Abstract
Objectives
Endoscopy is a minimally invasive technique for the drainage of peripancreatic fluid collections. This study evaluated the clinical outcomes and predictors of treatment success in consecutive patients undergoing endoscopic transmural drainage of peripancreatic fluid collections.
Methods
This is a retrospective study of patients who underwent endoscopic drainage of peripancreatic fluid collections over 7 years. Prior to drainage, an ERCP was attempted for stent placement in all patients with a pancreatic duct leak. Drainages were performed using conventional endoscopy or endoscopic ultrasound. Transmural stents and/or drainage catheters were deployed and endoscopic necrosectomy was undertaken when required. Data on clinical outcomes and complications were collected prospectively.
Results
A total of 211 patients underwent drainage of peripancreatic fluid collections that was classified as pseudocyst in 45%, abscess in 28%, and necrosis in 27%. Mean diameter of the fluid collection was 100.6 mm, and 34.5% of patients had pancreatic duct stent placement. Median duration of follow-up was 356 days. Treatment success was 85.3% and was higher for pseudocyst and abscess compared to necrosis (93.5% vs. 63.2%, p < 0.0001). Complications were encountered in 17 patients (8.5%) and was higher for drainage of necrosis than pseudocyst or abscess (15.8% vs. 5.2%, p = 0.02). Treatment success was more likely for patients with pseudocyst or abscess than necrosis (adjusted OR = 7.6, 95% CI [2.9, 20.1], p < 0.0001) when adjusted for serum albumin and white cell count, type of endoscopic modality or accessory used, pancreatic duct stenting, luminal compression, size and location of fluid collection.
Conclusions
Endoscopic therapy is a highly effective technique for the management of patients with non-necrotic peripancreatic fluid collections.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Peripancreatic fluid collections (PFCs) can arise as a result of acute or chronic pancreatitis, trauma, malignancy, or surgery.1,2 Drainage of these PFCs may be necessary as they can result in abdominal pain, gastric outlet or biliary obstruction, infection, and rarely rupture.3,4
Endoscopic drainage of PFCs is a clinically effective and safe technique that was first reported in the late 1980s.5,6 This method, with2,7–11 or without4,12–17 the concomitant use of endoscopic ultrasound (EUS), entails the creation of a fistulous tract between the PFC and the gastrointestinal lumen. When compared to the traditional surgical approach, not only are the clinical outcomes of endoscopic drainage comparable, but is also more economical and is associated with a shorter length of hospital stay.18,19 Therefore, endoscopy is increasingly being regarded as a minimally invasive alternative to surgery for the management of PFCs.
While several studies have reported on the endoscopic outcomes of PFC drainages, they involved multiple operators, varying techniques, and a small sample size. In the two largest series published on endoscopic management of PFCs that included 113 and 116 patients,2,12, respectively, not all subjects underwent transmural drainage as some were managed with only transpapillary pancreatic duct stent placement. In this study, we evaluate the clinical outcomes of endoscopy and determine the predictors of treatment success in 211 consecutive patients who underwent endoscopic transmural drainage of PFCs at a single center using a standardized technique.
Methods
Patients
This study was conducted by retrospective analysis of prospectively collected data on consecutive patients who underwent endoscopic transmural drainage of PFCs between January 2003 and December 2010. Included in the study were patients aged more than 19 years with symptomatic PFCs measuring 6 cm or greater in size that was treated by endoscopic transmural drainage. Excluded were patients who underwent only an endoscopic retrograde cholangiopancreatography (ERCP) for transpapillary pancreatic duct stent placement, PFCs that were less than 4 weeks old, or were located more than 1.5 cm from the EUS transducer. Some patients in this study had been included previously in a pilot trial that evaluated the technical outcomes of endoscopic drainage.11
Informed procedural consents were obtained from all patients prior to undergoing endoscopic transmural drainage. This study received approval from the University of Alabama Medical Center Institutional Review Board.
