating the role of diverting ileostomy.29,30 A case-matched design for factors found to be significant between the +RT and −RT groups was also considered. However, the large numbers of variables did not allow for sufficient numbers in the groups to allow for an adequate comparison. We hence conducted a multivariable analysis adjusting for the creation of diverting ostomy so as to identify predictors of outcome in this large cohort as an alternative design. Omission of diverting ostomy and use of neoadjuvant radiotherapy were not identified as predictors of leak in this study.
We have previously described the morbidity associated with defunctioning loop ileostomy in patients with ileo-anal pouch31 and the published morbidity of loop ileostomy creation and closure in studies on unselected patients ranges from 18 % to 33 %, with mortality ranging from 0 % to 2.5 %.32–35 In colorectal cancer patients the published morbidity associated with loop ileostomy is 19.2 % and mortality is 1.7 %.36 In this study, we also observed an adverse association between fecal diversion and bowel function after restorative rectal resection for specific variables. Pad usage was increased in diverted patients in the −RT group and stool incontinence was increased in diverted +RT patients. While continence after rectal cancer surgery is dependent on multiple factors, this may be related to the fact that patients with more adverse factors and lower anastomoses were selected out for diversion. We were not able to conclusively demonstrate the effect of radiotherapy on bowel function after restorative surgery, as 11.5 % of −RT patients did receive adjuvant radiotherapy.
Consistent with previous reports,13,28 including one from our unit,14 height of tumor (i.e., in the lower rectum) is a central factor in the decision to divert. We have also identified ASA grade 4, tumor size at surgery over 4 cm and male gender as predictors for anastomotic leak. Therefore, the decision to divert in restorative rectal cancer surgery should be made on a case by case basis taking into account patient and tumor characteristics. Our data support the use of a selective policy of diversion based on these factors, rather than a blanket approach towards patients receiving multimodal treatment for rectal cancer.
References
Sauer R, Becker H, Hohenberger W, Rodel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004 Oct 21;351(17):1731–1740.
Roh MS, Colangelo LH, O’Connell MJ, Yothers G, Deutsch M, Allegra CJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol 2009 Nov 1;27(31):5124–5130.
Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, et al. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med 2006 Sep 14;355(11):1114–1123.
MacFarlane JK, Ryall RD, Heald RJ. Mesorectal excision for rectal cancer. Lancet 1993 Feb 20;341(8843):457–460.
Fielding LP, Stewart-Brown S, Blesovsky L, Kearney G. Anastomotic integrity after operations for large-bowel cancer: a multicentre study. Br Med J 1980 Aug 9;281(6237):411–414.
Fujita S, Teramoto T, Watanabe M, Kodaira S, Kitajima M. Anastomotic leakage after colorectal cancer surgery: a risk factor for recurrence and poor prognosis. Jpn J Clin Oncol 1993 Oct;23(5):299–302.
McArdle CS, Hole D. Impact of variability among surgeons on postoperative morbidity and mortality and ultimate survival. BMJ 1991 Jun 22;302(6791):1501–1505.
Rullier E, Laurent C, Garrelon JL, Michel P, Saric J, Parneix M. Risk factors for anastomotic leakage after resection of rectal cancer. Br J Surg 1998 Mar;85(3):355–358.
Bedirli A, Kerem M, Karahacioglu E, Ofluoglu E, Yilmaz TU, Pasaoglu H, et al. Effects of two conventional preoperative radiation schedules on anastomotic healing in the rat colon. Eur Surg Res 2007;39(3):141–147.
Kuzu MA, Kuzu I, Koksoy C, Akyol FH, Uzal D, Kale IT, et al. Histological evaluation of colonic anastomotic healing in the rat following preoperative 5-fluorouracil, fractionated irradiation, and combined treatment. Int J Colorectal Dis 1998;13(5–6):235–240.
Milsom JW, Senagore A, Walshaw RK, Mostosky UV, Wang P, Johnson W, et al. Preoperative radiation therapy produces an early and persistent reduction in colorectal anastomotic blood flow. J Surg Res 1992 Nov;53(5):464–469.
Law WI, Chu KW, Ho JW, Chan CW. Risk factors for anastomotic leakage after low anterior resection with total mesorectal excision. Am J Surg 2000 Feb;179(2):92–96.
Karanjia ND, Corder AP, Bearn P, Heald RJ. Leakage from stapled low anastomosis after total mesorectal excision for carcinoma of the rectum. Br J Surg 1994 Aug;81(8):1224–1226.
Vignali A, Fazio VW, Lavery IC, Milsom JW, Church JM, Hull TL, et al. Factors associated with the occurrence of leaks in stapled rectal anastomoses: a review of 1,014 patients. J Am Coll Surg 1997 Aug;185(2):105–113.
Marusch F, Koch A, Schmidt U, Geibetaler S, Dralle H, Saeger HD, et al. Value of a protective stoma in low anterior resections for rectal cancer. Dis Colon Rectum 2002 Sep;45(9):1164–1171.