Protocol for Peripancreatic Fluid Collection Drainage
Prior to drainage, all patients underwent a contrast-enhanced computed tomography (CT) at our institution or already had a CT of suitable diagnostic quality at an outside institution within 1 week of planned intervention. Prior to drainage, inpatients were given 400 mg intravenous ciprofloxacin, which was continued for 48 h or until discharge, while outpatients were given 500 mg oral ciprofloxacin to be taken the night before and then continued twice daily for 5 days following drainage. All patients first underwent a routine ERCP prior to the drainage of PFCs. A pancreatogram was attempted to define the communication between the pancreatic duct and the pancreatic fluid collection, and in cases where the pancreatic duct was narrowed or obliterated, a transpapillary bridging stent was inserted, as long as the proximal duct could be reached with a guidewire. An ERCP was not performed in patients with a gastric outlet obstruction or with disconnected duct syndrome diagnosed by magnetic resonance cholangiopancreatography (MRCP).
Following ERCP, the duodenoscope was used to search for a luminal compression in the stomach and the duodenum. Once a luminal compression was found, transmural drainage of the PFC was undertaken by puncturing the gastric or the duodenal wall. If no luminal compression was identified or if the patient was at high risk for bleeding, an EUS-guided drainage was performed in the same endoscopic session.
Technique of Conventional Transmural Drainage (CTD)
All PFCs were drained using a triple-lumen needle knife catheter (Microknife XL; Microvasive Endoscopy, Boston Scienctific Corp, Natick, MA, USA) to create a cyst-enterostomy fistula. After access to the PFC, dilation of the fistula was performed by using an 8- to 15-mm biliary balloon dilator, and two 10Fr double-pigtail endoprostheses were placed.
Technique of EUS-guided Drainage
For EUS-guided drainage, a 19-gauge needle (EUSN-19-T; Cook Endoscopy, Winston-Salem, NC, USA) was introduced into the PFC. Before puncture, the cyst was evaluated by the EUS, and a color Doppler ultrasound was used to identify the regional vessels. A 0.035-inch guidewire was then introduced through the needle and coiled within the peripancreatic fluid collection under fluoroscopic guidance. The tract was sequentially dilated by first passing a 5Fr ERCP cannula and then an 8- to 15-mm biliary balloon dilator. Two to three 7Fr double-pigtail endoprostheses were then placed.
Technique for Drainage of Pancreatic Abscess/Necrosis
In patients with pancreatic abscess or necrosis, a 7Fr nasocystic catheter was placed in addition to the stents to facilitate periodic flushing with 200 cc of nomal saline and vigorous aspiration every 4 h. Patients were placed in both the right and left lateral decubitus positions at the time of flushing to ensure thorough evacuation of the pancreatic abscess or necrotic tissue. In patients with pancreatic necrosis, if the size of the PFC was 15 cm or more, two to three transmural tracts were created, and multiple 7Fr stents were placed in each track. Also, a nasocystic drainage catheter was placed in one tract to facilitate flushing with normal saline and for aspiration of the necrotic contents.
Technique for Drainage of Multiple PFCs
In patients with pseudocysts, only the largest PFC was drained at index procedure. PFCs at other locations were drained subsequently within 48–72 h if the symptoms were persistent. In patients with pancreatic abscesses or necroses, all PFCs were drained at the index procedure. EUS guidance was used to perform transmural drainage in patients with multiple PFCs due to difficulty with identification of individual PFCs by conventional endoscopy.
Follow-up
All patients who underwent transmural drainage of pseudocyts or abscess had a repeat contrast-enhanced CT and an outpatient clinic follow-up that included a history and physical examination at 8 weeks post-drainage. In patients with treatment success, all stents and feeding tubes were removed at this time. In patients with partial resolution of the fluid collection, they underwent a repeat endoscopy for placement of more transmural stents and were reassessed at 1 month. If clinical success was achieved at that time, all stents and tubes were removed. However, in patients with failed drainage, either the transmural drainage was re-attempted or they were referred for surgical management. In patients with necrosis who were intolerant of oral intake, a nasojejunal or gastrojejunostomy feeding tube was placed by interventional radiology for enteral nutrition. Also, at 72–96 h, a repeat CT of the abdomen was obtained in all patients with necrosis. If there was a decrease in size of the necrotic collection by >50% in association with improvement in patient symptoms and there was no necrotic fluid on aspiration of the drainage catheter, the nasocystic drain was removed. If symptoms were persistent, following interdisciplinary consultation with pancreatic surgeons, additional transmural drainage by placement of stents, endoscopic necrosectomy, or surgery was undertaken. The interval between endoscopy sessions and follow-up CT scans were not standardized and was dependent on the patient's clinical progress. A follow-up CT was obtained 8 weeks following patient discharge from the hospital. If the necrotic collection had resolved and the patients were symptomatically better, the transmural stents were retrieved by endoscopy. Patients with a persistent necrotic collection underwent surgery. For patients with a disconnected duct syndrome on ERCP or MRCP, the transmural stents were left in place indefinitely.
By protocol, we attempted to contact all patients by telephone at 6-month intervals for 18 months during which they were queried about the need for subsequent interventions for any pancreatitis-related complaints.
Definitions
Types of PFCs
This was determined by the radiologist from examination of the CT images and followed the definitions outlined in the Atlanta Classification.20
Treatment Success
Treatment success was defined as the complete resolution or a decrease in the size of the PFC to ≤2cm on CT, accompanied by the resolution of symptoms at 8 weeks follow-up.
Treatment Failure
This was defined as persistence or worsening of symptoms occurring in association with PFCs that have increased in size or remaining greater than 2 cm in size on follow-up CT at 8 weeks post-drainage or requiring surgery for definitive treatment.
Outcome Measures
The primary outcome measure was to evaluate the rate of treatment success for endoscopic drainage of PFCs. The secondary outcome measure was to identify predictors of treatment success for the endoscopic approach.
Statistical Analysis
The data analysis was conducted using the SAS (version 9.1 Cary, NC, USA) statistical software. Patient characteristics related to transmural drainage of PFCs constituted continuous variables such as age, serum albumin level, and white cell count that were reported in terms of their medians (interquartile range). Categorical variables such as gender, etiology, and type of therapy were reported in terms of their frequency counts and proportions. Similar measures were adopted for reporting characteristics of PFCs and technical details of endotherapy. The abscess and pseduocyst groups were combined to form one group, and a nonparametric two-sample Wilcoxon rank-sum test was used to compare the continuous variables in this group with the necrosis group. The frequencies of the categorical variables in these two groups were compared using a chi-square test. The technical and clinical outcomes in these groups were also compared using a two-sample Wilcoxon rank-sum test, and a Fisher's exact test was deployed in cases where sample size was considered to be small. Multiple logistic regression was used to evaluate the predictors of treatment success at endoscopy and results obtained were reported by using adjusted odds ratios (OR) and their corresponding 95% confidence intervals (CIs) and p values. All tests were conducted at the 5% level of significance.
Results
Patient and PFC Characteristics
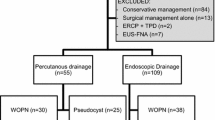
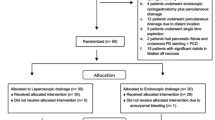
Over the investigation period, of 231 patients referred, a total of 211 subjects underwent endoscopic transmural drainage of PFCs that comprised 95 pseudocysts (acute 23, chronic 72), 59 abscesses, and 57 necrosis. Reasons for not performing transmural drainage in 20 patients were establishment of an alternate diagnosis of mucinous cystic neoplasm by EUS in 6, the PFC was determined at EUS to be less than 6 cm in size in 9, and was beyond the reach of the echoendoscope in 5 patients. The median age of the 211 patients was 52 years; 61% were men, and alcohol was the most common etiology (34%) of pancreatitis (Table 1). While there was no difference in patient age, gender, etiology of pancreatitis, or prior interventions between the patient cohorts, patients with necrosis were more hypoalbuminemic and had elevated white cell count than those with pseudocyst or abscess (Table 1). The median size of the PFCs was 90 mm (interquartile range 70–120 mm) with the diameter of necrotic collections being significantly larger than pseudocysts or abscesses (Table 2). The majority of PFCs (58.7%) were located in the body followed by tail (22.7%) and head (18.6%) of the pancreas, and 23 patients (10.9%) had multiple PFCs.
Technical Outcomes
Transpapillary pancreatic duct stents bridging the leak was successfully deployed in 72 (34.1%) patients. Placement of pancreatic duct stents was significantly more successful in patients with pseudocysts and abscesses compared to necrosis (40.2% vs. 17.5%, p = 0.002). Reasons for not placing a pancreatic duct stent in 92 of 154 patients with pseudocyst or abscess were a normal pancreatogram in 41 patients, failed cannulation in 13, post-surgical altered anatomy in 7, gastric outlet obstruction in 11, pancreatic duct stricture or stone in 5, and a disconnected duct syndrome in 15 patients. Reasons for not placing a pancreatic duct stent in 47 of 57 patients with necrosis were a disconnected duct syndrome in 31 patients, gastric outlet obstruction in 6, failed cannulation due to pancreas divisum or ansa loop in 4, normal pancreatogram in 4, and pancreatic duct stricture that precluded stent placement in 2.