Karanjia ND, Corder AP, Holdsworth PJ, Heald RJ. Risk of peritonitis and fatal septicaemia and the need to defunction the low anastomosis. Br J Surg 1991 Feb;78(2):196–198.
Huser N, Michalski CW, Erkan M, Schuster T, Rosenberg R, Kleeff J, et al. Systematic review and meta-analysis of the role of defunctioning stoma in low rectal cancer surgery. Ann Surg 2008 Jul;248(1):52–60.
Baraza W, Wild J, Barber W, Brown S. Postoperative management after loop ileostomy closure: are we keeping patients in hospital too long? Ann R Coll Surg Engl 2010 Jan;92(1):51–55.
Chude GG, Rayate NV, Patris V, Koshariya M, Jagad R, Kawamoto J, et al. Defunctioning loop ileostomy with low anterior resection for distal rectal cancer: should we make an ileostomy as a routine procedure? A prospective randomized study. Hepatogastroenterology 2008 Sep-Oct;55(86–87):1562–1567.
Giannakopoulos GF, Veenhof AA, van der Peet DL, Sietses C, Meijerink WJ, Cuesta MA. Morbidity and complications of protective loop ileostomy. Colorectal Dis 2009 Jul;11(6):609–612.
van de Pavoordt HD, Fazio VW, Jagelman DG, Lavery IC, Weakley FL. The outcome of loop ileostomy closure in 293 cases. Int J Colorectal Dis 1987 Nov;2(4):214–217.
Williams LA, Sagar PM, Finan PJ, Burke D. The outcome of loop ileostomy closure: a prospective study. Colorectal Dis 2008 Jun;10(5):460–464.
Pakkastie TE, Luukkonen PE, Jarvinen HJ. Anastomotic leakage after anterior resection of the rectum. Eur J Surg 1994 May;160(5):293–7; discussion 299–300.
da Luz Moreira A, Mor I, Geisler DP, Remzi FH, Kiran RP. Laparoscopic resection for rectal cancer: a case-matched study. Surg Endosc 2010 Jun 29.
Khaikin M, Bashankaev B, Person B, Cera S, Sands D, Weiss E, et al. Laparoscopic versus open proctectomy for rectal cancer: patients’ outcome and oncologic adequacy. Surg Laparosc Endosc Percutan Tech 2009 Apr;19(2):118–122.
Enker WE, Merchant N, Cohen AM, Lanouette NM, Swallow C, Guillem J, et al. Safety and efficacy of low anterior resection for rectal cancer: 681 consecutive cases from a specialty service. Ann Surg 1999 Oct;230(4):544–52; discussion 552–4.
Lyall A, Mc Adam TK, Townend J, Loudon MA. Factors affecting anastomotic complications following anterior resection in rectal cancer. Colorectal Dis 2007 Nov;9(9):801–807.
Eriksen MT, Wibe A, Norstein J, Haffner J, Wiig JN, Norwegian Rectal Cancer Group. Anastomotic leakage following routine mesorectal excision for rectal cancer in a national cohort of patients. Colorectal Dis 2005 Jan;7(1):51–57.
Matthiessen P, Hallbook O, Rutegard J, Simert G, Sjodahl R. Defunctioning stoma reduces symptomatic anastomotic leakage after low anterior resection of the rectum for cancer: a randomized multicenter trial. Ann Surg 2007 Aug;246(2):207–214.
Gastinger I, Marusch F, Steinert R, Wolff S, Koeckerling F, Lippert H, et al. Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg 2005 Sep;92(9):1137–1142.
Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, et al. Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 2005 Feb;48(2):243–250.
Bakx R, Busch OR, Bemelman WA, Veldink GJ, Slors JF, van Lanschot JJ. Morbidity of temporary loop ileostomies. Dig Surg 2004;21(4):277–281.
Phang PT, Hain JM, Perez-Ramirez JJ, Madoff RD, Gemlo BT. Techniques and complications of ileostomy takedown. Am J Surg 1999 Jun;177(6):463–466.
Garcia-Botello SA, Garcia-Armengol J, Garcia-Granero E, Espi A, Juan C, Lopez-Mozos F, et al. A prospective audit of the complications of loop ileostomy construction and takedown. Dig Surg 2004;21(5–6):440–446.
Saha AK, Tapping CR, Foley GT, Baker RP, Sagar PM, Burke DA, et al. Morbidity and mortality after closure of loop ileostomy. Colorectal Dis 2009 Oct;11(8):866–871.
Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum 2006 Jul;49(7):1011–1017.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nisar, P.J., Lavery, I.C. & Kiran, R.P. Influence of Neoadjuvant Radiotherapy on Anastomotic Leak After Restorative Resection for Rectal Cancer. J Gastrointest Surg 16, 1750–1757 (2012). https://doi.org/10.1007/s11605-012-1936-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-1936-0