Most PFC drainages were undertaken via the trans-gastric route (81.6%), followed by the trans-duodenal (13.2%), trans-esophageal (4.2%), and trans-jejunal routes (1%). PFCs were drained under EUS guidance in 150 patients (71.2%) and by CTD in 61 (28.8%). A definitive luminal compression was evident at endoscopy in only 107 patients (50.7%) and was significantly more likely to be present in patients with necrosis than pseudocyst or abscess (63.2% vs. 41.6%, p = 0.02). Of the 23 patients with multiple PFCs, 11 underwent EUS-guided drainage of more than one PFC. In 12 others, following EUS-guided drainage of the largest PFC, other PFCs were managed by percutaneous drainage (n = 9) or by conservative measures (n = 3). Reasons for not performing concomitant endoscopic drainage in these 12 patients were the presence of intervening vasculature in 3, fluid collection located within the splenic capsule in 4, and location of the PFC in the deep pelvis in 6 patients. While transmural stents were deployed in all patients, drainage catheters were more often placed in patients with necrosis than pseudocysts or abscesses (5.1% vs. 82.4%, p < 0.0001). Of the 57 patients with necrotic collections, 12 had PFCs that measured more than 150 mm in diameter. In these 12 patients, multiple transmural tracts were created with placement of a nasocystic catheter in one tract and multiple 7Fr stents in others. The remaining 35 patients with necrosis were treated with a nasocystic drainage catheter and multiple stents, all placed in a single transmural tract.
Treatment Outcomes
The overall treatment success was 85.3% and were higher for pseudocyst and abscess compared to necrosis (93.5% vs. 63.2%, p < 0.0001) (Table 3). Twenty-four of 95 patients (25.2%) with pseudocysts had acute collections, and there was no difference in treatment outcomes between patients with acute or chronic pseudocysts. Reasons for treatment failure in 10 of 154 (6.5%) patients with pseudocyst or abscess were perforation in 2 patients, infection in 2, persistence of the PFC in 5, and death due to delayed bleeding in 1 patient. Nine of these ten patients underwent surgery with good clinical outcomes. Reasons for treatment failure in 21 of 57 patients (36.8%) with necrosis were persistence of PFC in 15, post-procedural infection in 5, and perforation in 1 patient. While two patients died of multi-organ failure (not procedure-related), 19 underwent surgery with good clinical outcomes in 17; 2 patients died of post-surgical complications. Of the 36 patients with necrosis who had successful treatment outcomes, 4 required endoscopic necrosectomy, as transmural drainage alone was ineffective. Of the 12 patients with necrotic collections that measured more than 150 mm in diameter who were treated by creation of multiple transmural tracts, treatment was successful in 11 patients; 1 patient required endoscopic necrosectomy due to persistence of necrosis and had good clinical outcomes.
The median number of re-interventions for patients with necrosis was significantly more than for patients with pseudocyst or abscess (Table 3). While only 16 of 154 (10.3%) patients with pseudocyst or abscess required more than one intervention, 18 of 57 (31.6%) patients with necrosis required re-interventions. The median duration of post-procedure hospital stay was significantly longer for patients with necrosis than for those with pseudocyst or abscess (5 vs. 2 days, p < 0.0001). Of the 180 patients with pancreatic pseudocysts or abscesses who had successful treatment outcomes at a median follow-up of 367 days (IQR, 136–545), 9 (5%) patients developed recurrence of PFCs that was managed by endoscopic drainage in 5, percutaneous drainage in 3, and surgery in 1. Nineteen patients were lost to long-term follow-up. Three other patients with persistent pain, but no recurrence of PFC had pancreatic duct strictures on ERCP that was managed by transpapillary pancreatic duct stent placement. One other patient with persistent pain underwent total pancreatectomy with auto islet transplantation. Of the 36 patients with necrosis who had successful clinical outcomes at a median follow-up of 345 days (IQR, 120–511), 32 patients were doing well, 2 experienced recurrent pancreatitis, and 2 were lost to follow-up. Currently, 62 patients in our database are on long-term follow-up.
While the double pig-tail transmural stents were removed at follow-up endoscopy in all patients with treatment success and an intact main pancreatic duct, they were left permanently in place in 50 patients with a disconnected duct syndrome or main pancreatic duct stricture/stone that was not amenable for pancreatic endotherapy.
Procedural Complications
Complications were encountered in 17 patients (8.5%) that included perforation in 3, bleeding in 3, infection in 7, stent migration in 3, and death in 1 patient. The rate of complications was higher for drainage of necrosis than pseudocyst or abscess (15.8% vs. 5.2%, p = 0.02) .Of the three perforations, two were encountered in patients with pseudocysts and in one with necrosis. All three patients underwent surgery with successful repair of the perforation. Bleeding was encountered in two patients with pseudocysts and one with necrosis. Two cases required embolization with interventional radiology, and the other was managed conservatively. Five patients with necrosis and two with pseudocyst developed post-procedural infection that was managed with surgical debridement in three patients and by placement of additional transmural stents in four. In two patients with pancreatic necrosis and a disconnected duct syndrome, the transmural stents migrated causing a small bowel obstruction. While one patient underwent surgery, the stents migrated spontaneously with conservative therapy in another. In one patient with a pseudocyst, the stent migrated into the PFC and was removed using a snare. One patient died due to delayed bleeding following conventional transmural drainage of a pseudocyst. Autopsy revealed bleeding within the pseudocyst in this patient.
Predictors of Treatment Success
Multivariable logistic regression was performed to identify predictors of treatment success for endoscopic drainage (Table 4). Demographic, technical, and clinical factors of statistical significance were included in the model. The factors included were serum albumin and white cell count, type of PFC (pseudocyst and abscess versus necrosis), location of PFC (head vs. body and tail of pancreas), PFC size (<90 vs. >90 mm), presence or absence of luminal compression at endoscopy and type of endoscopic modality (EUS vs. CTD), and accessory (stents and drainage catheters vs. only stents) used for performing transmural drainage. Only the type of PFC remained significant with pseudocysts and abscesses having better treatment outcomes at endoscopy (adjusted OR = 7.6, 95% CI [2.9, 20.1], p < 0.0001) even after adjusting for all other factors in the model.
Discussion
In this study that encompassed a large cohort of patients who underwent endoscopic transmural drainage of PFCs, treatment outcomes were superior for patients with non-necrotic collections. Due to differences in the underlying pathology of various PFCs, differences in treatment outcomes are not unanticipated. In a study by Baron et al. of 113 patients,12 PFC resolution was significantly better for patients with chronic pseudocysts (92%) than acute pseudocysts (74%), or necrosis (72%). In another study of 116 patients by Hookey et al.,2 the treatment success rate for acute pseudocysts, chronic pseudocysts, abscess, and necrosis were 96.7%, 95.3%, 93%, 100%, and 25%, respectively. Similar to both reports, our treatment outcomes were better for patients with pseudocysts and abscesses.2,12 The difference in treatment outcomes for pancreatic necrosis between our study and others may be due to variation in timing of the interventions and the technique adopted.2,12 While the mean time to intervention in our necrosis cohort was 5 weeks, it was 3.2 and 7.2 weeks, respectively, in the other two reports.2,12 Additionally, the technique adopted for drainage of necrosis in our study was different: rather than using an 8-mm balloon, we used a 15-mm radial expansion balloon for dilating the transmural tract. Also, when the necrotic collections were 150 mm or larger in size, we created multiple transmural tracts for facilitating better drainage of the necrotic contents. When a subgroup analysis was performed, 11 of 12 patients treated with multiple tracts had treatment success compared to 25 of 45 patients treated by conventional drainage technique (91.6% vs. 55.5%, p = 0.02). Given these promising clinical outcomes, our current approach is to create multiple drainage tracts for patients with large necrotic collections. Four patients with necrosis who failed initial transmural drainage subsequently underwent endoscopic necrosectomy with good clinical outcomes. Two of these four patients had suffered an acute coronary event, and two others had severe obstructive lung disease. Three of these four patients required two sessions, and one required three sessions of necrosectomy. In a recent randomized trial that compared step-up approach and surgery for the management of pancreatic necrosis, patients treated by step-up approach had fewer complications and better clinical outcomes than those managed by surgical debridement.21 Also, 35% of patients randomized to step-up approach did not require necrosectomy and were managed successfully only by percutaneous drainage. This emphasizes our study findings that better drainage of the necrotic cavity may preclude the need for more invasive interventions in a subset of patients. Moreover, an initial attempt at endoscopic drainage did not preclude subsequent surgery in any patient in this series. As endoscopic necrosectomy is resource consuming, requires multiple sessions, is of prolonged duration, and associated with a mortality rate of nearly 10%, our approach is to operate on patients who fail transmural drainage unless they are too sick to undergo surgery.22 A major limitation of endoscopic necrosectomy is the lack of dedicated accessories to remove the necrotic material efficiently. Other authors have reported successful outcomes by using percutaneous drainage catheters for long-term flushing combined with endoscopic internal drainage of the necrotic cavity.23 Placement of percutaneous drainage catheters may lead to fistula formation when a PFC communicates with the main pancreatic duct.24 Also, these external catheters predispose to infection, cause patient discomfort, dislodge frequently, mandate prolonged hospital stay, and very often require other adjunctive treatment measures.25
The rate of PFC recurrence in this study was only 5% which is less than the 16% reported by other series.2,12 While there was no difference in the rate of recurrence between the PFC cohorts in our study, Baron et al. reported a recurrence rate of 29% for necrotic collections versus only 9% for pseudocysts.12 This difference may be due to the short duration of patient follow-up in this study (median 356 days). Another reason could be technique-related: Fifty-three of 211 (25.1%) patients in this study had a disconnected duct syndrome or main pancreatic stones or strictures that precluded pancreatic duct stent placement. In a majority of these patients, the transluminal stents were left in place indefinitely. We believe that these stents act as a conduit and facilitate drainage of pancreatic secretion from the disconnected gland. In a randomized trial that compared removal versus non-removal of transmural stents, the rate of PFC recurrence following stent removal was significantly higher.26 One third of patients in that study had spontaneous stent migration on long-term follow-up. It is likely that PFC resolution leads to eventual adherence of the walls of the cavity, which in turn leads to gradual migration of the stent toward the GI lumen. On the contrary, stent retrieval occurring before complete collapse of the cavity might lead to PFC recurrence, particularly if a communication exists between the cavity and the pancreatic duct. Therefore, the duration of stent placement may be more important than whether the stents are still present or retrieved after an adequate stent placement period. It is logical to assume that a majority of plastic stents occlude within a few weeks after placement and most drainage occurs along the sides rather than the lumen of the stent. The rate of procedural complications in this study was 8.5% which is similar to the 11% reported by Hookey et al.2 With the exception of one patient who died of delayed bleeding, other complications were identified and treated appropriately in most cases. Similar to the findings by Baron et al.,12 we observed a higher rate of complications in patients undergoing drainage of pancreatic necrosis. Unlike pseudocysts, necrotic collections are more viscous with large amounts of debris and hence are difficult to drain. Ineffective instrumentation predisposes to infection in these patients. Although endoscopic necrosectomy and creation of multiple transmural tracts for drainage of necrotic contents are few therapeutic options, surgery is the only definitive therapy for many patients. Therefore, close collaboration with pancreatic surgeons is an absolute necessity for optimal treatment outcomes in this patient population.
Although we did not observe any difference in the rate of complications based on the modality (EUS vs. CTD) used for transmural drainage (data not shown), we still believe that EUS is indispensible for the endoscopic drainage of PFCs as it enables identification of intervening vasculature, establishes an alternative diagnosis of cyst neoplasm in cases that mimic a pseudocyst, and facilitates safe access to PFCs that do not cause a luminal compression. In a randomized trial that compared EUS and conventional endoscopy for drainage of PFCs, conventional endoscopy was successful in only 33% of patients, whereas EUS guidance enabled PFC drainage in 100% of patients.27 Patients with pancreatic necrosis are generally more hypoalbuminemic, and as a consequence, the gastric mucosal edema makes identification of PFC-induced luminal compression difficult at endoscopy.28 Also, as some of these patients are on parenteral nutrition, the distension induced by the gallbladder can mimic a luminal compression caused by a PFC. In such instances, EUS is invaluable to facilitate safe access to the PFC. Prior studies have shown that EUS-guided drainage can be performed safely even at patient bedside and within 25 min in most patients.11,29 Given these inherent advantages, we have increasingly used EUS for performing most endoscopic transmural drainages.
There are several limitations to this study. Firstly, the study design was retrospective thereby limiting the ability to investigate the effectiveness of several variables on treatment outcomes. Secondly, we included only those patients who underwent endoscopic transmural drainage of PFCs and not those treated by transpapillary pancreatic duct stent placement alone. Thirdly, these results pertain to one center and one endoscopist, and hence, the findings may not be generalized. Fourthly, the duration of follow-up was only medium term. Finally, the good clinical outcomes reported in this study could be secondary to selection bias as sicker patients may have undergone surgery or percutaneous drainage.
In conclusion, endoscopy is an effective and safe technique for the drainage of non-necrotic PFCs. Given the suboptimal outcomes in patients with necrosis, close collaboration with surgery is important to identify patients who will benefit from either treatment modality. Better accessories and techniques are required to improve the outcomes of patients undergoing endoscopic drainage of necrotic PFCs.
References
Bollen TL, van Santvoort HC, Besselink MG, van Leeuwen MS, Horvath KD, Freeny PC, Gooszen HG; Dutch Acute Pancreatitis Study Group. The Atlanta Classification of acute pancreatitis revisited. Brit J Surg 2008; 95: 6–21.
Hookey LC, Debroux S, Delhaye M, Arvanitakis M, Le Moine O, Devière J. Endoscopic drainage of pancreatic-fluid collections in 116 patients: a comparison of etiologies, drainage techniques, and outcomes. Gastrointest Endosc 2006; 63: 635–43.
Seewald S, Ang TL, Teng KCYK, Soehendra N. EUS-guided drainage of pancreatic pseudocysts, abscesses and infected necrosis. Digest Endosc 2009; 21 (Suppl. 1): S61-S65.
Smits ME, Rauws EAJ, Tytgat GNJ, Huibregtse K. The efficacy of endoscopic treatment of pancreatic pseudocysts. Gastrointest Endosc 1995; 42: 202–7.
Sahel J, Bastid C, Pellat B, Schurgers P, Sarles H. Endoscopic cystoduodenostomy of cysts of chronic calcifying pancreatitis: a report of 20 cases. Pancreas 1987; 2: 447–53.
Cremer M, Deviere J, Engelholm L. Endoscopic management of cysts and pseudocysts in chronic pancreatitis: long-term follow-up after 7 years of experience. Gastrointest Endosc 1989; 35:1–9.
Ahn JY, Seo DW, Eum J Song TJ, Moon SH, Park do H, Lee SS, Lee SK, Kim MH. Single-step EUS-guided transmural drainage of pancreatic pseudocysts: analysis of technical feasibility, efficacy, and safety. Gut Liver 2010; 4: 524–529.
Lopes CV, Pesenti C, Bories E, Caillol F, Giovannini M. Endoscopic-ultrasound-guided endoscopic transmural drainage of pancreatic pseudocysts and abscesses. Scand J Gastroentero 2007; 42: 524–529
Kruger M, Schneider AS, Manns MP, Meier PN. Endoscopic management of pancreatic pseudocysts or abscesses after an EUS-guided 1-step procedure for initial access. Gastrointest Endosc 2006; 63: 409–16.
Antillon MR, Shah RJ, Stiegmann G, Chen YK. Single-step EUS-guided transmural drainage of simple and complicated pancreatic pseudocysts. Gastrointest Endosc 2006; 63: 797–803.
Varadarajulu S, Tamhane A and Blakely J. Graded dilation technique for EUS-guided drainage of peripancreatic fluid collections: an assessment of outcomes and complications and technical proficiency (with video). Gastrointest Endosc 2008; 68: 656–66.
Baron TH, Harewood GC, Morgan DE, Yates MR. Outcome differences after endoscopic drainage of pancreatic necrosis, acute pancreatic pseudocysts, and chronic pancreatic pseudocysts. Gastrointest Endosc 2002; 56: 7–17.
Weckman L, Kylänpää M-L, Puolakkainen P, Halttunen J. Endoscopic treatment of pancreatic pseudocysts. Surg Endosc 2006; 20: 603–607.
Cahen D, Rauws E, Fockens P, Weverling G, Huibregtse K, Bruno M. Endoscopic drainage of pancreatic pseudocysts: Long-term outcome and procedural factors associated with safe and successful treatment. Endoscopy 2005; 37(10): 977–983.
Binmoeller KF, Seifert H, Walter A, Soehendra N. Transpapillary and transmural drainage of pancreatic pseudocysts. Gastrointest Endosc 1995; 42: 219–24.
Sharma SS, Bhargawa N and Govil A. Endoscopic management of pancreatic pseudocyst: A long-term follow-up. Endoscopy 2002; 34: 203–207.
Beckingham IJ, Krige JEJ, Bornman PC, Terblanche J. Long term outcome of endoscopic drainage of pancreatic pseudocysts. Am J Gastroenterol 1999; 94: 71–74.
Varadarajulu S, Trevino J, Wilcox CM, Sutton B, Christein JD. Randomized trial comparing EUS and surgery for pancreatic pseudocyst drainage. Gastrointest Endosc 2010; 71: AB 116.
Varadarajulu S, Lopes TL, Wilcox CM, Drelichman ER, Kilgore ML, Christein JD. EUS versus surgical cyst-gastrostomy for management of pancreatic pseudocysts. Gastrointest Endosc 2008; 68:649–55.
Bradley EL III. A clinically based classification system for acute pancreatitis. Summary of the international symposium on acute pancreatitis, Atlanta, GA, September 11 through 13, 1992. Arch Surg 1993; 128 (5): 586–90.
van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, van Goor H, Schaapherder AF, van Eijck CH, Bollen TL, van Ramshorst B, Nieuwenhuijs VB, Timmer R, Laméris JS, Kruyt PM, Manusama ER, van der Harst E, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, van Leeuwen MS, Buskens E, Gooszen HG; Dutch Pancreatitis Study Group. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 2010; 362: 1491–1502.
Seifert H, Biermer M, Schmitt W, Jürgensen C, Will U, Gerlach R, Kreitmair C, Meining A, Wehrmann T, Rösch T. Transluminal endoscopic necrosectomy after acute pancreatitis: a multicentre study with long-term follow-up (the GEPARD Study). Gut 2009; 1260–1266.
Ross A, Gluck M, Irani S, Hauptmann E, Fotoohi M, Siegal J, Robinson D, Crane R, Kozarek R. Combined endoscopic and percutaneous drainage of organized pancreatic necrosis. Gastrointest Endosc 2010; 71: 79–84.
Adams DB, Harvey TS and Anderson MC. Percutaneous catheter drainage of infected pancreatic and peripancreatic fluid collections. Arch Surg 1990; 125: 1554–7.
Nealon WH, Bhutani M, Riall TS, Raju G, Ozkan O, Neilan R. A unifying concept: pancreatic ductal anatomy both predicts and determines the major complications resulting from pancreatitis. J Am Coll Surg 2009; 208: 790–9.
Arvanitakis M, Delhaye M, Bali MA Matos C, De Maertelaer V, Le Moine O, Devière J. Pancreatic-fluid collections: a randomized controlled trial regarding stent removal after endoscopic transmural drainage. Gastrointest Endosc 2007; 65: 609–19.
Varadarajulu S, Christein JD, Tamhane A, Drelichman ER, Wilcox CM. Prospective randomized trial comparing EUS and EGD for transmural drainage of pancreatic pseudocysts (with videos). Gastrointest Endosc 2008; 68: 1102–11.
Varadarajulu S. EUS followed by endoscopic pancreatic pseudocyst drainage or all-in-one procedure: a review of basic techniques (with video). Gastrointest Endosc 2009; 69 (2 Suppl): S176-81.
Varadarajulu S, Eloubeidi MA, Wilcox CM. The concept of bedside EUS. Gastrointest Endosc 2008; 67: 1180–4.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Varadarajulu, S., Bang, J.Y., Phadnis, M.A. et al. Endoscopic Transmural Drainage of Peripancreatic Fluid Collections: Outcomes and Predictors of Treatment Success in 211 Consecutive Patients. J Gastrointest Surg 15, 2080–2088 (2011). https://doi.org/10.1007/s11605-011-1621-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1621-8